Abstract
Background
There have been no useful imaging methods to diagnose benign paroxysmal positional vertigo (BPPV), a common cause of vertigo, depending on the characteristic symptom.
Objective
To visualize horizontal canal (HC) BPPV using 3DCT and assess its clinical usefulness.
Subjects and methods
Ten BPPV patients were diagnosed with distinct BPPV, canalolithiasis, and cupulolithiasis of the HC (hc-BPPV, hc-BPPV-cu), which were definitely diagnosed on the basis of criteria of BPPV by the Barany Society and 10 healthy subjects without a history of dizziness were investigated using 3DCT with several different CT window values (CTWVs).
Results
The HCs of BPPV patients were clearly visualized and the luminal aspects showed differences among ears with cupulolithiasis, canalolithiasis and no symptoms healthy subjects.
Conclusions and significance
3DCT images visualized the characteristic changes of the HC of patients with BPPV compared to healthy subjects. The HC images were coincident with the clinical condition of cupulolithiasis and canalolithiasis. This imaging technique is clinically useful for diagnosing, treating and assessing the prognosis of HC BPPV
Chinese abstract
背景:目前尚无有用的影像学方法来根据特征症状来诊断良性阵发性位置眩晕(BPPV)。良性阵发性位置眩晕是眩晕的常见原因。
目的:使用3DCT将水平管(HC)BPPV可视化, 并评估其临床实用性。
受试者和方法:十名BPPV 患者被诊断出明显的BPPV、和根据由Barany Society制定的BPPV标准明确诊断出的HC管结石症和嵴顶结石症(hc-BPPV, hc-BPPV-cu)。对10例无头晕病史的健康受试者使用3DCT和几种不同的CT窗口值(CTWV)进行研究。
结果:BPPV患者的HCs清晰可见, 并且管腔显示患有管结石症和嵴顶结石症及无症状健康受试者的耳朵存在差异。
结论和意义:3DCT图像将BPPV患者的HC的特征性变化可视化, 并将其与健康受试者相比。 HC图像与管结石症和嵴顶结石症的临床病症相符。这种成像技术在临床上可用于诊断、治疗并评估HC BPPV的预后。
Introduction
Benign paroxysmal positional vertigo (BPPV) is a very common cause of dizziness which is characterized by a sudden onset of the vertiginous attack provoked by some head positions [Citation1,Citation2].
Although there have been some arguments about the cause of BPPV [Citation3–7], it has been accepted as a peripheral vestibular disease, like cupulolithiasis [Citation8] and canalolithiasis [Citation9,Citation10].
BPPV has been diagnosed with peculiar symptoms such as paroxysmal positional vertigo provoked by a change in head position, leading to loss of balance, nausea, vomiting, headache and findings with or without characteristic benign paroxysmal positional nystagmus (BPPN) [Citation3].
The Barany Society presented new diagnostic criteria for BPPV (DC-BPPV), 2015 [Citation11]. The backbone of the DC-BPPV is composed of symptoms in the semicircular canal regions. Canalolithiasis and cupulolithiasis of horizontal canal (HC) (hc-BPPV, hc-BPPV-cu), and canalolithiasis of the posterior canal (pc-BPPV) are definitely diagnosed. Canalolithiasis of the anterior canal (ac-BPPV), cupulolithiasis of the posterior canal (pc-BPPV-cu), and lithiasis of multiple canals (mc-BPPV) are classified as emerging and controversial syndromes because of rare variants of BPPV and difficulty into differentiating from central positional nystagmus [Citation11].
The findings of BPPN are the most useful tools for diagnosing and treating BPPV. However, some patients with clinically apparent BPPV have no BPPN. Such cases of BPPV must be diagnosed with vague and indefinite decisions by the clinician’s knowledge and experiences.
In the medical field, image analysis is a very useful tool not only for diagnosing and treating the disease but also for obtaining new findings pertaining to the disease. Image analysis of the temporal bone has been a very useful and powerful tool for finding temporal bone conditions, especially middle ear lesions. In addition, image analysis of the Meniere disease [Citation12,Citation13] and its manifestation, i.e. endolymphatic hydrops [Citation14], has been reported, and its usefulness has also been recognized.
However, there has not been a useful image method to clarify BPPV. The development of image analysis of BPPV will be a very useful tool for diagnosing BPPV.
It is difficult to clarify the pc-BPPV-cu [Citation11].
Meanwhile, the hc-BPPV and hc-BPPV-cu are definitively diagnosed on the basis of the diagnostic criteria formulated by the Barany Society. In this study, we focused on HC to develop a new technique for visualizing BPPV of the HC with cone beam 3DCT, in patients with canalolithiasis and cupulolithiasis of BPPV compared to those of healthy controls without a history of dizziness.
Subjects and methods
Subjects
We studied 3DCT images of 10 patients (five males and five females; mean age 53.4 years, range 38–70 years) diagnosed with hc-BPPV or hc-BPPV-cu on right side using the DC-BPPV [Citation11]. Among the 258 patients who underwent 3DCT images from January 2018 to October 2020 (), we randomly selected HC BPPV patients on right side, aged 30–70 years in our records taking into consideration the predominant age of BPPV. The distribution of patient’s age and gender were also accounted for in the selection to have an impartial consideration. All patients were treated with the Gufoni maneuver.
Table 1. Records of BPPV patients.
Ten healthy volunteers, age matched to the selected patients (five males and five females; mean age 50.6 years, range 32–69 years) and without any history of dizziness were used as controls (). This study was performed with the consent of the patients and healthy volunteers.
Table 2. Records of healthy subjects.
Methods
CT images of each subjects were taken with a polyethylene tube with full water into the bilateral external ears to determine the CT window value (CTWV) of the endolymph (). In this study, CTWV of water means that the inner ear fluid was the count for endolymph.
Figure 1. Polyethylene tube with full water and its inserted view of the CT image of the temporal bone.
CT images were acquired using a cone beam CT scanner (3D Accuitomo; J. Morita Mfg. Corp., Kyoto, Japan) under the same conditions as previously reported studies [Citation12,Citation13]: 80 kV, 6 mA; voxel size: 0.125 mm × 0.125 mm; and slice thickness 0.5 mm. CT images were acquired for a column 6 cm in diameter and 6 cm in height. Reconstructed 3D images of the inner ear were obtained using the rendering software (IVIEW) in a perspective view with a viewing angle of 15° and 0.25 mm voxel size (0.25 × 0.25 × 0.25 mm).
The views of the cutting section were adopted with a view of perfect arc of the HC and analyzed.
The patency and definition of occluded substances of HC were assessed qualitatively and semi-quantitatively using each CTWV of water, meaning endolymph (red color), otoconia-like substance (OS) (yellow color), and bony substance (white color).
Results
shows a representative inner ear, vestibule and HC of healthy volunteers adopted in the present methods. The aspects of HC luminal conditions could be clearly visualized on three different CTWVs: endolymph, otoconia, and bone. Four pathological factors of the HC condition were defined: blocked portions, canalith jam, cupulolithiasis and canalolithiasis (). Blocked and jammed portions of the HC were different in their occluded substances. The blocked portion seemed to be occluded with bony like substances in white color or missing image. Canalith jam was occluded with yellow-colored OS (). Cupulolithiasis was stained with a clearly visualized yellow color at the ampulla. There are two patterns of cupulolithiasis in which the ampulla region was totally or partially occluded with yellow-colored OS ().
Figure 2. Representative 3DCT images of the utricle and semicircular canal. (A) Vestibule and semicircular canal. (B) HC with CTWVs of endolymph (red color) and OS (yellow color) at through arc view. (C) Recognition of HC with its through arc view. Shadow shows cutting face. A: anterior canal; Aa: ampulla of anterior canal; C: common crus; CTWV: CT window value; H, HC: horizontal canal; Ha: ampulla of horizontal canal; OS: otoconia-like substance; P: posterior canal; Pa: ampulla of posterior canal; V: vestibule.
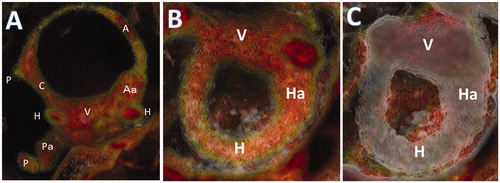
Figure 3. Five representative conditions of HC conditions, namely, normal, blocked, canalith jam, canalolithiasis and cupulolithiasis. The selection of CTWV shows its relative substance in the image. Column 1: HC image with three CTWVs, which are endolymph (red color), OS (yellow color) and bone (white color). Column 2: HC image with two CTWVs, which are endolymph (red color) and bone (white color). Colum 3: HC image with two CTWVs, which are OS (yellow color) and bone (white color). CTWV: CT window value; Bl: blocked; Cj: canalith jam; Cl: canalolithiasis; Cu: cupulolithiasis; Ha: ampulla of HC; HC: horizontal canal; OS: otoconia-like substance.
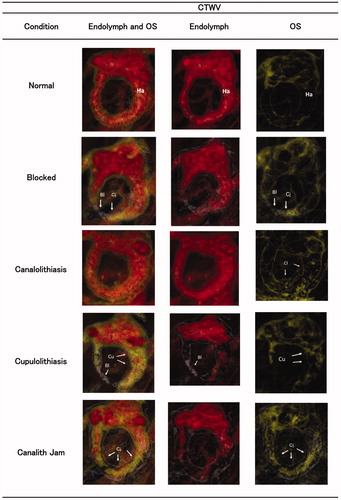
Figure 4. Two patterns of cupulolithiasis that are totally (A) or partially (B) occluded with OS (yellow color). (A) No dizzy healthy subject with totally occluded cupulolithiasis. (B) Dizzy patient with partially occluded cupulolithiasis. The ampulla of no-dizzy healthy subject with cupulolithiasis is totally occluded with OS (yellow color). Cj: canalith jam; Cu: cupulolithiasis. CTWV: CT window value; OS: otoconia-like substance.
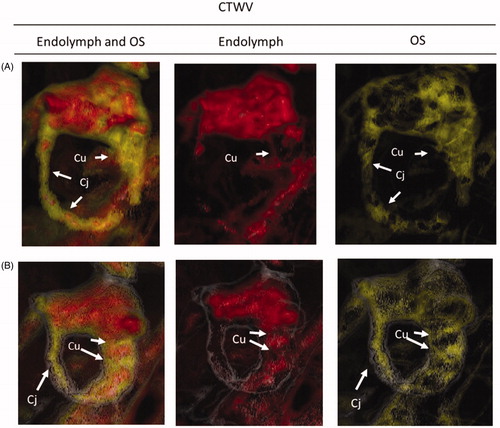
In 10 healthy subjects, there are three HCs with cupulolithiasis out of 20 HCs in which the ampullae were totally occluded with OS (yellow color) and no visible endolymph region with red color () ().
In contrast, seven HCs in four cupulolithiasis patients have a partially occluded portion of the ampulla with red colored endolymph like .
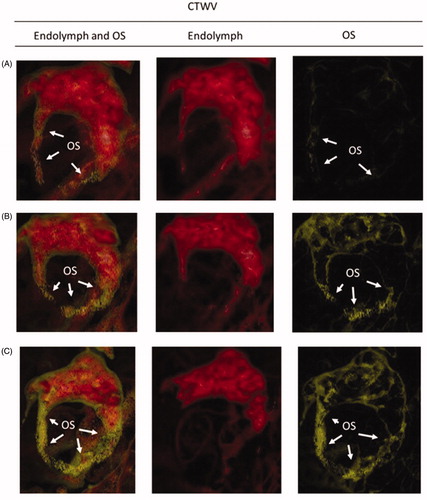
Regarding canalolithiasis, the injured degree of HC was classified by the ratio of existing endolymph (red color) and OS (yellow color) (). Level +3 indicates so much OS, like a jammed aspect, in the HC lumen that the endolymph is not visible (). Level +1 indicates that a small amount of OS (yellow) can be scarcely visible with CTWV of OS (yellow color) (A)). Level +2 is the degree between level +1 and level +3, meaning that the existing OS (yellow color) can be visible with CTWV of OS (yellow color) (). In six patients diagnosed with canalolithiasis, seven out of 12 HCs had level +2 OS, two out of 12 HCs had level +1 OS, and one out of 12 HCs had level +3 OS, respectively ().
Figure 5. The image score of injured level of canalolithiasis defined with the amount of OS. (A) Level +1: small amount OS (yellow color) can be somewhat visible with two CTWVS of endolymph (red color) and OS (yellow color), but scarcely visible only with single CTWV of OS. (B) Level +2: condition between level +1 and level +3. The existing OS (yellow color) can also be visible with CTWV of OS. (C) Level +3: so much OS like a jammed aspect, in the HC lumen where the endolymph is very small. CTWV: CT window value; HC: horizontal canal; OS: otoconia-like substance.
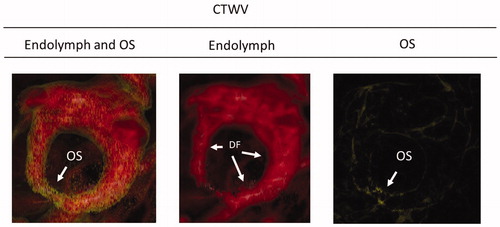
In the group of 20 HCs in 10 healthy subjects, canalolithiasis was suggested in seven HCs in six people. These seven HCs showed just a level +1 amount of OS and two HCs of which had no driving force. There were three HCs with cupulolithiasis in two healthy subjects. All these cases were totally occluded with yellow colored OS and regions devoid of water in the ampulla.
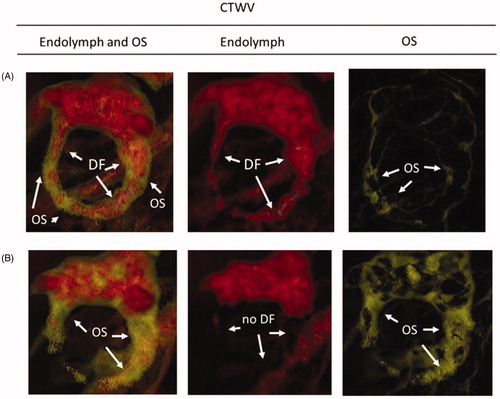
To move the existing OS in the HC, the existence of a driving force of the endolymph facing OS is necessary. The existence of a driving force was qualitatively judged whether it was around the OS between the ampulla of the HC ().
Figure 6. Existence of driving force of endolymph to move OS in the HC. It is defined as the presence or absence of endolymph (red color). (A) Driving force +: endolymph (red color) exists between the OS and the ampulla. (B) Driving forceー: no endolymph (red color) exists between around the OS and ampulla. CTWV: CT window value; DF: driving force; HC: horizontal canal; OS: otoconia-like substance.
and show the representative aspects of the HC of healthy subjects with cupulolithiasis and canalolithiasis, respectively.
Figure 7. Representative cases of healthy subjects without dizziness despite existing canalolithiasis. Small amount OS are recognized in the HC with two CTWVSs of endolymph (red color) and OS (yellow color), but its amount indicates level +1 with CTWV of OS (yellow color). CTWV: CT window value; DF: driving force; HC: horizontal canal; OS: otoconia-like substance; (cf. ): no dizzy patient with totally occluded cupulolithiasis.
Discussion
In a previous study, we reported the visualization of Meniere disease by assessing its temporal bone using cone beam CT with different CTWVs of several substances such as endolymph, soft tissue, OS and bone [Citation13]. In this study, we could clearly visualize the luminal aspect of HC using a similar technique and demonstrated its different conditions in BPPV patients and healthy subjects. In particular, the use of different CTWVs between the endolymph and OS could clearly show the luminal condition of the HC. This imaging study may not imply the real condition of the HC. There is some possibility of overestimation or underestimation of image analysis in 3DCT. However, the validity of this technique is reasonable because there are different colored regions (red and yellow) in the same HC, meaning different contents exist there, and that the same size diameter of HCs did not show the same color. These results indicate that the region colored in yellow is not a definite normal endolymph but includes the debris of detached utricular otoconia or its floating clots; there are some causes of inner ear disturbances.
Four patients with cupulolithiasis defined by the DC-BPPV could be fully detectable in this imaging study in which most cases have regions of both sides of the ears (seven out of eight HCs). These results suggest that the cupulolithiasis lesions tend to progress on both ears of the patient and more influential side of which will induce the attack of BPPV.
Although three HCs out of two healthy subjects had cupulolithiasis in the imaging study, they had no history of dizziness. The reason for the absence of dizziness can be explained by the fact that their ampulla region was almost totally occluded with OS, leading to no functioning and no power to provoke dizziness.
These events will prove the idea that if the ampulla region is totally occluded with OS, the ampulla will lose its function.
Seven out of eight HCs in the patients with diagnosed with cupulolithiasis had more than a level +2 amount of OS
These results also suggest that cupulolithiasis will ordinarily include canalolithiasis. Cupulolithiasis may be one of the progressive condition of canalolithiasis.
In the canalolithiasis group defined by the DC-BPPV, eight out of 12 HCs have level +2 to level +3 amount of OS. Meanwhile, some OSs exist in HC even in healthy subjects without the experience of BPPV attack in their history. Seven out of 20 HCs in 10 healthy subjects showed only a level +1 amount of OS. This small amount of OS will explain not enough power to provoke the ampulla to dizziness.
In the occurrence of a dizzy attack due to canalolithiasis, two factors are necessary, namely, some amount of existing OS in the HC and a driving force of the endolymph to move OS. When there is no endolymph between the OS and the ampulla, both ampullopetal and ampullofugal flow will not occur, even though a sufficient amount of OS exists to provoke the ampulla. From this point of view, the existence of the driving force was judged by the available endolymph or not ( and show driving force + or –). By assessing these two factors, the occurrence and prognosis of a dizziness attack of canalolithiasis may be assessed.
Two patterns of obstruction of the HC were recognized: canalith jam with OS and blocks probably due to bony-like substances. Canalith jam existed seven out of eight HCs (87.5%) in four cupulolithiasis patients, six out of 12 HCs (50%) in six patients with canalolithiasis and 12 out of 20 HCs (60%) in healthy subjects. Although the incidence of canalith jam is highest in cupulolithiasis cases, canalith jam may be an ordinal event in the HC also in healthy subjects.
The existence of canalith jam has been reported in the intractable case of BPPV of the posterior canal [Citation15], because of many source of otoconia in a jam can be the cause of a BPPV attack. However, 60% of the healthy group did not have a dizzy attack despite canalith jam existing in their HC. This may be explained by the fact that their existing free OS amounts are relatively smaller than those of the canalolithiasis and cupulolithiasis groups ( and ).
There is some difference in the incidence of ‘blocked portion’ in the HC between the healthy subjects and pathological groups of cupulolithiasis and canalolithiasis. There were six out of eight HCs (75%) and four out of 12 HCs (32.3%) with blocked portion, respectively, in the cupulolithiasis and canalolithiasis groups. Meanwhile, the ratio was relatively small in healthy subjects: three out of 20 HCs (15%). Although it is difficult to statistically analyze from these small number of cases, this result means that canalith jam is an ordinal event in the HC, but the incidence of blocks in the HC may be a pathognomonic event in the HC. When the blocked portion existed in the HC, both ampullopetal and ampullofugal endolymph flow decreases or is blocked. The degree of altered endolymph in the ampulla depends on the cases. Some surgeries have been performed in cases of intractable BPPV. In particular, canal plugging of the posterior canal has been reported [Citation16,Citation17]. This surgical effect depends on stopping ampullopetal and ampullofugal endolymph flow and its effect on the ampulla.
The spontaneous blocked event of the HC and total obstruction of the ampulla in healthy subjects could occur as a natural course by which no manifest dizziness may be felt like a surgery effect.
The alteration of canalith jam and block events in the HC due to time lapse or ageing effects should be elucidated in future study.
Patients with BPPV sometimes have multi-canal insults [Citation18–20], in which cases the decision of the lesional canals is difficult. In the cases of probable BPPV patients without BPPN, its diagnosis is not distinct. We adopted distinct HC BPPV patients diagnosed by just showing BPPN so that we could assess the usefulness of 3DCT imaging for the diagnosis of BPPV. However, there is a possibility that our HC BPPV patients had also multi-canal insulted, but which was not manifested. The imaging study of the assessment of multi-canal insults will be elucidated in a future study.
The present image data were almost completely coincident with the diagnosis of HC BPPV according to the DC-BPPV. This means that the present image study can precisely imply the lesions of HC BPPV and that the substances in the yellow color of CTWV imply OS or infectious particle or debris near the otoconia.
Although it is necessary to further investigate additional HC BPPV patients as a large sample and verify the differences between 3DCT imaging and histopathological analysis and statistical analysis, the present 3DCT image study will be a useful tool to diagnose HC BPPV and assess its prognosis.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Barany R. Diagnose von Krankheitserscheinungen im Bereiche des Otolithen apparates. Acta Otolaryngol. 1921;2:434–437.
- Dix MR, Hallpike CS. The pathology, symptomatology and diagnosis of certain common disorders of the vestibular system. Ann Otol Rhinol Laryngol. 1952;61(4):987–1016.
- Boniver R. Benign paroxysmal positional vertigo: an overview. Int Tinnitus J. 2008;14(2):159–167.
- Hall SF, Ruby RR, McClure JA. The mechanics of benign paroxysmal vertigo. J Otolaryngol. 1979;8(2):151–158.
- Gordon AG. BPPV―benign paroxysmal positional or bubble provoked positioning vertigo? J Neurol Sci. 1992;111(2):229–230.
- Gacek RR. Transection of the posterior ampullary nerve for the relief of benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 1974;83(5):596–605.
- Gacek RR. Pathology of benign paroxysmal positional vertigo revisited. Ann Otol Rhinol Laryngol. 2003;112(7):574–582.
- Schuknecht HF. Cupulolthiasis. Arch Otolaryngol. 1969;70:765–778.
- Parnes LS, McClure JA. Free-floating endolymph particles: a new operative finding during posterior semicircular canal occlusion. Laryngoscope. 1992;102(9):988–992.
- Kao WTK, Parnes LS, Chole RA. Otoconia and otolithic membrane fragments within the posterior semicircular canal in benign paroxysmal positional vertigo. Laryngoscope. 2017;127(3):709–714.
- von Brevern M, Bertholon P, Brandt T, et al. Benign paroxysmal positional vertigo: diagnostic criteria. J Vestib Res. 2015;25(3–4):105–117.
- Yamane H, Sunami K, Iguchi H, et al. Assessment of Meniere’s disease from a radiological aspect – saccular otoconia as a cause of Meniere's disease? Acta Otolaryngol. 2012;132(10):1054–1060.
- Yamane H, Iguchi H, Konishi K, et al. Three-dimensional cone beam computed tomography imaging of the membranous labyrinth in patients with Meniere's disease. Acta Otolaryngol. 2014;134(10):1016–1021.
- Nakashima T, Naganawa S, Sugiura M, et al. Visualization of endolymphatic hydrops in patients with Meniere's disease. Laryngoscope. 2007;117(3):415–420.
- Epley JM. Human experience with canalith repositioning maneuvers. Ann N Y Acad Sci. 2001;942:179–191.
- Parnes LS, McClure JA. Posterior semicircular canal occlusion in the normal hearing ear. Otolaryngol Head Neck Surg. 1991;104(1):52–57.
- Maas BDPJ, van der Zaag-Loonen HJ, van Benthem PPG, et al. Effectiveness of canal occlusion for intractable posterior canal benign paroxysmal positional vertigo: a systematic review. Otolaryngol Head Neck Surg. 2020;162(1):40–49.
- Lopez-Escamez JA, Molina M, Gamiz M, et al. Multiple positional nystagmus suggests multiple canal involvement in benign paroxysmal vertigo. Acta Otolaryngol. 2005;125(9):954–961.
- Tomaz A, Ganança MM, Ganança CF, et al. Benign paroxysmal positional vertigo: concomitant involvement of different semicircular canals. Ann Otol Rhinol Laryngol. 2009;118(2):113–117.
- Balatsouras DG. Benign paroxysmal positional vertigo with multiple canal involvement. Am J Otolaryngol. 2012;33(2):250–258.
