Abstract
Background
The treatment of head and neck cancer is an intensive multimodal treatment that has a great impact on the individual patient.
Aims/Objectives
This study aimed to evaluate acute and long-term complications associated with mandibular resections and reconstructions.
Material and Methods
We retrospectively retrieved data on complications and recurrences among patients that underwent mandibular resections and reconstructions for treating oral cavity cancer (n = 190 patients) and osteoradionecrosis (ORN, n = 72). Reconstructions included composite grafts (n = 177), soft tissue flaps (n = 61), or primary closure without any graft (n = 24).
Results
Forty-two patients that underwent reconstructions with composite grafts displayed serious complications (Clavien–Dindo ≥ IIIa). The complication rates were similar between patients treated for oral cavity cancer and patients treated for ORN. Patients that underwent a primary closure without any graft, had a significantly lower risk of complications compared to patients that underwent the other treatments. After hospitalization, 181 patients (69%) had at least one complication.
Conclusions
A majority of patients undergoing resection and reconstruction due to oral cancer/ORN suffered from postoperative complications regardless of indication, comorbidity status or reconstruction technique. The risk of Clavien–Dindo grade IIIa–V events was significantly lower for patients treated with primary closure without grafts
Significance
The results from this study clarifies the importance of in-depth analyse prior to decision of treatment for patients with head and neck cancer.
Chinese Abstract
背景:头颈癌的治疗是一种强化型多模式治疗, 对患者造成很大影响。
目的:本研究旨在评估与下颌骨切除和重建相关的急性和长期并发症。
材料和方法:我们回顾性检索了因治疗口腔癌(n = 190 )和放射性骨坏死(ORN, n = 72)而接受下颌骨切除和重建的患者的并发症和复发的数据。下颌骨重建包括复合移植物(n =177)、软组织瓣 (n = 61) 或没有任何移植物的闭合 (n = 24)。
结果:42 名接受复合移植物重建的患者表现出严重的并发症(Clavien-Dindo IIIa)。在接受口腔癌治疗的患者和接受 ORN 治疗的患者之间, 并发症发生率相似。接受无移植物闭合术的患者与接受其他治疗的患者相比, 并发症风险显著低。住院后, 181 名患者(69%)出现至少一种并发症。
结论:大部分患者因口腔癌/ORN而接受切除重建后, 都会出现术后并发症, 与适应症、合并症状态或重建技术无关。接受无移植物闭合治疗的患者, 发生 Clavien-Dindo IIIa-V 级事件的风险显著低。
意义:本研究的结果表明, 在决定头颈癌患者的治疗方法之前, 进行深入分析是很重要的。
Introduction
Head and neck cancer comprises a heterogeneous group of malignant tumours with differences in natural history, treatment, and prognosis. Although the incidence of HPV-associated oropharyngeal carcinoma has become nearly epidemic [Citation1], oral cavity cancer remains the most frequent head and neck cancer worldwide [Citation2]. The most common tumour within the oral cavity that affects the mandible is squamous cell carcinoma; this tumour originates from the epithelial cells that cover the tongue, the floor of the mouth, and the gingiva [Citation3]. A malignant tumour that originates from mandibular bone tissue is considered an orphan disease, which mainly includes sarcomas [Citation4,Citation5].
Malignant lesions from several sites in the oral cavity can invade the mandibular bone. Advanced stage oral cancer is often treated with surgery combined with radiotherapy, and sometimes chemotherapy and/or targeted therapy is included. Surgery aims to eradicate the tumour radically, and combined treatments have been shown to increase survival.
Mandibular reconstruction primarily aims to rehabilitate the patient functionally and aesthetically. Several different techniques for mandible reconstruction have been introduced over the past few decades, and their uses have been debated. The current gold standard for functional reconstruction is a microvascular technique with autogenous bone transplants [Citation6]. For patients with a high risk of early mortality, mandibular resections followed by less advanced reconstructions can be lifesaving.
Treatments that include radiotherapy run the risk of late radiotherapy consequences, including hypovascularity and hypoxia, which affect cellular activity, and collagen formation in the bone and surrounding tissues. One of the most debilitating complications of radiation therapy in patients treated for head and neck cancer is osteoradionecrosis (ORN) [Citation7].
The present study aimed to evaluate acute and long-term complications after mandibular resections and reconstructions in patients treated for oral cavity cancer or ORN.
Materials and methods
Patient data
We reviewed medical records from four tertiary hospitals in Sweden to identify patients that underwent segmental resections of the mandible due to malignant tumour or ORN, between 2000 and 2014. We identified 262 patients (153 men and 109 women, mean age: 67 years). The four hospitals covered the middle and northern parts of Sweden and comprised a population exceeding five million. We collected the following patient data: age, sex, type of surgery, chemotherapy, donor sites for composite grafting, and duration of the surgical procedure (). All data were recorded in a web-based database designed by the authors.
Table 1. Characteristics of the 262 patients included in the study.
We identified three reconstruction techniques: primary closure without any graft, soft-tissue flap, and composite flap. The surgical technique was based on tumour status, comorbidity, and performance status. Treatment plans were determined by a multidisciplinary tumour board, according to national and international praxis. We recorded data on comorbidities, tumour stage, and tumour site (i.e. gingiva, mandibular bone, floor of the mouth, tongue, or bucca).
Complications of the mandibular reconstruction were classified as early or late. Early complications occurred during the hospitalization period at the tertiary referral hospital and were graded according to Clavien–Dindo classifications [Citation8]. Late complications occurred after the initial hospitalization period and at least one month post-surgery, and comprised ORN, pathological mandibular fractures, transcutaneous oral fistula, pain, patient-reported trismus, osteosynthesis fracture, osteosynthesis material-related infection, and exposed osteosynthesis material. Age as a risk factor was in the present cohort assessed with a cut-off value of 65 years between young and old.
The study was performed according to the ethical standards of the Declaration of Helsinki, and it was approved by the Regional Ethical Review board in Umeå (Dnr: 2012-250-31 M, 2013-232-32 M, 2014-197-32 M).
Statistical analysis
Patients were divided into groups based on reconstruction techniques and indications. Complication rates were compared between groups. Categorical variables were compared with Fisher’s exact test. Continuous variables were compared with linear regression models (ANOVA). Associations between the early (Clavien–Dindo grade) and late complications and the various risk factors were assessed with unconditional logistic regression models. Results from these models are expressed as odds ratios and 95% confidence intervals (95% CI). P-values from these models were calculated with Wald tests.
Survival times were calculated from the date of mandibular resection to the date of death or December 31, 2016, whichever came first. Recurrence-free survival was calculated from the date of operation to the earliest date of recurrence, death, or December 31, 2016.
Survival was estimated with the Kaplan-Meier technique and expressed as the cumulative incidence. The time to death or failure was compared between groups with the log-rank test. Associations between clinical factors and time to death were modelled with proportional hazards regression, and results are expressed as the hazard ratio and 95% CI. All multivariate models included all of the factors listed in the corresponding tables. In all statistical analyses, p-values <.05 were considered significant.
Results
Sample
Of 262 patients that required segmental mandibular resections, 190 (72%) had oral cavity cancer and 72 (28%) had ORN (). Primary closures without grafts required significantly shorter operation times than the other reconstruction techniques. Patients that received composite grafts were younger and had less comorbidities than patients in the other groups. describes the different vascularized composite bone grafts and soft tissue flaps used in composite graft treatments.
Table 2. Patient and surgical characteristics for three reconstruction techniques.
Table 3. Descriptions of composite grafts in 177 patients and soft tissue flaps in 61 patients.
Three patients experienced events that led to death during the postoperative hospital stay. Sixty-three patients (24%) had Clavien–Dindo grade IIIa or higher complications, and 181 (69%) patients had one or more late complications. The risk of Clavien–Dindo grade IIIa–V events was significantly lower for patients treated with primary closure without any grafts, compared to patients treated with soft-tissue reconstructions (p = .049) or composite grafts (p = .028). The Clavien–Dindo grades of surgical complications were similar between patients treated for oral cavity cancer (n = 119) and those treated for ORN (n = 48).
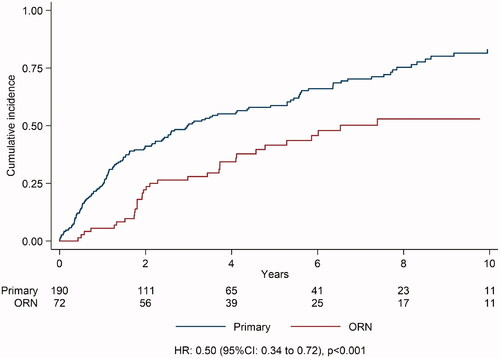
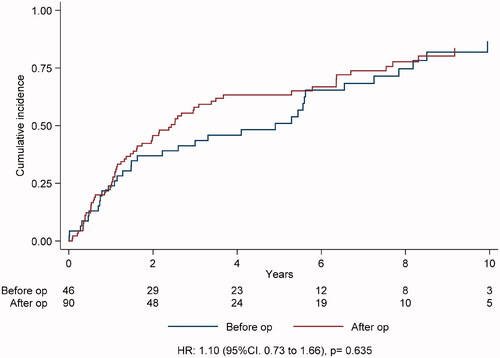
We performed multivariate unconditional logistic regression model analyses to evaluate whether early complications, late complications, and cancer recurrences were associated with age, sex, tumour site, tumour stage, reconstruction technique, and comorbidity (). For patients under 65 year the risk for late complications was significantly higher (p = 0.022). Patients with tumour stage 0–II demonstrated a significantly higher risk of late complications (p =.034). The incidence of cancer recurrence was significantly higher in patients aged <65 years (p = .022), women (p = .028), patients with tumours originating from the gingiva and primary bone versus other sites (p = .039), and patients treated for primary tumours versus ORN (p < .001). Among the 190 patients that underwent resections of a primary tumour, 136 received additional radiotherapy. The complications and recurrence rates were similar for patients that received preoperative (n = 46) and postoperative (n = 90) radiotherapy.
Table 4. Multivariate analysis of the risk of complications and recurrence.
The median follow-up for all 262 patients was 7.8 years (1.4 − 17 years). During the follow-up period, 170 patients died. The median times to all-cause death were 3.0 years, for the oral cavity cancer group, and 6.5 years for the ORN group. A multivariate Cox regression analysis of overall survival showed that stage III-IV tumours significantly increased the risk of death (p = .034). The cumulative incidence of death was significantly higher in the primary cancer group than in the ORN group (). Among patients with oral cavity cancer, the cumulative incidence of death was not significantly different between patients that received preoperative (n = 46) and those that received postoperative (n = 90) radiotherapy ().
Discussion
This retrospective study evaluated acute and long-term complications after mandibular resections and reconstructions in patients with oral cavity cancer (72%) or ORN (28%). Most reconstructions (67%) were performed with a composite graft, primarily a free vascularized fibula graft. Nearly one quarter of patients (23%) received soft tissue reconstruction. Few patients (9%) received primary closure without grafts, which resulted in a relatively shorter surgery. These patients tended to be older and had a lower rate of serious post-operative complications, compared to the two other groups. These findings indicated that the more vulnerable patients benefited from less advanced reconstructions, as reflected by the low complication rate.
We used the Clavien–Dindo classification to define early complications [Citation9]. We found that the serious complication (Clavien–Dindo ≥ IIIa) rates were similar between patients treated for oral cavity cancer and those treated for ORN. This finding was consistent with two previous studies [Citation10,Citation11] that reported approximately the same complication rates after free-flap reconstructions in patients with oral cancer and patients with oropharyngeal cancer. In the present study, we observed total or partial flap failure in 14% of patients.
A current issue of concern is how to treat oral cancers that involve the mandible in patients with a high risk of perioperative death. We showed that the incidence of Clavien–Dindo grade IIIa-V was lower in patients with primary closure than in patients that received other techniques. In addition, we found no association between age or comorbidity and the incidence of early complications. Similarly, Blackwell et al. [Citation12] showed that the incidence of medical and reconstructive complications did not differ between older and younger patients. However, our finding that primary closure was associated with a lower incidence of general complications may be most relevant to older, more vulnerable patients that might not tolerate a free-flap operation.
The literature offers little information about the success rates and long-term complications associated with mandibular reconstructions. Indeed, the use of reconstruction plates without bony reconstruction runs high risks of postoperative oral incompetence and hardware exposure [Citation5,Citation13]. Postoperative oral incompetence commonly reduces the physical function and results in oral disability. One shortcoming of this retrospective study is that we had no viable data on oral function. This topic must be analysed in a prospective study on patients undergoing mandibular resection and reconstruction.
In our cohort, over two-thirds of patients experienced at least one late complication. Moreover, we found that patients <65 years old and patients with an initially low tumour stage were at increased risk of late complications. We also found that the risk of cancer recurrence was significantly increased in patients <65 years of age, women, patients with tumours that originated from the gingiva and primary bone, and patients treated for oral cavity cancer (compared to those treated for ORN). It has been questioned whether, in the surgical management of head and neck cancer, mandibular microvascular reconstruction can be justified for older patients [Citation14]. Dimovska et al. [Citation15] suggested that comorbidity status should be the primary guide for surgical decision-making. However, in the present study, we found that comorbidity did not affect survival; the only prognostic factor for death was the initial tumour stage.
We found that the choice between preoperative and postoperative irradiation did not significantly impact the cumulative incidence of death in patients treated for oral cavity cancer. Previously, both Tall et al. [Citation16] and Mucke et al. [Citation17] found that preoperative radiotherapy was associated with an increased risk of flap failure. Consequently, Tall et al. [Citation16] recommended postoperative radiotherapy, when possible, or early reconstruction after radiotherapy.
The results from this retrospective study indicated that mandibular reconstruction was associated with a high incidence of complications, regardless of the indication, comorbidity status, and reconstruction technique. More comprehensive research is needed on late complications in mandibular reconstruction [Citation18].
In future, other factors, such as the oral cavity site, the effect on oral function, patient age, and the volume of bony free flaps, should be studied in a prospective manner to identify which patients are most likely to benefit from a given surgical treatment.
Methodological considerations/limitations
This study had some limitations. First, due to the retrospective approach, we might have underestimated the number of eligible patients, due to inconsistencies in reporting at the four tertiary hospitals. Second, our patients were treated over a period of 15 years. Thus, different surgeons could have been involved in patient care.
Disclosure statement
The authors declare no financial or personal relationships with other people or organizations that could inappropriately influence this study. Conflicts of interest: none. All authors have approved the final article.
Additional information
Funding
References
- Näsman A, Attner P, Hammarstedt L, et al. Incidence of human papillomavirus (HPV) positive tonsillar carcinoma in Stockholm, Sweden: an epidemic of viral-induced carcinoma? Int J Cancer. 2009;125(2):362–366.
- Filleul O, Preillon J, Crompot E, et al. Incidence of head and neck cancers in Belgium: comparison with worldwide and french data. Bull Cancer. 2011;98(10):1173–1183.
- Zini A, Czerninski R, Sgan-Cohen HD. Oral cancer over four decades: epidemiology, trends, histology, and survival by anatomical sites. J Oral Pathol Med. 2010;39(4):299–305.
- Young CW, Pogrel MA, Schmidt BL. Quality of life in patients undergoing segmental mandibular resection and staged reconstruction with nonvascularized bone grafts. J Oral Maxillofac Surg. 2007;65(4):706–712.
- Bianchi B, Ferri A, Ferrari S, et al. Reconstruction of anterior through and through oromandibular defects following oncological resections. Microsurgery. 2010;(a)30(2):97–104.
- Zaghi S, Danesh J, Hendizadeh L, et al. Changing indications for maxillomandibular reconstruction with osseous free flaps: a 17-year experience with 620 consecutive cases at UCLA and the impact of osteoradionecrosis. Laryngoscope. 2014;124(6):1329–1335.
- Raggio B, Winters R. Modern management of osteoradionecrosis. Curr Opin Otolaryngol Head Neck Surg. 2018;26(4):254–259.
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213.
- Miyamoto S, Nakao J, Higashino T, et al. Clavien-Dindo classification for grading complications after total pharyngolaryngectomy and free jejunum transfer. PLoS One. 2019;14(9):e0222570.
- Lodders JN, Schulten EA, de Visscher JG, et al. Complications and risk after mandibular reconstruction with fibular free flaps in patients with oral squamous cell carcinoma: a retrospective cohort study. J Reconstr Microsurg. 2016;32(6):455–463.
- Al-Hayder S, Elberg JJ, Charabi B. Clinical outcome and health-related quality-of-life following microsurgical reconstruction in patients with oral and oropharyngeal cancer. Acta Otolaryngol. 2017;137(5):541–545.
- Blackwell KE, Azizzadeh B, Ayala C, et al. Octogenarian free flap reconstruction: complications and cost of therapy. Otolaryngol Head Neck Surg. 2002;126(3):301–306.
- Bianchi B, Ferri A, Ferrari S, et al. Reconstruction of lateral through and through oro-mandibular defects following oncological resections. Microsurgery. 2010;30(7):517–525.
- Sarris EG, Harrington KJ, Saif MW, et al. Multimodal treatment strategies for elderly patients with head and neck cancer. Cancer Treat Rev. 2014;40(3):465–475.
- Dimovska EO, Clibbon JJ, Moncrieff MD, et al. Microsurgical reconstructions for head and neck cancers in elderly aged >80 years: an analysis of surgical outcomes and quality of life. Ann Surg Oncol. 2016;23(5):1684–1692.
- Tall J, Björklund TC, Skogh AC, et al. Vascular complications after radiotherapy in head and neck free flap reconstruction: Clinical outcome related to vascular biology. Ann Plast Surg. 2015; 75(3):309–315.
- Mücke T, Rau A, Weitz J, et al. Influence of irradiation and oncologic surgery on head and neck microsurgical reconstructions. Oral Oncol. 2012;48(4):367–371.
- Brown JS, Lowe D, Kanatas A, et al. Mandibular reconstruction with vascularised bone flaps: a systematic review over 25 years. Br J Oral Maxillofac Surg. 2017;55(2):113–126.