Abstract
Background
Digital modeling and three-dimensional (3D) printing techniques have been used to assist the resection of the laryngeal lesions and repair the remnant larynx in glottic cancer patients with anterior commissure involvement.
Aims/objectives
To evaluate the feasibility of digital modeling and 3D printing of titanium mesh for thyroid cartilage reconstruction in partial laryngectomy, and compare the advantages and disadvantages with crico-hyoido-epiglottopexy (CHEP).
Material and methods
Forty-four glottic cancer patients with anterior commissure involvement were randomly assigned into group A and group B. The digital modeling and 3 D printing were used for patients in group A, and patients in group B underwent the modified CHEP.
Results
In group A, 10 patients underwent tracheotomy and tracheal tube was removed after 2 weeks. All the patients were discharged within 10 d after surgery, and the majority of them had a satisfactory level of pronunciation. In group B, the majority of the patients were discharged 2 − 3 weeks after surgery with a moderate level of pronunciation.
Conclusions and significance
The proposed surgical method, employing digital modeling and 3D printing to facilitate resection of laryngeal lesions and reconstruction of residual larynx, exhibited to be beneficial for accurate reconstruction of thyroid cartilage and soft tissues.
Chinese Abstract
背景:数字建模和三维 (3D)打印技术已被用于辅助前连合受累声门癌患者的喉部病变切除及残喉修复。
目的:评估在进行部分喉切除术时, 钛网数字建模和 3D 打印对甲状腺软骨重建的可行性, 并将其与环舌骨会厌固定术(CHEP)进行优缺点比较。
材料与方法:44 名前连合受累声门癌患者随机分为A组和B组。采用数字建模和3D打印的患者为A组, 接受改良CHEP的患者为B组。
结果:A组10例患者接受气管切开术并在两周后拔除气管插管。所有患者均在术后 10 天内出院, 其中大部分患者有满意的发音水平。 B组大部分患者术后2-3 周出院, 发音水平中等。
结论和意义:本文建议的手术方法, 采用数字建模和 3D打印来辅助喉部病变切除和残喉重建, 显示出对甲状腺软骨和软组织的准确重建的有利之处。
Introduction
Laryngeal cancer (LC) is the second most common cancer of the head and neck, accounting for approximately 30–40% of all head and neck malignancies and 1–2.5% of all malignancies in the human body. Patients with early-stage glottic cancer have shown a relatively good prognosis [Citation1]. Both radiotherapy and laser surgery have exhibited similar therapeutic effects on early-stage glottic cancer. However, there is no perichondrium of the thyroid cartilage at the anterior commissure. Therefore, the therapeutic effects on patients with early-stage glottic cancer significantly decrease [Citation2,Citation3]. There is a noticeable challenge to accurately indicate the influence of anterior commissure involvement on local control, survival, and laryngeal preservation in patients with early-stage glottic cancer [Citation4–6]. A previous study reported that carbon dioxide laser microsurgery for early laryngeal carcinoma can prolong survival and improve quality of life of patients [Citation7]. In recent years, a number of scholars have used plasma radio-frequency ablation to achieve good results in the treatment of LC, while the long-term effects of the mentioned method need further verification [Citation8,Citation9].
Postoperative radiotherapy is recommended following surgical resection of the primary tumor for the majority of patients with high-grade tumors, and for selected patients with large or marginally excised, low-grade tumors. The crico-hyoido-epiglottopexy (CHEP) is an important option for laryngeal surgical preservation, especially for tumors with anterior commissure involvement and/or subglottic extension less than 5 mm [Citation7,Citation10,Citation11]. In order to avoid respiratory obstruction caused by laryngeal cavity edema and aspiration pneumonia during the recovery of swallowing function, patients undergoing CHEP need to receive tracheotomy and a gastric tube, seriously influencing patients’ quality of life postoperatively. Although several clinicians have achieved promising results through the improvement of CHEP (e.g. application of supra-cricoid partial laryngectomy (SCPL) [Citation12] with CHEP), it is still infeasible to avoid the occurrence of aspiration, and the quality of pronunciation is unsatisfactory as well [Citation13]. Thus, digital modeling and three-dimensional (3D) printing can be used to assist the precise removal and repair of thyroid cartilage. The structural support of larynx can be rebuilt, and then, patients’ quality of life can be elevated through a series of technical improvements. This study aimed to assess the feasibility of application of digital modeling and 3D printing of titanium mesh for reconstruction of thyroid cartilage in partial laryngectomy, and compare the advantages and disadvantages of the mentioned methods with CHEP.
Methods
Clinical data
This study included 44 male patients (mean age, 53 years old) who were diagnosed with LC with anterior commissure involvement in our hospital between March 2017 and March 2020, and required to undergo partial resection of laryngeal tumors. All patients were randomly allocated to groups A and B. According to the 2018 Union for International Cancer Control (UICC) TNM classification, cases in group A were assigned into subgroups of cT2N0M0 (n = 13), cT3N0M0 (n = 5), and cT2N1M0 (n = 4); cases in group B were assigned into subgroups of cT2N0M0 (n = 15) and cT3N0M0 (n = 7, in which one patient refused to undergo surgery) (). All the procedures were performed in accordance with the Declaration of Helsinki (1975). In addition, 3D-computed tomography (3D-CT) and endoscopy of the larynx were carried out to find out the exact site and size of tumor. In group A, the data of 3D-CT were imported into MIMICS version 21.0 software (Materialise NV, Leuven, Belgium), combined with the results of endoscopy of the larynx, in order to indicate osteotomy line of thyroid cartilage and laryngeal tumors formed in tissues of the larynx using digital modeling, and to make a personalized osteotomy guide plate and a customized titanium mesh by 3D printing (). As mentioned earlier, one case in group B refused to undergo surgery and left hospital after being diagnosed with LC by biopsy. The other cases in group B underwent the modified CHEP. On the basis of the original CHEP (retaining at least one cricoarytenoid joint), the hyoid bone was removed, the root of the tongue was pulled down, and the root of the epiglottic, the root of the tongue, and the submental muscle were sutured and fixed. The trachea was not dissociated, and the thyroid was kept intact (the preserve hyoid bone was preserved and the cricoid cartilage was lifted up in the original CHEP procedures)[Citation11].
Figure 1. (A) The setting of the osteotomy line and the guide plate. (B) Simulation of the 3D-printed personalized titanium model. (C) Fixing of the guide plate with the osteotomy line. (D) Reconstruction of the thyroid cartilage with the 3D-printed personalized titanium model.
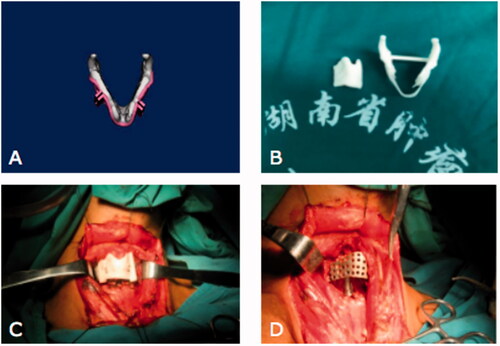
Table 1. Patient grouping.
Treatment
Surgical procedures
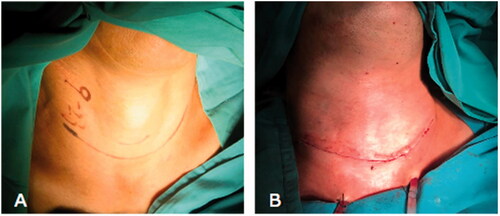
Group A: Tracheotomy was performed in 10 cases (cT2N0M0 (n = 3) for cases with severe mixed ventilation dysfunction; cT2N1M0 (n = 3); and cT3N0M0 (n = 4)) before general anesthesia. The other 12 cases underwent general anesthesia after nasal intubation without tracheotomy (). Transverse incision was performed along the lower neck skin 1–2 cm above the sternum, and the flap was exposed in the subplastysmal space to the hyoid bone level. If suspicious lymph nodes were detected by rapid frozen-section assessment for sentinel lymph nodes, selective neck dissection (II–IV) was carried out. The strap muscles were exposed and divided in the midline. The anterior wall of thyroid cartilage was exposed and vertical incisions were made on both sides of the thyroid cartilage using the personalized osteotomy guide plate. The laryngeal cavity and the tumor were exposed from the crico-thyroid membrane or above the thyroid cartilage. A 0.3–0.5 cm safe margin was made to guide tumor resection under direct vision. The residual margins were confirmed to be negative by rapid frozen section. A personalized titanium mesh was fixed on the residual thyroid cartilage with titanium nails to reconstruct the thyroid cartilage (). The inner aspect of the titanium mesh was covered by the omohyoid muscles. The sternohyoid muscles were used to cover the outer aspect of the titanium mesh. The skin was closed in two layers and the wound was covered with compression bandaging. In group B, all the cases underwent tracheotomy before general anesthesia, and then, they received the modified CHEP.
Postoperative treatment
No nasogastric tube was placed in patients in group A. Mash diet (oral feeding) was encouraged after 2 d of postoperative intravenous nutrition. Based on different degrees of aspiration, a mash was gradually transitioned to semi-fluid, fluid, and general diet. Patients in group B received nasogastric feeding through a gastric tube on the second day postoperatively. According to patients’ clinical conditions, mash diet (oral feeding) was given at 10–12 d after surgery. All the patients underwent intravenous injection of antibiotics for 7 d. The time to appropriate antimicrobial therapy for patients with pneumonia was properly calculated.
Postoperative treatment
Only three cases (cT2N1M0) in group A underwent radiotherapy.
Outcome measures
Aspiration
The degree of aspiration was divided to four grades: no aspiration (−); mild aspiration (+; eating mashed food without cough, while drinking liquid with cough); moderate aspiration (++; eating mashed food without cough); and severe aspiration (+++; unable to eat orally).
Pronunciation
According to the standard of pronunciation evaluation presented by Wu D [Citation14], the pronunciation can be divided to three levels: satisfactory, medium, and poor. The satisfactory level indicates a slight hoarseness as a sound is loud enough. The poor level means the necessity of a significant effort owning to the presence of whisper sounds. The medium level represents pronunciation between satisfactory and poor levels.
Removing gastric tube and tracheal tube
Gastric tube and tracheal tube were removed when there was no dyspnea and no aspiration during drinking liquid.
Postoperative length of hospitalization
The day of discharge was determined according to the wound healing, swallow function, and lung conditions.
Follow-up
The follow-up was conducted regularly. Endoscopy of larynx was performed every 3–6 months. CT scan of larynx and chest, and color Doppler ultrasound of abdomen were carried out every 6–12 months to evaluate local recurrence, lymph node metastasis, and distant metastasis.
Statistical analysis
Data were presented as mean ± standard deviation (SD). The Chi-square test was used to compare differences in aspiration and pronunciation after surgery between groups A and B. Statistical significance was set at p < .05. The Student’s t-test was employed to compare differences in length of stay and removal of tracheal tube after surgery between groups A and B. All the statistical analyses were undertaken using SPSS version 13.0 software (IBM, Armonk, NY).
Results
Aspiration
Group A: No gastric tube was placed in none of the cases. Mash was given on the third day postoperatively. A mild level of aspiration was found in 2 cT3 cases, and no aspiration was detected in the other cases. After swallowing exercises, all cases were discharged on the tenth day postoperatively with no aspiration ().
Table 2. Aspiration of the cases in the two groups.
Group B: One case refused to undergo surgery. Nasal feeding was performed on the second day postoperatively in the other cases. A moderate level of aspiration was found when mash was given orally on the 10–12th days postoperatively. After swallowing exercises, no aspiration was found in two cases; besides, 15 d after surgery, a mild level of aspiration was detected in eight cases, who were discharged with gastric tube and tracheal tube to practice swallowing. A moderate level of aspiration and pneumonia were found in one case, who was discharged when the pneumonia was controlled 21 d after surgery. After a prolonged practice, the case with pneumonia could eat orally with no aspiration 2 months after surgery ().
Pronunciation
No poor pronunciation was detected in none of the cases in either group A or group B. The percentage of cases with satisfactory and medium levels of pronunciation in group A was 86% (19/22) and 14% (3/22), respectively. The percentage of cases with satisfactory and medium levels of pronunciation in group B was 14% (3/21) and 86% (18/21), respectively ().
Table 3. Pronunciation of the cases in the two groups.
Time of removal of gastric tube and tracheal tube
Group A: No gastric tube was placed in any cases. Tracheal tube was removed within 10 d after surgery.
Group B: Tracheal tube was removed 2 weeks after surgery in seven cases, one month after surgery in nine cases, and 2 months after surgery in five cases.
Length of hospitalization
Group A: All cases were discharged about 10 d after surgery.
Group B: 16 cases were discharged 2 weeks after surgery, and five cases were discharged 3 weeks after surgery because of a moderate level of aspiration and/or pneumonia.
Follow-up
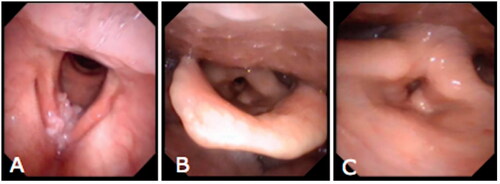
There was no recurrence and local/distant metastasis in any cases in either group A or group B during the follow-up of 12–48 months. Endoscopy showed that the mucosa of the larynx healed well in all cases. The shape of laryngeal cavity was roughly normal in group A (). CT scan of the larynx displayed that the effect of reconstruction of thyroid cartilage with titanium mesh was promising. The condition of the larynx in a case who underwent radiotherapy was satisfactory as well. No exposure of titanium mesh was detected.
Figure 3. The patient underwent radiotherapy after surgery. (A) Preoperative endoscopy of larynx shows the location of tumor in the right vocal fold, anterior commissure, and anterior 1/3 of the left vocal fold. (B) Endoscopy at 3 months after surgery shows that the mucosa of the larynx has been healed well. The shape of laryngeal cavity is roughly normal. (C) Endoscopy at 3 months after surgery shows an approximately normal activity of the left vocal fold.
Discussion
At present, there is no perfect treatment for LC patients with anterior commissure involvement, concerning both efficacy, and quality of life postoperatively. This may be due to the peculiarity of anterior commissure. The recurrence rate is relatively low because of the extended resection of anterior commissure and thyroid cartilage in open surgery, in which CHEP is a frequent therapeutic method. The advantage of CHEP includes wide indications, high rate of endotracheal intubation, and low recurrence rate of tracheal stenosis. However, aspiration and poor pronunciation are the common disadvantages. Some patients may suffer severe pneumonia because of long-term aspiration with tracheal tube. Thus, it is highly essential to preserve laryngeal function to the greatest extent in case of radical resection to shorten recovery time [Citation5].
We found that the deformation of thyroid cartilage and weakened support of the larynx after undergoing open surgery would inevitably lead to a series of adverse consequences. Therefore, the key to fabricate the larynx is to reconstruct the thyroid cartilage. Strength, plasticity, promising compression resistance, and biocompatibility are the most important characteristics for materials used to reconstruct the thyroid cartilage. Therefore, titanium has been widely used in orthopedics, plastic surgery, oral and maxillofacial surgery [Citation15,Citation16]. A previous study suggested that a titanium mesh could also be used to reconstruct the thyroid cartilage [Citation17]. However, the size, shape, and angle of the thyroid cartilage are different in different patients. It is highly complicated to ensure that a personalized titanium mesh is set accurately. We, in the present research, conducted excision of thyroid cartilage along the osteotomy line simulated computationally before surgery and under the guidance of a guide plate made by 3D printing, and then, fixed the titanium mesh with titanium nails in pin holes confirmed computationally before surgery, so as to reconstruct the thyroid cartilage accurately.
The results of this research revealed that the time of oral feeding in all the cases in group B who underwent CHEP was relatively delayed (10–12 d after surgery) with diverse levels of aspiration. A long-term swallowing practice was found essential before conducting oral feeding. However, in group A, only a mild level of aspiration was found when eating mash orally in 5 T3 cases who underwent resection of unilateral arytenoid cartilage. Aspiration disappeared after swallowing practice at 10 d after surgery. Moreover, aspiration was not detected in the remaining of the cases in group A.
A number of procedures in the modified CHEP may increase the risk and level of aspiration. Firstly, resection of thyroid cartilage leads to the loss of cartilage support and deformation of the larynx cavity. Second, arytenoid cartilage was dislocated due to the suture of mucosa margins aiming to close the wound after resection of primary laryngeal tumor. Third, the procedures may cause food to more likely fall into the throat and trachea because of changes in the positions of the larynx and oropharynx, and upward movement of residual larynx after undergoing the modified CHEP. The proposed surgical method used a personalized titanium mesh to reconstruct the thyroid cartilage and ensure the support of the larynx. In this way, reconstructed larynx, oropharynx, and hypopharynx did not shift to their original positions. Strap muscles were utilized to reconstruct a soft tissue defect of larynx to maintain the normal position and activity of the arytenoid cartilage. These improvements can significantly reduce the incidence of aspiration, relieve postoperative pain, and shorten the recovery time.
The quality of pronunciation mainly depends on the movement and resonance of vocal cords. When airflow passes through the moving arytenoid mucosa, arytenoid mucosa can produce a certain level of pronunciation [Citation18]. All the cases in this study underwent resection of a part of the vocal fold. However, the ability of pronunciation among cases in group A was better than that in cases in group B. First, suture of mucosal remnant in larynx would restrict the activity of arytenoid cartilage during the reconstruction of laryngeal function in the modified CHEP, which might affect the ability of pronunciation as well. Second, the laryngeal cavity became larger than normal and the amount of airflow passing through the arytenoid cartilage decreased after undergoing the modified CHEP. Using the proposed surgical method, we reserved most of the normal soft tissues during resection of the thyroid cartilage, and reconstructed the soft tissue with strap muscles. The original shape of glottis was maintained, and the strength of aryepiglottic fold and the closure of arytenoid mucosa were close to normal, which contributed to improve the quality of pronunciation.
Tracheotomy in the laryngeal surgery aims to prevent tracheal stenosis and dyspnea due to laryngeal mucosal edema after surgery, and it can be avoided when the larynx is normally reconstructed approximately. This justifies why there are significant advantages in the treatment of cases in group A in terms of the percentage of patients who received tracheotomy for prevention of pneumonia, high rate of endotracheal intubation, the length of hospitalization after surgery, and postoperative recovery time compared with those in group B. No recurrence and metastasis were observed in either group A or group B, because the modified CHEP and the proposed surgical method could both accomplish the extended resection of laryngeal tumor under direct vision.
Exposure of the titanium mesh is one of the risk factors after titanium implantation. The risk of exposure of titanium mesh tends to increase due to the movement of the thyroid cartilage during pronunciation and swallowing. A number of scholars assessed the feasibility and efficacy of laryngeal framework reconstruction using titanium mesh in patients with glottic cancer after frontolateral vertical partial laryngectomy, and found that titanium mesh could be a good alternative for reconstruction of the laryngeal framework [Citation17]. We, in the present research, found several challenges in the process of laryngeal framework reconstruction using titanium mesh. It is a time-consuming process to reshape the titanium mesh, and the edge of the titanium mesh is very sharp. Besides, accurate construction of the structure of larynx is an important drawback. These barriers may disrupt laryngotracheal reconstruction and affect the swallowing exercises and pronunciation. In this study, the personalized titanium mesh fabricated with 3D printing was very thin with a large number of small holes and the edge was obtuse, which appeared advantageous for reconstruction of the larynx and soft tissues. The risk of displacement and deformation of titanium mesh was reduced, which accordingly led to the reduction of the risk of exposure of titanium mesh.
In summary, the proposed surgical method possessed numerous advantages for patients with LC with anterior commissure involvement whose thyroid cartilage needs partial resection. It is therefore highly essential to further concentrate on application of digital modeling combined with 3D printing to assist the resection of laryngeal lesions and the reconstruction of residual larynx.
Disclosure statement
The authors declare that there are no conflicts of interest.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Zeitels SM. Glottic cancer: a metamorphosing disease. Ann Otol Rhinol Laryngol. 2016;125(6):452–456.
- Hakeem AH, Tubachi J, Pradhan SA. Significance of anterior commissure involvement in early glottic squamous cell carcinoma treated with trans-oral CO2 laser microsurgery. Laryngoscope. 2013;123(8):1912–1917.
- He F, Wang Y, Chen W, et al. Clinical research of early laryngeal carcinoma treated by carbon dioxide laser microsurgery. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2014;28(7):493–495.
- Huang S, Chen Y, Ye Q, et al. CO2 laser surgery for early glottic carcinoma. China Arch Oto Head Neck Surg. 2015;22(7):325–328.
- Bajaj Y, Uppal S, Sharma RK, et al. Evaluation of voice and quality of life after transoral endoscopic laser resection of early glottic carcinoma. J Laryngol Otol. 2011;125(7):706–713.
- Ning J, Zhu Z, Lin C, et al. Clinical research of early laryngeal carcinoma treated by carbon dioxide laser microsurgery. Cancer Res Clin. 2015;11:763–765.
- Wang XB, Pan XL, Lu YT, et al. A clinical study of the surgical treatment for early stage glottic carcinoma. J Oto Oph Shandong Univ. 2013;27(4):53–58.
- Shuang Y, Li C, Huang YW, et al. Comparison between radiofrequency co-ablation and CO2 laser for the treatment of early glottic carcinoma. J Audi Spee Path. 2015;23(4):372–376.
- Hong JC, Kruser TJ, Gondi V, et al. Risk of cerebrovascular events in elderly patients after radiation therapy versus surgery for early-stage glottic cancer. Radiat Oncol Biol Phys. 2013;87(2):290–296.
- Mantsopoulos K, Psychogios G, Koch M, et al. Comparison of different surgical approaches in T2 glottic cancer. Head Neck. 2012;34(1):73–77.
- Allegra E, Saita V, Azzolina A, et al. Impact of the anterior commissure involvement on the survival of early glottic cancer treated with cricohyoidoepiglottopexy: a retrospective study. Cancer Manag Res. 2018;10:5553–5558.
- Garozzo A, Allegra E, La Boria A, et al. Modified supracricoid laryngectomy. Otolaryngol Head Neck Surg. 2010;142(1):137–139.
- Tian H, Yu JJ, Zan L, et al. Curative effect evaluation between improved frontolateral partial laryngectomy and improved cricohyoidoepiglottopexy. Chin Oncol. 2013;23(7):535–539.
- Wu D, Yu JC, Yan HH, et al. Long-term outcome of laryngeal framework reconstruction using titanium mesh in glottic cancer after frontolateral vertica partial laryngectomy. J Clin Oto Head Neck Surg. 2017;31(7):552–555.
- Hashikawa K, Tahara S, Ishida H, et al. Simple reconstruction with titanium mesh and radial forearm flap after globe-sparing total maxillectomy: a 5-year follow-up study. Plast Reconstr Surg. 2006;117(3):963–967.
- Singh M, Ricci JA, Dunn IF, et al. Alloderm covering over titanium cranioplasty may minimize contour deformities in the frontal bone position. J Craniofac Surg. 2016;27(5):1292–1294.
- Liu XK, Zhang Q, Li Q, et al. Laryngeal framework reconstruction using titanium mesh in glottic cancer after frontolateral vertical partial laryngectomy. Laryngoscope. 2010;120(11):2197–2202.
- Yang HA, Guo X, Ma L, et al. Functional reconstruction of swallowing after supracricoid partial laryngectomy with anastomosis of cricoid cartilage, base of tougue and epiglottis. J China Med Univ. 2007;36(1):69–75.