Abstract
Background
Follow-up of cochlear implant effectiveness is mainly focused on 3 years postoperatively, and studies with more than 5 years of observation are rare, especially for local Chinese brands.
Objectives
Nurotron (Chinese domestic cochlear implant brand) CI recipients who participated in the clinical trial in 2009 were followed-up for 10 years prospectively, providing data to guide doctors and patients.
Material and Methods
From December 2009 to April 2010, 57 subjects underwent Nurotron Venus CI surgery at multiple-centers, and were continued to be followed up and assessed at 1, 2, 3, 4, 5, and 10 years after switch on.
Results
All recipients were successfully implanted with CIs with no difficulty in subsequent use with one reported case of re-implantation at 9 years after implantation. The aided hearing thresholds were significantly improved at one month after switch on (p < 0.0001) and remained stable afterwards for 10 years. Speech recognition scores were significantly higher than pre-operative results (p < 0.05) and continued to improve till 3 years after switch on. At 10 years post-operation, most subjects had improved QOL scores in most sub-items.
Conclusions and Significance
Nurotron Venus CI System provides long-term, stable results in hearing speech assistance capabilities and can improve the quality of life of CI recipients.
Chinese Abstract
背景
人工耳蜗效果的随访主要集中在术后 3 年;关于超过 5 年观察的研究很少, 尤其是针对中国本土品牌。
目的
对 2009 年参与临床试验的诺尔康(中国国产人工耳蜗品牌)CI 接受者进行 10 年前瞻性随访, 为指导医生和患者提供数据。
材料和方法
从2009 年 12 月至 2010 年 4 月, 57 名受试者在多中心接受了诺尔康维纳斯人工耳蜗植入手术, 并在开机后 1、2、3、4、5 和10 年持续接受随访和评估。
结果
所有接受者均成功植入 CI, 后续使用没有困难。报告了一例在植入后 9 年重新植入的病例。辅助听力阈值在开机后一个月内显著改善(p < 0.0001), 并在之后的10年内保持稳定。语音识别分数明显高于术前结果(p < 0.05), 并且在开机后3年内持续改善。术后第10年, 大多数受试者在大多数子项目中的生活质量得分都有所改善。
结论和意义
诺尔康维纳斯CI系统在听力言语辅助能力方面提供了长期、稳定的效果, 并可以改善CI接受者的生活质量。
Introduction
According to data from the seventh national census, China has a total population of 1.4 billion, which corresponds to a huge number of people with disabilities [Citation1]. Of the 85.02 million disabled people, there are approximately 27.8 million people with hearing disabilities. The Chinese government attaches great importance to the protection and development of persons with disabilities, and develops rehabilitation, education, and employment of persons with disabilities [Citation2]. However, this large group of persons with disabilities inevitably increases the social and economic burden. How to better integrate them into society has become an urgent problem that we need to solve [Citation2, Citation3].
Cochlear implantation is still the most effective intervention for patients with severe to profound sensorineural hearing loss to regain hearing [Citation4]. In 2009, Nurotron Biotechnology Co., Ltd. applied for the State Food and Drug Administration (SFDA) registration for its Nurotron Venus Cochlear Implant System [Citation5]. As an important step of registration, the PLA General Hospital and four hospitals jointly implanted the product for 60 patients with post-linguistic hearing loss and conducted a two-year evaluation in accordance with the clinical protocol. As a result, it was determined that the product complied with the use standard and could be used in clinical practice [Citation6].
Since then, several studies reported clinical outcomes of Nurotron cochlear implant system for hearing impaired patients with postlingual deafness. Li et al. [Citation7] followed 15 Nurotron CI adult recipients for 2 years and reported regular use of device. The aided hearing thresholds of all the recipients were within the speech spectrum. The average sentence and word recognition scores were 82.88 ± 21.40% and 56.67 ± 9.77%, respectively, which were comparable with another brand. Gao et al. [Citation6] reported 4 years follow-up outcomes of 60 adult patients who participated in the Nurotron clinical trial study. The average scores of open-set and closed-set speech tests improved respectively from scores of 0% and below 20% to scores above 80%. Liu et al. [Citation8] reviewed 3 and 6 months post-operative results of 13 postlingual Nurotron CI recipients. Results showed that CAP (categories of auditory performance) scores were significantly improved from 0.31 ± 0.48 preoperatively to 4.69 ± 1.03 and 6.23 ± 1.23, respectively at 3 months and 6 months post-activation. Word/phrase recognition scores were also significantly increased from 10.12 ± 0.31 preoperatively to 86.69 ± 8.34 at 6 months after switch-on.
In order to understand the overall experience and evaluate the long-term clinical effectiveness and safety outcomes of Nurotron cochlear implant, Nurotron CI recipients who participated in the clinical trial in 2009–2010 were followed-up and several aspects such as speech recognition, quality of life, tinnitus measurement were assessed at 10 years after switch-on.
Methods
Subjects
The study included 60 subjects with postlingual bilateral severe to profound sensorineural hearing loss who underwent unilateral Nurotron Venus CI surgery at multiple-centers from November 2009 to April 2010. Among them, 36 were males and 24 were females. At the time of surgery, the age ranged from 6 to 59 years old, with an average age of 26 ± 12 years. The duration of hearing deprivation ranged from 3 months to 15 years, with an average of 7 ± 5 years. There were 7 cases of large vestibular aqueduct syndrome (LVAS), others had no obvious inner ear malformations, 31 cases were ototoxic hearing loss, 5 cases were sudden hearing loss, 2 cases were deafness caused by meningitis, and 2 cases were noise-induced hearing loss. All recipients have normal mental and intellectual development, no other contraindications for cochlear implantation, and no systemic diseases. Thirty-three recipients had the experience of wearing hearing aids before the operation, and 5 had the experience of rehabilitation training.
Follow-up time
The test was first performed on the day the system was switched on, and then the recipients were followed up 2 months ± 1 week, 4 months ± 2 weeks, 6 months ± 2 weeks, 1 year ± 2 weeks, 2 years ± 2 weeks, 3 years ± 2 weeks, 4 years ± 2 weeks, 5 years ± 1 month and 10 years ± 3 months (some of the assessments were delayed due to COVID-19 pandemic) after the system was switched on.
Follow-up tasks
First of all, we evaluated the safety of the Nurotron Venus CI, including the assessment of the overall condition of the recipients after surgery, X-rays of the skull to check electrode position, changes in electrode impedance, peri- and post-operative complications, device wearing time and usage. Doctors who specialize in cochlear implants interviewed the patient or the patient’s family, reviewed imaging results, assessed the electrode impedance during programming, and document.
Subsequently, we evaluated the effectiveness of the recipients after implantation, which mainly included auditory ability tests and evaluation of open-set speech recognition. The HOPE test materials is the most commonly used in the Mandarin speech test, containing 25 monosyllable,10 sentences and 50 key words [Citation9, Citation10]. The quality-of-life (QOL) questionnaire (Nijmegen Cochlear Implant Questionnaire, NCIQ) was evaluated first time when switched on, and it was evaluated again at the ten-year follow-up. In the meantime, CAP (Categories of Auditory Performance) & SIR (Speech Intelligibility Rating) and telephone usage assessment were added in the ten-year follow-up [Citation11].
Statistical analysis
The data management and statistical analysis work of this study was performed by the Statistics Department of PLA General Hospital. Paired t-test was adopted for comparisons of normally distributed within-subject biometrics, and Wilcoxon Signed Rank test was adopted for comparisons of non-normally distributed within-subject biometrics. Data management was done in EPI DATA 3.0. All statistical tests were two-sided tests at 0.05 confidence level, performed by SPSS 22.
Results
Safety of Nurotron Venus CI System
During first year follow-up, three subjects among 60 subjects were excluded or withdrew from the study. One recipient was excluded as his hearing did not meet the criteria for cochlear implantation (chose to use hearing aids). Two recipients withdrew from the study due to their inability to comprehend the tasks required in the clinical trial because they were ethnic minorities and did not speak Mandarin. The actual number of successful follow-ups after 1, 2, 3, 4, 5, and 10 years were 57/52/45/40/33/42, respectively.
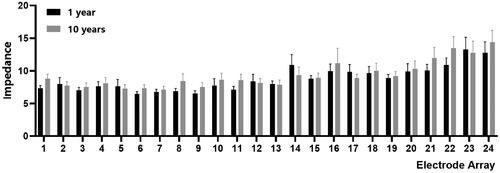
The CI recipients were in good postoperative general condition without related surgical complications. X-ray examination showed that the electrodes were located in the cochlea, and the system worked well after the switched on. The E1, E7, E13 and E19 electrode contacts were selected for representing the apical, middle and basal of the cochlea. Except for E13, the impedance increased at 10 years after operation compared with 1 year, and there was no statistically significant difference in the two impedance changes of all electrodes (). At the same time, the recipient’s CI usage was tracked during the follow-up process. The recipients wear CIs for more than 8 h a day on average, and no recipients have found any difficulty using the implants. Up to 10 years follow-up, there was 1 reported case of re-implantation due to implant failure (refer to session ‘special cases’ for more details). No other severe adverse event was reported.
Effectiveness of Nurotron Venus CI System
Aided hearing thresholds
The aided mean hearing thresholds at four frequencies (at 0.5, 1, 2 and 4 kHz) were 108.3 dBHL prior to surgery, 46.8 dBHL at 1 month, 43.6 dBHL at 2 months, 43.1 dBHL at 4 months, 41.5 dB HL at 6 months, 39.5 dBHL at 1 year, 41.9 dBHL at 2 years, 41.2 dBHL at 3 years, 42.3 dBHL at 4 years, 41.4 dBHL at 5 years, and 39.7 dBHL at 10 years after switch on.
The results of analysis of variance showed that the hearing threshold in the sound field was significantly improved at one month after switch on (p < 0.0001). The average hearing threshold was stable after 1 month switch on (p > 0.05).
Open-set speech recognition test
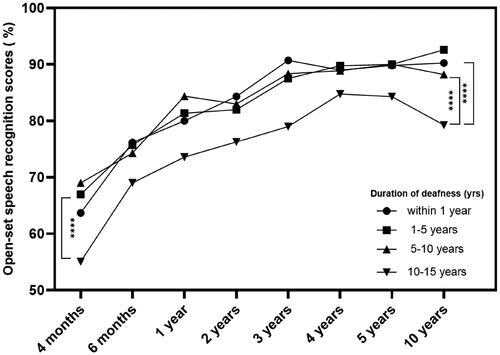
Before the surgery, the average HOPE test score of 57 subjects was 0%. The average HOPE sentence recognition scores at 2 months, 4 months, 6 months 1, 2, 3, 4, 5, and 10 years were 36%, 65%, 75%, 84%, 83%, 89%, 91%, 92%, and 90%, respectively, while the average scores of disyllabic words were 32%, 54%, 67%, 76%, 80%, 84%, 86%, 86% and 86%. Wilcoxon signed-rank test showed that post-operation average speech recognition scores at each time-point were significantly higher than pre-operation results (p < 0.05, and ). Furthermore, in the evaluation ten years after the switch on, the average score of CAP&SIR were 5.90 ± 1.20 and 4.35 ± 0.76, respectively.
Figure 2. Speech recognition scores of Nurotron Venus CI users from pre-operation to 10 years after switch on.
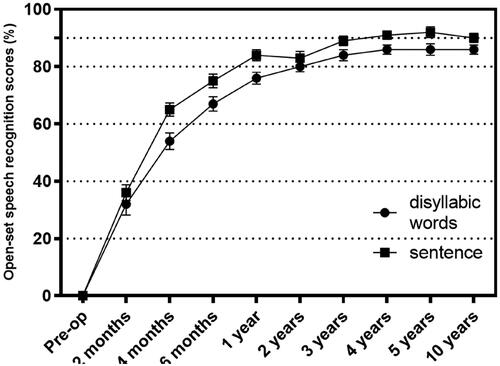
Table 1. HOPE sentence and disyllabic word recognition scores of Nurotron Venus CI users from pre-operation to 10 years after switch on.
At the meantime, we divided the recipients into four groups of severe to profound deafness duration, which were within 1 year, 1–5 years, 5–10 years, and 10–15 years according to the length of hearing deprivation, and calculated the average scores of HOPE in each group at each time point until ten years after surgery. It can be seen from the results () that there was no significant difference in the HOPE score of recipients with preoperative severe to profound deafness within 10 years. When pre-operative deafness duration reaches more than 10 years, the HOPE scores were significantly lower than other groups at all assessment time points (p < 0.0001).
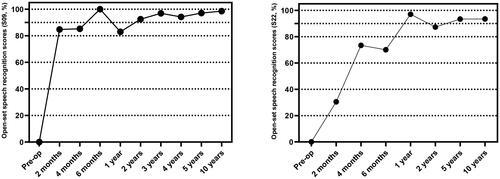
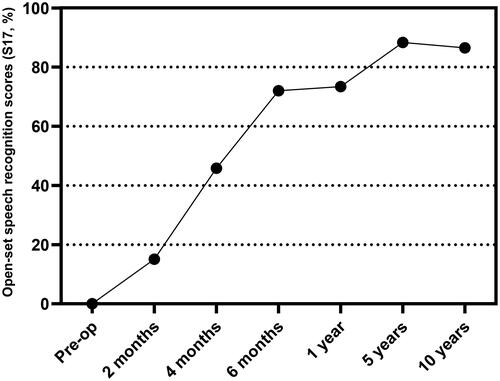
Special cases
S17 (), a male recipient with ototoxic hearing loss, had 13 years of severe to profound deafness before surgery, used hearing aids for 12 years, and had the surgery on the left side for the first time at the age of 36. All electrodes were successfully inserted into the cochlea during the first surgery. The average scores of sentences and disyllabic words in the HOPE test increased gradually after the switch on, reaching 88.33% at 5 years after surgery. At 9 years and 7 months after implantation, the recipient underwent CI removal and reimplantation due to implant failure. The HOPE test was evaluated again ten years after the first implantation, and the average score was similar to that in the fifth year, at 86.5%.
Figure 4. Open-set speech recognition scores of Nurotron Venus CI user (S17) from pre-operation to 10 years after switch on.
S09 and S22 () are two meningitis-induced hearing loss patients. The preoperative period of severe to profound deafness was 3 years and 10 years, respectively. S09 showed a good HOPE test score in the second month after switch on, reaching the score of 84.77%, and became stabilized at above 90% after 2 years from switch on. The HOPE test score of S22 was 30.50% at 2 months after switch on, 73.40% at 4 months and 70.1% at 6 months, which increased and stabilized at around 90% at 1 year.
Quality of life (QOL) surveys
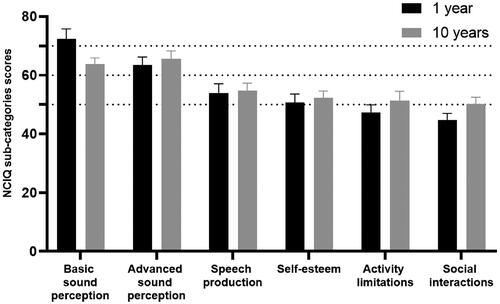
NCIQ survey was used to assess quality of life of CI users. The scores of basic sound perception, advanced sound perception, speech production, self-esteem, activity limitations, and social interactions in NCIQ at 1 year CI switch on were 72.4, 63.4, 54, 50.7, 47.3, 44.7, respectively, with an average score of 55.42. Re-evaluating the NCIQ scale at the 10 years after switch on showed that the scores of the above-mentioned dimensions were 63.7, 65.6, 54.7, 52.3, 51.3, and 50.2, with a total score of 56.3. The scores of NCIQ sub-categories and total average scores were similar between 1 and 10 years after switch-on. No significant differences were found between the total average NCIQ scores of 1-year post-implantation and 10-year post-implantation (p > 0.05, ).
Phone usage
There were 22 subjects (38.59%) who can use the telephone with the familiar/unfamiliar talkers. Among them, 14 people can communicate with familiar people on the phone, and 8 people can communicate with unfamiliar people or strangers on the phone.
Discussion
Hearing loss brings a huge burden to society and families. More than half of the sensorineural hearing loss is caused by genetic factors [Citation12]. In the early years, due to insufficient awareness and publicity, most deaf people married deaf people, resulting in ‘familial deafness’. Moreover, due to the low tolerance and understanding of society, the chance of getting a job for deaf people is much lower than that of people with normal hearing. Therefore, families of deaf people are often in financial difficulties.
Even though cochlear implantation is still the most effective way to treat sensorineural hearing loss, very few regions can medically reimburse the cost of cochlear implant systems via government medical insurance in China. If no funding of national project is available, it would be difficult for most post-lingual adults to afford the high equipment costs. Nurotron Venus CI System is favored by more and more Chinese families because of their huge price advantage with similar clinical effectiveness when comparing with other products of the same type [Citation5, Citation13]. Since Nurotron Venus CI System was approved by China Food and Drug Administration (CFDA, currently named National Medical Products Administration NMPA) for clinical treatment in 2011, it has helped thousands of hearing-impaired patients regain their hearing. This time, the 10-year in-depth follow-up of Nurotron Venus CI System has once again confirmed its safety and effectiveness.
In our follow-up data, we found that all 60 post-lingual hearing loss recipients had successfully implanted Nurotron Venus CI System. As for the implant itself, the impedance value is stable at 1 and 10 years after the surgery, indicating that the performance of the implant is stable. The results of the open-set speech recognition test showed significantly improvement at 2 months after switch on when comparing with the preoperative results. With the prolongation of the CI wearing time, the scores of CI users continued to increase until around 3rd years after implantation and maintained a stable level at around 88%, since then the differences between individuals were reduced overtime. Moreover, the results of statistical analysis showed that the average sentence and disyllabic words scores were not significantly different at 4, 5 and 10 years after surgery, which is similar to previous studies of other brands of CIs [Citation14–17].
Looking back on the special case, there was 1 re-implantation recipient within 9 years after the surgery, the incidence was 1.6%, which is similar to previous reports [Citation18, Citation19]. In addition, two meningitis recipients were observed and found to have different rate of improvement yet reaching similar performance after a year of switch on. S09 showed good hearing ability within a short period of time after surgery, while S22 only reached an open-set speech recognition rate of more than 90% after 1 year.
The quality of life of Nurotron Venus CI recipients was stable with slight improvement after implantation throughout 10 years. Comparing results of 1 year with 10 years, the NCIQ total score and advanced sound perception, speech production, self-esteem, activity limitations, and social interactions were similar at 1 and 10 years after surgery, which shows that quality of life can be maintained well in long term.
Conclusion
Continuous and in-depth observations for 10 years after surgery have confirmed that Nurotron Venus CIs are safe and effective for long-term use. CI users who are post-lingually deafened usually have higher expectations for the outcomes because they used to hear natural sounds before deafness. After implantation, the hearing, speech abilities, and quality of life of patients with post-lingual hearing loss have greatly improved. In all, comparing with similar products of other CI brands, the recipients of Nurotron Venus CIs receive similar benefits.
Authors’ contributions
Jianan Li, Lusen Shi, and Haiqiao Du contributed equally to this manuscript’s conception, research, and writing in this manuscript.
Disclosure statement
The authors have no conflicts of interest to disclose.
Data availability statement
Data generated or analyzed during this study are available from the corresponding author on request.
Additional information
Funding
References
- China, N.B.o.S.o. Communiqué of the Seventh National Population Census (No. 2). 2021. Available from: http://www.stats.gov.cn/english/PressRelease/202105/t20210510_1817187.html
- Li J, Li LSW. Development of rehabilitation in China. Phys Med Rehabil Clin N Am. 2019;30(4):769–773. doi: 10.1016/j.pmr.2019.07.010.
- Li JN, Chen S, Zhai L, et al. The advances in hearing rehabilitation and cochlear implants in China. Ear Hear. 2017;38(6):647–652. doi: 10.1097/AUD.0000000000000441.
- Zeng F-G. Celebrating the one millionth cochlear implant. JASA Express Lett. 2022;2(7):077201. doi: 10.1121/10.0012825.
- Rebscher S, Zhou DD, Zeng FG. Development and clinical introduction of the Nurotron cochlear implant electrode array. J Int Adv Otol. 2018;14(3):392–400. doi: 10.5152/iao.2018.6285.
- Gao N, Xu XD, Chi FL, et al. Objective and subjective evaluations of the Nurotron Venus cochlear implant system via animal experiments and clinical trials. Acta Otolaryngol. 2016;136(1):68–77. doi: 10.3109/00016489.2015.1086022.
- Li J, Ji F, Chen W, et al. Analysis of the performance of post-lingually deafened patients with Nurotron((R)) Venus cochlear implants. Acta Otolaryngol. 2014;134(6):609–614. doi: 10.3109/00016489.2014.894250.
- Liu M, Ou Yang YY, Chen XH, et al. Study of auditory rehabilitation performance of postlingual cochlear implantees with Nurotron cochlear. China Med Dev Inf. 2016;22(03):15–17+34. doi: 10.15971/j.cnki.cmdi.2016.03.003.
- Ji F, Xi X. The development of mandarin-Chinese phonetically balanced monosyllable words test list. J Otol. 2007;5:417–426.
- Ji F, Chen AT, Zhao Y, et al. Development of a script of phonemically balanced monosyllable lists of Mandarin-Chinese. J Oto. 2010;5:8–19. doi: 10.13489/j.cnki.11-4883/r.2010.01.003.
- Zhou H, Chen Z, Shi H, et al. Categories of auditory performance and speech intelligibility ratings of early-implanted children without speech training. PLoS One. 2013;8(1):e53852. doi: 10.1371/journal.pone.0053852.
- Yang T, Guo L, Wang L, et al. Diagnosis, intervention, and prevention of genetic hearing loss. Adv Exp Med Biol. 2019;1130:73–92. doi: 10.1007/978-981-13-6123-4_5.
- Zeng FG, Rebscher SJ, Fu QJ, et al. Development and evaluation of the Nurotron 26-electrode cochlear implant system. Hear Res. 2015;322:188–199. doi: 10.1016/j.heares.2014.09.013.
- Naples JG, Ruckenstein MJ. Cochlear implant. Otolaryngol Clin North Am. 2020;53(1):87–102. doi: 10.1016/j.otc.2019.09.004.
- Dhanasingh A, Jolly C. An overview of cochlear implant electrode array designs. Hear Res. 2017;356:93–103. doi: 10.1016/j.heares.2017.10.005.
- Canfarotta MW, Dillon MT, Buchman CA, et al. Long-term influence of electrode array length on speech recognition in cochlear implant users. Laryngoscope. 2021;131(4):892–897. doi: 10.1002/lary.28949.
- Balkany T, Hodges A, Menapace C, et al. Nucleus Freedom North American clinical trial. Otolaryngol Head Neck Surg. 2007;136(5):757–762. doi: 10.1016/j.otohns.2007.01.006.
- Chen J, Chen B, Shi Y, et al. A retrospective review of cochlear implant revision surgery: a 24-year experience in China. Eur Arch Otorhinolaryngol. 2022;279(3):1211–1220. doi: 10.1007/s00405-021-06745-1.
- Layfield E, Hwa TP, Naples J, et al. Failure and revision surgery after cochlear implantation in the adult population: a 10-year single-institution retrospective and systematic review of the literature. Otol Neurotol. 2021;42(3):408–413. doi: 10.1097/MAO.0000000000002940.