Abstract
A growing majority of people living in Residential Care Facilities (RCFs) for older people have dementia. Yet the implementation of evidence-based Dementia Design Principles (DDPs), known to reduce symptoms and improve wellbeing, remains limited. This paper reports on the development and application of Plan-EAT, a floorplan-based method of assessing dementia design quality in RCFs. Through the analysis of 34 published architectural exemplars, the method identifies strengths and weaknesses in the layouts of residential care buildings, across 39 assessment criteria organized under 9 DDPs. The paper concludes that the Plan-EAT could benefit architectural practice by providing an evidence-based means of assessing layout planning quality, in both existing cases and emerging RCF design proposals. The findings also highlight the need for care, where reliance is placed on published case studies, to inform the design of dementia supportive environments.
Introduction
An increasing majority of people living in Residential Care Facilities (RCFs) have a diagnosis of dementia (AIHW Citation2011, Citation2012; Prince et al. Citation2014), whilst the average level of cognitive capacity amongst residents has been declining (Matthews et al. Citation2013). With both trends expected to continue, the residential care sector is facing a growing need for RCFs that support rapidly increasing numbers of residents with increasingly severe levels of cognitive impairment (ACFA Citation2016; Wittenberg et al. Citation2020).
Past research demonstrates that the design of the physical environment is an influential element in supporting independence and wellbeing amongst people with dementia (Marquardt, Bueter, and Motzek Citation2014; Fleming et al., Citation2016; Nordin et al. Citation2017). Furthermore, several researchers have concluded that only minor gaps now remain in our knowledge about the design of RCFs for people with dementia (Marquardt, Bueter, and Motzek Citation2014; Bowes and Dawson Citation2019). However, despite the well-developed evidence-base, the recorded implementation of this within dementia design in completed RCFs has been limited and sub-optimal (Smith et al. Citation2012; Nordin et al. Citation2017; Hadjri, Faith, and McManus Citation2012), raising wide-ranging questions around causality, ranging from designer awareness through to matters of national policy, leading to speculation about potential causes, such as the need for education for architects (Dawson and Palmer Citation2020), lack of regulation (Castell Citation2008), or continued exclusion of people with dementia from the design process (Hendriks and Wilkinson Citation2020).
This paper investigates concerns about the quality, reliability, and usefulness of the three main sources of published information used by architects to gain knowledge about dementia design: Dementia Design Principles (DDPs), environmental assessment instruments, and published case studies. The first of these, DDPs (Fleming, Forbes, and Bennett Citation2003; Van Hoof et al. Citation2010) are intended to provide a loosely structured means of supporting design decision making for dementia. The second, environmental assessment instruments, (Sloane and Mathew Citation1990; Weisman et al. Citation1996; Parker et al. Citation2004; Cunningham et al. Citation2008; Fleming Citation2011) support the systematic, evidence-based evaluation of how likely an environment is to support the needs of occupants with dementia. The last, published case studies (Cohen and Day Citation1993; Judd, Marshall, and Phippen Citation1998; Utton Citation2007; Anderzhon et al. Citation2012; Feddersen and Lüdtke Citation2017; Palmer, Wallace, and Hutchinson Citation2021) document and discuss existing environments where various design challenges are deemed to have been resolved in a successful or innovative manner. Whilst all three of these sources are relevant to the present research this paper focusses on the latter two: environmental assessment instruments and case studies.
Several environmental assessment instruments for dementia design are available, though all focus on post occupancy evaluation (Sloane and Mathew Citation1990; Weisman et al. Citation1996; Parker et al. Citation2004; Cunningham et al. Citation2008; Fleming Citation2011). Despite this, recent research has identified that as much as 60% of the scoring in formal dementia design assessment tools can be determined at the earliest stages of design, with most of this through layout planning (Quirke Citation2019; Quirke et al. Citation2021). The present paper describes and demonstrates Plan-EAT, the first known tool to be identified as suitable for floorplan-based assessment of RCFs. The Plan-EAT method comprises a modified subset of questions derived from Fleming’s (Citation2011) Environmental Audit Tool (EAT) and is intended to be useable at any stage in the architectural design process provided floor plan drawings are available.
The architectural case study, which is frequently centred on the published plans of completed buildings, is one of the most effective and ubiquitous means by which architects develop and exchange new knowledge (Robinson Citation1990; Wang and Groat Citation2002). Although several collections of case studies in architectural design for RCFs have been published (Cohen and Day Citation1993; Judd, Marshall, and Phippen Citation1998; Utton Citation2007; Anderzhon et al. Citation2012; Feddersen and Lüdtke Citation2017; Palmer, Wallace, and Hutchinson Citation2021), to date these have not been critically assessed against the established dementia design evidence base. Given the significance of the architectural case study for the design of RCFs, Plan-EAT is used in the present paper to undertake a detailed, critical, assessment of the dementia design properties in the layout planning of 34 published exemplar cases.
This paper commences with a background to past research assessing the dementia design properties of RCFs. Thereafter the method employed in this paper, including its development, is introduced, and the results are presented. A discussion of the results centres on four ‘high’ and two ‘low’ scoring cases – relative to established DDPs – and patterns in the frequency of different DDPs. The paper concludes with a commentary on the implications of these findings.
Background
Past studies of design quality in RCFs have tended to conclude that there is significant room for improvement within the broad stock of existing RCFs (Smith et al. Citation2012; Nordin et al. Citation2017; Hadjri, Faith, and McManus Citation2012). The largest of these studies, a systematic design assessment of 56 Australian RCFs by Smith et al. (Citation2012) using the EAT (Fleming Citation2011) returned an average dementia design quality score of only 57.3%. The properties of RCF plans have also been examined, with sometimes contradictory results. As an example, Elmståhl, Annerstedt, and Åhlund (Citation1997) concluded that an L-Shaped configuration of circulation provided the best psychiatric outcomes for residents whilst ‘I’ shaped corridors provided the worst outcomes. Contradicting this, Marquardt and Schmieg (Citation2009) concluded that straight corridor configurations are most supportive of people with dementia, due to the way they assist orientation and wayfinding.
Further layout-based studies have tended to focus on spatial and normative cognitive properties, often using computational methods like Space Syntax to measure and compare levels of visual and physical accessibility or wayfinding (Peatross Citation1997; Hanson and Zako Citation2005; Lee, Ostwald, and Lee Citation2017; Lee, Ostwald, and Yu Citation2017). Such studies, while potentially useful for understanding the operations and potential impacts of these environments on staff and cognitively intact occupants, do not typically measure or assess quality in terms of DDPs. Only a few of these researchers have linked either their methods or outcomes to the established evidence base for dementia-specific design. For example, Hanson and Zako (Citation2005) used Space Syntax in conjunction with the Sheffield Care Environment Assessment Matrix (SCEAM) (Parker et al. Citation2004) to examine the planning characteristics required for people with dementia in RCF layouts, but their conclusions highlighted a lack of criteria within the SCEAM relating to layout configuration.
As these examples show, there is a knowledge gap caused by the lack of formal instruments for assessment of dementia-specific design quality in building layouts. They also identify a gap in the reliability of published case studies as architectural precedents in the design of dementia-appropriate environments. Both gaps are addressed in the present paper.
Research design, methodology and approach
For this paper, published examples of 28 facilities comprising 34 distinct unit layout types for the residential care of older people were collected from two major sources of case studies of RCFs (references withheld to ensure anonymity of cases). While additional or more recent case studies could have been sourced, the fact that these facilities have been identified by experts as good examples makes them a significant sample for review (see Table ). The facilities, comprising a total of 94 units accommodating up to 1353 residents, include examples from Asia, Australia, Europe, and North America. The unit sizes range from 6 to 76 resident bed spaces, with 18 residents on average, and a median of 15.
Table 1. Plan-EAT summary structure.
Table 2. Plan-EAT scores by dementia design principle.
Development of the Plan-EAT method
The Plan-EAT method is based on a subset of queries from the EAT (Fleming Citation2011). It is developed from previous research (Quirke et al. Citation2021) that mapped three established instruments: the EAT (Fleming Citation2011), the Dementia Design Audit Tool (Cunningham et al. Citation2008), and the Therapeutic Environment Screening Survey for Nursing Homes (Sloane et al., Citation1990); against key phases of decision-making in architectural design process and document type(s) associated with them (floor plans, specifications, etc). That research concluded that the EAT was amongst the most reliable of eight well-established tools, and the best suited to being re-purposed for use in assessing the floor plan layouts of RCFs. Thus, a subset of 39 of Fleming’s 72 original queries were adapted for the assessment of RCF floor plan drawings – thereby forming the Plan-EAT.
In a practical sense, Plan-EAT is a checklist, against which the properties of architectural plans can be reviewed or measured by expert assessors. It can operate in either a manual or software-based environment. Plan-EAT assessments result in a percentage-based overall score for dementia design quality. It also provides sub-scores under nine out of ten of Fleming’s established DDPs (Fleming, Forbes, and Bennett Citation2003; Fleming Citation2011): DDP#1 Safety, DDP#2 Size and Scale, DDP#3 Visual Access, DDP#4 Stimulus Reduction, DDP#5 Useful Stimuli, DDP#6 Movement and Engagement, DDP#8 Privacy and Social Interaction, DDP#9 Community Links, and DDP#10 Domestic Activity. Only Fleming’s DDP#7 Familiarity is excluded, as none of the assessment criteria under this DDP are directly observable or measurable from architectural plan drawings. The full set of Plan-EAT queries and their score values are shown in Appendix 1.
The number and scoring of Plan-EAT criteria varies by DDP (see Table ). For example, the simplest DDP, Size and Scale, contains only one query (Q) item:
Q2.01 How many people live in the unit?
By contrast, DDP#3 Visual Access contains ten assessment criteria. These are more sensitive to differences in spatial configuration, and hence are more directly measurable properties of floor plans. Examples include:
Q3.03 What proportion of confused residents can see the dining room as soon as they leave their bedroom?
Q3.04: Can the exit to the garden be seen from the lounge room?
Q3.09: Can a toilet be seen from the dining room?
Another variation occurs under DDP#4 Stimulus Reduction, which is comprised of queries related to negative or unhelpful features. Scores under this DDP are inverted, such that answers in the negative are required for points to be awarded in the positive. Query item Q4.05 is one example:
Q4.05 Are deliveries of food, linen etc. taken across public areas such as the lounge or dining room?
Although one DDP (DDP#7) is absent from the Plan-EAT, and the number of queries per individual DDP (see Table ) differs from the EAT (Fleming Citation2011), Fleming’s approach to score calculation is retained. Specifically, the points-value of individual queries – which vary from 1 to 4 – are retained. DDP scores are calculated by converting points achieved vs. the maximum available, into a percentage. Subsequently, an overall Plan-EAT score is calculated as an average of all DDP sub-scores (Table ) within which all DDPs maintain equal weighting to each other. With assessment item weighting varying significantly between existing audit tools (Quirke et al. Citation2021), Fleming’s established scoring schema is both the only evidence-based approach currently available, and an appropriate precursor to users potentially using the complete EAT in subsequent post occupancy evaluations.
Application of the Plan-EAT to published examples
The layout of each case was assessed against the full suite of Plan-EAT queries. For comparative purposes, average scores for the full set of case study layouts under each DDP were calculated in order to establish a benchmark profile, which is helpful for context in the interpretation of assessment outcomes. However, it is important to note that this benchmark may be less relevant as a reference for other cases.
Scope and limitations
A general limitation of the Plan-EAT comes from its focus on floorplans. Like any method which focusses on plans, it cannot consider the full spectrum of architectural properties that have been established as influencing the wellbeing of people living with dementia. Furthermore, while Plan-EAT has not yet been validated through extensive application, it demonstrates that indicators of dementia design quality can be usefully generated from critical review of architectural plans, and that this in turn can provide valuable insights for designers.
A practical limitation is that the method relies on the accuracy and completeness of information in the plans used for analysis. For the present paper, this limitation affected the assessment of some garden spaces, where floorplans contained insufficient landscape information. The absence of such information has the potential to undermine the veracity of assessment outcomes. In addition, the retention of the original wording from Fleming et al.’s EAT queries means that some assessment items include reference to features not visible in a floor plan. For example Q5.05 asks ‘Is the kitchen either looked into from the lounge or dining room or clearly marked with a sign or symbol?’ This also means that the Plan-EAT might return a slightly lower score for a given query compared to the application of EAT in a post occupancy evaluation of the same plan.
Although this paper is intended to inform and improve design of RCFs, the use of Plan-EAT and its outcomes are not meant to artificially provide simplistic answers to designers. Rather it is a tool that seeks to provide more nuanced information and basic benchmarking to assist designers, as part of a competent, widely informed, and collaborative design process, to create environments that optimize the overall wellbeing of people with dementia.
Results and discussion
The results of the Plan-EAT assessment of the 34 published examples returned a mean overall score of 68.4% (see Table ) which initially suggests on average, substantial room for improvement across the cases. However, the median score of 74.0% and 75th percentile score of 77.6% indicate that the cases cluster towards higher scoring layout types. In other words, the average score values are skewed downwards by a small number of exceptionally low scoring layouts.
The results identified several high scoring cases (Table ) likely to support the wellbeing of people with dementia, suggesting that these layouts are more reliable as precedents of design for dementia. Conversely, the results returned five cases with an average score of less than 50%. Such low scoring cases are less likely to provide appropriate support for needs of people with dementia and are therefore less reliable as precedents without first being subject to significant layout changes.
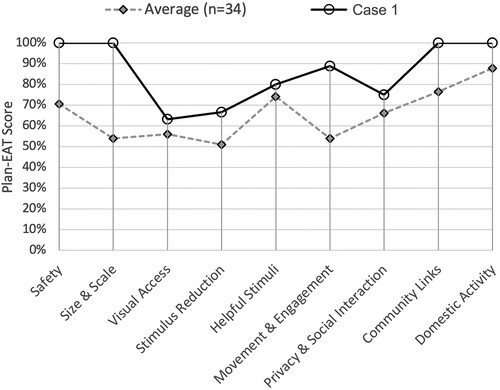
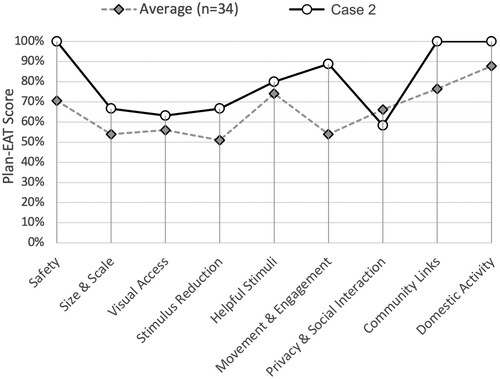
The results returned a wide array of scores under the nine individual DDPs. Some, including DDP#5 Useful Stimuli (Avg. 81.1%), DDP#9 Community Links (Avg. 84.0%), and DDP#10 Domestic Activity (Avg. 91.1%) returned very high scores on average. However, others including DDP#3 Visual Access (Avg. 55.7%), DDP#4 Stimulus Reduction (Avg. 48.9%), and DDP#6 Movement and Engagement (Avg. 55.8%) indicated significant average room for improvement across at least half of the cases. Meanwhile, five of the nine individual DDPs (#1 Safety, #2 Size and Scale, #5 Useful Stimuli, #9 Community Links, and #10 Domestic Activity) returned median scores that were substantially higher than the returned average – indicating that average scores for these DDPs are skewed downwards by a small number of layouts scoring poorly on these specific DDPs.
Upon a closer look at the results from individual queries, there are several areas where compliance with the Plan-EAT tended to be very high. For example, all layouts provide residents with constant and easy access to both a lounge and a dining room (Q10.07 and Q10.08). 30 of the 34 layout types allowed residents to see from the lounge room into the dining room (Q3.05, Q5.01) and vice-versa (Q5.02). Only two layouts prevented the staff from easily seeing into the lounge room, from the locations where they typically spend most of their time (Q3.10). Meanwhile, all but five layout types provided the staff with at least some degree of visual access for unobtrusive supervision of outdoor space (Q1.13) – though many could be improved. These and other high scoring items are useful for identifying the layout types that are likely to be more successful. Identifying areas where there is room for improvement, however, is potentially more useful and will have the greatest positive impact.
The four following criteria are examples of items with the lowest rates of compliance with the Plan-EAT. These provide an obvious starting point for improving the designs of many cases in the set. As an example, only 4 of the 34 layout types provide a toilet that is easily available from the outdoor area (Q.6.1 g). Similarly, only 4 of the 34 layout types prevent the residents from easily seeing the front entry door to the unit (Q.4.07). There is a variable, but generally low, provision of visibility from the lounge room to resident’s personal bedroom door (Q3.01) and there is also variable, but mostly only partial, provision of opportunities for residents to eat alone (without needing to retreat to their bedroom) (Q8.05). Such weaknesses, relating to visibility between spaces, could potentially be addressed with careful approaches to layout planning. However, others relating to the provision of alternative dining spaces (e.g. Q9.01), may be more difficult to achieve, and especially when other constraints, such as the cost of additional floor area, are considered.
To better understand the implications of the scores and the potential use of these case studies, four of the higher scoring layouts and two of the lower scoring ones are discussed hereafter. It is, however, important to understand several factors before considering the merits or applicability of these cases. First, older designs tend to score relatively poorly in Plan-EAT, simply because they predate most of the evidence contained in DDPs. For example, the two lowest scoring layouts analysed for the present paper were designed in the 1970s and 1980s. Second, some DDPs and queries in Plan-EAT emphasize the importance of smaller facilities, yet, in certain countries national care policies, and economic viability, drive larger facilities, sometimes with better staffing levels per resident. Third, architectural design is often constrained by complex site conditions, which may limit access to gardens or complicate wayfinding. Fourth, as this study focusses on layout planning it does not account for the role of some other aspects of RCF design, such as finishes, fixtures, and furniture, which can play a role in dementia design quality. All these factors shape the scores for the 34 cases in the paper, and thus the results must be interpreted with some care. The cases are named by their overall Plan-EAT rank score order.
Cases no. 1 & 2
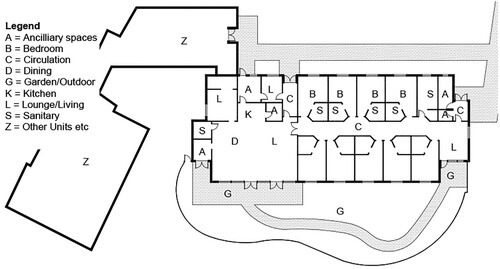
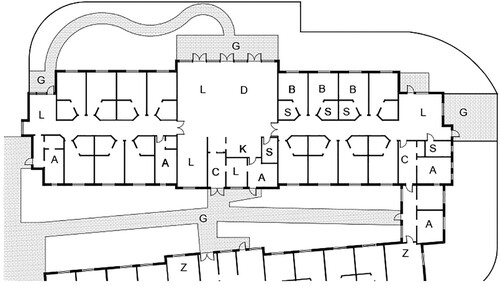
Both top-performing layout types were from the same facility. The development comprises of a single instance of a nine-resident, ‘special care unit’ (SCU) layout (Case 1, Figures and ) scoring 86.0%, and five instances of a 15-bed general layout type (Case 2, Figures and ) scoring 80.4%. The six distinct households are separated by gardens, but physically connected to other units via staff-only service areas.
Positive features of both layouts include constant and easy access to communal lounge and dining spaces (Q10.07, Q10.08), as well as providing resident access to a kitchen. Both accommodate the residents hosting and having meals with their families, whilst being removed from the main communal spaces (Q9.01). Both provide indoor and outdoor walking paths which avoid dead ends and take residents past a range of things to do and see (Qs. 6.1a, 6.1b, 6.2a, 6.2b). Both the SCU and general layouts provide consistent unobtrusive means for the staff to survey the spaces used by residents (Q3.10, Q6.1d, and others). Other notable strengths of the two layout types are the provision of several secondary communal spaces which allow for a range of different activities to occur simultaneously. For example, allowing dining to occur in several small groups (Q8.03), rather than in a single large group, or through the ability to support various small group activities without rearranging the furniture (Q8.03).
The relatively small number of weaknesses in both cases include that, only around half of residents can see the lounge and dining rooms as soon as they leave their bedroom (Q3.02 and Q3.03), and only around quarter would be able to see their own bedroom door from the communal lounge (Q3.01). Conversely the Plan-EAT, following standard DDPs, deems the easy visibility to the front entry from the communal spaces in both layout types to be an undesirable feature (Q4.07).
The main Plan-EAT score variations between the two layouts are due to differences in the number of residents living together (9 residents vs. 15) (Q2.01) and variations in options provided for dining in smaller groups (Q8.4 and Q8.5). See Appendix 1 for more detailed Plan-EAT assessment results.
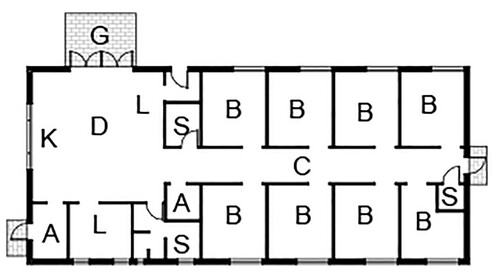
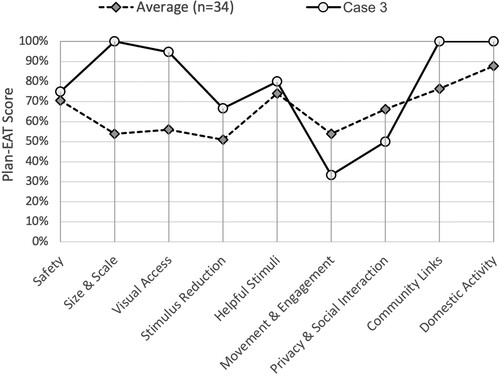
Case 3
The third highest scoring layout is a small, single-level detached unit, consisting of a simple layout (Figure ). It contains only eight single resident bedrooms (Q2.01), located off a short, but wide, corridor connecting one of three entry points to the building with an open-plan communal space. This communal space acts as the main kitchen, dining, and living spaces for the residents, containing a raised tatami mat seating area for socializing and a single large table for group activities. Access is provided from this main space to toilet and bathing areas, a formal tatami room, and a terraced deck.
Along with a high overall Plan-EAT score (77.7%), Case 3 performs well across most DDPs (Figure ), including DDP#2 Size and Scale (100% vs. 67% Avg.) and DDP#4 Stimulus Reduction (67% vs. 49% Avg.) where it outperformed the average score by over 30%. The weakest scores for this layout were under DDP#6 Movement and Engagement (33% vs. 56% Avg.) and #DDP 8 Privacy and Community (50% vs. 60% Avg.). However, the reduced score under DDP#6 was partly due to the absence of detailed information about the garden within available drawings. The slightly low score under DDP#8 Privacy and Social Interaction, is partly a consequence of the exceptionally small floor area of the unit, where the space provision per resident (34.9 m2) is less than two-thirds of the average across this study (57.5 m2). This makes it more difficult to accommodate multiple smaller dining groups (Q8.04) or lone dining (Q8.05) within communal spaces.
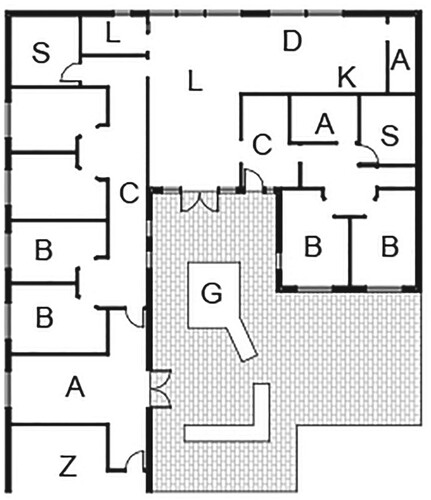
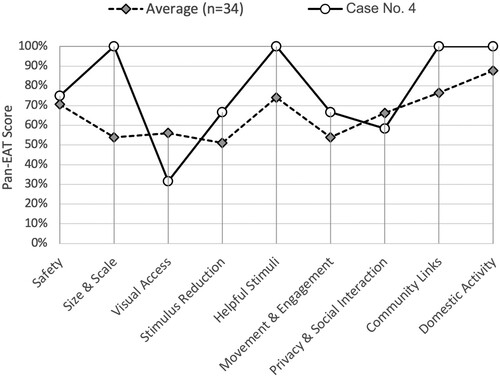
Case 4
The fourth highest scoring unit layout of Case 4 is one of 23 households in a facility designed as a self-contained suburban village centre, with its own supermarket, café, cinema, and other uses. Planned as a series of interlinking, landscaped courtyards, the residents can move independently around the development, free of safety concerns such as vehicular traffic. Only one layout was available in sufficient detail for examination in the present study and it is likely that the facility contains several other layout types which may provide varying results.
Case 4 (Figure ) is planned for a group of six people living together, each with their own bedroom, and an additional bedroom for guests or staff members to stay overnight when required. Bedrooms are not provided with en-suite bathrooms but instead, residents share two communal bathrooms. The communal social spaces of kitchen, dining, living, and a small terrace garden are set out in an open-plan manner with good visual access between them. Due to the number of residents, the communal spaces are notably closer to the scale of a conventional house than many other layout types analysed in the present study. A small, enclosed ‘snug’, located just off the main living room, provides for more intimate conversations or quiet activities.
Like other high-scoring layout types, Case 4 (77.6%) performs well across the majority of DDPs (Figure ). The main observable weakness from a Plan-EAT perspective is under DDP#3 Visual Access (32% vs 56% Avg.), where potential wayfinding difficulties are created by the lack of visual access between resident bedroom doorways and communal spaces, a factor which is the subject of three distinct queries (Qs 3.01, 3.02, and 3.03). However, considering the small overall scale of this layout type, this issue is unlikely to be as problematic as a similar lack of visual access might be in substantially larger units with more complex spatial arrangements.
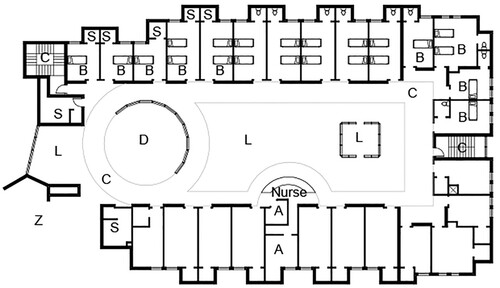
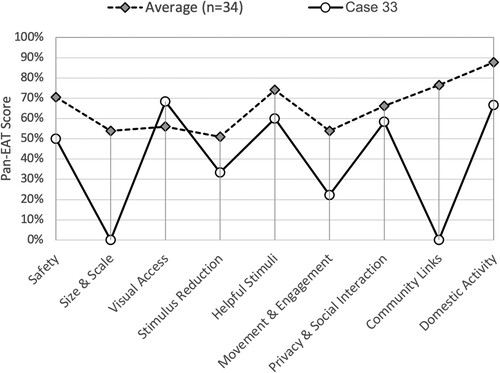
Case 33
Case 33 is a residential care facility located within a large geriatric health complex. Its layout type (Figure ), which is repeated identically over three floors, hosts 40 bedspaces per unit. Bedrooms are laid out around and opening into a large-scale communal space hosting dining, lounge, and activity areas. The open space is positioned in such a way that it can be viewed by a centrally located nurse station.
Scoring just 39.9% in the Plan-EAT assessment (Figure ), this was the second lowest scoring layout in this research. Although it performs slightly better than average under DDP#3 Visual Access (68% vs. 56%) it falls short on all other DDP’s. Positive features include, for example, that residents can see the lounge and the dining room from their bedroom door (Q3.02, Q3.03), whilst most bedroom doors can conversely be seen from the lounge room (Q3.01). A toilet can also be seen from both the dining and lounge rooms (Q3.08, Q3.09). However, this case has several weaknesses, with the most significant being lack of outdoor space available to residents, leading to reduced scores across several DDPs and being unable to address several assessment items relating to stimulation, engaging activity, and community. The unit is located on an upper floor, so it is possible that a garden may be available on another level. In this case wayfinding to any available outdoor space is likely to be problematic, and the space is unlikely to be easily supervised from the point(s) where staff spends most of their time. A remotely located garden also presents technical and ethical concerns beyond the strict limits of formal Plan-EAT. For example, conventional care practice is unlikely, for safety reasons, to allow residents to travel between levels unaccompanied, making use of the garden even more difficult and access less likely to occur on a sufficiently frequent basis for optimal benefit to residents’ wellbeing. Another significant concern about Case 33 is the unit capacity of up to 40 residents, whereas the available evidence gives strong indications that less than 10 residents per unit (Q2.01) is optimal for resident wellbeing. Meanwhile, the unit layout does not indicate the availability of separate spaces where residents can dine alone (Q8.05) or with visiting friends or relatives (Q9.01). This issue is compounded by the kitchen not being accessible to residents (Q10.01), and not being visible from either the lounge or dining rooms (Q5.05).
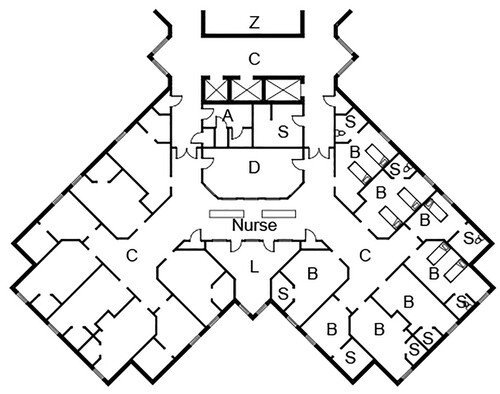
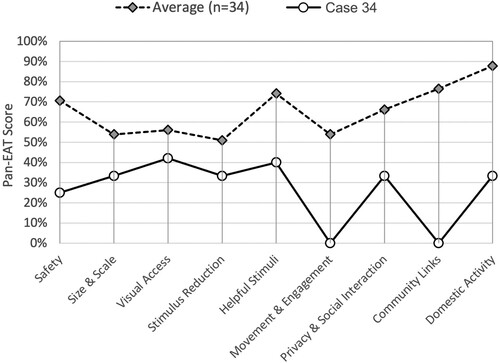
Case 34
Case 34 is the lowest scoring layout type in the study (Figure ), whilst another layout from the same facility scored third last of the 34 layout types reviewed. They are near identical in many respects, each hosting 26 bedspaces laid out in a Y-shaped configuration with the main dining and lounge spaces located close to the centre. A large nurse station occupies a central location with high visual accessibility over most communal areas of the unit. Like Case 33, the most significant weakness of Case 34 is the lack of outdoor space for residents. This leads to reductions in Plan-EAT scores (Figure ) and related issues of concern about the wellbeing of residents across many aspects of the design. Internally the layout is problematic due to the lack of direct visibility between key spaces of interest to residents.
Conclusions
The findings of this paper demonstrate a potentially valuable new method, the Plan-EAT, which can assist designers to self-assess and improve dementia design quality in the building layouts of RCFs. The method offers the first systematic evaluation of RCFs focused entirely on architectural layout planning, using evidence-based dementia-specific design assessment criteria.
This application of the Plan-EAT offers the first formal cross-evaluation of the some of the most well-known precedents used by architects for RCFs. Although the modest sample of cases, taken from published collections, limit the potential extrapolation of findings of the paper, the findings offer several tangible insights into dementia design that are relevant to both practice and research in the field. While noting the methodological limitations outlined previously, the results of this paper including the range of scores obtained, (low = 26.7% and Avg. =65.6%) raise concerns about the capacity of several cases to be reliable precedents in the architectural design of RCFs.
The future development and rigorous application of the Plan-EAT would benefit from more extensive inter-rater testing and external validation. Research that employs significantly expanded sampling of non-published RCF as representative cross sections of dementia care environments in various countries could also provide helpful insight into the design quality of the broad stock of existing dementia care environments.
Finally, the findings of this paper highlight some potential risks in over-reliance on narrow or unverified information sources during the architectural design of environments for people living with dementia. It is the authors’ view that architectural design should begin with a stated set of values and principles that counterbalance any tendency to take a simplistic view of the design process, e.g. The Dignity Manifesto of Design for People Living with Dementia (Fleming, Zeisel, and Bennett Citation2021).
Copies of the Plan-EAT are available, on request, from the corresponding author.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Aged Care Financing Authority. 2016. Fourth Report on the Funding and Financing of the Aged Care Sector, Aged Care Financing Authority. Canberra. https://webarchive.nla.gov.au/awa/20190509083436/https://agedcare.health.gov.au/2016-report-on-the-funding-and-financing-of-the-aged-care-industry.
- Anderzhon, J. W., D. Hughes, S. Judd, E. Kiyota, M. Wijnties, S. Judd, E. Kiyota, and M. Wijnties. 2012. Design for Aging: International Case Studies of Building and Program. Hoboken, NJ: Wiley.
- Australian Institute of Health and Welfare. 2011. Dementia Among Aged Care Residents: First Information from the Aged Care Funding Instrument. Canberra. http://www.aihw.gov.au/publication-detail/?id=10737419025.
- Australian Institute of Health and Welfare. 2012. Dementia in Australia. Australian Government Publishing Service. https://www.aihw.gov.au/reports/dementia/dementia-in-australia/contents/table-of-contents.
- Bowes, A., and A. Dawson. 2019. Designing Environments for People with Dementia: A Systematic Literature Review (pp. 1–92). Bingley: Emerald Group Publishing Limited.
- Castell, L. 2008. “Building Access for the Intellectually Disabled.” Facilities 26 (3/4): 117–130. doi:10.1108/02632770810849463.
- Cohen, U., and K. Day. 1993. Contemporary Environments for People with Dementia. Baltimore: John Hopkins University Press.
- Cunningham, C., J. Galbraith, M. Marshall, C. McClenaghan, M. McManus, D. G. McNair, R. Pollock, et al. 2008. Dementia Design Audit Tool. 1st Edition. Stirling: University of Stirling.
- Dawson, A., and P. Palmer. 2020. “United Kingdom: Environmental Design Education in a Changing World.” In World Alzheimer Report 2020: Design Dignity Dementia: Dementia-Related Design and the Built Environment Volume 1, edited by R. Fleming, J. Zeisel, and K. Bennett, 208–215. London: Alzheimer's Disease International.
- Elmståhl, S., L. Annerstedt, and O. Åhlund. 1997. “How Should a Group Living Unit for Demented Elderly be Designed to Decrease Psychiatric Symptoms?” Alzheimer Disease and Associated Disorders 11 (1): 47–52. doi:10.1097/00002093-199703000-00008.
- Feddersen, E., and I. Lüdtke. 2017. Living for the Elderly (2nd ed., p. 239). Basel: Birkhäuser.
- Fleming, R. 2011. “An Environmental Audit Tool Suitable for use in Homelike Facilities for People with Dementia.” Australasian Journal on Ageing 30 (3): 108–112. doi:10.1111/j.1741-6612.2010.00444.x. Blackwell Publishing Ltd.
- Fleming, R., I. Forbes, and K. A. Bennett. 2003. Adapting the Ward for People with Dementia, Adapting the Ward for People with Dementia. Sydney, NSW: The Hammond Group.
- Fleming, R., B. Goodenough, L-F. Low, L. Chenoweth, and H. Brodaty. 2016. “The Relationship Between the Quality of the Built Environment and the Quality of Life of People with Dementia in Residential Care.” Dementia (Basel, Switzerland) 15 (4): 663–680. doi:10.1177/1471301214532460.
- Fleming, R., J. Zeisel, K. Bennett, J. Golembiewski, K. Swaffer, and L. Henderson. 2021. The Dignity Manifesto of Design for People Living with Dementia. https://designdignitydementia.com/.
- Hadjri, K., V. Faith, and M. McManus. 2012. “Designing Dementia Nursing and Residential Care Homes.” Journal of Integrated Care 20 (5): 322–340. doi:10.1108/14769011211270765.
- Hanson, J., and R. Zako. 2005. “Configuration and Design in Caring Environments: Syntax and quality of life in.” 5th International Space Syntax Symposium.
- Hendriks, A., and H. Wilkinson. 2020. “The Involvement of People with Dementia in the Design Process: A (Political) Choice to Make.” In World Alzheimer Report 2020: Design Dignity Dementia: Dementia-Related Design and the Built Environment Volume 1, edited by R. Fleming, J. Zeisel, and K. Bennett, 126–132. London: Alzheimer’s Disease International.
- Judd, S., M. Marshall, and P. Phippen. 1998. Design for Dementia (p. 150). London: Hawker Publications.
- Lee, J. H., M. J. Ostwald, and H. Lee. 2017a. “Measuring the Spatial and Social Characteristics of the Architectural Plans of Aged Care Facilities.” Frontiers of Architectural Research. Elsevier B.V 6 (4): 431–441. doi:10.1016/j.foar.2017.09.003.
- Lee, J. H., M. J. Ostwald, and R. Yu. 2017b. “Investigating Visibility Properties in the Design of Aged-Care Facilities.” In International Conference of the Association for Computer-Aided Architectural Design Research in Asia (CAADRIA), Hong Kong, 365–374. Accessed 28 December 2020. http://papers.cumincad.org/data/works/att/caadria2017_016.pdf.
- Marquardt, G., K. Bueter, and T. Motzek. 2014. “Impact of the Design of the Built Environment on People with Dementia: An Evidence-Based Review.” Health Environments Research & Design Journal (HERD) 8 (1): 127–157. doi:10.1177/193758671400800111.
- Marquardt, G., and P. Schmieg. 2009. “Dementia-Friendly Architecture: Environments That Facilitate Wayfinding in Nursing Homes.” American Journal of Alzheimer’s Disease and Other Dementias 24 (4): 333–340. doi:10.1177/1533317509334959.
- Matthews, F. E., A. Arthur, L. E. Barnes, J. Bond, C. Jagger, L. Robinson, and C. Brayne. 2013. “A Two-Decade Comparison of Prevalence of Dementia in Individuals Aged 65 Years and Older from Three Geographical Areas of England: Results of the Cognitive Function and Ageing Study I and II.” The Lancet 382: 1405–1412. doi:10.1016/S0140-6736(13)61570-6.
- Nordin, S., K. McKee, H. Wijk, and M. Elf. 2017. “Exploring Environmental Variation in Residential Care Facilities for Older People.” Health Environments Research & Design Journal (HERD) 10 (2): 49–65. doi:10.1177/1937586716648703.
- Palmer, L., K. Wallace, and L. Hutchinson. 2021. Architecture for Dementia – Stirling Gold 2008-2020. Stirling: University of Stirling.
- Parker, C., S. Barnes, K. McKee, K. Morgan, J. Torrington, and P. Tregenza. 2004. “Quality of Life and Building Design in Residential and Nursing Homes for Older People.” Ageing and Society 24 (6): 941–962. doi:10.1017/S0144686X04002387.
- Peatross, F. D. 1997. “The Spatial Dimension of Control in Restrictive Settings.” In Space Syntax First International Symposium, 14.1–14.16. London: Space Syntax.
- Prince, M., M. Knapp, M. Guerchet, P. McCrone, M. Prina, A. Comas-Herrera, R. Wittenberg, et al. 2014. Dementia UK: Second Edition Overview (pp. 12–13). London: Alzheimer’s Society.
- Quirke, M. 2019. ‘Building Design for People with Dementia: A Comparative Analysis of Planning Quality in Residential Aged Care Units’ (p. 304). Newcastle, Australia: University of Newcastle. https://nova.newcastle.edu.au/vital/access/manager/Repository/uon:35038.
- Quirke, M., M. J. Ostwald, R. Fleming, M. Taylor, and A. Williams. 2021. “Design Stage Evaluation Tools for Residential Dementia Care Environments.” Facilities, doi:10.1108/F-09-2020-0106. Vol. ahead-of-print No. ahead-of-print.
- Robinson, J. W. 1990. “Architectural Research: Incorporating Myth and Science.” Journal of Architectural Education 44 (1): 20–32. https://www.jstor.org/stable/1424972.
- Sloane, P. D., M. Mitchell, G. Weisman, S. Zimmerman, K.M. Long, M. Lynn, M. Calkins, et al. 1990. “The Therapeutic Environment Screening Scale: An Observational Screening Instrument to Assess the Quality of Nursing Home Environments for Residents with Dementia.” American Journal of Alzheimer’s Disease and Other Dementias 5 (6): 22–26. doi:10.1177/153331759000500606.
- Smith, R., R. Fleming, L. Chenoweth, Y. H. Jeon, J. Stein-Parbury, and H. Brodaty. 2012. “Validation of the Environmental Audit Tool in Both Purpose-Built and non-Purpose-Built Dementia Care Settings.” Australasian Journal on Ageing 31 (3): 159–163. doi:10.1111/j.1741-6612.2011.00559.x.
- Utton, D. 2007. Designing Homes for People with Dementia (p. 140). London: Hawker Publications.
- Van Hoof, J., H. S. M. Kort, H. van Waarde, and M. M. Blom. 2010. “Environmental Interventions and the Design of Homes for Older Adults with Dementia: An Overview.” American Journal of Alzheimer’s Disease & Other Dementias 25 (3): 202–232. Doi:10.1177/1533317509358885.
- Wang, D., and L. Groat. 2002. Architectural Research Methods. New York: John Wiley and Sons Inc.
- Weisman, G., M. P. Lawton, P. S. Sloane, M. Calkins, and L. Norris-Baker. 1996. The Professional Environmental Assessment Protocol. Milwaukee, WI: University of Wisconsin at Milwaukee.
- Wittenberg, R., B. Hu, C. Jagger, A. Kingston, M. Knapp, A. Comas-Herrera, D. King, A. Rehill, and S. Banerjee. 2020. “Projections of Care for Older People with Dementia in England: 2015 to 2040.” Age and Ageing 49 (2): 264–269. doi:10.1093/ageing/afz154.