Abstract
The aim of this article is to investigate the effect of a physical rest-frame, habituation and age on simulator sickness in an advanced mobility scooter driving simulator. Twenty-six young and 34 older adults completed a total of 12 drives in an advanced mobility scooter driving simulator over two visits. A 2x2 crossover design was used to measure the effect of a rest frame that was added to the driving simulator on either the first or second visit. The Simulator Sickness Questionnaire was used to measure simulator sickness symptoms. A significant decrease in simulator sickness was observed between the first and the second visit. Older adults reported more severe simulator sickness symptoms compared to younger participants. No effect of rest-frame could be found. Habituation appears to be the most effective method to reduce simulator sickness in an advanced mobility scooter driving simulator. More research is needed to investigate simulator sickness in patient groups.
Practitioner summary: Experiencing simulator sickness is a major problem across all types of simulators. The present experiment investigated the effect of a rest-frame, habituation and age on developing simulator sickness symptoms in an advanced mobility scooter driving simulator. Habituation appeared to be the most effective method to reduce simulator sickness.
Introduction
Driving simulators have become a frequently used method to test driving behaviour because they have created the opportunity to teach and improve driving skills in a risk-free and cost-effective environment. The validity of driving simulators has been demonstrated by various studies (Lee, Cameron, and Lee Citation2003; Lew et al. Citation2005; Veldstra Citation2014; Meuleners and Fraser Citation2015; Klüver et al. Citation2016). However, simulator sickness, which is known as a by-product of high fidelity visual simulators, may be a threat to this validity (Kennedy et al. Citation1993; Mullen et al. Citation2011; Helland et al. Citation2016). The symptoms experienced when suffering from simulator sickness include headaches, dizziness, drowsiness, sweating or nausea, for example. In contrast to motion sickness in real traffic, symptoms are visually induced rather than caused by physical movement. The incidence of simulator sickness can differ greatly (La Viola 2000; Brooks et al. Citation2010; Stoner, Fisher, and Mollenhauer Citation2011; Bos et al. Citation2013; Keshavarz, Hecht, and Lawson Citation2014).
Possible explanations for simulator sickness
Several theories explaining possible causes and processes underlying simulator sickness have been proposed; however, none of these theories is generally acknowledged as superior (Keshavarz, Hecht, and Lawson Citation2014; Stoner, Fisher, and Mollenhauer Citation2011). The most widely accepted theory is the sensory conflict theory or cue conflict theory, which states that simulator sickness is the result of both a sensory conflict and the held expectations based on previous experience of the sensory system (Reason and Brand Citation1975; Oman, 1990). Accordingly, simulator sickness can occur in a stationary simulator when a subject has not yet established a pattern to match the contradictory information from the visual system (‘I am moving’) and the vestibular system (‘I am stationary’) (Stoner, Fisher, and Mollenhauer Citation2011). Sensory conflict theory is supported by the finding that people who have many years of driving experience in the real world experience more simulator sickness than people with less driving experience (Stoner, Fisher, and Mollenhauer Citation2011). In addition to that, the fact that simulator sickness symptoms can be reduced by repeated exposure to the simulator task (thus adapting expectation) also provides evidence for the sensory conflict theory. A number of studies have demonstrated a habituation effect on the occurrence of simulator sickness (Hill and Howarth Citation2000; Howarth and Hodder Citation2008; Teasdale et al. Citation2009; Domeyer, Cassavaugh, and Backs Citation2013; Zhang et al. Citation2015; Helland et al. Citation2016; Keshavarz Citation2016). Domeyer, Cassavaugh, and Backs (Citation2013), even showed a habituation effect after 2 days, suggested that simulator sickness symptoms may already decrease after a short period of time between exposure to the driving simulator.
Riccio and Stoffregen (Citation1991), however, rejected the sensory conflict theory and introduced an alternative theory to explain the occurrence of simulator sickness, the postural instability theory. Based on this theory, it is suggested that our sensory system is constantly trying to preserve postural stability in our environment. Accordingly, simulator sickness occurs when a person attempts to maintain stability in a new environment in which the body has not yet learned strategies to preserve postural stability (Riccio and Stoffregen Citation1991). Research on the postural instability theory revealed that postural instability can predict both motion and simulator sickness (Stoffregen and Smart Citation1998; Smart, Stoffregen, and Bardy Citation2002; Stoffregen et al. 2000; Stoffregen et al. Citation2017). A further study in which the position of participants was fixated reported relief in simulator sickness symptoms in older participants and thus supports the postural instability theory (Keshavarz et al. Citation2017).
Yet another explanation was proposed by Prothero et al. (Citation1999), which is known as the rest-frame hypothesis. According to this hypothesis, simulator sickness is not induced by conflicting motion cues but rather by the different ‘rest-frames’ in which these visual cues are presented. Derived from physics, a coordinate system that is used to define positions, angular orientations and motions is called a ‘reference frame’. When a reference frame is perceived to be stationary by the driver, the reference frame is called a rest-frame (Prothero et al. Citation1997). The virtual display that is presented in a virtual environment (VE) can be divided into two components. One component represents the content of the VE (i.e. the screen on which the simulation is projected) and the other component is matched to the observer’s so-called physical inertial environment (i.e. the room in which the simulator is stationed), also known as the independent visual background (IVB).
In support of this hypothesis, results of different studies showed that participants experienced less simulator sickness symptoms when they could see the laboratory wall (Prothero et al. Citation1999) or when an IVB (i.e. a grid or clouds) was added to the projection (Duh, Parker, and Furness Citation2001; Duh et al. Citation2001). Interestingly, a more natural IVB (clouds) was more effective than a background consisting of a grid pattern.
Factors that influence simulator sickness
A number of factors have been determined that influence the occurrence and severity of simulator sickness. First, graphics factors such as optical distortion, display flicker, image resolution or refresh rate (Kennedy and Fowlkes Citation1992; Kolasinski 1995; Mollenhauer Citation2004; Johnson Citation2005); in general, a wider field of view (Lin et al. Citation2002; Mollenhauer Citation2004; Johnson Citation2005) can influence simulator sickness negatively.
Second, related factors such as simulation duration, unnatural manoeuvres (freezing the screen), head movement, manoeuvre intensity, turn predictability (lack of visual cues), vehicle velocity and scene content (Kennedy and Fowlkes Citation1992; Kolasinski 1995; Mourant and Thattacheny Citation1999; Kennedy, Stanney, and Dunlap Citation2000; Jaeger and Mourant Citation2001; Johnson Citation2005; Mourant et al. Citation2007) can worsen symptoms. The third category comprises individual factors, which besides age (Brooks et al. Citation2010), include the amount of experience in the simulated environment, experience in non-simulated environments, history of motion sickness and medications, general health and sleep deprivation (Crowley Citation1987; Kennedy and Fowlkes Citation1992; Johnson Citation2005). In addition to that, cognitive factors can play a role in experiencing simulator sickness symptoms. Although research has not found significant differences between healthy and cognitively impaired individuals in simulator sickness incidence rates, the odds of cognitively impaired individuals (mostly stroke patients) were found to be 2.4 times larger compared to cognitively healthy individuals (Rizzo et al. Citation2003).
In general, Klüver et al. (Citation2015) concluded in their study that participant and scenario characteristics can explain the development of simulator sickness symptoms better than simulator characteristics.
The advanced mobility scooter driving simulator
Most research on simulator sickness has been conducted for aviation or car driving simulators. Dropout rates in these driving simulators can vary largely based on the type of simulator and characteristics of the participants (Trick and Caird Citation2011). With increasing use of alternative forms of mobility, especially mobility scooters, new types of driving simulators have been developed. The University of Groningen, in collaboration with Royal Dutch Visio (Centre of Expertise for Visually Impaired and Blind People, the Netherlands), was one of the first to develop an advanced mobility scooter driving simulator (AMSDS) for clinical and scientific purposes in different (patient) populations. However, chances on experiencing simulator sickness in the AMSDS appeared to be extremely high. In one particular experiment, nearly 70% (65 out of 94) of the participants had to end test procedures prematurely due to simulator sickness symptoms (Cordes et al. Citation2018). This high dropout rate is even more striking considering the fact that in experiments with the car driving simulator, situated in the same room and using the same display and underlying technology, a dropout rate of 25% would have been considered to be normal.
The present experiment
The high incidence of simulator sickness in the AMSDS compared to the regular driving simulator might be due to several differences between the two types of simulator. For instance, task-related factors in the mobility scooter might be relatively more demanding in the AMSDS because mobility scooters take sharper turns and have a relatively sharper acceleration and deceleration. Although it has been shown that a complex environment might lead to simulator sickness, the virtual environments included a city drive with much interacting traffic because a large degree of ecological validity was to be achieved. Therefore, it was not feasible to change scenario characteristics. Instead, the goal of the present study was to incorporate more achievable changes to the simulator and to test their effect on simulator sickness in the AMSDS. Based on the rest-frame hypothesis proposed by Prothero et al (Citation1999), a physical grid pattern was added to the screens of the simulator set-up with the expectation that a more visible independent background would reduce simulator sickness. In addition to that, the effect of a habituation across two sessions with 24 h in-between was investigated. Both solutions were tested in young and old adults.
Method
Participants
Twenty-six young adults (age between 18 and 30) and 34 older adults (age between 50 and 75) took part in the present study. Characteristics of the participants are presented in . Younger participants were recruited via social media and by approaching psychology students from the University of Groningen. Older participants were recruited via advertisements, flyers and personal contacts. All participants were in possession of a valid driver’s license. Exclusion criteria were ocular disease, vestibular disorders or any other medical/neurological conditions or medication that could interfere with driving performance. Students received study credit points for participating; other participants took part in the experiment on a voluntary basis. The experiment was approved by the Ethical Committee Psychology of the University of Groningen, the Netherlands, according to the Declaration of Helsinki. All participants provided written informed consent.
Table 1. Participants’ characteristics.
Apparatus
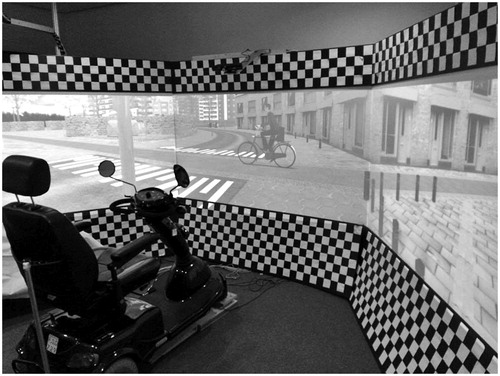
The AMSDS has been developed using ST Software (Groningen, the Netherlands). The mobility scooter that is used as a mock-up is a real vehicle with technical adjustments that has been attached to the simulation computers using steer recorders and switches (see ).
The software of the driving simulator consists of a calculation model of simulated traffic with autonomous characteristics in which all simulated traffic participants drive independently in a network of roads. This surrounding traffic is created in and controlled by a scripting tool that allows the type of interactions intended for the experiment. The scripting-tool also avoids traffic conflicts between simulated traffic participants and manages data collection.
The graphics hardware consists of three PC’s that run the software, controlling three computer displays with an imaging frequency of 60 Hz. The simulation was projected onto three screens. The sizes of the middle screen and side screens are 200 × 150 cm. The middle screen has a resolution of 1920 × 1080 pixels and the side screens both have a resolution of 1024 × 768 pixels. The dimensions of the projection on the screens are 200 × 110 cm. Horizontal and vertical field of view were 180° and 34° (middle screen) respectively.
The front of the mobility scooter was positioned about 80 cm in front of the middle screen, in such way that the participant’s view to all the screens was perpendicular to the middle while sitting in the mobility scooter. The software projected the movement of the mobility scooter in the simulated environment, based on the steering wheel forces. The software additionally generated the sounds of the engine and the sounds of the surrounding traffic through two speakers, situated behind the projection screen.
Because one of the original aims of the AMSDS was to assess fitness-to-drive in visually impaired people, the rest-frame could not be part of the visual projection, as it was implemented in other studies (Prothero et al. Citation1999; Duh, Parker, and Furness Citation2001; Lin, Habib, and Lahav Citation2004). Instead, the rest-frame was constructed of solid materials surrounding the screens on which the simulation was projected. Compared to the IVB conditions in the studies by Duh, Parker, and Furness (Citation2001) and Lin et al. (Citation2002), the characteristics of the rest-frame in the current study also comprised a grid-shaped pattern. The rest-frame consisted out of six black synthetic covers on which a grid was added by attaching white paper squares onto the plates (see ). In the experimental condition, a rest-frame was added to the screens. In addition, to keep the contrast of the projection optimal for people with low vision, luminance in the simulator room was kept to a minimal. In the control condition, participants saw the white projection screens.
Virtual environments
The driving simulation study comprised six drives in rural environments under different conditions (see ). Visual complexity and speed increased over the number of drives. During all of the drives, participants had to follow a winding road. During the test drives in which the participants controlled their own speed, participants were asked to start driving with a speed they felt comfortable with. When the first half of the drive was finished, participants were asked to drive as fast as they could, provided that they were still driving safely. Environments without any obstacles included a winding road surrounded by nature (i.e. meadows, trees), whereas the more complex environments included obstacles and were located in a residential area with several crossings. Obstacles included stationary objects with different visibility and moving traffic agent (cars, cyclists and pedestrians) that either appeared at crossings or on the same lane participants were travelling on. Participants were instructed to keep a steady position on the road and to avoid collisions with obstacles or other traffic participants.
Table 2. Different virtual driving environments.
Procedure
The experiment took place at the University Medical Centre Groningen, the Netherlands, where the AMSDS was stationed. All participants visited the laboratory on two consecutive days. Each visit lasted approximately 45 min. The interval between the two visits was exactly 24 h. Before the experiment started, participants were informed about the possibility of experiencing simulator sickness and their right to stop the experiment at any moment.
At the start of the first visit, participants completed a questionnaire about demographic information, driving experience, self-perceived driving skills and general health. Participants were then asked to complete a practice drive to get used to operating the AMSDS. Upon successful completion of the practice drive, participants moved on to the six test drives. A crossover design (AB|BA) with stratified random allocation (based on age group) was used to determine which participant completed the driving simulation tasks with or without the rest-frame on the first visit. On the second visit, participants immediately started with the six test drives but now in a different condition compared to the first visit (with or without the rest-frame).
After each drive, participants filled in the Simulator Sickness Questionnaire (SSQ, Kennedy et al. Citation1993) and the Misery Scale (MISC, Emmerik, De Vries, and Bos Citation2011) to monitor simulator sickness symptoms. The SSQ consists of 16 items, each containing a single symptom related to simulator sickness that can be scored on a scale from 0 (not experiencing the symptom) to 3 (strongly experiencing the symptom). Sum score of the SSQ after each drive could range from 0 to 235.62 points. The MISC is a 10-point scale, reaching from 0 (not experiencing symptoms) to 10 (throwing up). Intermediate scores range from 1 (feeling uneasy but without symptoms of nausea), 2–5 (dizziness, feeling warm, sweating, headache, etc. without feeling nauseous) and 6–9 (degrees of nausea). The MISC was used as a tool for the test leader to monitor simulator sickness during the trials and prevent participants from developing severe symptoms of simulator sickness, such as vomiting. When participants scored 6 or higher the experiment was stopped to ensure the wellbeing of the participants.
At the end of the second visit, participants were debriefed and given an additional short questionnaire in which they were asked how they experienced the study and whether they preferred to drive in the AMSDS with or without the rest-frame.
Statistical analysis
The main effects of frame (presence or absence), habituation (1st versus 2nd visit) and age (older and younger adults) were investigated. In addition, interaction effects between frame and age and habituation and age were examined. Repeated measures ANOVAs with age as a between-subject factor were used for this purpose.
The SSQ is subdivided into three subscales: Nausea (e.g. burping, stomach awareness), oculomotor (e.g. blurred vision, eyestrain) and disorientation (e.g. dizziness, vertigo) (Kennedy et al. Citation1993). Scores for the two visits have been calculated for the individual subscales and for the SSQ total score for each of the six drives according to Kennedy et al. (Citation1993). The average SSQ total scores of the individual drives were determined for either the presence/absence of the frame or the first or second visit in the laboratory. Independent variables were presence/absence of the rest-frame, visit and age group; dependent variables were the average SSQ total scores per condition. In case participants dropped out during the first visit due to severe simulator sickness symptoms, the SSQ total score for their last completed drive was adopted to restore missing data. Differences in SSQ total scores of visit 1 for the different age groups were calculated accordingly using an independent sample t-test. The data of participants that did not show up for the second visit were excluded pairwise for the analysis of variance.
P-values < .05 were defined as significant. Effect sizes were calculated for main effects using the effect size r (Field Citation2009). Effect sizes were classified as followed: r = 0.10: small effect, r = 0.30: medium effect, r = 0.50: large effect.
Results
Dropout and preliminary analysis
Six participants of the older age group did not show up for the second visit of the experiment. Two of these participants did not complete any drives in the first visit either as they decided to stop after the practice drive of the first visit. Two participants completed only a limited number of the drives of the first visit and another two participants completed all drives of the first visit. One participant, belonging to the older age group as well, stopped halfway through the drives of the first visit, but returned for the second visit and completed all six drives of the second visit. In contrast, all participants of the younger age group completed all drives of both the first and the second visit.
Main analysis
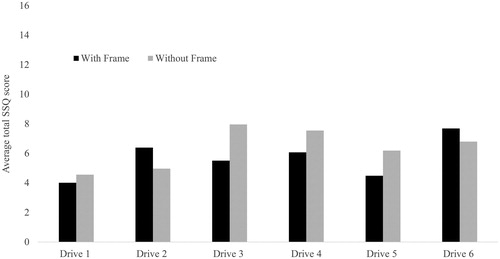
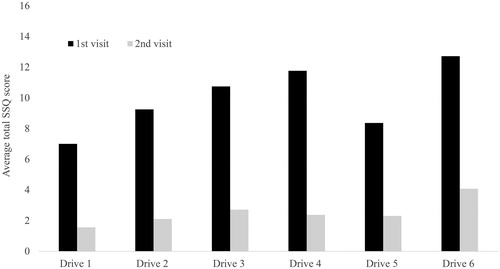
The results of the analysis of variance showed that there was a significant main effect of visit (F(1,52) = 27.94, p < .001, r = 0.59) and age group (F(1,52) = 4.65, p = .036, r = 0.29) with regard to the total SSQ score. Effect sizes were large and medium, respectively. Reported simulator sickness symptoms decreased in the second visit of the experiment and older adults reported more severe symptoms than young adults (). Furthermore, independent sample t-tests revealed that there was a significant difference between older and younger adults on the first (t(42.1) = −2.57, p = .014, r = 0.37) but not on the second visit (t(34.3) = −1.98, p = .056, r = 0.32). Medium effect sizes could be found in both comparisons. No effect of frame was found (F(1,52) = 0.19, p = .662, r = .09) and the effect size was small. Interaction effects between frame and age group (F(1,52) = 0.10, p = .719) and visit and age group (F(1,52) = 2.84, p = .097) were neither found to be significant. However, the size of the p-value suggests that the effect of visit might have been stronger in the older age group. Generally, it could be observed that the standard deviations of older participants were noticeably higher than those of the younger participant group, showing higher variability of simulator sickness symptoms in older adults ().
Table 3. SSQ scores for main and interaction effects.
With regard to the subscales, there were no main effects for frame, no interaction effect for frame and age group and no interaction effect for visit and age group for all three subscales. In line with the main effect for visit on the total SSQ score, the main effect for visit was found on all three subscales (lower SSQ scores on second visit).
In , the average SSQ score for the presence/absence of the frame is shown for the individual drives. It can be observed that SSQ scores seem to be higher for the no-frame condition in all drives, except for drive 2. Likewise, shows the average SSQ score for the time of the visit. Supporting the statistically significant result, SSQ scores are lower for the second visit in all drives.
Analysis of the short questionnaire that was filled in after debriefing showed no preference for driving with or without the rest-frame. About half of the participants preferred to drive with rest-frame since the frame had a calming effect and offered stability. However, the other half preferred to drive without the rest-frame as they thought the frame caused more chaos and actually resulted in feelings of distress, dizziness and instability. Among the participants who felt uncomfortable driving with the rest-frame, it was often suggested that the feelings of instability were caused by the black and white squares, as the squares appeared to be moving during the simulation.
Discussion
The present study investigated the effect of a physical rest-frame, habituation and age on experiencing simulator sickness in an AMSDS.
Based on previous studies using a projected rest-frame (Prothero et al. Citation1999; Duh, Parker, and Furness Citation2001; Lin, Habib, and Lahav Citation2004), it was hypothesised that adding a rest-frame to the display of the VE in the AMSDS would relieve simulator sickness symptoms in participants. Unlike these studies, however, the use of a physical rest-frame in this study did not significantly alleviate simulator sickness symptoms. This result might be an indication that a physical variant of an IVB is not as effective as the projected counterpart which was used in the study by Duh, Parker, and Furness (Citation2001). Another explanation might be that the rest-frame in our experiment was not visible enough. Duh, Parker, and Furness (Citation2001) used bright projections to light up the grid from the background, whereas in our study illumination was reduced to enhance the contrast of the projected VE. Because the AMSDS was set-up to investigate driving in people with visual impairments, good contrast of the projected VE is of great importance. Lin et al. (Citation2002) further suggested in their study that IVB brightness and luminance may contribute to the positive effects of the IVB. However, approximately half of the participants of the present study reported that they were irritated by the rest-frame, rather than gaining a benefit from it. In line with that, a study by Keshavarz, Hecht and Zschutschke (Citation2011) revealed that, especially, a well-visible background might lead to an increase in simulator sickness symptoms. The authors hold an intra-visual conflict – more specifically, the conflict between the two images of the projection and the laboratory surrounding – responsible for this effect. These results thus suggest that the grid used in the present study might have had an adverse rather than beneficial effect on experiencing simulator sickness.
With regard to age, it can be concluded that the older participants in our study experienced more simulator sickness than younger participants. Although no difference between younger and older participants could be found as a function of frame or visit, we found a significant difference in experienced simulator sickness between the group of older participants and the group of younger participants. The higher dropout rate in the older age group (six dropouts compared to none in the younger group) also supports the notion that older participants experience simulator sickness more severely compared to younger participants. This result is in consonance with outcomes reported by Brooks et al. (Citation2010) and Keshavarz et al. (Citation2017). Different explanations of this phenomenon have been given in the literature. In line with the cue conflict theory (Stoner, Fisher, and Mollenhauer Citation2011), an explanation could be that older participants reported more physical driving experience and thereby experienced a stronger conflict in the driving simulator based on this experience. However, Chang et al. (Citation2017) did not find any differences in incidence and severity of simulator sickness between drivers and non-drivers of the same age-group. In a similar study, Stoffregen et al. (Citation2017) reported that although drivers developed simulator sickness quicker than non-drivers compared to non-drivers, severity of the symptoms was not affected by experience. Another explanation could be based on the postural sway theory. Keshavarz et al. (Citation2017) showed in their study that older but not younger participants experienced simulator sickness in an unrestrained condition as compared to the condition where head and torso were fixed to the seat. This could be explained by reduced postural control in the older participants.
With regard to habituation, we found that participants experienced considerably less simulator sickness symptoms during the second visit in the AMSDS than during the first visit. This finding is supported by the results of other studies as well (Hill and Howarth Citation2000; Howarth and Hodder Citation2008; Teasdale et al. Citation2009; Domeyer, Cassavaugh, and Backs Citation2013; Zhang et al. Citation2015; Keshavarz Citation2016). Generally, it has been shown that long, continuous exposure to simulator tasks can result in the worsening of symptoms, whereas a distributed exposure, or habituation to the simulator tasks, can reduce severity of simulator sickness symptoms (McCauley and Sharkey Citation1992; Kennedy, Stanney, and Dunlap Citation2000). The habituation effect in our study was already noticeable within 24 h, rather than the 48 h proposed by Domeyer, Cassavaugh, and Backs (Citation2013). However, habituating participants to driving simulator tasks can be a time and cost-consuming procedure and can be difficult to implement. Keshavarz (Citation2016) suggested that a shorter training of similar tasks might alleviate simulator sickness symptoms as well. More research needs to be done to investigate the most effective way of habituation to reduce simulator sickness symptoms.
Compared to the first mobility scooter driving simulator study testing driving performance in visually impaired individuals (Cordes et al. Citation2018), the dropout rate of the participants (10%) was surprisingly low. Reasons for the low incidence of symptoms could be the chosen age group and health condition of the participants of the present study. Participants of the first mobility scooter driving simulator study were only older adults (50–75 years of age) and had some form of visual impairment (low visual acuity, visual field defects). Because driving simulators are especially useful to test driving performance of individuals with compromised health (e.g. motor, visual or cognitive impairment), future research needs to assess simulator sickness susceptibility of these populations.
Simulator sickness is a complex phenomenon and dependent on many different factors. The present study has looked at a number of well-reported variables that influence simulator sickness; however, other factors might have played a role as well. The simulator was set-up in a fully immersed environment which on the one hand increased ecological validity, but on the other hand has also shown to be one of the main factors of experiencing simulator sickness (Stoner, Fisher, and Mollenhauer Citation2011). Another research institute using a mobility scooter simulator found that decreasing the size of the screens reduced simulator sickness notably (Het Roessingh, personal communication). Furthermore, the urban environment in some of the simulator drives contained many features that increased optical flow, another factor that has been shown to worsen sickness. Lastly, the type of task in AMSDS required participants to steer around objects, which could have been yet another factor increasing simulator sickness. However, in this study, it was not realistic to change screen size or scenario characteristics because the virtual environments were used for other research purposes as well.
In conclusion, habituation seems to be the easiest and most promising method to reduce simulator sickness symptoms in the AMSDS, whereas the inclusion of a rest-frame as used in this study is a redundant addition to the simulator set-up. More research has to be done to explore additional factors and different patient groups before the driving simulator can be used for clinical purposes.
| Abbreviations | ||
| AMSDS | = | advanced mobility scooter driving simulator |
| IVB | = | independent visual background |
| MISC | = | misery scale |
| SSQ | = | simulator sickness questionnaire |
| VE | = | virtual environment |
Acknowledgements
The authors want to thank the participants who took part in this study, Peter van Wolffelaar (ST Software) and Jeroen Meijer (Infabula) for creating the driving simulator and their technical support, and Jelte Bos (TNO) for his advice with regard to simulator sickness.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
References
- Bos, J. E., W. D. Ledegang, A. J. A. Lubeck, and J. F. Stins. 2013. “Cinerama Sickness and Postural Instability.” Ergonomics 56 (9): 1430–1436 doi:10.1080/00140139.2013.817614.
- Brooks, J. O., R. R. Goodenough, M. C. Crisler, N. D. Klein, R. L. Alley, B. L. Koon, W. C. Logan, J. H. Ogle, R. A. Tyrrell, and R. F. Wills. 2010. “Simulator Sickness during Driving Simulation Studies.” Accident Analysis and Prevention 42 (3): 788–796. doi:10.1016/j.aap.2009.04.013.
- Chang, C.-H., F.-C. Chen, W.-C. Kung, and T. A. Stoffregen. 2017. “Effects of Physical Driving Experience on Body Movement and Motion Sickness during Virtual Driving.” Aerospace Medicine and Human Performance 88 (11): 985–992. doi:10.3357/AMHP.4893.2017.
- Cordes, C., J. Heutink, K. A. Brookhuis, W. H. Brouwer, and B. J. M. Melis-Dankers. 2018. “Driving slow motorised vehicles with visual impairment–a simulator study.” Cogent Psychology. doi:10.1080/23311908.2018.1485473.
- Crowley, J. S. 1987. “Simulator Sickness: A Problem for Army Aviation.” Aviation, Space, and Environmental Medicine 58 (4): 355–357.
- Domeyer, J. E., N. D. Cassavaugh, and R. W. Backs. 2013. “The Use of Adaptation to Reduce Simulator Sickness in Driving Assessment and Research.” Accident Analysis and Prevention 53:127–132. doi:10.1016/j.aap.2012.12.039.
- Duh, H. B.-L., H. Abi-Rached, D. E. Parker, and T. A. Furness. 2001. “Effects on Balance Disturbance of Manipulating Depth of an Independent Visual Background in a Stereographic Display.” Proceedings of the Human Factors and Ergonomics Society Annual Meeting 45 (27): 1882–1885. doi:10.1177/154193120104502706.
- Duh, H. B.-L., D. E. Parker, and T. A. Furness. 2001. “An ‘Independent Visual Background’ Reduced Balance Disturbance Evoked by Visual Scene Motion: Implication for Alleviating Simulator Sickness,” 3–8. doi:10.1145/365024.365051.
- Emmerik, M. L. V., S. C. De Vries, and J. E. Bos. 2011. “Internal and External Fields of View Affect Cybersickness.” Displays 32 (4): 169–174. doi:10.1016/j.displa.2010.11.003.
- Field, A. 2009. Discovering Statistics using SPSS. London, England: Sage Publications [Database] Ltd.
- Helland, A., S. Lydersen, L.-E. Lervåg, G. D. Jenssen, J. Mørland, and L. Slørdal. 2016. “Driving Simulator Sickness: Impact on Driving Performance, Influence of Blood Alcohol Concentration, and Effect of Repeated Simulator Exposures.” Accident Analysis and Prevention 94:180–187. doi:10.1016/j.aap.2016.05.008.
- Hill, K. J., and P. A. Howarth. 2000. “Habituation to the Side Effects of Immersion in a Virtual Environment.” Displays 21 (1): 25–30. doi:10.1016/S0141-9382(00)00029-9.
- Howarth, P. A., and S. G. Hodder. 2008. “Characteristics of Habituation to Motion in a Virtual Environment.” Displays 29 (2): 117–123. doi:10.1016/j.displa.2007.09.009.
- Jaeger, B. K., and R. R. Mourant. 2001. “Comparison of Simulator Sickness Using Static and Dynamic Walking Simulators.” Proceedings of the Human Factors and Ergonomics Society Annual Meeting 45 (27): 1896–1900. doi:10.1177/154193120104502709.
- Jeng-Weei Lin, J., D. E. Parker, M. Lahav, and T. A. Furness. 2005. “Unobtrusive Vehicle Motion Prediction Cues Reduced Simulator Sickness during Passive Travel in a Driving Simulator.” Ergonomics 48 (6): 608–624. doi:10.1080/00140130400029100.
- Johnson, D. M. 2005. Introduction to and Review of Simulator Sickness Research. VA: U.S. Army Research Institute.
- Kennedy, R. S., and J. E. Fowlkes. 1992. “Simulator Sickness is Polygenic and Polysymptomatic: Implications for Research.” The International Journal of Aviation Psychology 2 (1): 23–38. doi:10.1207/s15327108ijap0201_2.
- Kennedy, R. S., Norman, E. Lane, K. S. Berbaum, Michael, and G. Lilienthal. 1993. “Simulator Sickness Questionnaire – An Enhanced Method for Quantifying Simulator Sickness.” The International Journal of Aviation Psychology 3 (3): 203–220. doi:10.1207/s15327108ijap0303_3.
- Kennedy, R. S., K. M. Stanney, and W. P. Dunlap. 2000. “Duration and Exposure to Virtual Environments: Sickness Curves during and across Sessions.” Presence: Teleoperators and Virtual Environments 9 (5): 463–472. doi:10.1162/105474600566952.
- Keshavarz, B., H. Hecht, and B. D. Lawson. 2014. “Visually Induced Motion Sickness: Causes, Characteristics, and Countermeasures.” In Handbook of Virtual Environment: Design, Implementation, and Applications, edited by K. M. Stanner and K. S. Hale, 648–681. Boca Raton, FL: CRC Press.
- Keshavarz, B., H. Hecht, and L. Zschutschke. 2011. “Intra-Visual Conflict in Visually Induced Motion Sickness.” Displays 32 (4): 181–188. doi:10.1016/j.displa.2011.05.009.
- Keshavarz, B. 2016. “Exploring Behavioral Methods to Reduce Visually Induced Motion Sickness in Virtual Environments.” In Virtual, Augmented and Mixed Reality, edited by S. Lackey, and R. Shumaker, 147–155. Switzerland: Springer International Publishing.
- Keshavarz, B., A. C. Novak, L. J. Hettinger, T. A. Stoffregen, and J. L. Campos. 2017. “Passive Restraint Reduces Visually Induced Motion Sickness in Older Adults.” Journal of Experimental Psychology: Applied 23 (1): 85–99. doi:10.1037/xap0000107.
- Klüver, M., C. Herrigel, C. Heinrich, H.-P. Schöner, and H. Hecht. 2016. “The Behavioral Validity of Dual-Task Driving Performance in Fixed and Moving Base Driving Simulators.” Transportation Research Part F 37:78–96. doi:10.1016/j.trf.2015.12.005.
- Klüver, M., C. Herrigel, S. Preuß, H.-P. Schöner, and H. Hecht. 2015. “Comparing the Incidence of Simulator Sickness in Five Different Driving Simulators.” Paper presented at the Max Planck Institute for Biological Cybernetics, Tübingen, September 1–8.
- Kolasinski, E. M. 1995. Simulator Sickness in Virtual Environments. VA: U.S. Army Research Institute.
- LaViola, J. J. Jr, 2000. “A Discussion of Cybersickness in Virtual Environments.” ACM SIGCHI Bulletin 32 (1): 47–56. doi:10.1145/333329.333344.
- Lee, H. C., D. Cameron, and A. H. Lee. 2003. “Assessing the Driving Performance of Older Adult Drivers: On-Road versus Simulated Driving.” Accident Analysis and Prevention 35 (5): 797–803. doi:10.1016/S0001-4575(02)00083-0.
- Lew, H. L., J. H. Poole, E. H. Lee, D. L. Jaffe, H.-C. Huang, and E. Brodd. 2005. “Predictive Validity of Driving-Simulator Assessments following Traumatic Brain Injury: A Preliminary Study.” Brain Injury 19 (3): 177–188. doi:10.1080/02699050400017171.
- Lin, J. J. W., A. Habib, and M. Lahav. 2004. “Virtual Guiding Avatar: An Effective Procedures to Reduce Simulator Sickness in Virtual Environments.” Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, 719–726.
- Lin, J. J.-W., H. Abi-Rached, D.-H. Kim, D. E. Parker, and T. A. Furness. 2002. “A ‘Natural’ Independent Visual Background Reduced Simulator Sickness.” Proceedings of the Human Factors and Ergonomics Society 46th Annual Meeting, 2124–2128.
- McCauley, M., and T. Sharkey. 1992. “Cybersickness: Perception of Self-Motion in Virtual Environments.” Presence: Teleoperators and Virtual Environments 1 (3): 311–318. doi:10.1162/pres.1992.1.3.311.
- Meuleners, L., and M. Fraser. 2015. “A Validation Study of Driving Errors Using a Driving Simulator.” Transportation Research Part F 29:14–21. doi:10.1016/j.trf.2014.11.009.
- Mollenhauer, M. A. 2004. Simulator adaptation syndrome literature review. MI: Realtime technologies.
- Mourant, R. R., P. Rengarajan, D. Cox, Y. Lin, and B. K. Jaeger. 2007. “The Effect of Driving Environments on Simulator Sickness.” Human Factors and Ergonomics Society Annual Meeting Proceedings 51 (18): 1232–1236. doi:10.1177/154193120705101838.
- Mourant, R. R., and T. R. Thattacheny. 1999. “Simulator Sickness in a Virtual Environments Driving Simulator.” Proceedings of the IEA 2000/HFES 2000 Congress. 535–537.
- Mullen, N., J. Charlton, A. Devlin, and M. Bédard. 2011. “Simulator Validity: Behaviours Observed on the Simulator and on the Road.” In Handbook of Driving Simulation for Engineering, Medicine, and Psychology, edited by Donald Fisher, Matthew Rozzo, Jeff Caird, and John Lee, 13.1–13.17. Boca Raton, FL: CRC Press.
- Mullen, N. W., B. Weaver, J. A. Riendeau, L. E. Morrison, and M. Bédard. 2010. “Driving Performance and Susceptibility to Simulator Sickness: Are They related?” The American Journal of Occupational Therapy 64 (2): 288–295. doi:10.5014/ajot.64.2.288.
- Oman, C. M. 1990. “Motion sickness: a synthesis and evaluation of the sensory conflict theory.” Canadian journal of physiology and pharmacology 68 (2): 294–303.
- Prothero, J. D., M. H. Draper, T. A. Furness, D. E. Parker, and M. J. Wells. 1999. “The Use of an Independent Visual Background to Reduce Simulator Side-Effects.” Aviation, Space, and Environmental Medicine 70: 277–283.
- Prothero, J. D., Draper, M. H. T. A. Furness, Don, E. Parker, and M. J. Wells. 1997. “Do Visual Background Manipulations Reduce Simulator Sickness?” Proceedings of the International Workshop on Motion Sickness: Medical and Human Factors, 18–31. https://doi.org/10.1177/154193129503902111.
- Reason, J. T., and J. J. Brand. 1975. Motion Sickness. Oxford, England: Academic Press.
- Riccio, G. E., and T. A. Stoffregen. 1991. “An Ecological Theory of Motion Sickness and Postural Instability.” Ecological Psychology 3 (3): 195–240. doi:10.1207/s15326969eco0303_2.
- Rizzo, M., R. A. Sheffield, L. Stierman, and J. Dawson. 2003. “Demographic and Driving Performance Factors in Simulator Adaptation Syndrome.” Proceedings of the Second International Driving Symposium on Human Factors in Driver Assessment, Training and Vehicle Design, 201–208.
- Smart, L. J., T. A. Jr, Stoffregen, and B. G. Bardy. 2002. “Visually Induced Motion Sickness Predicted by Postural Instability.” Human Factors 44 (3): 451–465. doi:10.1518/0018720024497745.
- Stoffregen, T. A., C.-H. Chang, F.-C. Chen, and W.-J. Zeng. 2017. “Effects of Decades of Physical Driving on Body Movement and Motion Sickness during Virtual Driving.” PLoS One 12 (11): e0187120. doi:10.1371/journal.pone.0187120.
- Stoffregen, T. A., L. J. Hettinger, M. W. Haas, M. M. Roe, and L. J. Smart. 2000. “Postural Instability and Motion Sickness in a Fixed-Base Flight Simulator.” Human Factors: The Journal of the Human Factors and Ergonomics Society 42 (3): 458–469. doi:10.1518/001872000779698097.
- Stoffregen, T. A., and L. J. Smart. 1998. “Postural Instability Precedes Motion Sickness.” Brain Research Bulletin 47 (5): 437–448. doi:10.1016/S0361-9230(98)00102-6.
- Stoner, H. A., L. Fisher, and M. Mollenhauer Jr. 2011. “Simulator and Scenario Factors Influencing Simulator Sickness.” In Handbook of Driving Simulation for Engineering, Medicine, and Psychology, edited by D. L. Fisher, M. Rizzo, J. Caird, and J. D. Lee, 14–19. Boca Raton, FL: CRC Press.
- Teasdale, N., M. Lavalliere, M. Tremblay, D. Laurendeau, and M. Simoneau. 2009. “Multiple Expositions to a Driving Simulator Reduce Simulator Symptoms for Elderly Drivers.” Proceedings of the Fifth International Driving Symposium on Human Factors in Driver Assessment, Training, and Vehicle Design.
- Trick, L., and J. Caird. 2011. “Methodological Issues When Conducting Research On Older Drivers.” In Handbook of Driving Simulation for Engineering, Medicine, and Psychology, edited by Donald Fisher, Matthew Rozzo, Jeff Caird, and John Lee, 13.1–13.17. Boca Raton, FL: CRC Press.
- Veldstra, J. 2014. “When the Party is Over… Investigating the effects of Alcohol, THC and MDMA on Simulator Driving Performance.” PhD diss., University of Groningen.
- Zhang, L.-L., J.-Q. Wang, R.-R. Qi, L.-L. Pan, M. Li, and Y.-L. Cai. 2015. “Motion Sickness: Current Knowledge and Recent Advance.” CNS Neuroscience & Therapeutics 22 (1): 15–0. doi:10.1111/cns.12468.