Abstract
Lower extremity musculoskeletal discomfort (MSD) is prevalent, but understudied, in nurses. A comprehensive, theoretical, aetiological model of lower extremity work-related MSD in hospital in-patient staff nurses was developed through a review of the literature to provide a framework for aetiological and intervention research. The framework informed the design of a survey of 502 hospital staff nurses. Symptom prevalence ranged from 32% in hip/thigh to 59% in ankle/foot regions. Logistic regression modelling using survey data showed that different work and personal factors were associated with discomfort in different regions of the lower extremity. Individual factors (e.g. older age, higher BMI or having any foot condition), physical factors (e.g. higher frequency of patient handling), psychosocial factors (e.g. lower job satisfaction) were associated with discomfort in one or more parts of the lower extremity. Future research should target these factors for intervention, to attempt to reduce occurrence of lower extremity discomfort in nurses.
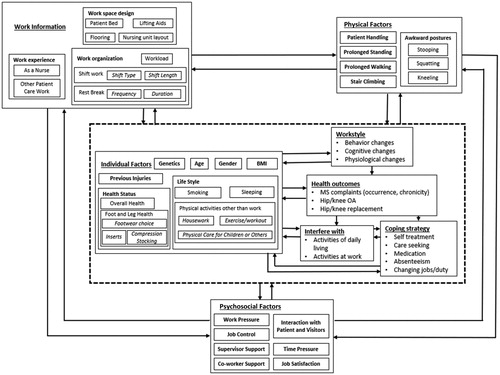
Practitioner Summary: Practitioners may find useful the illustrated, theoretical aetiological model of factors that could influence the prevalence of lower extremity discomfort in nurses. The model could guide conversations with nurses and observational analyses of nursing work. The model and survey results may provide ideas for intervention exploration.
Abbreviations: MSD: musculoskeletal discomfort; BMI: body mass index; MSK: musculoskeletal; ICU: intensive care unit; NLERF: nurses' lower extremity MSD risk factor; NASA-TLX: NASA-task load index
Introduction
Due to elevated incidence over the years, low back pain and upper extremity musculoskeletal (MSK) symptoms in nurses have been topics of great interest for occupational health researchers (Alexopoulos et al. Citation2011; Cheung et al. Citation2006; Engels et al. Citation1996; Stubbs et al. Citation1983). Davis and Kotowski’s (Citation2015) review of MSK disorder prevalence in nurses included 123 studies investigating back pain. Many administrative and engineering controls have been developed to reduce injuries to the back and shoulders caused by patient handling tasks (Nelson et al. Citation2006; Reme et al. Citation2012). Far fewer studies of nurses report on symptoms in other body regions, for example, lower extremity regions, including knee, ankle and foot (Cameron et al. Citation2008; Fochsen et al. Citation2006). That said, Stolt et al. (Citation2016) examined 35 studies from around the world (US, Europe, Asia, the Middle East, Africa, New Zealand and Australia), that focussed on lower extremity MSK disorders in nurses; a wide range of symptom prevalence was reported in those studies, from less than 10–100%.
Given our limited understanding and wide range of prevalence reports of lower extremity symptoms in nurses, there appears to be an opportunity to contribute to the knowledge base with additional research focussed on work-related and individual risk factors for symptoms in specific areas of the lower extremity, as well as intervention factors to reduce symptoms. Further, an ecological model could be useful in guiding this future research. Researchers have provided models at various levels of detail and targeting specific parts of the body to guide research into MSK symptom development (Armstrong et al. Citation1993; Barr and Barbe Citation2002; Bongers et al. Citation1993; National Academy of Sciences, Panel on Musculoskeletal Disorders and the Workplace Commission on Behavioral and Social Sciences and Education Citation2001). While Garcia, Graf, and Laubli (Citation2017) developed a multi-factor statistical model for lower limb pain in a general working population, there do not appear to be any models specifically developed to guide lower extremity MSK symptom research in nurses.
Therefore, the aims of this study were to (1) develop a conceptual model of exposure factors related to lower extremity MSK symptoms in nurses, based on the existing literature; (2) use the model to inform the collection of data on region-specific lower extremity symptoms and associated work-related and individual exposure factors in a cohort of hospital floor nurses in the USA; and (3) use statistical modelling to investigate the strength of the associations between model-informed exposure factors and symptom data.
Conceptual model
Risk factors associated with work-related MSK symptoms are generally categorised as physical, psychosocial, work organisational and individual (personal). Risk factors that may affect a nurse’s lower extremity MSK system are also likely to fall into these categories.
Physical factors
Nurses, especially those who perform bedside nursing care, spend much of their time standing and walking. Welton et al. (Citation2006) reported that registered nurses in hospital adult medical-surgical units walked almost 9000 steps during a 12-h shift. In studies involving participants from the general population or other occupations, significant associations were found between lower extremity MSK disorders (plantar fasciitis and varicose veins) or lower extremity symptoms and standing or walking for significant portions of a day (Riddle et al. Citation2003; Roelen et al. Citation2008). Stair climbing is a reported source of knee strain in general populations (Allen et al. Citation2010; Lau et al. Citation2000).
Studies have shown that patient handling tasks are associated with lower back pain and knee pain, due to the mechanical loads on the lower back and the knees experienced during those tasks (Daraiseh et al. Citation2003; Warming et al. Citation2009). In other occupations (farming and construction), hip osteoarthritis has also been associated with long term exposure to heavy lifting (Jensen Citation2008). Awkward postures that occur during nursing work, such as squatting, kneeling or stooping, can also put excessive loading on knees. The literature shows strong evidence of an association between knee MSK disorders, especially knee osteoarthritis and occupational exposures to kneeling and squatting in farming workers and construction workers (Fransen et al. Citation2011). However, this association has not been explored in nursing populations.
Psychosocial factors
Psychosocial risk factors, such as high work demand, little control over work and stress, have been found to be associated with MSK disorders of the back and upper extremity, in nurses and other work populations (Bongers et al. Citation2006; Warming et al. Citation2009). However, mixed results have been reported regarding links between psychosocial risk factors and lower extremity MSK disorders. No significant association was found between knee complaints and psychosocial factors (stress, supervisor support and work demand) in nurses (Lagerström et al. Citation1995; Warming et al. Citation2009) while in other studies leg complaints were positively associated with perceived work pressure in nurses (Engels et al. Citation1996) and lower extremity disorders were found to be associated with low job control in carpenters (Lemasters et al. Citation1998). Other psychosocial factors that are relevant to nurses’ work include interactions with patients and visitors, time pressure, co-worker support and job satisfaction (Daraiseh et al. Citation2003).
Work information
Work information includes work experience (as a nurse or other patient care work), work space design (any particular work space design that could impact the physical factors, such as patient bed, lifting aids (Pheasant and Ergs Citation1987), flooring (Cham and Redfern Citation2001), nursing unit layout (Cohen et al. Citation2004; Fay et al. Citation2017)), as well as work organisation factors (Koehoorn et al. Citation2006). Shift work, particularly shifts that occur outside of a traditional 8-h daytime schedule, can have adverse health effects on nursing personnel, both physically and psychologically (He Citation2013; Samaha et al. Citation2007). Cameron et al. (Citation2008) found that shift length, shift type and resulting sleep quality were significantly correlated with pain or discomfort in the lower extremities of older nurses. Cohen et al. (Citation2004) found that workload measures (including self-perceptions of workload and objective assessments of number of tasks and staffing ratio) were correlated to MSK injury rates in care aides and licenced practical nurses.
Individual factors
Nurses who were obese or morbidly obese were more likely to have foot/ankle MSK symptoms that limited their activity, when compared with nurses who were underweight or had normal BMI (odds ratio 4.43; Reed et al. Citation2014). Obesity has also been identified as a primary risk factor for knee osteoarthritis (Kulkarni et al. Citation2016). Other individual factors could potentially affect the nurse’s lower extremity health, including age, gender, previous injury, health status (overall and foot/leg health), footwear choice (including inserts and compression stocking; Chiu and Wang Citation2007; Kurup, Clark, and Dega Citation2012), and personal habits/behaviours and responsibilities (smoking, sleeping pattern, other physical activities other side work, such as housework, exercise/workout, physical care for children or others; Samaha et al. Citation2007).
The information presented above is a succinct summary of the extensive literature review performed for this study on four primary categories of risk factors. Through that literature review, we learned that some risk factors for lower extremity symptoms have been studied specifically in nurses, but may not have been examined for their effects in specific regions of the lower extremity or that findings for some factors have been mixed (e.g. psychosocial factors). Further, some factors found to pose problems for the lower extremity in other occupations or the general public have not been studied in nurses (e.g. awkward postures). And, finally, some factors studied in nurses and associated with MSK symptoms in other parts of the body have not been examined for associations with lower extremity symptoms (e.g. patient handling). Based on this extensive but incomplete knowledge and a desire to fill some of these knowledge gaps, a conceptual, aetiological model of development of lower extremity work-related MSK symptoms and disorders in hospital inpatient staff nurses was developed (). It stems from the existing literature and provides a framework for future research.
Workstyle
An additional factor not widely examined in the lower extremity MSK literature or nursing literature but included in this theoretical model is ‘workstyle’. Workstyle describes a worker’s response to the demands of his/her work (Feuerstein Citation1996). Among a range of responses, high levels of reactivity to work demands (high workstyle) may manifest in not taking breaks, working while in pain, and/or working in awkward postures. Workstyle has been shown to be predictive of upper extremity pain and functional limitations in computer users (Nicholas, Feuerstein, and Suchday Citation2005). Workstyle scores were found to be higher in nursing assistants who reported experiencing work-related MSK symptoms in various body parts, including parts of the lower extremity, in comparison to nursing assistants who did not report symptoms (Cheung, Ching, et al. Citation2018; Cheung, Szeto, et al. Citation2018). Given these results in nursing assistants, workstyle was also included in the new conceptual model.
Health outcomes
Studies of nurses have reported pain and discomfort in lower extremity regions, including knee, ankle and foot (Cameron et al. Citation2008; Fochsen et al. Citation2006; Stolt et al. Citation2016). Cameron et al. (Citation2008) reported more than 40% of nurses participating in their study experienced leg/foot pain that interfered ‘somewhat, quite a lot, or a great deal’ with their ability to work. The cost of musculoskeletal discomfort (MSD), in terms of extent of impairment, disability and interference with activities on or off the job has been viewed as an important outcome for many years (Kuorinka et al. Citation1987; National Academy of Sciences, Panel on Musculoskeletal Disorders and the Workplace Commission on Behavioral and Social Sciences and Education Citation2001).
Coping strategies
Another type of outcome of MSD symptoms would be coping strategies used in response to discomfort/pain. Strategies reported to be used by nurses include self-treatment, over-the-counter medication, seeking treatment from a physician or physiotherapist and taking days off (Cameron et al. Citation2008; Alexopoulos et al. Citation2011).
In the Nurses’ Lower Extremity Musculoskeletal Discomfort Risk Factor (NLERF) Model (), the hypothesised influential factors are grouped in four categories: physical factors, work organisation, psychosocial factors and individual (personal) factors. These factors could potentially influence the nurses’ workstyle by behavioural, cognitive and physiological means, and these interacting factors could influence health outcomes. The MSK symptoms and disorders might interfere with an individual’s activities at work and outside of work, and different individuals might have different strategies to cope with those outcomes. Changes in workstyle, lower extremity health, as well as the coping strategies would, in turn, affect some of the risk factors.
Using the model as a framework, data were collected via a cross-sectional survey that assessed the prevalence of lower extremity problems in acute care hospital staff nurses and gathered data on a wide range of potential risk factors. In particular, the relationships between lower extremity discomfort and various potential risk factors including physical factors, work organisational factors, psychosocial factors, workspace design factors and individual factors were explored. The study was approved by the Institutional Review Board of the authors’ university.
Methods
Participants
A total of 766 staff nurses from 19 inpatient nursing units in several hospitals in the Midwestern region of the USA were contacted during the recruiting process. A convenience sampling method was used. Efforts were made to include nurses representing different types of units (medical/surgical, intensive care unit (ICU), etc.).
Nurse lower extremity discomfort questionnaire
The questionnaire developed for this study was structured based on the NLERF Model. Subject-matter expert interviews were conducted with four nursing PhD students and one nursing researcher to help refine the questionnaire. These nursing students all had nursing experience, and some of them were also full-time practicing staff nurses or nurse practitioners. The nursing students were asked to ‘read out loud’ each question and all the response choice options, and explain how they would interpret those questions. The content and wording of the questions and response options were adjusted based on these nurses’ input. The interview with the nursing researcher was focussed on the appearance of the questionnaire (usability), such as the formatting and structure. The questionnaire was adjusted based on the nursing researcher’s input. Pilot testing of the questionnaire was conducted with two practicing nurses. The focus was to determine the length of time that a nurse would require for completing the survey.
The questionnaire included nine sections: work organisation, health status and history (including MSD, as well as systemic problems; coping strategies), individual factors, organisational factors, physical factors, psychosocial factors, workspace design and demographic information. Portions of existing validated surveys were adopted from the literature where possible, primarily for psychosocial factors and outcomes; new questions were developed where necessary. Existing surveys used included: NASA TLX workload scale (Hart and Staveland Citation1988); for psychosocial factors the survey included a work pressure scale (Carayon Citation1994; Faucett and Rempel Citation1994; Sainfort Citation1990; items were adjusted based on nursing work; included a new item on ability to mentally relax after work), job control scale (Haims Citation1999; Greenberger Citation1982; Hurrell and McLaney Citation1988; McLaney and Hurrell Citation1988), supervisor support scale (Caplan et al. Citation1975), co-worker support scale (Caplan et al. Citation1975; included new item on availability of co-worker assistance), one item on interaction with difficult patient/family (Sommerich Citation2004; this item has been adjusted based on nursing work), quantitative workload scale to assess time pressure (Quinn et al. Citation1971), facet free job satisfaction scale (Quinn et al. Citation1971); modified Nordic MSK questionnaire (Kuorinka et al. Citation1987) for MSK health outcomes and coping strategies.
Statistical analysis
Microsoft Excel, Statistical Analysis System (SAS, Cary, NC), and STATA Data Analysis and Statistical Software (College Station, TX) were used to conduct the statistical analyses. Logistic regression modelling (Hosmer, Lemeshow, and Sturdivant Citation2013) was conducted to estimate the relationship between potential risk factors and the MSK health condition of interest, which was the prevalence of lower extremity body part discomfort that interfered with normal activities (on the job or off). In preparation for the logistic regression modelling, the first step was to review the data, and for some variables, it was necessary to collapse some of the response categories due to the small number of responses in some categories. Separate models were created for the hip/thigh, knee and foot/ankle regions. Subjects with missing data were only excluded from the body part model for which data were missing. The modelling process was similar to that used by Roquelaure et al. (Citation2009). The following steps were performed in the construction of the logistic regression models for each lower extremity region:
Step 1: A univariate logistic regression model was run for each independent variable. Any independent variable not determined to be statistically significant (WALD test p-value >.20) was excluded from further analysis. If there were more than two levels for a categorical variable, the p-value of each individual level was considered and the variable was included if the p-value of any individual level was below .20.
Step 2: Each of the remaining independent variables was grouped into one of four categories (Demographic and Individual factors, Work Organisation factors, Physical factors and Psychosocial factors). For each category, backward selection multivariate logistic regression was used to select statistically significant variables within the category. Non-significant variables (p-value >.10) were excluded from further analysis. Age and Gender were forced into every model because they are potential confounders (Greenland, Daniel, and Pearce Citation2016). Then, multivariate logistic regression was used to construct a model with the remaining variables in the four categories. Variables that were not statistically significant (p-value >.10) were excluded from the final model. For each final model, coefficients, odds ratio point estimates and confidence intervals were calculated.
Prior to performing the logistic regression modelling, Cronbach’s alpha was calculated for the psychosocial scales from the questionnaire to confirm their performance in this group of respondents: NASA TLX workload (0.6462), work pressure (0.7930), job control (0.7738), supervisor support (0.9006), co-worker support (0.8773), quantitative workload (0.8349) and facet free job satisfaction (0.8204).
Results
Participant demographics
Out of the 766 nurses contacted, four declined to participate in the study during the recruiting process, thus, 762 surveys were distributed. A total of 512 surveys were collected. After examining the collected surveys, 10 were excluded for being incomplete, for the respondent not being an inpatient staff nurse, or for the respondent working multiple nursing jobs (the survey was not designed to capture exposure to multiple employment situations). A total of 502 returned surveys were used for the analysis, providing a response rate of 66%.
Eighty-four percent of respondents were female (n = 424), 15% were male (n = 74) and four did not provide information about gender. The percentage of males in the study was higher than in the U.S. nursing population (7% male) as assessed via a national survey conducted in 2013 (Budden et al. Citation2013). The mean age of the respondents was 36.4 years. Compared with the national nursing population, the average age of the participants in this study is younger (50 vs. 36.4 years; Budden et al. Citation2013). The mean BMI for the group of respondents was 27.4. This is similar to a survey of nurses in the U.S. conducted in 2007 (27.2; Miller, Alpert, and Cross Citation2008), and is slightly less than the U.S. national population means for adult females and males (29.2 and 28.7, respectively) reported by Fryar, Gu, and Ogden (Citation2012).
Prevalence of lower extremity discomfort
Percentages of respondents that experienced any discomfort in the last 12 months, the frequency of experiencing that discomfort, and the percentages of respondents whose discomfort interfered with activities on or off the job are shown in for the hip/thigh, knee, and ankle/foot regions of the lower extremity. In spite of survey pilot testing, some of the study respondents inadvertently overlooked the set of questions regarding lower extremity discomfort, thus the numbers of respondents in are smaller than the overall number of survey respondents.
Table 1. Twelve-month prevalence of lower extremity discomfort in study respondents.
Model building results
Basic summary statistics of the independent variables found to be significant during the univariate logistic regression process are provided in . The results of the model building for hip/thigh, knee and ankle/foot are shown in .
Table 2. Descriptive statistics of factors found to be significant in the univariate regression process.
Table 3. Step 1 results: potential risk factors and univariate analyses for hip/thigh discomfort that interferes with normal activities (on the job or off).
Table 4. Step 2 results: multivariate model for factors associated with hip/thigh discomfort that interferes with normal activities (on the job or off).
Table 5. Step 1 results: potential risk factors and univariate analyses for knee discomfort that interferes with normal activities (on the job or off).
Table 6. Step 2 results: multivariate model for factors associated with knee discomfort that interferes with normal activities (on the job or off).
Table 7. Step 1 results: potential risk factors and univariate analyses for foot/ankle discomfort that interferes with normal activities (on the job or off).
Table 8. Step 2 results: multivariate model for factors associated with foot/ankle discomfort that interferes with normal activities (on the job or off).
Hip/thigh discomfort modelling
In the univariate analysis (), age, BMI, having sciatic nerve pain, use of shoe inserts and more years of nursing experience were associated with hip/thigh discomfort (p < .05). Other variables retained for further analysis included smoking status (ever a smoker), frequency of exercise, having a foot condition, bending forward more frequently, using patient handling device (lifting aids) less often, lower perceived workload and lower perceived job control (p < .20). As shown in , the final multivariate model of hip/thigh discomfort included four individual factors and one work information factor. Age, BMI, having sciatic nerve pain and less frequent use of lifting aids were found to be associated with 12-month prevalence of interfering hip/thigh discomfort. Survey respondents who reported having sciatic nerve pain were more likely (OR 5.2; OR CI 2.6–10.4) to report hip/thigh discomfort that interfered with their normal activities than respondents who did not report sciatic nerve pain. Survey respondents who reported that they never or less than half of the time used patient handling device (lifting aids) were more likely (OR 1.9; CI 1.04–3.5) to report interfering hip/thigh discomfort than respondents who reported that they used lifting aids half of the time or more often.
Knee discomfort modelling
In the univariate analysis (), increasing age, higher BMI, poor reported health status, having a foot condition, use of compression stockings, more years of nursing experience, more patient handling, higher TLX workload (frustration), higher work pressure, lower job control, lower supervisor support and lower job satisfaction were significantly associated with 12-month prevalence of interfering knee discomfort (p < .05). Having more patients appears to be protective for knee discomfort, though it is important to understand that patient acuity is generally inversely related to the number of patients assigned to a nurse. Additionally, female gender, smoking status (ever a smoker), exercising more often than rarely, working on a higher acuity hospital unit, higher TLX workload (physical), higher TLX workload (effort) and more interaction with difficult patients and families were retained for further analysis (p < .20).
As shown in , the final multivariate model of knee discomfort includes four individual, one work information and one psychosocial factor. Age, having any foot condition, use of compression stockings and more patient handling were found to be associated with 12-month prevalence of interfering knee discomfort. Survey respondents who reported having any foot condition (bunions, corns and calluses, plantar warts, plantar fasciitis, flat foot, high arch or other foot conditions) were more likely (OR 1.8; CI 1.04–3.1) to report knee discomfort that interfered with their normal activities than respondents who reported no foot conditions. Survey respondents who reported wearing compression stockings were more likely (OR 2.6; CI 1.5–4.4) to report interfering knee discomfort than respondents who reported no use of compression stockings. Survey respondents who reported more frequent patient handling activities were more likely (OR 1.9; CI 1.1–3.3) to report interfering knee discomfort than respondents who reported doing less patient handling. Respondents who reported higher ratings of supervisor support tended to be less likely to report interfering knee discomfort (OR 0.7; CI 0.5–1.0).
Ankle/foot discomfort modelling
In the univariate analysis (), age, BMI, health status, foot condition, having sciatic nerve pain, use of shoe inserts, more years of nursing experience, less use of patient handling devices (lifting aids), greater work pressure, greater time pressure and lower job satisfaction were significantly associated with ankle/foot discomfort (p < .05). Additionally, female gender, providing physical care for teenage/adult, performing housework more often, higher quality of sleep, working day shift, higher TLX workload (temporal), higher TLX workload (frustration) and lower job control were retained for further analysis (p < .20).
As shown in , the final multivariate model for 12-month prevalence of interfering ankle/foot discomfort includes seven independent variables. BMI, having any foot condition, greater likelihood of using any type of lifting aid and low job satisfaction were found to be associated with interfering ankle/foot discomfort. Survey respondents who reported having any foot condition were more likely (OR 3.2; CI 1.8–5.7) to report ankle/foot discomfort that interfered with their normal activities than respondents who reported no foot conditions. Survey respondents who reported using patient handling devices (lifting aids) half or less than half the time were less likely (OR 0.48; CI 0.27–0.87) to report interfering ankle/foot discomfort than respondents who reported always using lifting device or using them more than half of the time. Survey respondents who reported high job satisfaction were less likely (OR 0.72; CI 0.56–0.92) to report interfering ankle/foot discomfort than respondents who reported low job satisfaction. Respondents who were older or reported use of shoe inserts tended to be more likely to report interfering ankle/foot discomfort (OR 1.02; CI 1.0–1.05 and OR 1.7; CI 0.9–3.0, respectively).
All three multivariate models (hip/thigh, knee and ankle/foot) were determined to be acceptable, with areas under the receiver operating characteristic (ROC) curve of 0.747, 0.698 and 0.755, respectively. After performing goodness-of-fit tests, the p-values were 0.7654, 0.9790 and 0.3690.
Discussion
This study used a new framework for examining the relationship between work, psychosocial and individual factors and the prevalence of lower extremity MSD in hospital staff nurses. Specifically, logistic regression models were constructed from survey data that documented the prevalence of lower extremity MSD severe enough to interfere with activities on or off the job. The results are consistent with other studies showing elevated prevalence of lower extremity discomfort in hospital staff nurses (Anap, Iyer, and Rao Citation2013; Attar Citation2014; Attarchi et al. Citation2014). The prevalence of MSK discomfort in the lower extremities in nurses reported by other researchers ranges from less than 10–100% (Alexopoulos et al. Citation2011; Attar Citation2014; Botha and Bridger Citation1998; Cameron et al. Citation2008; Choobineh et al. Citation2010; Daraiseh et al. Citation2003; Davis and Kotowski Citation2015; Kee and Seo Citation2007; Stolt et al. Citation2016). It was particularly concerning to see that two-thirds of the nurses in this study who reported foot/ankle discomfort experienced it daily or on most days that they work. Percentages were lower for those with hip/thigh or knee discomfort, but still showed that well over one-third of nurses reporting discomfort were working while experiencing pain in those areas (46 and 37%, respectively).
Individual factors
In this study, increasing age was associated with interfering hip/thigh and knee discomfort; greater BMI was associated with interfering hip/thigh and ankle/foot discomfort; having any foot condition was associated with interfering knee and ankle/foot discomfort. This is consistent with other research on nurses (Nealy et al. Citation2012). Interestingly, gender was not a significant factor in the final model for any of the parts of the lower extremity. Choobineh et al. (Citation2010) also found no differences in hip/thigh or knee MSK prevalence in male and female operating room nurses, but female nurses had a higher prevalence of foot/ankle pain.
Physical factors
Greater frequency of patient handling was associated with knee discomfort and less frequent use of patient handling device (lifting aids) was associated with hip/thigh discomfort in this study. Researchers have found that patient handling tasks are associated with knee pain due to the mechanical loads on the knees during patient handling tasks (Daraiseh et al. Citation2010; Marras et al. Citation1999). Interestingly, in this study, more frequent use of lifting devices was associated with foot/ankle discomfort; this result needs to be investigated further, as it is contrary to the association with hip/thigh discomfort and to what would be hypothesised.
Psychosocial factors
Lower job satisfaction and lower supervisor support were associated with interfering ankle/foot and knee discomfort, respectively, in this study. In a prior study of nurses, lower job satisfaction was associated with knee pain (Arsalani et al. Citation2014), while lower supervisor support was associated with hip/thigh discomfort (Erick and Smith Citation2014) and lower limb discomfort (Seifert, Messing, and Dumais Citation1997) in studies of other professions (teachers in developing countries and bank employees, respectively). No other psychosocial factors were found to be associated with lower extremity discomfort in this study. In contrast, an earlier study by Engels et al. (Citation1996) found a high work pace and work interruptions were associated with leg discomfort in nurses working in nursing homes.
Work organisation
None of the work organisation or work experience factors were associated with lower extremity discomfort in the final models, though in the univariate analyses working night shift appeared to have a protective effect for each of the lower extremity regions. As a point of comparison, a 2012 study reported that working rotating night shifts was linked to varicose veins in a sample of middle age nurses and midwives (Burdelak et al. Citation2012). Length of shift could not be investigated in this study for association with lower extremity discomfort, because almost all survey respondents worked 12-h shifts.
In this study, we attempted with several questions on the survey, to ask about different aspects of workload, including self-reported quantitative workload, NASA TLX workload rating scales and self-reported work pressure (scale included questions on understaffing and perceptions of patient load and acuity), and overtime. Overtime did not make it through the first step of the statistical analysis, and the other variables were not retained in any of the three final models. In the study conducted by Cohen et al. (Citation2004) workload was objectively quantified by resident-staff ratio and resident dependency-staff ratio, and these were found to correspond to MSK injury rates. In that study perceived workload was significantly correlated with resident dependency-staff ratio, but perceived workload was not associated with injury rates. As such, Cohen et al. demonstrated the value of measuring workload, rather than relying on worker perceptions. Results from this study are consistent with those of Cohen et al. showing that nurses’ perceptions about workload were not strongly associated with more serious MSK outcome measures.
Several questions in the survey pertained to the workstyle construct, such as taking (or not taking) breaks and working while in pain/discomfort. About 20% of participants did not take a mid-shift meal break, but only took short/brief breaks, although their shifts were 12 h long. Another 20% only took a mid-shift meal break, but no other breaks in their 12-h shifts. While this way of characterising breaks did not turn out to be associated with lower extremity discomfort, working for extended periods without sufficient breaks remains an area of concern. It is also unknown whether lower extremity discomfort would be associated with workstyle, as assessed by the workstyle questionnaire developed by Feuerstein (Citation1996) (original or short form). Future studies could include the workstyle questionnaire instrument when investigating lower extremity discomfort in nursing populations, to provide a more complete picture of the relationship between workstyle and lower extremity discomfort.
In this study, the lower extremity was divided into three regions, in contrast to some other studies where the lower extremity was investigated as a single unit. The analysis from this cross-sectional study showed that discomfort in the three different regions was associated with different factors. Interfering hip/thigh discomfort was associated with age, BMI, having sciatic nerve pain and less frequent use of lifting aids; interfering knee discomfort was associated with age, having any foot condition, use of compression stockings, more patient handling and less supervisor support; and interfering foot/ankle discomfort was associated with age, BMI, having any foot condition, use of shoe inserts, greater likelihood of using lifting aids and lower job satisfaction. Thus, looking at the three regions separately proved to be beneficial, and provided more insights in the model building process. When considering interventions to reduce MSK discomfort in nurses, the intervention could be more targeted to a specific region, priority could be given to interventions that target more than one region of the lower extremity, or it could be recognised if multiple interventions were to be initiated that each part of the lower extremity was being addressed by at least one of the interventions.
An important strength of the study was the strong response rate (over 60%). A key factor in this was the hands-on approach to participant recruitment. Each potential participant was personally invited, in a face-to-face conversation, to participate in the study. During the recruitment process each potential participant was handed a paper survey and a $5 bill as an incentive. The goal of providing the incentive at the time of recruitment is to establish trust between the researcher and the potential participant (Dillman, Smyth, and Christian Citation2008) and the paper survey served as a physical reminder of the survey. Lockboxes for depositing completed surveys were conveniently located in the break room of each unit and also served as visual reminders to complete the survey.
There are some limitations to this study. First, this was a cross-sectional study. As such, the effects of some of the ergonomics practices (such as the use of lifting devices) cannot be determined from the study results. Some nurses could have adopted some work practices proactively, to try to prevent development of MSK discomfort, while others could have adopted the same work practices reactively, to ameliorate symptoms. As such, whether or not the association between a work practice and MSK discomfort is causal cannot be established. Follow-up interviews with survey participants could be useful to determine which work practices may be effective in preventing or ameliorating MSK discomfort. Further, as with any cross-sectional study, participants may represent ‘survivors’, where more vulnerable people already chose to leave the job. For example, we discovered through a later conversation with one of the study participants, that the individual had left the inpatient hospital staff nurse position held during the survey and had taken a less physically demanding job a few months after the survey was conducted, due to persistent knee problems. Another limitation was that the foot and ankle were not examined separately in the survey, nor were different parts of the foot, all of which could potentially provide more detailed insights. Another limitation of the study is that in the logistic regression modelling process, other than ‘foot conditions’, potential associations between pain in different regions of the lower extremity were not examined. One more limitation was that in spite of iterative testing and modification during pilot testing, about 10% of participants did not provide responses to questions about lower extremity discomfort, due to a survey design oversight. Lastly, a broad range of patient handling aids was grouped together (gait belt, portable floor lift, ceiling lift, stand assist device and slide board) in one of the questions. Breaking them out might have yielded more useful information.
Conclusions
Lower extremity MSK discomfort is prevalent in nurses. This study makes a contribution to the knowledge base, by proposing an ecological model to further the understanding of the range of factors that could influence the lower extremity health of nurses. The model is based on an extensive review of the literature on lower extremity MSK disorders; it includes physical, work organisational, psychosocial and individual factors reported or hypothesised to be associated with lower extremity MSK discomfort in nurses. The model provides a new framework for further aetiological and interventional research to address the prevalence of lower extremity discomfort experienced in hospital staff nurses. Analysis of data from a survey of nurses, based on the new ecological model, verified that individual (e.g. older age, higher BMI or having any foot condition) and work environment factors (physical factors, e.g. higher frequency of patient handling; psychosocial factors, e.g. lower job satisfaction and supervisor support) were associated with lower extremity discomfort in one or more parts of the lower extremity. Prior to making recommendations to modify the new model, findings should be examined from additional studies based on the model, including those that employ different study designs.
Researchers and practitioners may be able to use the findings of this study to improve (reduce) nurses’ experience with lower extremity MSD. They could use the new model to raise awareness of factors that have been associated with lower extremity MSDs in other studies (some in nurses and some in other work or general populations), and to investigate and attempt to address those factors in their own nursing populations. Consistent with prior reports concerning nurses (Stolt et al. Citation2016), BMI was associated with lower extremity discomfort in this study (in the hip/thigh and foot/ankle). Some studies have shown that workplace weight loss programmes can be effective, resulting in weight loss and other health benefits (Pritchard, Nowson, and Billington Citation2002; Nahm, Warren, and Friedmann Citation2014); such an intervention would have the potential to also have a positive effect on nurses’ lower extremity discomfort. In this study, foot conditions were associated with knee and foot/ankle discomfort. Foot health and care for feet is important for nurses’ health and for career viability. Stolt et al. (Citation2018) reported on nurses’ perceptions of foot health, including factors that promote or hinder foot health and ways employers could support foot health (e.g. in-service education on foot self-care, selection of proper footwear and use of compression stockings; regular foot assessment and treatment if needed; and considering ways to reduce nurses’ time on feet). This study also found that more positive perceptions of supervisor support and job satisfaction were associated with lower likelihood of reporting interfering knee and foot/ankle discomfort, respectively. Efforts that aim to improve these perceptions of work could have an effect on lower extremity discomfort and other positive consequences (e.g. improved nurse retention and patient satisfaction (Stordeur et al. Citation2003)). Statistical modelling also identified higher frequency of patient handling and using patient-handling devices less often when handling patients as being associated with reporting interfering discomfort in the knee and hip/thigh, respectively. Efforts to reduce manual patient handling could have a positive effect on lower extremity discomfort, as well as other benefits (e.g. reducing injury rates, reducing lost work days and increase in job satisfaction (Nelson et al. Citation2006); improved employee retention and patient care (Celona Citation2010; Thomas, Celona, and Matz Citation2010)). As such, researchers and practitioners could use the new aetiological model and the findings from this study, in combination with research findings from relevant intervention studies, to positively affect the work life and health of their nursing populations.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Alexopoulos, E. C., D. Tanagra, I. Detorakis, P. Gatsi, A. Goroyia, M. Michalopoulou, and E. Jelastopulu. 2011. “Knee and Low Back Complaints in Professional Hospital Nurses: Occurrence, Chronicity, Care Seeking and Absenteeism.” Work 38 (4): 329–335. doi:10.3233/WOR-2011-1136.
- Allen, K. D., J. C. Chen, L. F. Callahan, Y. M. Golightly, C. G. Helmick, J. B. Renner, and J. M. Jordan. 2010. “Associations of Occupational Tasks with Knee and Hip Osteoarthritis: The Johnston County Osteoarthritis Project.” The Journal of Rheumatology 37 (4): 842–850. doi:10.3899/jrheum.090302.
- Anap, D., C. Iyer, and K. Rao. 2013. “Work Related Musculoskeletal Disorders Among Hospital Nurses in Rural Maharashtra, India: A Multi Centre Survey.” International Journal of Research in Medical Sciences 1 (2): 101. doi:10.5455/2320-6012.ijrms20130513.
- Armstrong, T. J., P. Buckle, L. J. Fine, M. Hagberg, B. Jonsson, A. Kilbom, I. A. Kuorinka, B. A. Silverstein, G. Sjogaard, and E. R. Viikari-Juntura. 1993. “A Conceptual Model for Work-Related Neck and Upper-Limb Musculoskeletal Disorders.” Scandinavian Journal of Work, Environment & Health 19 (2): 73–84. doi:10.5271/sjweh.1494.
- Arsalani, N., M. Fallahi-Khoshknab, M. Josephson, and M. Lagerström. 2014. “Musculoskeletal Disorders and Working Conditions among Iranian Nursing Personnel Musculoskeletal Disorders and Working Conditions among Iranian Nursing Personnel.” International Journal of Occupational Safety and Ergonomics 20 (4): 671–680. doi:10.1080/10803548.2014.11077073.
- Attar, S. M. 2014. “Frequency and Risk Factors of Musculoskeletal Pain in Nurses at a Tertiary Centre in Jeddah, Saudi Arabia: A Cross Sectional Study.” BMC Research Notes 7 (1): 61. doi:10.1186/1756-0500-7-61.
- Attarchi, M., S. Raeisi, M. Namvar, and M. Golabadi. 2014. “Association between Shift Working and Musculoskeletal Symptoms among Nursing Personnel.” Iranian Journal of Nursing and Midwifery Research 19 (3): 309–314.
- Barr, A. E., and M. F. Barbe. 2002. “Pathophysiological Tissue Changes Associated with Repetitive Movement: A Review of the Evidence.” Physical Therapy 82 (2): 173–187. doi:10.1093/ptj/82.2.173.
- Bongers, P. M., C. R. De Winter, M. A. J. Kompier, H. Vincent, and V. H. Hildebrandt. 1993. “Psychosocial Factors at Work and Musculoskeletal Disease.” Scandinavian Journal of Work, Environment & Health 19 (5): 297–312. doi:10.5271/sjweh.1470.
- Bongers, P. M., S. Ijmker, S. van den Heuvel, and B. M. Blatter. 2006. “Epidemiology of Work Related Neck and Upper Limb Problems: Psychosocial and Personal Risk Factors (Part I) and Effective Interventions from a Bio Behavioural Perspective (Part II).” Journal of Occupational Rehabilitation 16 (3): 279–302. doi:10.1007/s10926-006-9044-1.
- Botha, W. E., and R. S. Bridger. 1998. “Anthropometric Variability, Equipment Usability and Musculoskeletal Pain in a Group of Nurses in the Western Cape.” Applied Ergonomics 29 (6): 481–490. doi:10.1016/S0003-6870(97)00081-1.
- Budden, J. S., E. H. Zhong, P. Moulton, and J. Cimiotti. 2013. “Highlights of the National Workforce Survey of Registered Nurses.” Journal of Nursing Regulation 4 (2): 5–14. doi:10.1016/S2155-8256(15)30151-4.
- Burdelak, W., A. Bukowska, J. Krysicka, and B. Pepłońska. 2012. “Night Work and Health Status of Nurses and Midwives. Cross-Sectional Study.” Medycyna Pracy 63 (5): 517–529.
- Cameron, S. J., M. Armstrong-Stassen, D. Kane, and F. B. P. Moro. 2008. “Musculoskeletal Problems Experienced by Older Nurses in Hospital Settings.” Nursing Forum 43 (2): 103–114. doi:10.1111/j.1744-6198.2008.00101.x.
- Caplan, R. D., S. Cobb, J. R. P. P. French, R. Van Harrison, and S. R. R. Pinneau. 1975. Job Demands and Worker Health: Main Effects and Occupational Differences, 342. Washington, DC: US Department of Health, Education, and Welfare.
- Carayon, P. 1994. “Stressful Jobs and Non-Stressful Jobs: A Cluster Analysis of Office Jobs.” Ergonomics 37 (2): 311–323. doi:10.1080/00140139408963648.
- Celona, J. N. 2010. “Establishing the Business Case—Understanding and Increasing the Value of a PHAMP at Your Institution.” In Patient Handling and Movement Assessments: A White Paper, edited by C. M. Borden, 45–57. Boca Raton, FL: The Facility Guidelines Institute.
- Cham, R., and M. S. Redfern. 2001. “Effect of Flooring on Standing Comfort and Fatigue.” Human Factors 43 (3): 381–391. doi:10.1518/001872001775898205.
- Cheung, K., S. S. Y. Ching, K. Y. Ma, and G. Szeto. 2018. “Psychometric Evaluation of Theworkstyle Short Form among Nursing Assistants With Work-Related Musculoskeletal Symptoms.” International Journal of Environmental Research and Public Health 15 (4): 823. doi:10.3390/ijerph15040823.
- Cheung, K., M. Gillen, J. Faucett, and N. Krause. 2006. “The Prevalence of and Risk Factors for Back Pain among Home Care Nursing Personnel in Hong Kong.” American Journal of Industrial Medicine 49 (1): 14–22. doi:10.1002/ajim.20243.
- Cheung, K., G. Szeto, G. Lai, and S. Ching. 2018. “Prevalence of and Factors Associated with Work-Related Musculoskeletal Symptoms in Nursing Assistants Working in Nursing Homes.” International Journal of Environmental Research and Public Health 15 (2): 265. doi:10.3390/ijerph15020265.
- Chiu, M. C., and M. J. J. Wang. 2007. “Professional Footwear Evaluation for Clinical Nurses.” Applied Ergonomics 38 (2): 133–141. doi:10.1016/j.apergo.2006.03.012.
- Choobineh, A., M. Movahed, S. H. Tabatabaie, and M. Kumashiro. 2010. “Perceived Demands and Musculoskeletal Disorders in Operating Room Nurses of Shiraz City Hospitals.” Industrial Health 48 (1): 74–84. doi:10.2486/indhealth.48.74.
- Cohen, M., J. Village, A. S. Ostry, P. A. Ratner, Y. Cvitkovich, and A. Yassi. 2004. “Workload As a Determinant of Staff Injury in Intermediate Care.” International Journal of Occupational and Environmental Health 10 (4): 375–383. doi:10.1179/oeh.2004.10.4.375.
- Daraiseh, N., A. M. Genaidy, W. Karwowski, L. S. Davis, J. Stambough, and R. I. Huston. 2003. “Musculoskeletal Outcomes in Multiple Body Regions and Work Effects among Nurses: The Effects of Stressful and Stimulating Working Conditions.” Ergonomics 46 (12): 1178–1199. doi:10.1080/0014013031000139509.
- Daraiseh, N. M., S. N. Cronin, L. S. Davis, R. L. Shell, and W. Karwowski. 2010. “Low Back Symptoms Among Hospital Nurses, Associations to Individual Factors and Pain in Multiple Body Regions.” International Journal of Industrial Ergonomics 40 (1): 19–24. doi:10.1016/j.ergon.2009.11.004.
- Davis, K. G., and S. E. Kotowski. 2015. “Prevalence of Musculoskeletal Disorders for Nurses in Hospitals, Long-Term Care Facilities, and Home Health Care: A Comprehensive Review.” Human Factors 57 (5): 754–792. doi:10.1177/0018720815581933.
- Dillman, D. A., J. D. Smyth, and L. M. Christian. 2008. Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method. 3rd ed. Hoboken, NJ: John Wiley & Sons, Inc.
- Engels, J., Van Der Gulden, J., Senden T. F. and Hof, B. V. 1996. “Work Related Risk Factors for Musculoskeletal Complaints in the Nursing Profession: Results of a Questionnaire Survey.” Occupational and Environmental Medicine 53 (9): 636–641. doi:10.1136/oem.53.9.636.
- Erick, P. N., and D. R. Smith. 2014. “Occupational Medicine & Health Affairs the Prevalence and Risk Factors for Musculoskeletal Disorders among School Teachers in Botswana.” Occupationl Medicine and Health Affairs 2: 178. 10.4172/2329-6879.1000178.
- Faucett, J., and D. Rempel. 1994. “VDT- Related Musculoskeletal Symptoms: Interactions Between Work Posture and Psychosocial Work Factors.” American Journal of Industrial Medicine 26 (5): 597–612. doi:10.1002/ajim.4700260503.
- Fay, L., A. Carll-White, A. Schadler, K. B. Isaacs, and K. Real. 2017. “Shifting Landscapes: The Impact of Centralized and Decentralized Nursing Station Models on the Efficiency of Care.” Herd 10 (5): 80–94. doi:10.1177/1937586717698812.
- Feuerstein, M. 1996. “Workstyle: Definition, Empirical Support and Implications for Prevention, Evaluation and Rehabilitation of Occupational Upper Extremity Disorders.” In Beyond Biomechanics: Psychosocial Aspects of Musculoskeletal Disorders in Office Work, edited by S. Sauter and S. D. Moon, 177–206. Boca Raton, FL: CRC Press.
- Fochsen, G., M. Josephson, M. Hagberg, A. Toomingas, and M. Lagerström. 2006. “Predictors of Leaving Nursing Care: A Longitudinal Study among Swedish Nursing Personnel.” Occupational and Environmental Medicine 63 (3): 198–201. doi:10.1136/oem.2005.021956.
- Fransen, M., M. Agaliotis, L. Bridgett, and M. G. Mackey. 2011. “Hip and Knee Pain: Role of Occupational Factors.” Best Practice & Research. Clinical Rheumatology 25 (1): 81–101. doi:10.1016/j.berh.2011.01.012.
- Fryar, C. D., Q. Gu, and C. L. Ogden. 2012. “Anthropometric Reference Data for Children and Adults: United States, 2007–2010.” Vital and health statistics. Series 11, Data from the national health survey. doi:10.1186/1471-2431-8-10.
- Garcia, M.-G., M. Graf, and T. Laubli. 2017. “Lower Limb Pain among Workers: A cross-sectional analysis of the fifth European Working Conditions Survey.” International Archives of Occupational and Environmental Health 90 (7): 575–585. doi:10.1007/s00420-017-1220-4.
- Greenberger, D. B. 1982. Personal Control at Work: Its Conceptualization and Measurement. Madison, WI: University of Wisconsin.
- Greenland, S., R. Daniel, and N. Pearce. 2016. “Outcome Modelling Strategies in Epidemiology: Traditional Methods and Basic alternatives.” International Journal of Epidemiology 45 (2): 565–575. doi:10.1093/ije/dyw040.
- Haims M. C. 1999. “A Longitudinal Study of the Process & Content of a Participatory Work Organization Intervention.” Unpublished dissertation, University of Wisconsin.
- Hart, S. G., and L. E. Staveland. 1988. “Development of NASA-TLX (Task Load Index): Results of Empirical and Theoretical Research.” Advances in Psychology 52 (C): 139–183. 10.1016/S0166-4115(08)62386-9.
- He, C. 2013. “Physical and Psychosocial Demands on Shift Work in Nursing Homes.” PhD Thesis, University of Cincinnati.
- Hosmer, D. W., S. Lemeshow, and R. X. Sturdivant. 2013. Applied Logistic Regression, 3rd ed. Hoboken, NJ: Wiley Series in Probability and Satistics.
- Hurrell, J. J., and M. A. Mclaney. 1988. “Exposure to Job Stress — a New Psychometric Instrument.” Scandinavian Journal of Work, Environment & Health 14 (1): 4–6.
- Jensen, L. 2008. “Hip Osteoarthritis: Influence of Work with Heavy-Lifting, Kneeling, Climbing Stairs or Ladders, or Combining Kneeling/Squatting with Heavy Lifting.” Occupational and Environmental Medicine 65 (1): 6–19. doi:10.1136/oem.2006.032409.
- Kee, D., and S. R. Seo. 2007. “Musculoskeletal Disorders among Nursing Personnel in Korea.” International Journal of Industrial Ergonomics 37 (3): 207–212. doi:10.1016/j.ergon.2006.10.020.
- Koehoorn, M., P. A. Demers, C. Hertzman, J. Village, and S. M. Kennedy. 2006. “Work Organization and Musculoskeletal Injuries Among a Cohort of Health Care Workers.” Scandinavian Journal of Work, Environment & Health 32 (4): 285–293. doi:10.5271/sjweh.1012.
- Kulkarni, K., T. Karssiens, V. Kumar, and H. Pandit. 2016. “Obesity and Osteoarthritis.” Maturitas 89: 22–28. doi:10.1016/j.maturitas.2016.04.006.
- Kuorinka, I., B. Jonsson, A. Kilbom, H. Vinterberg, F. Biering-Sørensen, G. Andersson, and K. Jørgensen. 1987. “Standardised Nordic Questionnaires for the Analysis of Musculoskeletal Symptoms.” Applied Ergonomics 18 (3): 233–237. doi:10.1016/0003-6870(87)90010-X.
- Kurup, H. V., C. I. M. Clark, and R. K. Dega. 2012. “Footwear and Orthopaedics.” Foot and Ankle Surgery: Official Journal of the European Society of Foot and Ankle Surgeons 18 (2): 79–83. doi:10.1016/j.fas.2011.03.012.
- Lagerström, M., M. Wenemark, M. Hagberg, and E. W. Hjelm. 1995. “Occupational and Individual Factors Related to Musculoskeletal Symptoms in Five Body Regions among Swedish Nursing Personnel.” International Archives of Occupational and Environmental Health 68 (1): 27–35. doi:10.1007/BF01831630.
- Lau, E. C., C. Cooper, D. Lam, V. N. Chan, K. K. Tsang, and A. Sham. 2000. “Factors Associated with Osteoarthritis of the Hip and Knee in Hong Kong Chinese: obesity, Joint Injury, and Occupational Activities.” American Journal of Epidemiology 152 (9): 855–862. doi:10.1093/aje/152.9.855.
- Lemasters, G. K., M. R. Atterbury, A. D. Booth-Jones, A. Bhattacharya, N. Ollila-Glenn, C. Forrester, and L. Forst. 1998. “Prevalence of Work Related Musculoskeletal Disorders in Active Union Carpenters.” Occupational and Environmental Medicine 55 (6): 421–427. doi:10.1136/oem.55.6.421.
- Marras, W. S., K. G. Davis, B. C. Kirking, and P. K. Bertsche. 1999. “A Comprehensive Analysis of Low-Back Disorder Risk and Spinal Loading during the Transferring and Repositioning of Patients Using Different Techniques.” Ergonomics 42 (7): 904–926. doi:10.1080/001401399185207.
- Mclaney, M. A., and J. J. Hurrell. 1988. “Control, Stress, and Job Satisfaction in Canadian Nurses.” Work & Stress 2 (3): 217–224. doi:10.1080/02678378808259169.
- Miller, S. K., P. T. Alpert, and C. L. Cross. 2008. “Overweight and Obesity in Nurses, Advanced Practice Nurses, and Nurse Educators.” Journal of the American Academy of Nurse Practitioners 20 (5): 259–265. doi:10.1111/j.1745-7599.2008.00319.x.
- Nahm, E. S., J. Warren, and E. Friedmann. 2014. “Implementation of a Participant-Centered Weight Management Program for Older Nurses: A Feasibility Study.” Online Journal of Issues in Nursing 19 (3): MS4.
- National Academy of Sciences, Panel on Musculoskeletal Disorders and the Workplace Commission on Behavioral and Social Sciences and Education. 2001. Musculoskeletal Disorders and the Workplace: Low Back and Upper Extremities. Washington, DC: National Academy Press.
- Nealy, R., C. McCaskill, M. R. Conaway, and S. M. Burns. 2012. “The Aching Feet of Nurses: An Exploratory Study.” Medsurg Nursing: Official Journal of the Academy of Medical-Surgical Nurses 21 (6): 354–359. doi:10.1016/S0047-2352(99)00013-6.
- Nelson, A., M. Matz, F. Chen, K. Siddharthan, J. Lloyd, and G. Fragala. 2006. “Development and Evaluation of a Multifaceted Ergonomics Program to Prevent Injuries Associated with Patient Handling Tasks.” International Journal of Nursing Studies 43 (6): 717–733. doi:10.1016/j.ijnurstu.2005.09.004.
- Nicholas, R. A., M. Feuerstein, and S. Suchday. 2005. “Workstyle and Upper-Extremity Symptoms: A Biobehavioral Perspective.” Journal of Occupational and Environmental Medicine 47 (4): 352–361. doi:10.1097/01.jom.0000158705.50563.4c.
- Pheasant, S., and F. Ergs. 1987. “Some Anthropometric Aspects of Workstation Design.” International Journal of Nursing Studies 24 (4): 291–298. doi:10.1016/0020-7489(87)90021-6.
- Pritchard, J. E., C. A. Nowson, and T. Billington. 2002. “Benefits of a Year-Long Workplace Weight Loss Program on Cardiovascular Risk Factors.” Nutrition & Dietetics 59 (2): 87–96.
- Quinn, R., S. Seashore, R. Kahn, T. Mangion, D. Cambell, G. Staines, and M. McCullough. 1971. Survey of Working Conditions: Final Report on Univariate and Bivariate Tables. Washington, DC: US Government Printing Office.
- Reed, L. F., D. Battistutta, J. Young, and B. Newman. 2014. “Prevalence and Risk Factors for Foot and Ankle Musculoskeletal Disorders Experienced by Nurses.” BMC Musculoskeletal Disorders 15 (1): 196. doi:10.1186/1471-2474-15-196.
- Reme, S. E., J. T. Dennerlein, D. Hashimoto, and G. Sorensen. 2012. “Musculoskeletal Pain and Psychological Distress in Hospital Patient Care Workers.” Journal of Occupational Rehabilitation 22 (4): 503–510. doi:10.1007/s10926-012-9361-5.
- Riddle, D. L., M. Pulisic, P. Pidcoe, and R. E. Johnson. 2003. “Risk Factors for Plantar Fasciitis: A Matched Case-Control Study.” The Journal of Bone and Joint Surgery-American Volume 85 (5): 872–877. doi:10.2106/00004623-200305000-00015.
- Roelen, C. A. M., K. J. Schreuder, P. C. Koopmans, and J. W. Groothoff. 2008. “Perceived Job Demands Relate to Self-Reported Health Complaints.” Occupational Medicine 58 (1): 58–63. doi:10.1093/occmed/kqm134.
- Roquelaure, Y., C. Ha, C. Rouillon, N. Fouquet, A. Leclerc, A. Descatha, A. Touranchet, M. Goldberg, and E. Imbernon. 2009. “Risk Factors for Upper-Extremity Musculoskeletal Disorders in the Working Population.” Arthritis & Rheumatism 61 (10): 1425–1434. doi:10.1002/art.24740.
- Sainfort, P. C. 1990. “Work Environment and Psychological Categories of Office.” Proceedings of the Human Factors Society Annual Meeting 34 (12): 849–853. doi:10.1177/154193129003401205.
- Samaha, E., S. Lal, N. Samaha, and J. Wyndham. 2007. “Psychological, Lifestyle and Coping Contributors to Chronic Fatigue in Shift-Worker Nurses.” Journal of Advanced Nursing 59 (3): 221–232. doi:10.1111/j.1365-2648.2007.04338.x.
- Seifert, M., K. Messing, and L. Dumais. 1997. “Star Wars and Strategic Defense Initiatives: Work Activity and Health Symptoms of Unionized Bank Tellers during Work Reorganization.” International Journal of Health Services: Planning, Administration, Evaluation 27 (3): 455–477. doi:10.2190/7KUK-2D4L-0G1N-8DNY.
- Sommerich, C. M. 2004. “Ergonomics Assessment Methodology for Work-Worker Systems: Final Progress Report.” Niosh K01 Oh00016901. Columbus, OH: NIOSH.
- Stolt, M., M. Miikkola, R. Suhonen, and H. Leino-Kilpi. 2018. “Nurses’ Perceptions of Their Foot Health: Implications for Occupational Health Care.” Workplace Health & Safety 66 (3): 136–143. doi:10.1177/2165079917727011.
- Stolt, M., R. Suhonen, P. Virolainen, and H. Leino-Kilpi. 2016. “Lower Extremity Musculoskeletal Disorders in Nurses: A Narrative Literature Review.” Scandinavian Journal of Public Health 44 (1): 106–115. doi:10.1177/1403494815602989.
- Stordeur, S., W. D’hoore, B. van der Heijden, M. Dibisceglie, M. Laine, and E. van der Schoot. 2003. “Leadership, Job Satisfaction and Nurses’ Commitment.” In Working Conditions and Intent to Leave the Profession among Nursing Staff in Europe, edited by H. M. Hasselhorn, P. Tackenberg, and B. H. Müller, 28–45. Wuppertal, Germany: University of Wuppertal.
- Stubbs, D. A., P. W. Buckle, M. P. Hudson, P. M. Rivers, and C. J. Worringham. 1983. “Back Pain in the Nursing Profession I. Epidemiology and Pilot Methodology.” Ergonomics 26 (8): 755–765. doi:10.1080/00140138308963397.
- Thomas, P., J. N. Celona, and M. W. Matz. 2010. “Part 1. Establishing the Business Case for a Patient Handling and Movement Program.” In Patient Handling and Movement Assessments: A White Paper edited by C. M. Borden, 42–44. Dallas, TX: The Facility Guidelines Institute.
- Warming, S., D. H. Precht, P. Suadicani, and N. E. Ebbehøj. 2009. “Musculoskeletal Complaints among Nurses Related to Patient Handling Tasks and Psychosocial Factors-Based on Logbook Registrations.” Applied Ergonomics 40 (4): 569–576. doi:10.1016/j.apergo.2008.04.021.
- Welton, J. M., M. Decker, J. Adam, and L. Zone-Smith. 2006. “How Far Do Nurses Walk?” Medical-Surgical Nurses: Official Journal of the Academy of Medical-Surgical Nurses 15 (4): 213–216.