Abstract
Altitude hypoxia episodes are increasingly common in military aviation. Hypoxia training is mandatory for fighter pilots, but evidence-based data on the effects of training are scarce. The purpose of this study was to validate the normobaric hypoxia (NH) training effect. Data were collected from 89 pilots from the Finnish Air Force (FINAF). This survey was conducted in a tactical F/A-18C Hornet simulator in two sessions under normobaric conditions, in which the pilots performed flight missions and breathed 21% oxygen (O2) in nitrogen (N2), and blinded to the pilot, the breathing gas was changed to a hypoxic mixture containing either 8, 7 or 6% O2 in N2. The time taken to notice hypoxia symptoms and peripheral capillary O2 saturation was measured. A mean of 2.4 years after the initial training, pilots recognised their hypoxic symptoms 18 s quicker with 8% O2 mixture, 20 s quicker with 7% O2 and 10 s quicker with 6% O2. Our data indicate that NH training in a flight simulator helps pilots to recognise hypoxia symptoms earlier, and may, thus, enhance flight safety.
Practitioner Summary: We show that hypoxia training enhances pilots’ ability to recognise symptoms of acute normobaric hypoxic exposure up to 2.4 years after an initial NH training session. Based on these data, refreshment NH training is nowadays mandatory every 3 years in the FINAF as opposed to the North Atlantic Treaty Organisation (NATO) Standardisation Agreement (STANAG) requirement of 5-year intervals between hypoxia trainings.
Abbreviations: O2: oxygen; TUC; time of usefull consciousness; SpO2: peripheral capillary oxygen saturation; NATO: North Atlantic Treaty Organization; STANAG: stanrdization agreement; HH: hypobaric hypoxia; NH: normobaric hypoxia; FINAF: finnish air force; N2: nitrogen; ECG: electrocardiogram; CI: confidence interval; SD: standard deviation
Introduction
Altitude hypoxia continues to be a major threat in aviation. During the last decade, oxygen (O2)-deprivation and cabin pressurisation problems have been reported in several military aircraft including the F/A-18 Hornet, F-22 Raptor, F-35 Joint Strike Fighter, A-10 Thunderbolt and T-45 Jet trainer (Carey Citation2017). The US Navy has reported an upward trend in the number of physiological episodes including hypoxia symptoms from the year 2010 (12/100,000 F/A-18AD flight hours) to 2017 (over 101/100,000 flight hours) (Rice et al. Citation2019).
O2 deprivation induces tissue hypoxia and a number of other physiological symptoms which can vary between individuals. Symptoms of hypoxia may be mental confusion, light-headedness, tiredness, hot flushes, dizziness, air hunger, tingling skin and visual impairment (Woodrow, Webb, and Wier Citation2011). Hypoxia events increase perceived stress and effort, weaken cognition abilities, impair pattern recognition, increase heart rate and decrease respiratory muscles function (Bustamante-Sánchez, Delgado-Terán, and Clemente-Suárez Citation2019). Hypoxia also causes reduced working memory and impaired decision making, negative effects on oculomotor activity and a decrease in flight performance, all of which lead to a risk of aviation mishap (Cable Citation2003; Temme, Still, and Acromite Citation2010; Petrassi et al. Citation2012; Kowalczuk Citation2016).
At high altitude, pilots need both a certain O2 concentration in breathing gas and a pressurised cockpit in order to avoid hypoxia symptoms. It is critically important for pilots to recognise their own individual hypoxia symptoms to prevent life-threatening incidents. Time of useful consciousness (TUC) values decrease sharply when altitude increases, due to low partial pressure of O2. Typically, the first hypoxia symptoms appear when peripheral oxygen saturation (SpO2) decreases below 80% (Varis, Parkkola, and Leino Citation2019). However, by the time pilots recognise their symptoms, hypoxia is already affecting their cognition and decision-making. It is vitally important to recognise hypoxia symptoms as fast as possible to maximise one’s TUC and safe execution of hypoxia emergency procedures. To practice such emergency procedures in a safe environment a hypoxia training is arranged for aircrew improving their performance in hypoxic incidents.
Hypoxia research data indicate that only 31% of military pilots who have previously experienced the loss of cabin pressure can recognise their hypoxia symptoms (Files, Webb, and Pilmanis Citation2005). However, as many as 94% of F/A-18 Hornet pilots were able to recognise their hypoxia symptoms during the initial hypoxia training in a tactical simulator when they expected hypoxia (Artino, Folga, and Swan Citation2006).
North Atlantic Treaty Organisation (NATO) Standardisation Agreement (STANAG) number 3114 edition 9 requires refreshment of hypoxia training at 5-year intervals, using either hypobaric hypoxia (HH) chambers or normobaric hypoxia (NH) devices (NSO, Citation2020). Hypoxia training is seldom conducted in tactical flight simulators, even though it has been reported to be more realistic and effective than traditional hypoxia training (Artino, Folga, and Swan Citation2006). Analysis of hypoxic exposures in flight simulators has shown that pilots’ flight performance decreases during NH (Temme, Still, and Acromite Citation2010). Hypoxia effects remain for a certain time even when treated with 100% emergency O2 due to the O2 paradox (Malle et al. Citation2016; Varis, Parkkola, and Leino Citation2019). There is no mandated hypoxia training frequency requirement in civil airline aviation although hypoxia-induced civil aviation accidents have happened. Some well-documented hypoxia-induced fatal accidents include the Boeing 737 crash in 2005 in Greece and the Learjet 35 Charter flight crash in 1999 in the USA (NTSB Citation2000). Hence, it has been under discussion if civil aircrew members could also benefit from hypoxia training (Cable and Westerman Citation2010).
The effectiveness of hypoxia training has been evaluated in a few studies. Pilots remember their individual symptoms several years after their training (Smith Citation2008; Woodrow, Webb, and Wier Citation2011; Johnston et al. Citation2012) and the hypoxia symptom profiles seem to be similar compared to those experienced in in-flight hypoxia events with NH training (Deussing, Artino, and Folga Citation2011). However, to the best of our knowledge no validation study of NH training in a flight simulator has been published so far and hypoxia symptoms remember data is from chamber (HH) refreshment training.
The aim of this study was to evaluate the effectiveness of NH training in a military flight simulator in a tactical situation. In this study, we compared the recognition time of hypoxia symptoms during the pilots’ first NH training session (baseline) and 2.4 years later during their second NH training (experimental). Our study hypothesis was that pilots would recognise hypoxia symptoms significantly faster during a second training.
Methods
Subjects
Data for this study were anonymously collected from the first-ever NH training sessions of Hornet pilots in the Finnish Air Force (FINAF). The study was performed in two Hornet squadrons in Finland between November 2008 and February 2015, with a total of 89 pilots (88 male and one female). Every pilot attended NH training on two occasions, the second after 2.4 years on average. All subjects were healthy military pilots (age between 25 and 35 years) they were on active flight status in the FINAF (flight experience range 400−2000 h) and had passed aeromedical evaluation in the aeromedical centre, Helsinki, Finland within the previous 12 months. The study protocol followed the tenets of the Declaration of Helsinki and was approved by the Committee on Research Ethics of the University of Eastern Finland, Joensuu, Finland (no. 24/2018). The study had the institutional approval of the Defence Command Finland. Each participant gave informed consent on a voluntary basis. Before the study, all subjects had completed a hypoxia theory lesson and most of them (93%) had also participated in a hypobaric chamber training more than 5 years earlier.
Equipment
Flight simulator
A fixed-based tactical F/A-18C Hornet WTSAT simulator (Boeing Corporation, Chicago, IL) was used with a field of view of 180 degrees. The pilots’ flight gear consisted of a Joint Helmet Mounted Cueing System helmet (JHMCS, Collins Aerospace, Charlotte, NC) and an oxygen mask (Gentex Corporation, Zeeland, ML) as normally worn while flying a fighter aircraft.
Hypoxic gas mixtures
To provide differences in the hypoxia onset rate five high-pressure cylinders with different concentrations of O2: 100, 21, 8, 7 and 6% were used. These cylinders were connected to the simulator and allowed a flight surgeon to manually change the selection to each subject. To simulate the diminished O2 present at altitude and induce hypoxia under normobaric conditions, the following mixtures of breathing O2 and nitrogen (N2) were prepared:
8% O2 and 92% N2 at 760 mmHg to simulate conditions at 6200 m (20,341 ft).
7% O2 and 93% N2 at 760 mmHg to simulate conditions at 7000 m (22,966 ft).
6% O2 and 94% N2 at 760 mmHg to simulate conditions at 7900 m (25,919 ft).
Measurement devices
Peripheral capillary oxygen saturation (SpO2) was measured from the forehead (Nonin Medical Inc., Plymouth, MN).
Wireless electrocardiograms (ECGs) were continuously monitored by a flight surgeon to assure safety.
Experimental design
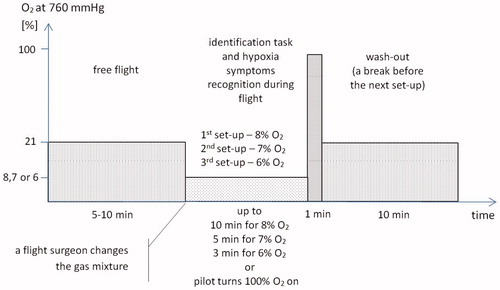
The hypoxia training was carried in two training sessions (initial and experimental) during tactical identification flight missions in a flight simulator. Each training session consisted of three set-ups (). In each set-up, without the subjects’ knowledge, the O2 concentration was decreased to 8, 7 or 6%, from the normal 21%. The typical duration of the set-up before low O2 gas was 5–10 min. Before breathing the hypoxic gas mixtures, the subjects used the O2 mask to breath 21% O2 in 78% N2 at 760 mmHg. Pilots continued their set-up until they noticed hypoxia symptoms and executed emergency procedures including switching on 100% emergency O2. After each set-up, there was a 10-min wash-out before the next set-up to reduce the cumulative effect.
Figure 1. Experimental setup description.
No control set-up (21% O2) was performed since the subjects acted as their own controls in the second (experimental) hypoxia training.
Procedure
Pilots performed a hypoxia symptoms recognition task while completing the tactical identification flight missions. Their primary task was to visually identify unknown aircraft and actively fly the fighter while maintaining the speed, altitude and heading ordered by the fighter controller via radio. However, subjects were told to treat all of the tasks (aircraft identification and hypoxia symptoms recognition) as equally important.
O2 mixtures were given in a specific order in a training session. The first set-up was executed with a cylinder containing 8% O2, the second with a 7% O2 cylinder and the third with a 6% O2 cylinder. Pilots were instructed to abort a flight mission as early as they recognise the first hypoxia symptoms. They continued their set-up until they noticed hypoxia symptoms (for example cognitive performance problems and skin tingling) and executed emergency procedures including switching on 100% emergency O2 (). Due to the pilots’ safety the maximum exposure times of set-ups were limited to 600 s/8% O2, 300 s/7% O2 and 180 s/6% O2. To avoid any negative consequences of training, the flight surgeon can abort or cancel the hypoxia set-up if necessary. Too deep hypoxia exposure will not support training goals because of the risk that the pilot cannot remember what happened during deep hypoxia. NH exposures may cause memory problems and more adverse effects which need to be taken into account after the simulator training (Varis, Parkkola, and Leino Citation2019).
During the flight missions, a flight nurse recorded the pilots’ SpO2, heart rate and hypoxia symptoms recognition time as reported by the subject via intercom during the set-ups. The correctness of aircraft identification or flight performance was not recorded. The measurements taken during the first (initial/baseline) and the second (experimental) NH training were identical. To evaluate the effectiveness of NH training the pilots’ SpO2 and hypoxia symptoms recognition time were taken. Our primary outcome was the time taken to notice hypoxia symptoms during the experimental hypoxia training session compared to the baseline session.
The total duration of the training session was in average 50 min. The study was done during a normal workday, between 8:00 AM and 4:00 PM.
Statistical analysis
Exposure-level differences between the three O2 concentrations were subjected to Friedman’s two-way analysis of variance. Differences in recognition times and SpO2 values within each group between training sessions (initial and experimental) were analysed with a paired t-test. Pearson’s correlation coefficient was used to test correlations between the hypoxia symptoms recognition time and SpO2 value and correlations between the initial and the experimental sessions. Differences were regarded as statistically significant when the p value was less than .05. For multiple comparisons, the Bonferroni correction was applied. Results are expressed as mean values with a standard deviation or median with 25 and 75 percentiles where appropriate. For the primary outcome measure, which was the time taken to notice hypoxia symptoms during the experimental hypoxia training session compared to the baseline session; we calculated the mean difference and a 95% confidence interval (CI) for the difference.
Results
We compared the results from the initial (baseline) NH training session with those from the second (experimental) NH training session for the 89 pilots, all of whom had data for both sessions (, and ). The mean time difference between baseline session and experimental session was 2.4 (SD 1.3) years.
Figure 2. The level of oxygen saturation (SpO2) at the time recognition of hypoxia using of a reduced 8, 7 or 6% oxygen breathing mixture. Solid line is the regression line for the initial training session and dashed line for the experimental training session. The two outliers’ values are presented in grey rectangles.
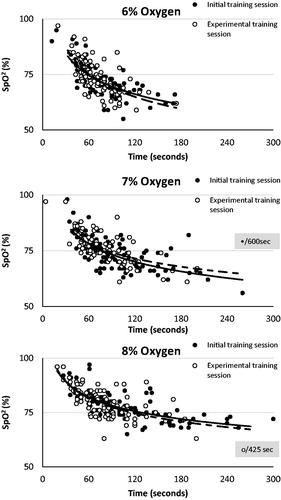
Figure 3. Hypoxia recognition time difference between the initial (baseline) and the second (experimental) training session. Medians are highlighted with black line. Negative value means that in the experimental session the pilots were able to recognise hypoxia faster than in the initial training session and positive values vice versa.
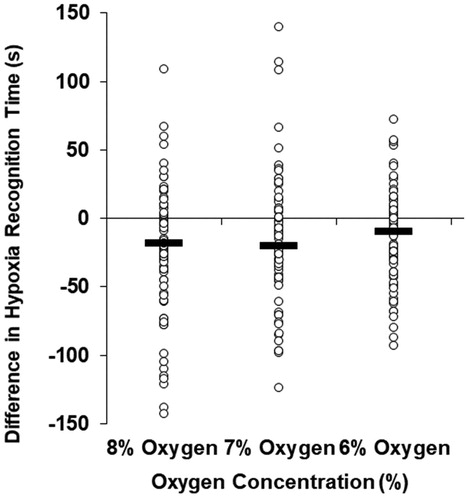
Table 1. Time of hypoxia symptoms recognition and level of oxygen saturation (SpO2) in three oxygen concentrations in baseline NH training and in experimental NH training.
The number of participants differs in each set-up because for some of the subjects the NH training was reduced to two exposures (instead of the full three, i.e. 8, 7 and 6%) based on the flight surgeon’s evaluation and decision during the NH training.
Initial (baseline) normobaric hypoxia training session
In the first set of exposures, a difference was found between the three set-up concentrations in the time taken to recognise hypoxia (p = .002, df 2, test value 12.167) and in the SpO2 value at that time point (p < .001, df 2, test value 59.421). In the first set-up (n = 89), with the 8% inspired O2 concentration, the mean duration to hypoxia symptom recognition was the longest, 103 (SD 52) s, and the mean of the SpO2 value at that point was the highest, 78 (6)%. With the 7% inspired O2 concentration (n = 72), the mean duration was 100 (64) s and the mean SpO2 value was 74 (7)%. With the 6% inspired O2 concentration (n = 75), the mean duration was the shortest, 81 (33) s and the mean SpO2 value was the lowest, 73 (7)%.
The symptoms reported by the pilots (n = 75) in the baseline training session were tingling skin (68%), hot flushes (60%), cognitive impairment (41%), dizziness (39%), difficulty in breathing (36%), visual impairment (32%) and light-headedness (13%).
Second (experimental) normobaric hypoxia training session
In the second set of exposures, the time taken to recognise hypoxia was similar in the three set-up inspired O2 concentration: with 8% O2, it was 85 (51) s; with 7% O2, it was 80 (36) s; with 6% O2, it was 71 (25) s (p = .498, df 2, test value 1.393). The mean of the SpO2 value at the time of hypoxia recognition was highest with the 8% O2, 80 (7)%, with the 7% O2, it was 77 (7)%, and with 6% O2, it was 74 (8)% (p < .001, df 2, test value 24.951).
When compared to the initial hypoxic training session, mean of hypoxic recognition time was shortened by 18 s (95% CI 8–37; p = .002, df 88, paired t-test) while inspiring 8% O2 (n = 89), by 20 s (95% CI 5–42; p = .014, df 71, paired t-test) while inspiring 7% O2 (n = 72); and by 10 s (95% CI 5–21; p = .002, df 74, paired t-test) while inspiring 6% O2 (n = 75). displays all the individual hypoxic recognition times during the baseline and experimental training sessions. displays all the differences in recognition time between the initial and the experimental training, negative values mean that the recognition was quicker in the experimental session compared to the baseline session.
Two pilots reported symptoms of hypoxia relatively early, one pilot in the initial training with 6% O2 reported hypoxia symptoms at 12 s and another with 7% at 4 s. Two pilots did not report hypoxia symptoms during the safety window and were switch to breath 100% O2, one with 7% O2 in the initial training and one with 8% O2 in the experimental session. However, these pilots were included in the data analysis ().
Discussion
Most pilots were able to recognise hypoxia in a substantially shorter time in the experimental session. Two-thirds (64%) of this cohort were better able to recognise hypoxia symptoms in the experimental training session compared to the baseline training session. With the 8% O2 gas mixture, 62% of the pilots recognised hypoxia symptoms quicker; with the 7% O2 gas mixture, 44% recognised them quicker; and with the 6% O2 gas mixture, 85% recognised the symptoms quicker than in the baseline training.
There seems to be a substantial between-individual variation in subjects’ hypoxia recognition times. In the experimental session, the median recognition time for 8% O2 hypoxia was 80 s with interquartile range of 52–96 s (). However, a 10-fold between-individual variation emerged in our study: in one outlier the hypoxia symptoms recognition time was 425 s. It is known fact, that not all pilots report any identified hypoxia symptoms after being exposed to HH in chamber training (Smith Citation2008). One explanation could be slow ventilation rate and lack of hyperventilation symptoms. In this study, the SpO2 at the time of recognition varied considerably between 65 and 97% in the initial training session, and between 63 and 97% in the experimental session. Most pilots were able to recognise hypoxia symptoms with SpO2 values of 78–79% or higher, but for some pilots SpO2 values had decreased below 70% before they were able to recognise the symptoms of hypoxia
Hypoxia symptoms can vary from one training exposure to another, and this variation may affect the pilots’ ability to recognise the symptoms. One of the reasons for this may be increased ventilation rates resulting in a combination of hypoxia and hypocapnia (Loeppky et al. Citation1997; Temme et al. Citation2017). This combination may lead to respiratory alkalosis, which shifts the O2 dissociation curve to the left. Initially, with decreased O2 tension, unloading of O2 at peripheral tissues is favoured, but in hypoxia and hypocapnia haemoglobin has an increased affinity for O2 and unloads it more reluctantly. Consistent with our findings, others have shown that there is considerable variation in response to hypoxia, and people tend to forget their symptoms of hypoxia (Woodrow, Webb, and Wier Citation2011).
There are some weaknesses in this study, the main one being that the pilots knew they were taking part in hypoxia training. The Hawthorne effect (Sedgwick and Greenwood Citation2015) may have modified some pilots’ behaviour, as six pilots in both training sessions reported the first hypoxia symptoms after less than 60 s exposure to 8% O2, and their SpO2 values were over 90%. A blinded control scenario with 21% O2 in random order would provide more information about false positives. Hypoxia training has to identify pilots that are trying to ‘guess’ rather than respond to physiological stimuli without system warning, e.g. master caution. On the other hand, both training sessions involved the same situation.
Another weakness of this study is that there is less physical and mental stress when flying in a simulator compared to real flying situations. This might have expedited hypoxia symptom recognition in our study, so our research results might be biased in an unsafe direction. Further studies are needed to evaluate whether this kind of fixed hypoxia training schedule is sufficient or whether training should be organised on a more individual basis. The latter is supported by the fact that, in this study, the median time to recognise hypoxia decreased less than the mean time. Pilots who took a relatively long time to recognise hypoxia in the initial training improved their skills substantially in the second training. As a result, the between-individual variation was considerably less in the experimental than in the baseline training.
In future training, to reduce a cumulative effect of repeated NH exposures, set-ups can be limited to two consecutive exposures at a time. The first set-up should be done with 8% O2 and the second with either 7 or 6% O2, to demonstrate different hypoxia onset rates and TUCs. It is assumed that at least an 10-min wash-out time should be used to reduce the cumulative effect of hypoxia training between consecutive exposures, but more research is needed on this issue. Also in future pilots’ sleep quality and fatigue should be controlled which were not done in this study.
Johnston et al. (Citation2012) have documented that after hypoxia chamber training, i.e. hypoxic hypoxia, hypoxia symptoms replication can be achieved 4.5 years subsequently. However, that study used only 26 subjects, all were not military pilots, and the range between hypoxia trainings was 1–12 years. In a survey of aircrew (n = 49), 10% of subjects could not remember even a single hypoxia symptom from their previous hypoxia chamber training 3 years earlier (Smith Citation2008).
Based on our results, the Air Force Command Finland now requires NH training every 3 years instead of the earlier 5 year intervals. In addition, it is mandatory to do hypoxia refreshment training in a tactical fighter simulator as opposed to hypobaric chamber training. The Royal Australian Air Force has gone even further due to concerns of increasing numbers of in-flight hypoxia-like symptoms. They require NH training in a tactical F/A-18F Hornet simulator annually (Hampson Citation2019). The Norwegian Air Force also changed their hypoxia training in 2017 due to the introduction of fifth-generation fighters, and now they require NH training of F-35 pilots annually (Kjeserud Citation2020).
One option when arranging hypoxia training is to attach it to annual emergency procedures training in a tactical fighter simulator. This way, pilots would not know in which year emergency procedures training will consist of both NH training and other emergency procedures. However, this approach would be labour-intensive due to training safety, and normal emergency procedure’s training does not require the presence of flight surgeons/flight nurses.
Conclusions
In this study, NH training in a tactical fighter simulator improved fighter pilots’ ability to recognise hypoxia symptoms after 2.4 years from the initial NH training. It has not been scientifically established how often training sessions should be repeated. NATO STANAG 3114 edition 9 require hypoxia refreshment training at intervals not exceeding five years. More frequent refresher hypoxia training is at the discretion of individual nations. Since 2018 NATO hypoxia recognition training can be done either as NH training or as HH training in an altitude chamber.
At present, few surveys of HH training in chambers (Woodrow, Webb, and Wier Citation2011) support NATO STANAG 3114 with a 5-year interval of hypoxia training. Nowadays, most hypoxia training is executed as NH training. Our results indicate that the recognition of NH symptoms is maintained or improved for up to 2.4 years after an initial training session, albeit with considerable between-individual variability in response times. In the absence of longer-term follow-up data, we recommend that pilots undergo NH training in a tactical simulator at shorter intervals than a 5-year cycle.
Acknowledgements
The authors acknowledge senior flight surgeon Jarmo Skyttä, M.D., for his valuable work during data collection. The authors would also like to thank all the participants involved in this research.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Artino, A. R., R. V. Folga, and B. D. Swan. 2006. “Mask-on Hypoxia Training for Tactical Jet Aviators: Evaluation of an Alternate Instructional Paradigm.” Aviation Space and Environmental Medicine 77 (8): 857–863.
- Bustamante-Sánchez, A., M. Delgado-Terán, and V. J. Clemente-Suárez. 2019. “Psychophysiological Response of Different Aircrew in Normobaric Hypoxia Training.” Ergonomics 62 (2): 277–285. doi:10.1080/00140139.2018.1510541.
- Cable, G. 2003. “In-Flight Hypoxia Incidents in Military Aircraft: Causes and Implications for Training.” Aviation Space and Environmental Medicine 74 (2): 169–172.
- Cable, G. G., and R. Westerman. 2010. “Hypoxia Recognition Training in Civilian Aviation: A Neglected Area of Safety?” JASAM 5 (1): 4–6. http://www.hypoxic-training.com/new_abstracts/2010_JASAM_Cable_Westerman_Neglected_Area_of_Safety_Normobaric_Hypoxia_Training.pdf
- Carey, B. U. S. 2017. “Military tackles vexing issue of physiologic episodes.” Aviation International News, October 27, 2017. Accessed 7 April 2020. https://www.ainonline.com/october-2017.
- Deussing, E. C., A. R. Artino, and R. V. Folga. 2011. “In-flight Hypoxia Events in Tactical Jet Aviation: Characteristics Compared to Normobaric Training.” Aviation Space and Environmental Medicine 82 (8): 775–781. doi:10.3357/asem.2941.2011.
- Files, D. S., J. T. Webb, and A. A. Pilmanis. 2005. “Depressurization in Military Aircraft: Rates, Rapidity, and Health Effects for 1055 Incidents.” Aviation Space and Environmental Medicine 76 (6): 523–529.
- Hampson, G. 2019. “Hypoxia Recognition and Recovery Training in Royal Australian Air Force F/A-18F and EA-18G Aircrew.” Aerospace Medicine and Human Performance. 90 (3): 176.
- Johnston, B. J., G. S. Iremonger, S. Hunt, and E. Beattie. 2012. “Hypoxia Training: Symptom Replication in Experienced Military Aircrew.” Aviation Space and Environmental Medicine 83 (10): 962–967. doi:10.3357/asem.3172.2012.
- Kjeserud, J. A. 2020. “Hypoxia Training in the Norwegian Armed Forces: Lessons Learned and Future Plans.” Aerospace Medicine and Human Performance. 91 (3): 229–230.
- Kowalczuk, K. P., S. P. Gazdzinski, M. Janewicz, M. Gąsik, R. Lewkowicz, and M. Wyleżoł. 2016. “Hypoxia and Coriolis Illusion in Pilots during Simulated Flight.” Aerospace Medicine and Human Performance 87 (2): 108–113. doi:10.3357/AMHP.4412.2016.
- Loeppky, J. A., M. Icenogle, P. Scotto, R. Robergs, H. Hinghofer-Szalkay, and R. C. Roach. 1997. “Ventilation during Simulated Altitude, Normobaric Hypoxia and Normoxic Hypobaria.” Respiration Physiology 107 (3): 231–239. doi:10.1016/S0034-5687(97)02523-1.
- Malle, C., C. Bourrilhon, P. Quinette, M. Laisney, F. Eustache, and C. Piérard. 2016. “Physiological and Cognitive Effects of Acute Normobaric Hypoxia and Modulations from Oxygen Breathing.” Aerospace Medicine and Human Performance 87 (1): 3–12. doi:10.3357/AMHP.4335.2016.
- NTSB. 2000. http://www.airsafe.com/events/reports/payne-stewart-1999.pdf
- NSO. 2020. “Aeromedical training for flight personnel.” Brussels Belgium: North Atlantic Treaty Organization. 2018. Standardization agreement 3114, NATO STANAG 3114 ed.9. Accessed September 24. https://nso.nato.int/nso/zPublic/stanags/CURRENT/3114EFed09.pdf
- Petrassi, F. A., P. D. Hodkinson, P. L. Walters, and S. J. Gaydos. 2012. “Hypoxic Hypoxia at Moderate Altitudes: Review of the State of the Science.” Aviation Space and Environmental Medicine 83 (10): 975–984. doi:10.3357/asem.3315.2012.
- Rice, G. M., D. Snider, S. Drollinger, C. Greil, F. Bogni, J. Phillips, A. Raj, K. Marco, and S. Linnville. 2019. “Dry-EEG Manifestations of Acute and Insidious Hypoxia during Simulated Flight.” Aerospace Medicine and Human Performance 90 (2): 92–100. doi:10.3357/AMHP.5228.2019.
- Sedgwick, P., and N. Greenwood. 2015. “Understanding the Hawthorne Effect.” BMJ 351: h4672. doi:10.1136/bmj.h4672.
- Smith, A. M. 2008. “Hypoxia Symptoms in Military Aircrew: long-Term Recall vs. Acute Experience in Training.” Aviation, Space, and Environmental Medicine 79 (1): 54–57. doi:10.3357/asem.2013.2008.
- Temme, L. A., P. St Onge, M. Adams, D. L. Still, J. K. Statz, and S. T. Williams. 2017. “A Novel, Inexpensive Method to Monitor, Record, and Analyze Breathing Behavior during Normobaric Hypoxia Generated by the Reduced Oxygen Breathing Device.” Military Medicine 182 (S1): 210–215. doi:10.7205/MILMED-D-16-00053.
- Temme, L. A., D. C. Still, and M. T. Acromite. 2010. “Hypoxia and Flight Performance of Military Instructor Pilots in a Flight Simulator.” Aviation Space and Environmental Medicine 81 (7): 654–659. doi:10.3357/asem.2690.2010.
- Varis, N., K. Parkkola, and T. Leino. 2019. “Hypoxia Hangover and Flight Performance after Normobaric Hypoxia Exposure in a Hawk Simulator.” Aerospace Medicine and Human Performance 90 (8): 720–724. doi:10.3357/AMHP.5289.201.
- Woodrow, A. D., J. T. Webb, and G. S. Wier. 2011. “Recollection of Hypoxia Symptoms between Training Events.” Aviation, Space, and Environmental Medicine 82 (12): 1143–1147. doi:10.3357/asem.2987.2011.
