Abstract
Safe patient care in hospitals relies on teamwork. Transactive Memory Systems (TMS), are shared cognitive systems that have been linked to team performance in other domains, but have received limited attention in healthcare. This study investigated the role of TMS, psychological safety and interpersonal conflict in predicting team performance in hospital ward teams where team membership is dynamic and often loosely defined. Hospital staff (n = 106) in four wards completed a battery of instruments assessing team performance, TMS, psychological safety and interpersonal conflict. TMS was a weak predictor of team performance, but the relationship was mediated by psychological safety. Overall, team performance was predicted by high psychological safety, low interpersonal conflict and low reliance on team members’ knowledge (i.e. TMS credibility). These findings suggest that, in hospital teams, TMS is not a strong predictor of team performance but team culture is critical to ensure the quality and safety of patient care.
Practitioner summary: This study investigated the role of Transactive Memory Systems (TMS) and cultural factors in hospital team performance. Team performance was predicted by psychological safety, low interpersonal conflict and low reliance on team members’ untested knowledge. This highlights the importance of a supportive and psychologically safe team culture for safe care in hospitals.
Abbreviations: TMS: transactive memory systems; HCA: health care assistant
Introduction
Safe and effective patient care in clinical settings relies on teamwork; multiple professionals, from different healthcare disciplines, work together with the common purpose of managing and treating a patient. Recent comprehensive reviews have shown that poor teamwork contributes to a large proportion of preventable patient harm and patient mortality (Rosen et al. Citation2018; Schmutz, Meier, and Manser Citation2019). Thus, a promising route to improving the safety and quality of patient care is to identify the factors that contribute to better teamwork within hospital systems. Teamwork research in healthcare has predominantly focused on stable, co-located groups of individuals working together on well defined, time limited tasks (Rosen et al. Citation2018), such as surgical or trauma teams. However, this does not reflect most teamwork occurring in hospitals. For example, hospital ward staff co-ordinate their activities with many other professional teams and deliver care around the clock (Chesluk et al. Citation2015). Although care on wards relies on the co-ordination and articulation of tasks, team composition and team responsibilities are often not well defined, well-structured or stable. These characteristics of ward teams suggest that teamwork may be challenging, but there has been limited investigation of ward teams and factors associated with team performance.
One promising avenue for increasing our understanding of healthcare team co-ordination is team cognition. Team members’ shared cognitive systems, such as Transactive Memory Systems (TMS), have been consistently linked to team performance in other professional domains (Kim, Mu, and Moon Citation2018; Ren and Argote Citation2011; Bachrach et al. Citation2019; DeChurch and Mesmer-Magnus Citation2010) and communication has been shown to be central in the functioning of TMS (Peltokorpi and Hood Citation2019). Research in hospital teams has shown that frequent team interactions and satisfaction with the quality of team communication are linked to better TMS (Liao et al. Citation2015; Tan et al. Citation2014). However, TMS is under researched in the healthcare domain. Most TMS research in healthcare has focussed on identifying predictors of TMS (Liao et al. Citation2015), or used TMS as an outcome measure of teamwork, to assess, for example, the effects of new technology on teamwork (Lazzara et al. Citation2015), or used it to predict aspects of teamwork, such as leadership style (Ong, Koh, and Lim Citation2020), team effectiveness, job satisfaction and team identification (Michinov et al. Citation2008). The relationship between TMS and team performance in hospital ward teams, with loosely defined and dynamic team membership, remains unclear.
Psychological and cultural factors, such as psychological safety and interpersonal conflict, create environments that can foster or hinder communication in healthcare teams and so are likely to impact team cognition and affect teamwork performance. For example, staff members’ perceptions of how psychologically safe it is to ‘speak up’ within a team will influence team communication (O'Donovan and McAuliffe Citation2020). Studies have found associations between TMS and psychological safety in other industries (Kim, Kim, and Jo Citation2021). However, this remains to be explored in healthcare teams.
Bridging these gaps in current research, the aim of this study was to examine the relationship between TMS and team performance in hospital ward teams and examine the influence of psychological safety and interpersonal conflict on (i) team performance and (ii) the relationship between TMS and teamwork performance. In the following sections, we briefly review these concepts in more detail.
Transactive memory systems
Transactive memory refers to knowledge about what other people know. Transactions with other people, such as requesting information and communicating with them, are required to retrieve the information they hold (Bachrach et al. Citation2019). In teamwork research, a transactive memory system is a cognitive system that is shared between team members and it includes knowledge about what other team members know. It is closely related to team constructs such as shared mental models, which refer to a team’s shared understanding of tasks, the team, and the environment (Bachrach et al. Citation2019). TMS is more narrowly focussed and refers to shared understanding of the team and the expertise of its members, not the tasks or environment (Lewis Citation2003).
A TMS is a shared understanding of which members know, and are responsible for, what knowledge (Wegner Citation1987; Moreland and Myaskovsky Citation2000). It has three dimensions: (1) Specialisation, which refers to knowledge about each team members’ specialised knowledge; (2) Credibility, which refers to beliefs about the reliability of other members’ knowledge and (3) Coordination, which is the process of effectively coordinating knowledge between team members (Lewis Citation2003). TMS attempts to explain how expertise is recognised and coordinated within teams and leads to shared interpretations of the information available to team members. For example, when information is required by an individual who does not possesses it, in teams with effective TMS, information can be requested directly from the relevant team member (Wegner Citation1987; Whelan and Teigland Citation2013), because the expertise of team members is known and trusted. Co-ordination of information between team members is thus facilitated.
The degree to which teams can develop an effective TMS is likely to be inhibited by having team members from different disciplines, loosely formed team structures, episodic teamwork and high member turnover, all of which are ubiquitous in healthcare teams (Chesluk et al. Citation2015). However, there are factors that facilitate the development of TMS. For example, team and professional identity mediate the relationship between communication quality and TMS but in different ways. Team identification is positively related to TMS and the relationship is stronger for those with low professional identity. High professional identity predicts high TMS for both high and low team identification (Liao et al. Citation2015). Communication is also important; effective TMS relies on effective communication (Peltokorpi and Hood Citation2019). Research in a range of professional domains has shown that the frequency and quality of the communication among team members directly influences the development and functioning of TMS and the resulting team performance, and vice versa (Liao, Jimmieson, and O’Brien Citation2012; Pearsall and Ellis Citation2006; Peltokorpi and Manka Citation2008; Pearsall, Ellis, and Bell Citation2010). Poor communication reduces the ability of team members to recognise the expertise of individuals within the team, reducing the ability of the team to effectively use its expertise (Kotlarsky, van den Hooff, and Houtman Citation2015). Further research is needed to investigate the relationship between TMS and team performance, moving beyond investigation of factors predictive of TMS to explore performance. In particular, clarity is needed about how social and cultural team factors mediate between TMS and team performance.
Psychological safety
Psychological safety is a shared belief that the team is a safe environment for interpersonal risk taking, where team members feel safe to question others, offer and receive feedback and engage in open discussions (Edmondson Citation1999). Theoretical models of teamwork suggest that effective teams must enable members to ‘speak up’ when lapses or errors in teammates’ performance are observed (Salas, Sims, and Burke Citation2005) and indeed empirical studies have found that ‘speaking up’ is related to better team performance (Kolbe et al. Citation2012). Psychological safety facilitates team communication especially in relation to identifying problems and correcting team performance.
The presence of psychological safety has been shown to improve knowledge sharing among healthcare teams, suggesting that psychological safety may facilitate the development of an effective TMS (Kessel, Kratzer, and Schultz Citation2012). This is plausible as psychological safety is an element of effective team communication, which has itself been found to predict the development of TMS (Liao et al. Citation2015). However, it is still unclear how psychological safety and TMS interact to influence performance. We hypothesise that the presence of a psychologically safe environment will improve the relationship between TMS and team performance in the context of healthcare teams.
Interpersonal conflict
Interpersonal conflict, or relationship conflict as it is sometimes known, is defined as ‘a dynamic process that arises among individuals who experience negative emotional reactions to perceived disagreement’ (Barki and Hartwick Citation2004). This is distinguished from task or process focussed conflict, in which people have disagreements over ideas, strategies or approaches (Jehn Citation1997). A meta-analysis involving studies in multiple professional domains revealed a significant negative relationship between interpersonal conflict and team performance, particularly for complex tasks (De Dreu and Weingart Citation2003). An empirical study of management teams in the financial sector found that although TMS was positively associated with team performance, this relationship no longer existed when high levels of interpersonal conflict were present (Rau Citation2005).
Healthcare teams are frequently managing stressful and pressured situations and under such circumstances interpersonal conflict can arise (Almost et al. Citation2016). The presence of interpersonal conflict, but not task focussed conflict, in healthcare teams has been linked to poorer staff and patient outcomes (Rosenstein Citation2011; Laschinger Citation2014). Therefore, it would be expected that similar to studies in other professional domains, interpersonal conflict would weaken the relationship between TMS and healthcare team performance.
In summary, previous studies of TMS in healthcare teams have highlighted its importance for team outcomes such as communication quality, leadership, job satisfaction and team identification, and identified the important mediating and moderating effects of team and professional identity respectively on the relationship between TMS and team outcomes. In this study we investigated this relationship further by investigating the role of TMS, psychological safety and interpersonal conflict in predicting team performance. Psychological safety and interpersonal conflict are both crucial factors affecting team performance in healthcare, and it is still unclear whether and how these variables are related to TMS and its effects on performance. We studied ward teams, which have generally received less attention than other teams with clearly defined and time limited tasks such as surgery. The aim of this study, therefore, was to investigate how psychological and cultural factors affect team performance, and the relationship between TMS and team performance, in ward teams.
The following research questions were investigated:
Does TMS score predict team performance?
Does psychological safety predict team performance?
Does interpersonal conflict predict team performance?
Does psychological safety moderate the relationship between TMS and team performance?
Does interpersonal conflict moderate the relationship between TMS and team performance?
Methods
Participants
All healthcare staff working within three diverse hospital areas (Older Adult Unit, Surgery and Acute Assessment Unit) in a central London hospital were eligible to participate. Participants (n = 106) included nurses (n = 59), doctors (n = 10), Allied Health Professionals (n = 21) and Health Care Assistants (n = 16). Following agreement from ward managers and dissemination of study information to staff in meetings and via email, participants gave informed consent for the study. They completed a battery of survey instruments via the Qualtrics on-line platform on hand held devices disseminated by the research team during their shift. The survey battery, described in detail below (see measures), assessed: staff demographic information, team composition, psychological safety, interpersonal conflict, Transactive Memory Systems (TMS) and team performance. Participants were asked to respond to the questions considering the teams they most frequently work in during a shift.
Wards
The four wards varied in terms of their function, team stability and patient turnover. The older adult unit had stable team members and slow patient turnover (e.g. weeks). The Acute Assessment Unit is designed to only take patients for a short duration (i.e. 24–48 h) and although they may have a core nursing team, the ward team is dynamic with the majority of staff joining their ward team to complete time-limited episodes of work. Both surgical wards had different patient demands with one managing shorter stay patients and the second managing more complex patients who require longer admissions. Nurses often move between wards and surgeons manage patients across multiple wards, not just surgical wards, requiring them to join multiple ward teams to provide patient care.
Measures
Demographic and team information
Participants’ gender, professional group (doctor, nurse, Allied Health Professionals, Health Care Assistants) and years of experience (i.e. qualified staff - number of years spent working as a qualified healthcare professional; for HCA’s- years of experience as a HCA) were recorded. Because ward staff can be members of different teams (e.g. single or multi-professional), at the start of the questionnaire participants were asked to indicate whether their answers referred to their experience of working in a uni-professional team (e.g. nursing team), or multi professional, (i.e. teams including members from multiple professional disciplines) team. They were asked to answer the questions on the battery in relation to this team.
Transactive memory system
A 15-item self-report instrument was used to assess the Transactive Memory System (TMS) in organisational teams (Lewis Citation2003). Participants are asked to rate each of the 15 statements (e.g. each team member has specialised knowledge of some aspect of our project) on a 5-point scale (1 strongly disagree – 5 strongly agree). The instrument has three distinct factors, (1) team specialisation – differentiation of knowledge between team members (2) team credibility – members' beliefs about the reliability of other team members’ knowledge (3) team coordination – members' ability to effectively coordinate their knowledge. A mean score across all three factors was calculated providing an overall TMS score. Higher scores indicate a better team TMS. The scale is reliable and has shown convergent, criterion-related and discriminant validity (Lewis Citation2003). Items in each factor demonstrated good internal consistency (specialisation α = .84, credibility α = .81, coordination α = .83).
Psychological safety
A 7-item self-report structured instrument was used to assess team psychological safety, which is a shared belief that the team is safe for interpersonal risk taking (Edmondson Citation1999). Across the seven statements, participants are asked to select the option that most accurately reflects their opinion (e.g. It is safe to take a risk on this team) on a 7-point Likert scale (1 very inaccurate − 7 very accurate). Higher scores indicate participants feel more psychologically safe. Items formed a single scale (α = .73).
Interpersonal conflict
Participants' perception of interpersonal conflict was assessed using six items (Hinds and Mortensen Citation2005). Participants were presented with six questions relating to interpersonal conflict within their team (e.g. how much friction is there among members in the team?). Participants were asked to select the option that most accurately reflects their opinion on a six-point scale (1-not at all to 6 – very much). The items have good reliability (α = .89). Higher scores indicate more interpersonal conflict.
Team performance
Team performance was assessed using three items, which have demonstrated good reliability (α = .84) (Hinds and Mortensen Citation2005). Participants were asked: ‘compared with the very best team you are working with/have worked with in the past, rate the performance of your team on a six point scale (1 poor to 6 excellent) on the items of efficiency, quality and work excellence’. Mean overall scores were calculated to give an overall team performance score, with higher scores indicating better team performance.
Statistical analysis
Descriptive analyses
The relationship between team composition (uni vs multi-professional) and professional group (doctor, nurse,health care assistant and allied health professional) was examined using a Chi Squared test. Independent samples T-tests compared participants’ scores on assessments of psychological safety, interpersonal conflict, TMS and team performance by team composition (uni vs multi-professional).
Spearman’s Rho correlations analysed the inter-correlations between variables.
Predictors of team performance
A multiple regression analysis examined the relationship between demographic measures (ward, professional group and years of experience) and team performance.
To investigate the research questions and identify predictors of team performance, a hierarchical regression analysis was used with team performance entered as the dependent variable. The predictor variables were entered in 4 models: model 1 – TMS subscales (i.e. TMS specialisation, TMS credibility and TMS coordination); model 2 – psychological safety and model 3 – interpersonal conflict. Model 4 – investigated the moderating role of psychological safety and interpersonal conflict on the relationship between TMS and team performance. It included two interaction terms (i) Psychological safety*TMS and (ii) Interpersonal conflict*TMS. The statistical significance was set at p = .05 for all analyses.
Results
Participant demographic information
The majority of participants were female (n = 83, 78%). Professional groups included: doctors (n = 10, 9.4%), nurses (n = 59, 55.7%), HCAs (n = 16, 16%) and Allied Healthcare Professionals (n = 21, 19.9%). Staff were based in four diverse hospital wards [older adult unit (n = 21, 20%) surgical unit 1 (n = 21, 20%), surgical unit 2 (n = 33, 31%) and acute assessment unit (n = 31, 29%)]. Participants had on average 5.16 years of experience (Range 0 – 33 years, sd = 7.23).
Descriptive analyses
Participants’ mean scores and standard deviations across all instruments (psychological safety, interpersonal conflict, TMS and team performance) are displayed in .
Table 1. Means, standard deviations and ranges for all variables alongside Spearman’s correlations between variables.
Team composition
Fifty-two participants (49%) reported working in a uni-professional team, while 39 participants (37%) reported working in a multi-professional team. A further 15 participants (14%) declined to answer this question. These participants were excluded from any analyses involving team composition. There was no significant difference between professional groups in terms of team composition (Chi (3) = 2.50, p = .48) (see ), TMS (F(3, 105) = .70, p = .55) or team performance (F(3, 105) = .90, p = .44). Compared to participants working in uni-professional teams, participants working in multi-professional teams had significantly higher psychological safety (p = .02) and TMS scores (p = .03) ().
Figure 1. Participants’ team composition (uni vs multi-professional) by professional group.
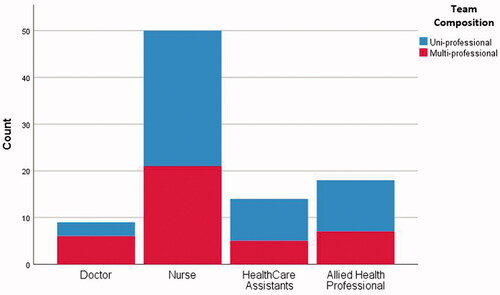
Table 2. Independent samples T-test comparing participants' measurement scores by team composition.
Inter-relationships between variables
Spearman’s correlations are displayed in . Team performance was significantly positively associated with TMS (p < .01) and psychological safety (p < .01) and significantly negatively associated with interpersonal conflict (p < .01). TMS was significantly positively associated with psychological safety (p < .01) and significantly negatively associated with interpersonal conflict (p < .05).
Predictors of team performance
Ward, professional group and years qualified were not significant predictors of team performance (F(7,105) = 1.21, p = .31), as such they were not included in the subsequent hierarchical regression analyses.
Hierarchical regression analyses exploring the predictors of team performance are displayed in (models 1 – 4). Staff demographic variables (professional group and years of experience) and team composition were not included in the analyses as they were not significantly related to team performance (see descriptive analyses above). Multicollinearity was tested in each model and found not to be present.
Table 3. Hierarchical regression analysis predicting team performance (dependent variable).
Model 1, which included the TMS subscales of specialisation, credibility, and coordination as independent variables, was significant (p = .02) and explained 6% of the variance in team performance. Of all three subscales, TMS coordination was the only significant variable, with higher TMS coordination scores associated with better team performance (p = .01).
Model 2 included the addition of psychological safety. This model was highly significant (p < .001) and explained 20% of the variance in team performance, a significant increase of 14% on model 2 (R2 Change = .14, p < .001). Within this model, psychological safety was the best predictor of team performance, with greater psychological safety being significantly associated with better team performance (p < .001). TMS coordination was no longer significantly associated with team performance once psychological safety was included in the model (p = .23). However, TMS credibility did show a significant negative relationship with team performance, with lower reported TMS credibility associated with better team performance.
Model 3 included the addition of interpersonal conflict. This model was highly significant (p < .001) and explained 23% of the variance in team performance, a significant increase of 4% (R2 Change=.04, p = .02). Within this model, psychological safety, interpersonal conflict and TMS credibility were all significantly associated with team performance. Better team performance was associated with greater psychological safety (p = .005), lower interpersonal conflict (p = .02) and lower reported TMS credibility (p = .03).
Model 4 included the addition of interaction effects between predictor variables (TMS*Psychological Safety and TMS*Interpersonal conflict). This model was again highly significant (p < .001) and explained 25% of the variance in team performance, a non-significant increase of 3% (R2 Change = .03, p = .14). Neither interaction effect was significant (p>.05), suggesting that neither psychological safety or interpersonal conflict moderate the relationship between TMS and team performance in this model. However, the interaction effect for psychological safety did approach significance (p = .06).
Discussion
The aim of this study was to investigate how psychological and cultural factors affect team performance and the relationship between TMS and team performance in hospital ward teams. The findings revealed that better team performance was predicted by teams feeling psychologically safe, experiencing low levels of interpersonal conflict and relying less on other team members’ knowledge. Although psychological safety and interpersonal conflict were independent predictors of team performance, and mediated the relationship between the TMS subscale coordination and team performance, they did not moderate the relationship between TMS and team performance.
More effective Transactive Memory Systems (TMS), specifically, coordination of knowledge between team members did predict better team performance. However, this relationship was weak and TMS explained only a small proportion (6%) of the variance in team performance. Psychological safety was a much stronger predictor of performance than TMS, explaining an additional 13% of the variance. Interpersonal conflict was also a significant predictor of performance adding a further 4% of predictive power to the model. Furthermore, when controlling for cultural factors, low TMS credibility predicted better team performance. The relationship between TMS and team performance was not moderated by interpersonal conflict. Although not significant, psychological safety did approach significance (p = .06) and a study with a larger sample size is required to examine this relationship further. The present results suggest that, within this context where teams are less well defined, TMS may not be particularly helpful for understanding team performance. These findings highlight the critical role team culture plays in team performance in ward teams in hospital settings.
In line with previous studies across a range of professional domains (Kim, Mu, and Moon Citation2018; Ren and Argote Citation2011; Bachrach et al. Citation2019; DeChurch and Mesmer-Magnus Citation2010), we found that effective TMS was a significant, albeit weak, predictor of team performance. Specifically, the TMS subscale coordination, which evaluates the ability of a team to work together to accomplish tasks in a coordinated and efficient way, was a significant predictor of better team performance. Our findings suggest that TMS predicted approximately 6% of the variance in team performance, which is a similar proportion to that identified in previous meta-analyses across a variety of professional domains (e.g. 7% (DeChurch and Mesmer-Magnus Citation2010)). TMS appears to have limited predictive power while more specific variables, such as psychological safety and interpersonal conflict, that focus on specific aspects of communication have greater explanatory power. These findings are important for informing future interventions for improving healthcare teamwork.
Interestingly, when psychological safety and interpersonal conflict were controlled for, the TMS subscale of coordination was no longer a significant predictor of team performance, and the TMS subscale of credibility (i.e. the reliability of other members’ knowledge) became significant but with a negative relationship to team performance (i.e. low TMS credibility predicted better team performance). The negative relationship between TMS credibility and team performance may seem counterintuitive, but one possible explanation might be that critiquing and questioning the knowledge or expertise of other team members, rather than just trusting that it is reliable, might lead to better performance. Teams in which members change constantly, teamwork is episodic and team structures are ill defined, such as those found in wards, might experience weaker TMS and compensatory behaviours are therefore used, such as not implicitly relying on team members’ untested knowledge. Offering support to this hypothesis, empirical studies in healthcare have found the ability of staff to question the performance of team members is related to better team performance (Kolbe et al. Citation2012), a finding confirmed in this study. This relationship warrants further in depth investigation in healthcare teams of different types.
Although we gathered data on whether team members based their responses of working in a uni or multi professional team we were unable to use this as a variable in the regression models because of the sample size. Nevertheless, we found that multi-professional team members reported higher levels of psychological safety and higher TMS scores than uni-professional team members. This was unexpected and there are a number of potential explanations. Higher psychological safety in multi professional teams could indicate a greater ability to contribute professional expertise in a team where other professionals rely on that expertise and expect to receive it. Similarly, the presence of different professional groups could assist TMS formation because the knowledge and expertise held by different professions is more easily identified than in teams where all members have the same training and knowledge base. Previous studies have identified team and professional identity as important mediators of the relationship between TMS and communication quality, but this was based on measures of social identity, which we did not use in this study (Liao et al. Citation2015). The relationship between TMS and team structures and membership is a promising avenue for future research.
Overall, the findings suggest that better team performance is predicted independently by high levels of psychological safety, low levels of interpersonal conflict and low reliance on team members’ untested knowledge (TMS credibility). Interventions to improve teamwork will have to consider how to improve team culture and psychological safety alongside being mindful of the ability of teams to develop a shared cognitive system. However, constantly changing membership, episodic teamwork, and loose team structures, such as experienced in healthcare, may inhibit the development of effective TMS. Questioning colleagues may be a more effective technique for high performance than trusting their expertise, and this questioning is facilitated by psychological safety and low interpersonal conflict. There may be other healthcare settings, such as primary care or mental health inpatient wards in which team membership is more consistent and teams can more effectively develop a shared cognitive system such as TMS.
Implications and recommendations
The study showed that TMS is only weakly related to team performance and psychological safety and interpersonal conflict are more strongly related to performance. Our findings stress the importance of feeling psychologically safe and having low interpersonal conflict for healthcare teams to be effective, along with not assuming the expertise of team members. We interpret the results as indicative of the limits of the TMS construct in understanding teams in which there may be reduced opportunity to develop the knowledge required for an effective TMS. Improving the performance of such teams may require psychological safety to allow team members to question and challenge each other in the absence of intimate knowledge of team members’ abilities. These findings underline the importance of understanding the unique characteristics of healthcare teams that might make generalising from research in other domains risky.
In reality, healthcare professionals frequently find it difficult to communicate effectively with colleagues and speak up when lapses occur, suggesting a lack of psychological safety in current practice (Schwappach and Gehring Citation2015; Schwappach and Richard Citation2018; Martinez et al. Citation2017). There are a number of factors that may be contributing to this. Firstly, the influence of hierarchies and power dynamics (Morrow et al. Citation2016) both within and between professional silos, that inhibit communication and create a barrier to effective TMS development (Kotlarsky, van den Hooff, and Houtman Citation2015; Hollingshead et al. Citation2010). Nurses and junior doctors are particularly vulnerable to the effects of hierarchy within healthcare teams (Martinez et al. Citation2017; Morrow, Gustavson, and Jones Citation2016; Okuyama, Wagner, and Bijnen Citation2014). Secondly, tightening budgets and increasing patient demands mean hospitals are prioritising space for clinical use at the expense of staff protected spaces and moving away from traditional ward based team structures towards more transient and episodic teamworking (Chesluk et al. Citation2015). As a result, opportunities for staff to communicate with each other outside of the pressurised clinical encounter are diminishing, which has been shown to impact TMS development (Liao, Jimmieson, and O’Brien Citation2012; Pearsall and Ellis Citation2006; Peltokorpi and Manka Citation2008; Pearsall, Ellis, and Bell Citation2010). Taken together, the current landscape of hospital teams limits both the quality and frequency of communication teams have, creating barriers to effective TMS development and team performance.
Organisations could take steps to improve their staff’s team performance, and in turn improve patient safety, by facilitating the development of psychological safety and a positive team culture within their organisation. One way this could be achieved is by providing non-clinical spaces for healthcare staff where they can engage in conversations with colleagues outside of the direct pressure of the clinical setting. Ensuring that adverse incidents are managed non-punitively is also likely to be important for increasing the likelihood of open communication in future. Finally, interprofessional teamwork training has been shown to facilitate the development of TMS (Moreland and Myaskovsky Citation2000). Senior team members could be supported to have a greater awareness of the role of hierarchy on team communication and performance, particularly with more junior team members.
Strengths and limitations
A strength of this study is the fact that participants were recruited from diverse hospital wards and professional groups. Furthermore, the instrument battery used valid and reliable survey instruments. A limiting feature of this study was the relatively small sample size, which precluded sub group analyses of ward type and team composition. A second limitation of this study is the reliance on self-report data, and the lack of an objective measure of team performance. However, identifying an objective measure of team performance for ward teams is challenging. There is no gold standard measure that could be applied to all teams. Perceived outcomes are commonly used in TMS research and other questionnaire studies (Bachrach et al. Citation2019) and can identify avenues for future studies. The present study provides an insight into staff experience of teamwork within this system.
Conclusions
This is one of the first studies to examine the influence of team culture and TMS on team performance in hospital ward teams where stakes are often high and poor teamwork can compromise patient safety and lead to harm (Rosen et al. Citation2018; Schmutz, Meier, and Manser Citation2019). In line with studies in other professional disciplines (Kim, Mu, and Moon Citation2018; Ren and Argote Citation2011; Bachrach et al. Citation2019; DeChurch and Mesmer-Magnus Citation2010), TMS explained only a small amount of the variance in team performance. High psychological safety, low interpersonal conflict, and not trusting team members’ expertise were predictors of better team performance, highlighting the importance of being able to challenge colleagues safely. These findings highlight the critical role of team culture in ensuring safer patient care in hospital settings. The findings suggest that interventions to create safe team environments and effectively manage interpersonal conflict should be considered as a means to improve healthcare teamwork.
Acknowledgements
ML, and this study, were supported by the NIHR Imperial Patient Safety Translational Research Centre (PSTRC). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Infrastructure support for this research was also provided by the NIHR Imperial Biomedical Research Centre (BRC). The team would like to sincerely thank Lily Roberts and Annaliza Sevillano for their support with data collection on this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Almost, J., A. C. Wolff, A. Stewart‐Pyne, L. G. McCormick, D. Strachan, and C. D'Souza. 2016. “Managing and Mitigating Conflict in Healthcare Teams: An Integrative Review.” Journal of Advanced Nursing 72 (7): 1490–1505. doi:https://doi.org/10.1111/jan.12903.
- Bachrach, D. G., K. Lewis, Y. Kim, P. C. Patel, M. C. Campion, and S. Thatcher. 2019. “Transactive Memory Systems in Context: A Meta-Analytic Examination of Contextual Factors in Transactive Memory Systems Development and Team Performance.” Journal of Applied Psychology 104 (3): 464. doi:https://doi.org/10.1037/apl0000329.
- Barki, H., and J. Hartwick. 2004. “Conceptualizing the Construct of Interpersonal Conflict.” International Journal of Conflict Management 15 (3): 216–244. doi:https://doi.org/10.1108/eb022913.
- Chesluk, B., E. Bernabeo, S. Reddy, L. Lynn, B. Hess, T. Odhner, and E. Holmboe. 2015. “How Hospitalists Work to Pull Healthcare Teams Together.” Journal of Health Organization and Management 29 (7): 933–947. doi:https://doi.org/10.1108/JHOM-01-2015-0008.
- De Dreu, C. K., and L. R. Weingart. 2003. “Task versus Relationship Conflict, Team Performance, and Team Member Satisfaction: A Meta-Analysis.” Journal of Applied Psychology 88 (4): 741. doi:https://doi.org/10.1037/0021-9010.88.4.741.
- DeChurch, L. A., and J. R. Mesmer-Magnus. 2010. “The Cognitive Underpinnings of Effective Teamwork: A Meta-Analysis.” Journal of Applied Psychology 95 (1): 32. doi:https://doi.org/10.1037/a0017328.
- Edmondson, A. 1999. “Psychological Safety and Learning Behavior in Work Teams.” Administrative Science Quarterly 44 (2): 350–383. doi:https://doi.org/10.2307/2666999.
- Hinds, P. J., and M. Mortensen. 2005. “Understanding Conflict in Geographically Distributed Teams: The Moderating Effects of Shared Identity, Shared Context, and Spontaneous Communication.” Organization Science 16 (3): 290–307. doi:https://doi.org/10.1287/orsc.1050.0122.
- Hollingshead, A. B., D. P. Brandon, K. Yoon, and G. Naina. 2010. “Communication and Knowledge-Sharing Errors in Groups.” In Communication and Organizational Knowledge, edited by H. E. Canary & R. D. McPhee, 133–150. London: Routledge.
- Jehn, K. A. 1997. “A Qualitative Analysis of Conflict Types and Dimensions in Organizational Groups.” Administrative Science Quarterly 42: 530–557. doi:https://doi.org/10.2307/2393737.
- Kessel, M., J. Kratzer, and C. Schultz. 2012. “Psychological Safety, Knowledge Sharing, and Creative Performance in Healthcare Teams.” Creativity and Innovation Management 21 (2): 147–157. doi:https://doi.org/10.1111/j.1467-8691.2012.00635.x.
- Kim, D., H. Mu, and T. Moon. 2018. “Impact of Transactive Memory Systems on Team Performance and the Moderating Effect of Joint Decision Making.” International Conference on Software Engineering, Artificial Intelligence, Networking and Parallel/Distributed Computing: Springer, 1–13.
- Kim, S. M., M. J. Kim, and S. J. Jo. 2021. “The Relationships between Perceived Team Psychological Safety, Transactive Memory System, Team Learning Behavior and Team Performance among Individual Team Members.” Leadership & Organization Development Journal 42 (6): 958–975. doi:https://doi.org/10.1108/LODJ-09-2020-0402.
- Kolbe, M., M. J. Burtscher, J. Wacker, B. Grande, R. Nohynkova, T. Manser, D. R. Spahn, and G. Grote. 2012. “Speaking up is Related to Better Team Performance in Simulated Anesthesia Inductions: An Observational Study.” Anesthesia & Analgesia 115 (5): 1099–1108. doi:https://doi.org/10.1213/ANE.0b013e318269cd32.
- Kotlarsky, J., B. van den Hooff, and L. Houtman. 2015. “Are we on the Same Page? Knowledge Boundaries and Transactive Memory System Development in Cross-Functional Teams.” Communication Research 42 (3): 319–344. doi:https://doi.org/10.1177/0093650212469402.
- Laschinger, H. K. S. 2014. “Impact of Workplace Mistreatment on Patient Safety Risk and Nurse-Assessed Patient Outcomes.” The Journal of Nursing Administration 44 (5): 284–290. doi:https://doi.org/10.1097/NNA.0000000000000068.
- Lazzara, E. H., L. E. Benishek, B. Patzer, M. E. Gregory, A. M. Hughes, K. Heyne, E. Salas, F. Kuchkarian, A. Marttos, and C. Schulman, 2015. “Utilizing Telemedicine in the Trauma Intensive Care Unit: does It Impact Teamwork? Telemedicine and eHealth 21 (8): 670–676.
- Lewis, K. 2003. “Measuring Transactive Memory Systems in the Field: Scale Development and Validation.” The Journal of Applied Psychology 88 (4): 587–604. doi:https://doi.org/10.1037/0021-9010.88.4.587.
- Liao, J., A. T. O'Brien, N. L. Jimmieson, and S. L. Restubog. 2015. “Predicting Transactive Memory System in Multidisciplinary Teams: The Interplay between Team and Professional Identities.” Journal of Business Research 68 (5): 965–977. doi:https://doi.org/10.1016/j.jbusres.2014.09.024.
- Liao, J., N. L. Jimmieson, and A. T. O’Brien. 2012. “Developing Transactive Memory Systems: Theoretical Contributions from a Social Identity Perspective.” Group & Organization Management 37 (2): 204–240. doi:https://doi.org/10.1177/1059601112443976.
- Martinez, W., L. S. Lehmann, E. J. Thomas, J. M. Etchegaray, J. T. Shelburne, G. B. Hickson, D. W. Brady, A. M. Schleyer, J. A. Best, N. B. May, and S. K. Bell. 2017. “Speaking up about Traditional and Professionalism-Related Patient Safety Threats: A National Survey of Interns and Residents.” BMJ Qual Saf 26 (11): 869–880. doi:https://doi.org/10.1136/bmjqs-2016-006284.
- Michinov, E., E. Olivier-Chiron, E. Rusch, and B. Chiron. 2008. “Influence of Transactive Memory on Perceived Performance, Job Satisfaction and Identification in Anaesthesia Teams.” British Journal of Anaesthesia 100 (3): 327–332. doi:https://doi.org/10.1093/bja/aem404.
- Moreland, R. L., and L. Myaskovsky. 2000. “Exploring the Performance Benefits of Group Training: Transactive Memory or Improved Communication?” Organizational Behavior and Human Decision Processes 82 (1): 117–133.
- Morrow, K. J., A. M. Gustavson, and J. Jones. 2016. “Speaking up Behaviours (Safety Voices) of Healthcare Workers: A Metasynthesis of Qualitative Research Studies.” International Journal of Nursing Studies 64: 42–51. doi:https://doi.org/10.1016/j.ijnurstu.2016.09.014.
- O'Donovan, Róisín, and Eilish McAuliffe. 2020. “Exploring Psychological Safety in Healthcare Teams to Inform the Development of Interventions: Combining Observational, Survey and Interview Data.” BMC Health Services Research 20 (1): 810. doi:https://doi.org/10.1186/s12913-020-05646-z.
- Okuyama, A., C. Wagner, and B. Bijnen. 2014. “Speaking up for Patient Safety by Hospital-Based Health Care Professionals: A Literature Review.” BMC Health Services Research 14 (1): 1–8.
- Ong, Y. H., M. Y. H. Koh, and W. S. Lim. 2020. “Shared Leadership in Interprofessional Teams: Beyond Team Characteristics to Team Conditions.” Journal of Interprofessional Care 34 (4): 444–452. doi:https://doi.org/10.1080/13561820.2019.1653834.
- Pearsall, M. J., A. P. Ellis, and B. S. Bell. 2010. “Building the Infrastructure: The Effects of Role Identification Behaviors on Team Cognition Development and Performance.” The Journal of Applied Psychology 95 (1): 192. doi:https://doi.org/10.1037/a0017781.
- Pearsall, M. J., and A. P. Ellis. 2006. “The Effects of Critical Team Member Assertiveness on Team Performance and Satisfaction.” Journal of Management 32 (4): 575–594. doi:https://doi.org/10.1177/0149206306289099.
- Peltokorpi, V., and A. C. Hood. 2019. “Communication in Theory and Research on Transactive Memory Systems: A Literature Review.” Topics in Cognitive Science 11 (4): 644–667. doi:https://doi.org/10.1111/tops.12359.
- Peltokorpi, V., and M-L. Manka. 2008. “Antecedents and the Performance Outcome of Transactive Memory in Daycare Work Groups.” European Psychologist 13 (2): 103–113. doi:https://doi.org/10.1027/1016-9040.13.2.103.
- Rau, D. 2005. “The Influence of Relationship Conflict and Trust on the Transactive Memory: Performance Relation in Top Management Teams.” Small Group Research 36 (6): 746–771. doi:https://doi.org/10.1177/1046496405281776.
- Ren, Y., and L. Argote. 2011. “Transactive Memory Systems 1985–2010: An Integrative Framework of Key Dimensions, Antecedents, and Consequences.” Academy of Management Annals 5 (1): 189–229. doi:https://doi.org/10.5465/19416520.2011.590300.
- Rosen, M. A., D. DiazGranados, A. S. Dietz, L. E. Benishek, D. Thompson, P. J. Pronovost, and S. J. Weaver. 2018. “Teamwork in Healthcare: Key Discoveries Enabling Safer, High-Quality Care.” American Psychologist 73 (4): 433. doi:https://doi.org/10.1037/amp0000298.
- Rosenstein, A. H. 2011. “The Quality and Economic Impact of Disruptive Behaviors on Clinical Outcomes of Patient Care.” American Journal of Medical Quality 26 (5): 372–379. doi:https://doi.org/10.1177/1062860611400592.
- Salas, E., D. E. Sims, and C. S. Burke. 2005. “Is There a “Big Five” in Teamwork?” Small Group Research 36 (5): 555–599.
- Schmutz, J. B., L. L. Meier, and T. Manser. 2019. “How Effective is Teamwork Really? The Relationship between Teamwork and Performance in Healthcare Teams: A Systematic Review and Meta-Analysis.” BMJ Open 9 (9): e028280. doi:https://doi.org/10.1136/bmjopen-2018-028280.
- Schwappach, D., and A. Richard. 2018. “Speak up-Related Climate and Its Association with Healthcare Workers’ Speaking up and Withholding Voice Behaviours: A Cross-Sectional Survey in Switzerland.” BMJ Qual Saf 27 (10): 827–835. doi:https://doi.org/10.1136/bmjqs-2017-007388.
- Schwappach, D., and K. Gehring. 2015. “Frequency of and Predictors for Withholding Patient Safety Concerns among Oncology Staff: A Survey Study.” European Journal of Cancer Care 24 (3): 395–403. doi:https://doi.org/10.1111/ecc.12255.
- Tan, K. T., F. B. B. Adzhahar, I. Lim, M. Chan, and W. S. Lim. 2014. “Transactive Memory System as a Measure of Collaborative Practice in a Geriatrics Team: Implications for Continuing Interprofessional Education.” Journal of Interprofessional Care 28 (3): 239–245. doi:https://doi.org/10.3109/13561820.2014.901938.
- Wegner, D. M. 1987. “Transactive Memory: A Contemporary Analysis of the Group Mind.” In Theories of Group Behavior, edited by B. Mullen and G. R. Goethals, 185–208. Cham: Springer.
- Whelan, E., and R. Teigland. 2013. “Transactive Memory Systems as a Collective Filter for Mitigating Information Overload in Digitally Enabled Organizational Groups.” Information and Organization 23 (3): 177–197. doi:https://doi.org/10.1016/j.infoandorg.2013.06.001.
