Abstract
Ambient cold exposure can pose health risks, and this study was aimed at investigating associations with musculoskeletal disorders. A postal survey was performed on 12,627 men and women, ages 18–70 years, living in northern Sweden. Statistical associations were determined using multiple logistic regression. The study sample consisted of 6,886 women (54.5%), and 5,741 men. Reporting high occupational ambient cold exposure was statistically significantly associated with neck pain (OR 1.36; 95% CI 1.16–1.59), low back pain (OR 1.38; 95% CI 1.17–1.63), and lumbar radiculopathy (OR 1.36; 95% CI 1.07–1.73), after adjusting for age, gender, body mass index, physical work load, daily smoking, and stress. We conclude that ambient cold exposure during work was an independent predictor of neck pain, low back pain, and lumbar radiculopathy. In occupational health care settings, cold exposure should be recognised as a possible risk factor for musculoskeletal disorders.
Practitioner summary: This cross-sectional, survey-based study investigated associations between self-reported occupational ambient cold exposure and musculoskeletal disorders. It showed significant associations between high cold exposure and neck pain, low back pain and lumbar radiculopathy. In occupational health care settings, cold exposure should be recognised as a possible risk factor for musculoskeletal disorders.
1. Introduction
1.1. Musculoskeletal disorders
Pain in the neck and lower back are common musculoskeletal disorders (MSD) that frequently cause disability and sick leave (Aasmoe et al. Citation2008). In Western countries, such conditions have been reported to be among the most costly health problems in society (Hellsing, Linton, and Kälvemark Citation1994). Previously, MSD have been defined as all complaints referring to muscles, joints, tendons, ligaments, and bones (Pienimäki Citation2002). Pain that accompanies such conditions can be classified as either nociceptive, nociplastic or neuropathic (Shraim, Massé-Alarie, and Hodges Citation2021). Common neck and low back pain are normally of nociceptive origin, while lumbar radiculopathy (or sciatica) is mainly a neuropathic condition. Suffering from long-standing MSD can affect the quality of life as well as the work ability (Dueñas et al. Citation2016; Sormunen et al. Citation2009). Therefore, it is important to study occupational risk factors for such conditions. Several systematic reviews have covered this topic, and concluded on physical as well as psychological and organisational risk factors (Horsley Citation2011; Farioli et al. Citation2014). However, there is a growing body of evidence indicating that effects of occupational cold exposure should also be taken into consideration.
1.2. Occupational cold exposure
Occupational cold exposure has been defined as being subjected to ambient temperatures at or below 10 °C (International Organization for Standardization Citation2008). However, since cold exposure is modified by wind, humidity, heat radiation, clothing, and individual factors (e.g. body composition), exposure estimates can also be based on the subjective experience of being cold-exposed, regardless of actual ambient temperature (Mäkinen et al. Citation2006). For MSD, the effects of contact cold have been emphasised, e.g. for workers in fish- or meat-processing industries (Aasmoe et al. Citation2008; Pienimäki Citation2002). Swedish official statistics report that about 22% of men and 13% of women are occupationally exposed to a cold climate for at least one quarter of the working hours (The Swedish Work Environment Agency Citation2018). Another report states that more than 350,000 people in Sweden are occupationally exposed to a cold climate for more than half of their time spent working (Hassi et al. Citation2002). Thus, the working population is commonly subjected to ambient cold, and there is rising concern that such exposure can have an underestimated negative effect on the musculoskeletal system (Mäkinen and Hassi Citation2009).
1.3. Previous knowledge on cold exposure effects
A Finnish study on the general population reported cold-related musculoskeletal pain in 32% of men and 28% of women (Pienimäki et al. Citation2014). Such symptoms have been reported to be twice as common among those with established MSD compared to healthy individuals (Näyhä et al. Citation2011), and subjects with low back disorders seem to be especially vulnerable (Pienimäki et al. Citation2014; Lewis, Souvlis, and Sterling Citation2010). In Norway, a large population-based survey found that working in a cold environment was associated with long-standing MSD (Farbu et al. Citation2019). In prospective analyses, cold work was also associated with future MSD (Farbu et al. Citation2021). To the authors’ knowledge, no large community-based surveys on the topic have been performed in Sweden.
Looking at distinct sites of pain in the locomotor system, a narrative review from 2002 on ten scientific articles reported on several studies that indicated an association between cold work and low back pain (Pienimäki Citation2002). Data on neck pain was scarce, and only one study had investigated effects on lumbar disc diseases (Elsner, Nienhaus, and Beck Citation1997). Another review from the same year, based on 27 scientific articles, described the epidemiological evidence for cold-related MSD as very weak, and called for further studies (Hildebrandt et al. Citation2002). Since then, the association between cold exposure and low back pain has been further substantiated (Aasmoe et al. Citation2008; Sormunen et al. Citation2009; Burström et al. Citation2013; Dovrat and Katz-Leurer Citation2007; Skandfer et al. Citation2014), and the evidence for an association to neck pain strengthened by several studies (Aasmoe et al. Citation2008; Sormunen et al. Citation2009; Burström et al. Citation2013). However, the associations with lumbar disc herniation and radiculopathy have not been further elucidated. Many of the studies in this field have small sample sizes, and focus on specific occupational groups, and this limits the generalisability of results. Also, most studies have studied artificially cooled indoor environments, which in Sweden is much rarer than outdoor exposure. Finally, the gender perspective is not always considered. Some papers only focus on male workers, while other acknowledge that the ergonomic exposure as well as the susceptibility to a cold environment may differ between genders (Sormunen et al. Citation2009). Thus, there is a need for large-scale community-based studies including both men and women, also taking outdoor exposure into account, and adjusting for ergonomic exposures.
1.4. Aims
The primary aim of the study was to determine the statistical association between occupational ambient cold exposure and neck pain, low back pain, and lumbar radiculopathy among subjects of working age, living in northern Sweden. The secondary aims were to investigate any presence of an exposure-response pattern, gender differences, and effects of leisure-time ambient cold exposure.
2. Materials and methods
2.1. Study design and setting
This cross-sectional questionnaire-based study was part of the Cold and Health In Northern Sweden (CHINS) research project, which was initiated in 2015 to broadly explore adverse health effects from ambient cold exposure, and has previously been described in detail (Stjernbrandt et al. Citation2017). The survey was initiated on the fifth of February 2015 and ended on the fifth of May 2015, and no reminder to respond was administered.
2.2. Participants
The study sample included men and women between 18–70 years, living in northern Sweden, who were drawn from the national Swedish population register. The postal survey collected data on MSD, in addition questions on anthropometry, general health status, tobacco habits, and occupation (Supplementary data 1). There was no economical compensation or any other incentive to respond to the survey. The study protocol was approved by the Regional Ethical Review Board situated at Umeå University (DNR 2014-286-31 M).
2.3. Variables and statistical analyses
Since continuous variables were not normally distributed, data were described as median values and interquartile ranges (IQR), while categorical variables were presented as numbers and valid percentages. Dependent variables were: neck pain (‘Do you have aching/pain in your neck/shoulders?’); low back pain (‘Do you have aching/pain in your low back?’); and lumbar radiculopathy [‘Do you have pain that radiates from the back to below the knees (sciatica)?’]. The answers were given on a four-grade scale, as ‘none’, ‘insignificant’, ‘somewhat’, or ‘a lot’. Answering ‘a lot’ was considered a positive response. No onset or duration of symptoms was recorded. Occupational or leisure-time ambient cold exposure were assessed by two questionnaire items: ‘During work I am exposed to outdoor or cold environments’; and ‘During leisure time I am exposed to outdoor or cold environments’. The answers were given on whole number numerical rating scales (NRS), ranging from one (‘do not agree’) to ten (‘fully agree’). Correlation between scales was investigated using Spearman’s rank correlation coefficient (rs). Cold exposure was categorised by tertiles, and body mass index (BMI) by clinically used thresholds for under- and overweight. Geographical location, as determined by postal code, was divided into three groups (coastal/inland/alpine), and previous diseases grouped into either cardiovascular diseases (hypertension, angina pectoris, myocardial infarction, or stroke), pulmonary diseases (asthma, or chronic obstructive pulmonary disease), or joint diseases (e.g. osteoarthritis). Current occupation was specified in free-form text, and manually coded in accordance with the International Standard Classification of Occupations (ISCO) (International Labour Organization Citation2012). The major ISCO categories were grouped into manual work (armed forces occupations, skilled agricultural, forestry and fishery workers, crafts and related trades workers, plant and machine operators and assemblers, elementary occupations, and self-employed), or desk work (managers, professionals, clerical support workers, and service and sales workers). Physical work load was determined by a job–exposure matrix that categorised the exposure into low, medium or high, based on the two-level ISCO coding (Supplementary data 2). Binary logistic regression was used for simple and multiple regression analyses. Independent variables used for adjusting were: age (years); gender (male/female), BMI (kg/m2); physical work load (low/medium/high); daily smoking (yes/no); and stress (low/high). A p value <0.05 was considered statistically significant. Statistical analyses were performed using SPSS (version 27.0, IBM Corporation, Armonk, NY, USA).
3. Results
3.1. Recruitment
The study population consisted of 12,627 subjects (response rate 35.9%). A previously published non-responder analysis based on the sampling frame showed that the response rate was slightly higher among women than men, and increased with age (Stjernbrandt et al. Citation2017).
3.2. Descriptive data
The study population consisted of 6,886 women (54.5%), and 5,741 men (45.5%), with a median age of 54 (IQR 23), and median BMI of 25.5 (IQR 5). Neck pain was reported by 2,225 (17.9%), low back pain by 2,031 (16.4%), and lumbar radiculopathy by 873 (7.0%).
In the study population, 2,284 (18.8%) were retired, 678 (5.6%) were students, 239 (2.0%) unemployed, 173 (1.4%) on sick leave, and 65 (0.5%) on parental leave. Among the non-working subjects, the occurrence of neck pain did not differ from those working (18.3%; p = 0.39), while there was a significantly higher occurrence of low back pain, and lumbar radiculopathy among non-workers (19.6% and 8.9%, respectively; p < 0.01 for both). A further 448 subjects (3.6%) had not specified their current occupation. Since non-working subjects had no occupational ambient cold exposure, they were excluded from analyses regarding occupational cold exposure, leaving 8,740 currently working study participants. In this group, 4,098 (46.9%) performed manual work while 4,642 (53.1%) mainly held desk jobs. Among the manual workers, the job–exposure matrix (Supplementary data 2) revealed that 1,819 (44.4%) had a medium physical load (i.e. ambulatory work), while 2,279 (55.6%) had a high load (e.g. heavy lifting or climbing).
Among those in the highest occupational ambient cold exposure tertile (NRS 6–10; N = 1,958), there was a predominance of men (N = 1,248; 63.7%), and the median age was lower than in the sample as a whole (median 49; IQR 21). Among highly occupationally cold-exposed men, the three most common occupations were drivers of heavy equipment (15.5%), construction workers (13.0%), and technicians (9.1%). The corresponding categories for women were teachers (e.g. in pre-school; 30.0%), care workers (27.0%), and agricultural workers (4.9%). Other descriptive data can be found in .
Table 1. Characteristics of the working study population (N = 8,740), separated by level of occupational cold exposure.
3.3. Effects of occupational exposure
In simple analyses, there were statistically significant associations between high occupational ambient cold exposure (NRS 6–10) and low back pain (OR 1.27; 95% CI 1.10–1.47), and lumbar radiculopathy (OR 1.35; 95% CI 1.09–1.67), but not for neck pain (OR 1.14; 95% CI 0.99–1.31). In the multiple analyses, high occupational ambient cold exposure was a significant predictor for all three outcomes after adjusting for age, gender, BMI, physical workload, daily smoking, and stress (). There was a general trend towards higher point estimates for all three outcomes with increasing exposure tertiles, and this was also seen when analysing exposure with a higher resolution, using the ten-degree NRS ().
Figure 1. Associations between occupational ambient cold exposure and neck pain, low back pain, and lumbar radiculopathy, based on the fully adjusted regression model for currently working subjects (N = 8,740).
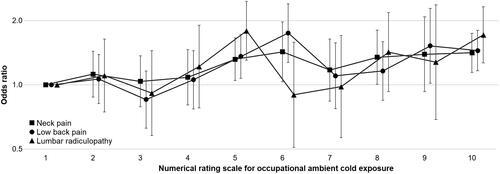
Table 2. Multiple logistic regression for neck pain, low back pain, and lumbar radiculopathy, among working subjects (N = 8,740).
3.4. Gender differences
Neck pain was more commonly reported by women (22.3%) than men (12.1%), as was low back pain, and lumbar radiculopathy (18.5% versus 11.3%, and 7.1% versus 5.3%, respectively). When reiterating the multiple logistic regression model, stratified by gender instead of using it as a covariate, high occupational ambient cold exposure (NRS 6–10) was not significantly associated with neck pain among women (OR 1.16; 95% CI 0.91–1.37), but was significantly associated among men (OR 1.81; 95% CI 1.39–2.35). For low back pain, both women (OR 1.32; 95% CI 1.06–1.64) and men (OR 1.38; 95% CI 1.06–1.79) had significant associations. Finally, for lumbar radiculopathy, neither were significantly associated (OR 1.24; 95% CI 0.89–1.72, and OR 1.39; 95% CI 0.96–2.02, respectively).
3.5. Effects of leisure-time exposure
There was a low correlation between occupational and leisure-time ambient cold exposure (rs = 0.27; p < 0.01). The multiple logistic regression model was reiterated, analysing all subjects (N = 12,627), and using leisure-time instead of occupational cold ambient exposure (based on similar categorisation into tertiles). However, reporting a high leisure-time ambient cold exposure (NRS 8–10) was not associated with neck pain (OR 1.10; 95% CI 0.95–1.28), low back pain (OR 1.01; 95% CI 0.86–1.18), or lumbar radiculopathy (OR 1.15; 95% CI 0.91–1.44).
4. Discussion
4.1. Main findings and interpretation
Reporting high occupational ambient cold exposure was statistically significantly associated with neck pain, low back pain, and lumbar radiculopathy in a multiple logistic regression model. There was a trend towards a dose-effect pattern where increasing cold exposure indicated higher point estimates for reporting the outcomes. In gender-specific analyses, only low back pain was associated with high occupational cold exposure for both men and women. Leisure-time cold exposure was not significantly associated with any of the outcomes.
The occurrence of either neck or back pain in the present study (40.8% of women, and 23.4% of men) was comparable to official Swedish statistics, reporting that 45% of women, and 28% of men have recurrent pain in the neck or back (The Swedish Work Environment Agency Citation2018). Since there were no questions on onset or duration of pain in the present study, it cannot be concluded on whether the symptoms were short- or long-term. However, a previous prospective study on neck and back pain in Sweden reported that such symptoms are often recurring, and become chronic (>3 months duration) in about 13% of cases (Hellsing, Linton, and Kälvemark Citation1994). Regarding exposure, the occupations with high ambient cold exposure in the present study have also recently been reported to be heavily cold exposed in official Swedish statistics, i.e. professional drivers and construction workers among men; and teachers and care workers among women (The Swedish Work Environment Agency Citation2018). This underscores gender-dependent differences in occupational cold exposure, and that occupational health surveillance systems, and efforts to reduce cold exposure, should not only be focussed on traditionally male-dominated manual occupations but also on jobs with a predominance of female workers. In a previous report, the mean monthly temperature in northern Sweden during winter-time spanned from −9 to 5 °C (Stjernbrandt et al. Citation2017), indicating that ambient cold exposure in this region can be much more intensive than the limit in the definition of occupational cold exposure (International Organization for Standardization Citation2008), which emphasises the relevance of this workplace hazard in this context.
The present study reported occupational ambient cold exposure as an independent predictor of neck pain (OR 1.36; 95% CI 1.16–1.59), and low back pain (OR 1.38; 95% CI 1.17–1.63), after adjusting for age, gender, BMI, physical work load, daily smoking, and stress. The covariates were determined by the authors’ preunderstanding of risk factors based on the previous literature, and not on a data-driven approach. The results can be compared with previous Scandinavian studies, all using different strategies to determine the association between cold exposure and neck and back pain. In a Swedish study on male construction workers (N = 134,754), working in a cold climate was associated with work-hindering neck pain (OR 1.48; 95% CI 1.24–1.76), and low back pain (OR 1.19; 95% CI 1.06–1.35), after adjusting for age, BMI, and tobacco use (Burström et al. Citation2013). The authors suggested that the higher OR for neck pain might be due to the fact that the neck is less protected from cold and draught. In a laboratory setting, such factors have also been shown to induce increased resting activity in neck muscles (Sundelin and Hagberg Citation1992), supporting this theory. In a Norwegian population-based study (N = 6,553), working in a cold environment was associated with neck pain lasting three months or more (OR 1.46; 95% CI 1.13–1.89), but not back pain (OR 1.18, 95% CI 0.91–1.52), after adjusting for age, gender, smoking, educational level, physical activity level, and insomnia (Farbu et al. Citation2019). In a prospective study based on the same sample (N = 2,347), working in a cold environment at baseline was associated with MSD lasting three months or more, seven to eight years later (incidence rate ratio 1.15; 95% CI 1.03–1.29) (Farbu et al. Citation2021). However, anatomical location was not specified. Further, in a study on the Norwegian seafood production industry (N = 1,767), often being cold at work was associated with reporting neck and back pain (Bang et al. Citation2005). In a sub-sample of manual workers from the same study (N = 873), such cold exposure was associated with both neck pain (OR 10.5; 95% CI 3.1–35.3), and back pain (OR 11.0; 95% CI 4.5–26.8), after adjusting for age, gender, smoking, educational level, and duration of work (Aasmoe et al. Citation2008). Finally, in a Finnish study on men and women in the food-processing industry (N = 1,117), extensive cooling was associated with neck pain (OR 6.47; 95% CI 2.79–14.99), and low back pain (OR 5.76; 95% CI 2.93–11.31), after adjusting for gender, physical activity level, duration of work, BMI, and perceived work ability (Sormunen et al. Citation2009).
Research on the topic have also been performed outside of Scandinavia. In a study on Russian mine workers (N = 3,530), working in cold conditions (<10 °C) was associated with reporting low back pain (OR 1.82; 95% CI 1.55–2.15) , after adjusting for gender, BMI, duration of work, physical fitness level, and stress (Skandfer et al. Citation2014). In a study on Israeli male workers in the frozen food industry (N = 122), working at temperatures <20 °C was associated with back symptoms at work (OR 4.11; 95% CI 1.30–12.78), after adjusting for age, smoking, educational level, job satisfaction, and type of work task (Dovrat and Katz-Leurer Citation2007). There was also a significantly higher occurrence of neck pain among cold store workers compared to those working at room temperature, but the effect size was not specified. In a Colombian study on meat-processing plant workers (N = 162), being cold-exposed at work was associated with neck pain [prevalence ratio (PR) 3.36; 95% CI 1.75–6.44], and low back pain (PR 2.24, 95% CI 1.52–3.92) (Piedrahı́ta, Punnett, and Shahnavaz Citation2004). Finally, in a Turkish study on ammunition factory workers (N = 955), neck and low back pain was common, especially among men (Pinar et al. Citation2013). In a multiple logistic regression model, being exposed to cold during work was associated with MSD (OR 1.84; 95% CI 1.37–2.47), after adjusting for BMI, smoking, duration of work, physical work load, vibration exposure, and chronic diseases. Of note, 11.4% of low back pain was actually considered discopathy or radiculopathy. The present study also included lumbar radiculopathy, which was associated with high occupational ambient cold exposure (OR 1.36; 95% CI 1.07–1.73) in the multiple model. To the authors’ knowledge, there is only one previous study that has focussed separately on this outcome, and that was a German case-control study on men and women (N = 587) attending an orthopaedic outpatient clinic. In that study, working in a cold environment was associated with degenerative lumbar disc disease in men (OR 2.20; 95% CI 1.30–3.72), but not in women (OR 1.60; 95% CI 0.78–3.31) (Elsner, Nienhaus, and Beck Citation1997).
It is hard to compare effect sizes since both exposure and outcomes are defined differently between studies. Mandating chronic, work-related, or work-hindering pain can be more specific, and result in larger effect sizes. Differences in statistical approaches, and selection of covariates also affect the estimated strength of the relations. However, it is important to point out that all studies point in the same direction, showing increases in odds, prevalence, or incidence rate ratios for neck and back pain among subjects working in cold environments.
The mechanisms behind cold-induced pain in the neck and back are obscure, but several theories have been put forward. Cold-induced vasospasm has been reported to be more frequent among subjects with chronic low back pain compared to healthy individuals, and correlated to the pain intensity (Lapossy et al. Citation1994). Thus, one plausible mechanism could be that reduced muscular blood flow induces ischaemic nociceptive pain during situations with high physical demands. Other suggested mechanistic explanations include an increased muscular tone at rest, and reduced contractive force during physical demands, inducing fatigue (Burström et al. Citation2013; Dovrat and Katz-Leurer Citation2007; Skandfer et al. Citation2014; Oksa, Rintamäki, and Rissanen Citation1997). Also, local cooling may negatively affect the biomechanical properties of the supportive tissues (Racinais and Oksa Citation2010). Finally, cold-induced central sensitisation could possibly augment pain responses (Sundstrup et al. Citation2015). For lumbar disc disease, it has been postulated that cooling may affect the diffusion of fluid in the intervertebral space, when combined with heavy work (Hildebrandt et al. Citation2002). This could increase the risk of lumbar disc herniation and nerve root compression, resulting in neuropathic pain. Being overweight has been reported to reduce the risk of cold-related complaints, due to an insulatory effect (Pienimäki et al. Citation2014). On a final note, personal protective equipment (e.g. heavy caps and coats), used to protect the worker from ambient cold, may increase the physical workload, affect posture, and hinder movements, thus contributing to the development of MSD (Dovrat and Katz-Leurer Citation2007; Piedrahı́ta, Punnett, and Shahnavaz Citation2004).
In the gender-based subgroup analyses in the present study, all three outcomes were more commonly reported among women, but only low back pain was associated with occupational ambient cold exposure for both men and women, when analysed separately. However, an important caveat is that the study was not fully statistically powered to determine gender effects. In other research, female gender, as well as increasing age, have been reported to be susceptibility factors for cold-induced discomfort (Sormunen et al. Citation2009). Such gender differences have been suggested to be due to differences in work task exposure, expression of symptoms, coping strategies, and biological susceptibility (Sormunen et al. Citation2009). The reasons for occupational ambient cold exposure being a stronger predictor for MSD than leisure-time exposure are not known. Possible explanations could be that occupational exposure is generally of longer duration, demands a higher physical activity level, and cannot easily be avoided during severe cold conditions. Another possible difference is that leisure-time exposure is voluntary, and might be refrained from among subjects with current MSD.
4.2. Limitations
There are several limitations in the present study. First of all, the response rate was low, which may have affected the generalisability of results. However, a previously published responder analysis only showed minor distortions compared to the sampling frame (Stjernbrandt et al. Citation2017). Also, a recent review concluded that survey response rates are only weakly associated with demographic representativeness (Hendra and Hill Citation2019). Other authors have stated that large-scale population-based recruitment strategies may provide good generalisability despite low response rates, if sources of sampling bias are limited (Blair and Zinkhan Citation2006), which was believed to be the case in the present study. Another potential limitation is the subjective exposure assessments, that was based on scales that have not been validated. However, previous studies have shown no clear association between actual objective measurements of air temperature and velocity in relation to the subjective experience of being cold (Bang et al. Citation2005). Ambient factors are also modified by clothing and body composition, among other factors. Therefore, self-reported data can be justified, and has been used by several other authors (Aasmoe et al. Citation2008; Sormunen et al. Citation2009). Further, a more detailed ergonomic exposure assessment, using validated questionnaire items, would likely have been more specific than the simple job–exposure matrix employed in this study. The outcomes were also self-reported, and it is possible that the accuracy would have been improved by demanding physician-diagnosed conditions, or using health care registers for diagnoses. However, this was beyond the scope of the present study. Finally, the higher prevalence of low back pain, and lumbar radiculopathy in the non-working group could indicate a healthy worker effect, which may have attenuated the role of occupational factors in the analyses.
4.3. Strengths and implications
Scientific reports on cold-related MSD are scarce, and the present study represents one of the largest epidemiological studies to date on this topic. It was population-based, considered both indoor and outdoor ambient cold exposure, included both men and women, and the results were adjusted for common confounding factors reported by previous authors. The occurrence rates of the studied outcomes corresponded with other reports in this region, which supports that the sample was representative of the population. Since there is evidence to suggest that both ambient and contact cold exposure potentiates the effects of ergonomic exposures, such factors should be included in future studies on MSD. Cold exposure could also prove important to assess in occupational health surveillance systems, and for this purpose the International organisation for standardisation (ISO) document 15743:2008 could be employed. This standard includes methods and a checklist for technical cold risk assessment and management, a structured approach and questionnaire for use by occupational health-care professionals in identifying subjects with cold-related symptoms, and guidelines on how to apply thermal standards and other validated methods when assessing cold-related risks.
4.4. Conclusions
Ambient cold exposure during work was an independent predictor of neck pain, low back pain, and lumbar radiculopathy. In occupational health care settings, cold exposure should be recognised as a possible risk factor for musculoskeletal disorders.
| Abbreviations | ||
| MSD | = | musculoskeletal disorders |
| CHINS | = | Cold and Health In Northern Sweden |
| IQR | = | interquartile range |
| NRS | = | numerical rating scale |
| BMI | = | body mass index |
| ISCO | = | International Standard Classification of Occupations |
| OR | = | odds ratio |
| ISO | = | International Organization for Standardization |
TERG-2021-0384-File005.pdf
Download PDF (37.8 KB)TERG-2021-0384-File004.pdf
Download PDF (210.6 KB)TERG-2021-0384-File001.docx
Download MS Word (18 KB)Acknowledgements
The authors gratefully acknowledge the valuable contributions of Ingrid Liljelind, Tohr Nilsson, and Jens Wahlström at the Department of Public Health and Clinical Medicine at Umeå University, in designing the CHINS surveys.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The dataset used for this paper can be made available upon personal request.
Additional information
Funding
References
- Aasmoe, L., B. Bang, C. Egeness, and M. L. Løchen. 2008. “Musculoskeletal Symptoms among Seafood Production Workers in North Norway.” Occupational Medicine 58 (1): 64–70. doi:10.1093/occmed/kqm136.
- Bang, B. E., L. Aasmoe, L. Aardal, G. S. Andorsen, A. K. Bjørnbakk, C. Egeness, I. Espejord, and E. Kramvik. 2005. “Feeling Cold at Work Increases the Risk of Symptoms from Muscles, Skin, and Airways in Seafood Industry Workers.” American Journal of Industrial Medicine 47 (1): 65–71. doi:10.1002/ajim.20109.
- Blair, E., and G. Zinkhan. 2006. “Nonresponse and Generalizability in Academic Research.” Journal of the Academy of Marketing Science 34 (1): 4–7. doi:10.1177/0092070305283778.
- Burström, L., B. Järvholm, T. Nilsson, and J. Wahlström. 2013. “Back and Neck Pain Due to Working in a Cold Environment: A Cross-Sectional Study of Male Construction Workers.” International Archives of Occupational and Environmental Health 86 (7): 809–813. doi:10.1007/s00420-012-0818-9.
- Dovrat, E., and M. Katz-Leurer. 2007. “Cold Exposure and Low Back Pain in Store Workers in Israel.” American Journal of Industrial Medicine 50 (8): 626–631. doi:10.1002/ajim.20488.
- Dueñas, M., B. Ojeda, A. Salazar, J. A. Mico, and I. Failde. 2016. “A Review of Chronic Pain Impact on Patients, Their Social Environment and the Health Care System.” Journal of Pain Research 9: 457–467. doi:10.2147/JPR.S105892.
- Elsner, G., A. Nienhaus, and W. Beck. 1997. “Occupationally-Induced Degenerative Discopathies in the Area of the Lumbar Spine.” Sozial- Und Praventivmedizin 42 (3): 144–154. doi:10.1007/BF01300565.
- Farbu, E. H., A. C. Höper, T. Brenn, and M. Skandfer. 2021. “Is Working in a Cold Environment Associated with Musculoskeletal Complaints 7-8 Years later? A Longitudinal Analysis from the Tromsø Study.” International Archives of Occupational and Environmental Health 94 (4): 611–619. doi:10.1007/s00420-020-01606-6.
- Farbu, E. H., M. Skandfer, C. Nielsen, T. Brenn, A. Stubhaug, and A. C. Höper. 2019. “Working in a Cold Environment, Feeling Cold at Work and Chronic Pain: A Cross-Sectional Analysis of the Tromsø Study.” BMJ Open 9 (11): e031248 doi:10.1136/bmjopen-2019-031248.
- Farioli, A., S. Mattioli, A. Quaglieri, S. Curti, F. S. Violante, and D. Coggon. 2014. “Musculoskeletal Pain in Europe: The Role of Personal, Occupational, and Social Risk Factors.” Scandinavian Journal of Work, Environment & Health 40 (1): 36–46. doi:10.5271/sjweh.3381.
- Hassi J, Mäkinen T, Holmér I, Påsche A, Risikko T, Toivonen L, Hurme M, editors. 2002. Handbook for Cold Work. 1st ed. Stockholm: The Swedish National Institute for Working Life.
- Hellsing, A. L., S. J. Linton, and M. Kälvemark. 1994. “A Prospective Study of Patients with Acute Back and Neck Pain in Sweden.” Physical Therapy 74 (2): 116–124. doi:10.1093/ptj/74.2.116.
- Hendra, R., and A. Hill. 2019. “Rethinking Response Rates: New Evidence of Little Relationship between Survey Response Rates and Nonresponse Bias.” Evaluation Review 43 (5): 307–330. doi:10.1177/0193841X18807719.
- Hildebrandt, V. H., P. M. Bongers, F. J. H. van Dijk, H. C. G. Kemper, and J. Dul. 2002. “The Influence of Climatic Factors on Non-Specific Back and Neck-Shoulder Disease.” Ergonomics 45 (1): 32–48. doi:10.1080/00140130110110629.
- Horsley, R. 2011. “Factors That Affect the Occurrence and Chronicity of Occupation-Related Musculoskeletal Disorders.” Best Practice & Research. Clinical Rheumatology 25 (1): 103–115. doi:10.1016/j.berh.2011.01.006.
- International Labour Organization. 2012. International Standard Classification of Occupations (ISCO-08). Geneva: International Labour Organization.
- International Organization for Standardization. 2008. Ergonomics of the Thermal Environment – Cold Workplaces – Risk Assessment and Management. Geneva: International Organization for Standardization; ISO 15743:2008.
- Lapossy, E., P. Gasser, P. Hrycaj, B. Dubler, W. Samborski, and W. Muller. 1994. “Cold-Induced Vasospasm in Patients with Fibromyalgia and Chronic Low Back Pain in Comparison to Healthy Subjects.” Clinical Rheumatology 13 (3): 442–445. doi:10.1007/BF02242940.
- Lewis, C., T. Souvlis, and M. Sterling. 2010. “Sensory Characteristics of Tender Points in the Lower Back.” Manual Therapy 15 (5): 451–456. doi:10.1016/j.math.2010.03.006.
- Mäkinen, T. M., and J. Hassi. 2009. “Health Problems in Cold Work.” Industrial Health 47 (3): 207–220. doi:10.2486/indhealth.47.207.
- Mäkinen, T. M., V. P. Raatikka, M. Rytkönen, J. Jokelainen, H. Rintamäki, R. Ruuhela, S. Näyhä, and J. Hassi. 2006. “Factors Affecting Outdoor Exposure in Winter: Population-Based Study.” International Journal of Biometeorology 51 (1): 27–36. doi:10.1007/s00484-006-0040-0.
- Näyhä, S., J. Hassi, P. Jousilahti, T. Laatikainen, and T. M. Ikäheimo. 2011. “Cold-Related Symptoms among the Healthy and Sick of the General Population: National FINRISK Study Data, 2002.” Public Health 125 (6): 380–388. doi:10.1016/j.puhe.2011.02.014.
- Oksa, J., H. Rintamäki, and S. Rissanen. 1997. “Muscle Performance and Electromyogram Activity of the Lower Leg Muscles with Different Levels of Cold Exposure.” European Journal of Applied Physiology 75 (6): 484–490. doi:10.1007/s004210050193.
- Piedrahı́ta, Hugo, Laura Punnett, and Houshang Shahnavaz. 2004. “Musculoskeletal Symptoms in Cold Exposed and Non-Cold Exposed Workers.” International Journal of Industrial Ergonomics 34 (4): 271–278. doi:10.1016/j.ergon.2004.04.008..
- Pienimäki, T. 2002. “Cold Exposure and Musculoskeletal Disorders and Diseases. A Review.” International Journal of Circumpolar Health 61 (2): 173–182. doi:10.3402/ijch.v61i2.17450.
- Pienimäki, T., J. Karppinen, H. Rintamäki, K. Borodulin, T. Laatikainen, P. Jousilahti, J. Hassi, and S. Näyhä. 2014. “Prevalence of Cold-Related Musculoskeletal Pain according to Self-Reported Threshold Temperature among the Finnish Adult Population.” European Journal of Pain 18 (2): 288–298. doi:10.1002/j.1532-2149.2013.00368.x.
- Pinar, T., Z. A. Cakmak, M. Saygun, R. Akdur, N. Ulu, I. Keles, and H. S. Saylam. 2013. “Symptoms of Musculoskeletal Disorders among Ammunition Factory Workers in Turkey.” Archives of Environmental & Occupational Health 68 (1): 13–21. doi:10.1080/19338244.2011.627893.
- Racinais, S., and J. Oksa. 2010. “Temperature and Neuromuscular Function.” Scandinavian Journal of Medicine & Science in Sports 20 (Suppl 3): 1–18. doi:10.1111/j.1600-0838.2010.01204.x.
- Shraim, M. A., H. Massé-Alarie, and P. W. Hodges. 2021. “Methods to Discriminate between Mechanism-Based Categories of Pain Experienced in the Musculoskeletal System: A Systematic Review.” Pain 162 (4): 1007–1037. doi:10.1097/j.pain.0000000000002113.
- Skandfer, M., L. Talykova, T. Brenn, T. Nilsson, and A. Vaktskjold. 2014. “Low Back Pain among Mineworkers in Relation to Driving, Cold Environment and Ergonomics.” Ergonomics 57 (10): 1541–1548. doi:10.1080/00140139.2014.904005.
- Sormunen, E., J. Remes, J. Hassi, T. Pienimäki, and H. Rintamäki. 2009. “Factors Associated with Self-Estimated Work Ability and Musculoskeletal Symptoms among Male and Female Workers in Cooled Food-Processing Facilities.” Industrial Health 47 (3): 271–282. doi:10.2486/indhealth.47.271.
- Stjernbrandt, A., B. Björ, M. Andersson, L. Burström, I. Liljelind, T. Nilsson, R. Lundström, and J. Wahlström. 2017. “Neurovascular Hand Symptoms in Relation to Cold Exposure in Northern Sweden: A Population-Based Study.” International Archives of Occupational and Environmental Health 90 (7): 587–595. doi:10.1007/s00420-017-1221-3.
- Sundelin, G., and M. Hagberg. 1992. “Effects of Exposure to Excessive Drafts on Myoelectric Activity in Shoulder Muscles.” Journal of Electromyography and Kinesiology 2 (1): 36–41. doi:10.1016/1050-6411(92)90006-5.
- Sundstrup, E., M. D. Jakobsen, M. Brandt, K. Jay, R. Persson, and L. L. Andersen. 2015. “Central Sensitization and Perceived Indoor Climate among Workers with Chronic Upper-Limb Pain: Cross-Sectional Study.” Pain Research and Treatment 2015: 793750 doi:10.1155/2015/793750.
- The Swedish Work Environment Agency. 2018. The Work Environment 2017. Stockholm: The Swedish Work Environment Agency; Report 2018:2, ISSN 1652–1110.
