Abstract
In healthcare work settings, flow disruptions (FDs) pose a potential threat to patient safety. Resilience research suggests that adaptive behavioural strategies contribute to preventing cognitive overload through FDs at crucial moments. We aimed to explore the nature and efficacy of operating room (OR) team strategies to prevent FDs in robot-assisted surgery. Within a mixed-methods design, we first asked surgical professionals, which strategies they apply, and secondly, identified behavioural strategies through direct observations. Findings were analysed using content analysis. Additionally, FDs were assessed through live observations in the OR. The sample included four interviewed experts and 15 observed surgical cases. Sixty originally received strategies were synthesised into 17 final OR team strategies. Overall, 658 FDs were observed with external FDs being the most frequent. During high-risk episodes, FDs were significantly reduced (p < 0.0001). The identified strategies reveal how OR teams deliberatively and dynamically manage and mitigate FDs during critical tasks. Our findings contribute to a nuanced understanding of adaptive strategies to safeguard performance in robot surgery services.
Practitioner Summary: Flow disruptions (FDs) in surgical work may become a severe safety threat during high-risk situations. With interviews and observations, we explored team strategies applied to prevent FDs in critical moments. We obtained a comprehensive list of behavioural strategies and found that FDs were significantly reduced during a specific high-risk surgical task. Our findings emphasise the role of providers’ and teams’ adaptive capabilities to manage workflow in high-technology care environments.
Background
In surgery, the operating room (OR) work environment is characterised by multitasking, frequent breaks, and disruptions (Katz Citation2017; Shouhed et al. Citation2012). Some of these disruptions demand attention capacities, cause delays in work or affect performance (i.e. decision making, technical performance) with potentially serious consequences for patients (Sanderson, McCurdie, and Grundgeiger Citation2019). Consequently, during the management of unexpected events and high-risk situations, providers, as well as the OR teams’ ability to successfully handle disruptive events, can be impaired (Wiegmann et al. Citation2007). Resilience, as a system’s adaptive response to constraints or unexpected events as well as care providers’ individual capability to maintain performance, has received increasing attention in healthcare (Hollnagel, Wears, and Braithwaite Citation2015; Kolodzey et al. Citation2020). First defined as an individual’s ability to recover quickly from difficulties (‘to bounce back’), this concept has been applied to a variety of specific settings (Atkinson, Martin, and Rankin Citation2009). Although resilience definitions vary in surgery, many emphasise the capacity of individual staff members and teams to successfully handle difficult situations and evolve adaptive skills (Arnold-Forster Citation2020). Eventually, resilience helps surgical teams to face highly challenging and disrupting work conditions without compromising patient safety (Jung, Elfassy, and Grantcharov Citation2020). A growing body of literature on resilience in healthcare has spurred an increasing interest, in how effective and successful adaption under difficult circumstances takes place (Robertson et al. Citation2016; Smith and Plunkett Citation2019).
As the application of new technologies (i.e. robotic systems) expands in the OR, technology implementation, as well as demanding working conditions, require steady adaptions of the OR team (Jung, Elfassy, and Grantcharov Citation2020). Especially, because technological innovations do not necessarily improve the ergonomics of the surgical workplace (Arora and Sevdalis Citation2011). During the past decade, robot-assisted surgery (RAS) has been established globally as a standard practice for an increasing number of surgical interventions (Leal Ghezzi and Campos Corleta Citation2016). Besides the changes in technical workflow and the advantages that RAS systems offer (Dalsgaard et al. Citation2020), there is also a significant impact on how surgical teams work together, particularly, with new challenges for team communication and cooperation (Schreyer et al. Citation2022; Allers et al. Citation2016). Spatial requirements, walking paths, and team responsibilities change with the introduction of remote control stations and robotic arms holding and moving surgical devices inside the patient (Tiferes et al. Citation2016). At the same time, the increasing adoption of new technologies in the OR creates a greater risk of device or equipment failures, which may lead to severe consequences for patient care (Palmer et al. Citation2013; Law et al. Citation2019). It is therefore essential, to consider ergonomic and team challenges imposed by new technologies in the course of evaluations of modern OR work environments (Bruun et al. Citation2021; Catchpole et al. Citation2019).
Together with the risk of equipment failures, there is a wide range of additional events with the potential to hamper the surgical workflow as well as the inherent need for steady adaptations. Beeper calls, visitors, or small talks, are highly frequent disruptive events, in both conventional and RAS ORs, and have been described as ‘flow disruptions’ (FDs) (Antoniadis et al. Citation2014; McMullan et al. Citation2021). We define such incidences as events that disturb the workflow of the surgical team or distract from the primary task of patient care (Wiegmann et al. Citation2007; Mentis et al. Citation2016). Occurrence rates of 13 FDs per hour have been reported (Bellandi et al. Citation2018; Campbell, Arfanis, and Smith Citation2012). With higher FD rates in the OR, stress and cognitive demands of the surgical team have shown to be significantly increased (Jung, Elfassy, and Grantcharov Citation2020; Bretonnier et al. Citation2020). In simulated surgical tasks, performance outcomes (i.e. task time, errors, economy of motion) deteriorated when FD levels increased (Goodell, Cao, and Schwaitzberg Citation2006; Merry et al. Citation2008).
Concerning the performance and safety consequences of FDs in the course of surgical interventions, it has been proposed that negative effects on patient outcomes are inevitable; but this assumption could not be empirically confirmed yet (Koch et al. Citation2020; Feuerbacher et al. Citation2012). Drawing upon recent resilience research in surgery and under consideration of the OR as an adaptive socio-technical system, we assume that surgical teams can regulate and control the occurrence of FDs to some extent. Previous research revealed, that a large portion of FDs in the OR is initiated by the staff itself (i.e. small talk, teaching) and might be therefore prone to manage in frequency and timing (Sevdalis, Healey, and Vincent Citation2007). Moreover, given this larger share of self-initiated FDs, it might be conceived, that providers or teams are capable to reduce FDs in non-opportune moments, e.g. avoiding FDs if needed (Li, Magrabi, and Coiera Citation2012). Consequently, fewer or less severe FDs might be experienced during high-risk or stressful situations, when absolute attention and ‘full focus’ are required. Currently, few real-world studies examining the rates of FDs separately for individual intraoperative episodes are available. Although some have investigated FDs in critical episodes in anaesthesia and nursing (Broom et al. Citation2011; Clark Citation2013), so far the whole multi-professional, surgical team has not been addressed. Moreover, since high-risk tasks have the greatest potential for adverse safety events, a more granular and dynamic view over the time of the entire procedure is essential (Keller et al. Citation2020). Resilience research suggests that acquired behavioural strategies might be contributing to preventing the cognitive load from being further intensified through FDs at crucial moments (Murden et al. Citation2018; Wahlström et al. Citation2018).
To the best of our knowledge, no study so far has explored in detail how the quantity or quality of FDs changes in the course of intraoperative low- and, particularly, high-risk episodes. Moreover, naturalistic investigations into behavioural strategies or team actions being applied to mitigate FDs in real-world settings are sparse (Clark Citation2013). We thus believe that this study is a major contribution to the understanding of the complex system dynamics and resiliency in determining the impact of FDs on patient safety in the OR. Investigations into functional and dysfunctional deviations help to understand how complex adaptive systems operate, as well as how humans adapt their behaviour to respond to ever-changing work conditions in complex and interdependent (healthcare) work environments (Cohen et al. Citation2022). Examination of successful strategies to handle interruptions helps to organise work for high reliability and establish improvement efforts that go beyond simple ‘no interruption-’ or sole FD-elimination measures (Gao, Rae, and Dekker Citation2021). For surgical practice, such an investigation is another step towards interventions to encourage or expand existing team actions to establish smooth flow during technology-facilitated surgery.
Following these thoughts, our study had two aims:
To assess and describe team strategies to prevent harmful FDs during high-risk episodes.
To quantify FDs during perioperative low-risk compared to high-risk situations to identify changes in frequency and quality and therefore explore the effectiveness of collected behavioural strategies.
Methods
Design
We set up a stepwise and multi-method approach that combined semi-structured interviews and observations in the OR. First, we explored individual and OR team behavioural strategies to prevent or avoid harmful FDs during critical surgical procedure steps. Second, we determined differences in the occurrence of FDs during high-risk and low-risk episodes in the OR. This study is part of a larger project that was approved by the Ethics Committee of the Medical Faculty, Munich University (No. 19-696). Both patients and surgical team members gave their written consent to the study. Before the start of the data collection, each observer completed preliminary training observations (195 h in total) to ensure accurate observations and to minimise the Hawthorne effect.
Setting and surgical procedure
This study took place at the LMU University Hospital in Munich, Germany, in 2020 and 2021. All observations were made at an academic urological department during elective robot-assisted partial nephrectomy (RAPN) procedures. This minimally invasive treatment option for patients with renal tumours is well-established and routinely carried out in this hospital. Required surgical steps include exposure of the kidney, clamping of the renal artery, and excision of the tumour (Desai et al. Citation2003). The intraoperative period of renal clamping, also known as warm ischaemia time, is a high-risk period for surgical outcomes and patient safety: it is recommended to end the clamping of the renal artery after 20 min at the latest to avoid severe organ damage (Porpiglia et al. Citation2007). This increases the demands and time pressure in this period for the OR team substantially (Patel and Eggener Citation2011). For all surgical cases, the da Vinci Surgical System Model Si and X (Intuitive Inc., Sunnyvale CA) were used. This involves the main surgeon sitting at a separate console and controlling the required surgical devices remotely.
Step 1: Identification of strategies to prevent FDs in high-risk situations
In the first step, we aimed to explore OR team strategies to ensure a calm and non-disruptive environment during intraoperative high-risk periods. To obtain as many strategies as possible, we combined semi-structured expert interviews with participatory observations in the OR. We applied a working definition of FDs as intraoperative events that may distract or interrupt the surgical team from their primary task of taking care of the present patient (Shouhed et al. Citation2012; Antoniadis et al. Citation2014; Mentis et al. Citation2016).
Through e-mail and personal contact, we approached urological professionals of one university hospital (LMU University Hospital, Munich, Germany) with pertinent experiences with RAPN procedures to participate in our interviews. With open-ended questions, they were asked to list as many strategies and practices as possible that they had in mind to ensure a safe and uninterrupted workflow during the high-risk episode of clamping the renal artery in RAPN procedures. For each strategy or practice, they identified, the timing (e.g. ‘before surgery’, ‘during the high-risk episode’) and the team members using this strategy or being involved had to be specified. We provided a definition and examples of potential FDs during the interview and it was explicitly pointed out that strategies could also be relevant before or after surgical interventions. Additionally, gender, professional group (e.g. nursing team), and overall working experience of the interviewees were collected as well as their total number of RAPN procedures completed. To be included, OR professionals had to be involved in at least ten RAPN procedures as active team members. We included physicians (all urological surgeons) and nursing professionals. The interviews were anonymized for further analysis.
In addition to the interviews, further observable strategies were collected in multiple sessions by a trained observer. For this purpose, the observer attended RAPN procedures and noted visible FD prevention strategies or team actions. The observer (first author, AK) had previous experience with the assessment of intraoperative flow disruptions and also knew the RAPN procedure and required steps very well. Additionally, pairwise observations (author MW) were conducted to establish agreement and validate observations. Both observers have experience in observing and recording flow disruptions during robotic procedures in urology (>200 h) and were familiar with teamwork challenges and relevant steps during RAPN (Schreyer et al. Citation2022). Strategies that were verbally communicated by the surgical team were noted by the observer, such as intraoperative briefings and or provider behaviours that targeted workflow or procedure steps of the current intervention, i.e. additional preparatory steps or self-initiated check-ups. For each observed behaviour, scope, timing, and OR staff members involved were specified.
Subsequently, all collected strategies (via interviews and observations) were entered into a joint datasheet. We synthesised and combined these original strategies in a multi-step content analysis based on inductive reasoning (Hsieh and Shannon Citation2005). This approach allows to explore the data without predefined theories. The goal is to get from specific answers to more general results (Elo and Kyngäs Citation2008). The following three rounds of data synthesis were applied:
Round 1: Removing duplicates
Merging equal strategies
Merging strategies that were listed separately for different professional groups (i.e. nursing team and console surgeon)
Round 2: Phrasing/reformulation of too detailed and specific strategies
Round 3: Generating categories of similar strategies, labelling the categories with a keyword, providing a description and examples
The individual rounds of this process were completed by two of the authors. Disagreements were discussed until consensus was reached. The final list of strategies was shared with two OR team members to validate the plausibility of categories, and keywords and to minimise any possible interpretation errors by the researchers (i.e. definition of indicators or behavioural exemplars for each strategy).
Step 2: Quantitative assessment and evaluation of flow disruptions across low- and high-risk phases
In a second step, we assessed flow disruption events during robot-assisted partial nephrectomies through standardised observations in the OR. Observations began when the console urologist started operating the robot (main surgical intervention) and ended with the undocking of the robotic system from the patient. For each FD event timing, source category, and severity grade were determined (Willett et al. Citation2018; Healey, Sevdalis, and Vincent Citation2006). Following previous studies, we defined FD source categories as External factors (e.g. door openings, phone calls), communication (e.g. question remains unheard, misunderstandings), equipment (e.g. instrument breakdowns), coordination (e.g. failure of task coordination, unclear responsibilities), training/teaching (e.g. explanatory comments on the surgical approach), patient factors (e.g. adhesions, high BMI), surgeon task consideration (e.g. rethinking next surgical steps), and environmental factors (e.g. light changes, limited space) (Koch et al. Citation2022; Weigl et al. Citation2018; Catchpole et al. Citation2016). Definitions of each severity level can be found in .
Table 1. FD severity level definitions.
Episodes with potentially low risks were compared to episodes with high risks. For this purpose, we divided the intraoperative observations into three consecutive parts: pre-clamping (low risk), clamping of the renal artery (high risk), and post-clamping (low risk). The clamping episode started in the second when the console surgeon intermits the blood flow of the renal artery and ends with the removal of the clamp.
Statistical analyses
We calculated descriptive statistics (counts and rates per hour) with means and standard deviations (SD) for all observed FDs. To compare the means of the individual surgical episodes we applied dependent t-tests. We applied a significance level of alpha (p < 0.05) for statistical tests. Due to multiple testing (n = 25) within analyses for individual comparisons for FD sources, we also conducted a Bonferroni-Holm correction. All statistical analyses were realised with SPSS Statistics 27 (IBM Inc., Chicago, IL, USA).
Results
Sample
In step 1, four surgical professionals (two nurses, and two physicians) participated in our interviews by phone or in writing. Their experience with RAPN procedures ranged from 15 to 300 previously performed interventions. In addition to the collection of strategies through interviews, one trained observer accompanied several OR teams and gathered further visible strategies during five RAPN interventions.
For step 2, and to evaluate the occurrence of FDs in surgical procedures, we collected observational data during 15 complete surgical RAPN interventions. None of the included cases required intraoperative conversion to open surgery or a substantial modification of the routine surgical treatment plan (e.g. removal of the whole kidney). Each procedure involved an OR team of at least five surgical members (two surgeons, two nurses, and one anaesthetist). The main surgical phase (console time) had an average duration of 117.1 min (SD, Standard deviation = 28.8 min). The first episode, the ‘pre-clamping episode’ had a mean duration of 74.12 min (SD = 25.38), the high-risk ‘clamping episode’ of 17.27 min (SD = 2.64), and the ‘post-clamping episode’ of 25.48 min (SD = 6.08).
Step 1: Identification of strategies to prevent FDs in high-risk situations
We originally obtained 39 reported OR team strategies and actions for preventing or avoiding FDs through the interviews (e.g. preoperative selection of suitable patients). Twenty-one additional behavioural strategies could be identified in the course of live observations (e.g. short team debriefing after clamping episode). Through an inductive content analysis, we eventually collated 17 strategies. depicts the data collection and synthesis process.
Figure 1. Process of collecting and synthesising FD prevention strategies.
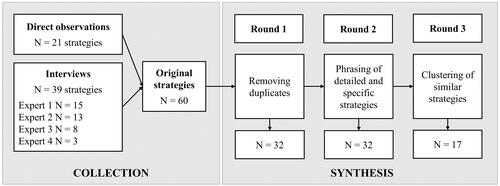
Within the first round of removing duplicates, such as ‘Goes through checklist items’ (source: interviewee 1) or ‘Check-up before the clamping phase’ (source: observer) were combined into one strategy: ‘Going through a checklist before clamping episode’. The second round was applied to phrase strategies, for example: ‘Before ischemia time, hang (or turn around) the signs (in DIN-A4 format) “Do not disturb” outside on the two OR doors in front to the operating corridor and sterile corridor’ was shortened into ‘Turning around “Do not disturb signs” on OR doors’. In the last round similar strategies were clustered together and labelled: e.g. ‘preparing bulldogs’, ‘preparing seems’, and ‘preparing haemostatics’ were clustered into ‘Intraoperative preparation of emergency medical equipment and additional supply material’ and labelled with Additional surgical supplies.
lists the final OR team strategies to prevent or reduce FDs. We sorted the behaviours concerning the temporal order in the course of the procedure. For each strategy, the column ‘team role’ indicates the surgical team member applying the strategy and the profession and team function performed (e.g. console surgeon, circulating nurse, cf. ).
Table 2. Provider-reported strategies to prevent FDs in high-risk situations.
Some of the strategies are very specific to one team role (e.g. Patient selection through the main surgeon); while others are applied by the entire team (e.g. Avoiding self-initiated interruptions). Furthermore, some strategies are meant to improve teamwork (e.g. Mutual support, Effective communication); others are meant for the individual task- and self-regulation (e.g. Precise surgical preparation, Avoiding self-initiated interruptions, cf. ).
A comprehensive table with all originally obtained strategies, condensation procedure as well as a list of final strategies can be found in the Supplementary Material (see Supplemental Online Material 1).
Step 2: Assessment and evaluation of flow disruptions in partial nephrectomies
In 15 partial nephrectomies, a total of 658 FDs were observed with a mean count of 43.87 per surgery (SD = 20.67). depicts rates per hour of observed flow disruptions for each surgical episode and FD source.
Figure 2. Hourly FD rates for each intraoperative episode and disruptions source category.
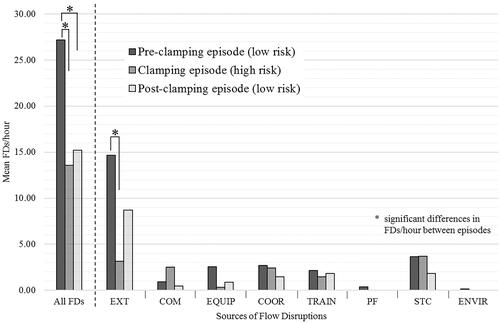
The majority of FDs were recorded during the pre-clamping episode (76.75%). The different source categories occurred with very different frequencies: the by far most common FDs observed were external disturbances (i.e. visitors, telephone calls) with a rate of 11.39 per hour across all episodes. All counts of FDs for each episode and rates per hour (descriptive statistics) in tabular form can be found in the Supplementary Material (see Supplemental Online Material 2).
Testing for significant changes in the overall mean rates of FDs per hour between the individual phases revealed that the pre-clamping episode had significant more FDs/hour than the clamping episode [T(14) = 7.839; p < 0.0001] and also than the post-clamping episode [T(14) = 5.346; p = 0.0001]. No difference [T(14) = −.854; p = 0.41] in the overall mean rates per hour could be found between the clamping episode and the time after (‘post-clamping). Concerning the individual source categories, we detected a significant decrease in external FDs from the pre-clamping to the clamping episode [T(14) = 6.887; p < 0.0001]. No significant changes in the remaining FD source categories could be detected. Results of all t-tests and Bonferroni-Holm corrected p-levels can be found in the Supplementary Material (see Supplemental Online Material 3).
Discussion
This study focussed on behavioural strategies of surgical teams to dynamically adapt and manage FDs across high-risk episodes. We developed a comprehensive list of behavioural strategies and task steps; all indicating that the OR team deliberatively reduces FDs during high-risk episodes to manage the complexity and safety of demanding perioperative phases. Moreover, a significant reduction of FDs during the high-risk clamping episode was observed compared to the pre-clamping. This suggests that the mitigation strategies we described might actually be effective, although causality cannot be assumed. Altogether, we conceive this as surgical resilience with the OR team proactively acting as well as responding adaptively to difficult task demands and mentally taxing task episodes.
The successful management of challenges and high-risk situations in the OR is essential to avoid errors and guarantee patient safety. Patients undergoing surgery are at higher risk to witness medical errors than other patients in hospital care (Makary et al. Citation2006; McCulloch et al. Citation2017). Flow disruptions have the potential to become severe safety threats, are very common though in surgical day routines, and cannot be entirely banned (Allers et al. Citation2016; Jung et al. Citation2020). Consequently, it is essential to find ways to deal with these events, prevent avoidable FDs and effectively manage those that can’t be avoided (Ahmed et al. Citation2015).
In the first part of our mixed-methods study, we collected a comprehensive list of FD prevention strategies. The interviewed surgical professionals paid attention to the professional role and contributions of each of the five OR team professions, respectively: main/console surgeon, bedside assistant, sterile nurse, circulating nurse, and anaesthetist. This observation resonates well with previous findings that preventing FDs is a joint effort of the entire surgical team (Clark Citation2013; Sverdrup, Schei, and Tjølsen Citation2017). Our spectrum of adjustments and joint strategies indicates that the team shares a common awareness of the potential impact of FDs in critical episodes. Situation awareness has already been highlighted as a key skill of care providers to react to dynamically changing work environments (Weigl et al. Citation2020; Parush et al. Citation2011).
Additional on-site observations enabled us to augment the list of reported strategies with visible actions that have not been brought up by the surveyed professionals. Finally, we established a classification system with behavioural examples that should also be easily applicable to a wide range of other surgical procedures (i.e. laparoscopic or open surgery). Our identified strategies can be attributed to all phases of the surgical procedure including the focus on thorough preparations of instruments and supplies, joint check-ups, and avoidance of self-initiated FDs, such as small talk. Our findings resonate well with similar research on nursing personnel’s efforts to avoid perioperative FDs (i.e. checking all equipment, creating checklists, and asking for quiet) (Clark Citation2013).
In the second step of our study, we assessed the occurrence of FDs in course of the procedure as well as across three distinct task episodes. The aim of this part was to explore whether the obtained prevention strategies (e.g. placement of OR door sign to prevent external staff to enter the OR) potentially have the desired effect and reduce the occurrence of FDs during high-risk episodes. Within the comparison of three consecutive surgical episodes (pre-clamping—clamping—post-clamping), we detected a significant decrease in the overall FD rate per hour during the high-risk episodes compared to the previous low-risk episode. Surprisingly, this effect persisted in the last surgical episode (low risk) with a likewise low rate of FDs as during the high-risk episode. The question of whether the surgical team compensates for the higher efforts and demands of the previous high-risk episode with some additional quiet time (i.e. recuperation or stress recovery), or whether there is another explanation, needs to be answered by future investigations. Within the in-depth analyses of changes in the individual FD source categories, we were able to detect a substantial decrease in external disruptions during the high-risk episode. External FDs include disruptive OR visitors as well as small talk and telephone calls (Catchpole et al. Citation2016). The fact that this category of FDs could be reduced in highly demanding situations indicates that the incidences of such events can be deliberatively and effectively managed by the surgical team (Al-Hakim Citation2011; Rivera-Rodriguez and Karsh Citation2010).
Today, we know that there is a broad range of different FDs, some (i.e. equipment failures) with a potentially greater impact than others (i.e. door openings) (Wheelock et al. Citation2015). Surgeons report that there are many FDs that they do not even notice and in low-risk routine situations some FDs, such as small talk might be helpful to stay concentrated (Widmer et al. Citation2018). On the other side, in stressful situations, certain FDs (i.e. coordination failures) bind attention, increase mental workload or stimulate stress experience with hazards to patient safety (Koch et al. Citation2020). It has been emphasised that the surgical team suffers from the negative consequences of FDs through higher stress and workload levels (Weber et al. Citation2018). At the same time, effective teamwork has been found to mitigate the impact of FDs (Schraagen et al. Citation2011). However, our study is the first to explore the capability of the entire OR team to self-manage the amount of experienced FDs (Cohen et al. Citation2022). Our findings propose that each individual member of the surgical team adaptively contributes to the safety of the OR and that promoting those skills may be an effective approach to FD handling and prevention. In the context of previous work on resilience, we believe that these findings contribute to a better understanding of the complex interplay within the socio-technical working system while managing OR safety. Our findings corroborate that OR teams adjust and apply strategies that establish resilience to interruptions to eventually maintain reliability and maintain a stable state of operation (Gao, Rae, and Dekker Citation2021). FDs fundamentally demonstrate mismatches between the demands of the work and the ability of the sociotechnical system to support it (Catchpole et al. Citation2021). In terms of resiliency (or Safety-II perspective), our findings show how OR teams respond to complexity and varying challenges (Hollnagel, Wears, and Braithwaite Citation2015). If we define FDs as functional or dysfunctional deviations, resiliency can be conceived as a successful adaption to changing conditions, progress as well contextual challenges (Sanderson, McCurdie, and Grundgeiger Citation2019; Koch et al. Citation2020). Subsequently, this may prevent well-intentioned FD safety interventions that do not have the desired effect (Gao, Rae, and Dekker Citation2021).
A certain proportion of FDs are specific to robot-assisted surgical interventions (e.g. malfunctions of the robotic system, communication failures due to a high noise level of the cooling fan), while others are part of almost all kinds of surgeries (e.g. beeper calls, door openings). Robot-assisted surgery and high-technology ORs are part of the present and the future in surgery and introduce new challenges to surgical work, team communication, and cooperation. Non-verbal and implicit communication, for example, is hard to realise with the main surgeon facing the robotic console with potentially serious consequences for information exchange (Catchpole et al. Citation2019; Manuguerra et al. Citation2021). Surgical teams successfully apply adjustment strategies on how to interact when facing stressful situations and adverse events (Gill and Randell Citation2016). Our observations thus contribute to an increasing literature base on how inherent teamwork challenges and risks in high technology ORs interact. The RAPN procedure with the application of a robotic surgical system provides an excellent example of the working environment of current and future ORs.
The surgical teams in our sample, and especially the surgeon operating the da Vinci robotic system, had a high degree of experience in RAS interventions. Therefore, no FDs have been considered that might arise from the learning process when integrating the RAS system in pre-existing surgical work systems (Catchpole et al. Citation2016). For future studies, it might be of interest to monitor FDs during this implementation phase to explore challenges posed by the introduction of new technologies (i.e. psychomotor skill acquisition for the main surgeon; sharing their workspace with robotic arms for the bedside assistant surgeon and sterile nurse) (Goldstraw et al. Citation2012).
Altogether, our study advances previous work, particularly in two points: First, we paid attention to the entire multi-professional OR team (surgeons, nurses, anaesthetists) to obtain a comprehensive perspective on the intraoperative challenges and incidences of repeated FDs. There are few studies on the handling or prevention of intraoperative FDs and they mostly focus on individual professions (i.e. nurses) and neglect joint OR team efforts and cooperation. As the surgical team is more than the sum of its single members, this barely reflects reality (Vincent et al. Citation2004; Werner and Holden Citation2015). Good teamwork and communication are associated with fewer errors and are based on mutual familiarity, i.e. teams that work together frequently tend to perform better (Shouhed et al. Citation2012; Catchpole et al. Citation2008). Fostering effective collaboration and thereby improving patient safety in the OR presupposes an in-depth understanding of dynamic adjustments, resilience, and team processes that are applied in everyday work (‘work as done’). Knowledge of adaptive teamwork in challenging situations can help to prevent adverse events and design purposeful interventions (McCulloch et al. Citation2017). The second strength of our study is the consideration of the task-induced variation of FDs over time and the comparison of low-risk and high-risk intraoperative episodes. Previous studies mainly reported overall FD frequencies and few attempts have been made to systematically differentiate between individual episodes or respective tasks in course of the procedure (Jung et al. Citation2020). Evidence from other areas, nevertheless, points to the timing of FDs as a key determinant of their impact (Li, Magrabi, and Coiera Citation2012; Clark Citation2013; Iqbal and Bailey Citation2005). The surgical intervention (RAPN) we selected for our study offers an excellent setting for our research objective by allowing a clear differentiation between intraoperative high-risk and low-risk episodes. This enables conclusions on the team’s efforts to prevent FDs across specific high-risk episodes.
Limitations
Although we were able to record a substantial number of FDs throughout each defined surgical episode, we included a limited number of 15 patient cases. Unfortunately, due to the unsteady frequency of this specific type of surgery and the constraints caused by the Covid-19 pandemic during the data collection period, we were not able to incorporate more surgical cases or other hospital sites. As a consequence, some FD source categories were not prevalent enough to obtain statistical power. In addition, observed interventions are very homogeneous (RAPN) and there was high staffing continuity in the surgical team. Consequently, our obtained prevention strategies draw upon teamwork during RAPN procedures specifically and generalisability across other surgical domains and interventions (i.e. non-robotic-assisted surgeries) should be carefully considered. Nonetheless, we deem various strategies generic to effective surgical teamwork and resilient handling of unexpected events.
The second major limitation concerns the actual impact of the individual strategies on FD rates (i.e. causal relationship). We captured team strategies aiming to reduce FDs and we found that the FD rate actually decreased. Yet, we cannot conclude whether the strategies are (exclusively) causing these changes and which strategies are the most efficient ones. Future OR simulation or observation studies should investigate associations of strategy use with the process, provider, or patient outcomes. Furthermore, our method does not allow for deeper insights into potential matches of observed team strategies with specific surgical tasks in the course of the procedure. A nuanced assessment of specific technical and team tasks in the course of the intervention may allow a better understanding of how strategy application and timing match with concurrent work processes (e.g. temporary postponement of a surgical task).
Additionally, we want to pay attention to some minor limitations: First, our standardised evaluations of FDs’ severity levels revealed mainly low levels with no visible impact or team interference (i.e. little variance). Since the severity or level of team interference of individual FDs can potentially determine patient outcomes, it is advisable for future studies to apply a more granular rating system (Antoniadis et al. Citation2014; Healey, Sevdalis, and Vincent Citation2006). On-site observations through expert observers have some constraints, particularly within hectic OR environments. Although the duration of FDs could be relevant, we are unable to take them into account in our study. This is a well-known challenge within live observations of FDs and the use of video-based recordings could be a satisfactory solution (Weigl et al. Citation2020; Galvan et al. Citation2005). However, these are often difficult to realise for reasons of data privacy, compliance, and costs. Second, data from interviews are inherently vulnerable to certain types of cognitive bias (Persoon et al. Citation2011). Since we interviewed study participants after their shifts there might have been some recall bias concerning their intraoperative FD prevention strategies. However, we tried to address this limitation through additional live observations with the collection of further strategies and actions that might have not been remembered. We acknowledge that observations of intraoperative team strategies require contextual knowledge, domain experience, and interpretation effort of the external observer, i.e. if the purpose of some specific provider action was intended to actually reduce FDs. With the cross-validation of our final strategies with surgical experts, we tried to avoid misinterpretation of behaviours and the inclusion of irrelevant/incorrect strategies.
Implications
We assume two feasible ways to apply our findings to surgical training and education: First, creating an awareness of the impact of FDs and empowering surgical team members to take action in critical situations could support OR staff in finding effective measures for managing FDs during critical episodes (Li, Magrabi, and Coiera Citation2012). Second, our list of specific strategies might be used to develop respective training interventions for teams to maintain stable performance and adjust to workflow changes in high-technology operations. Training in general resilience competence could further improve teams’ ability to adapt to complex and challenging situations. Training of physicians’ resilience skills has already been shown to be effective (Ng et al. Citation2019).
We conceive our explorative findings as a base for further investigations and suggest three issues that might be approached in the future: First, the actual effectiveness of the identified FD mitigation strategies should be tested. Determining which strategies are most effective in mitigating OR with particular attention to distraction content, surgical progress as well as team and context factors is of great interest (Ayas et al. Citation2022). Ideally, this could be done in a randomised controlled trial to be able to detect causality. The interaction with surgical workflow and work processes as well as the impact of applied strategies on individual working steps should be taken into account. Since it is conceivable that the strategies applied may also fail to achieve impact or even lead to undesirable or adverse (side) effects, future investigations should carefully evaluate potential practice recommendations. A more detailed view of timing of strategy application with respect to concurrent task steps and working processes is necessary. Second, we designed our study with a focus on proactive strategies and actions to prevent FDs. The next step would also be to explore strategies and actions to handle or manage FDs that have already occurred, i.e. interruption handling strategies. We assume that well-functioning OR teams invest attentional resources into FD mitigation strategies before the actual occurrence (primary prevention or early apprehension) as well as efforts into adapting to or handling disruptive events (secondary prevention). Future research should strive to elicit how effective resilience practices determine a team’s strategies and vice versa. Moreover, further investigations should scrutinise how routine work practices and tasks match with strategy application in the course of the procedure, e.g. when to use opportune moments for short dyadic or team briefings in the course of the procedure to speak about anticipated problems or expected interferences in the workflow (Tschan et al. Citation2021). Third, our study is limited to front-end care providers’ perspectives and capabilities. Taking a more holistic perspective on the entire hospital work system at an individual, team, and organisation level, further factors should be explored that effectively contribute to the prevention of FDs in critical perioperative situations (Smith and Plunkett Citation2019). Additionally, we strongly believe that the timing/position of FDs during a surgical intervention plays a key role in the impact on providers’ workload and patient outcomes (i.e. complication rates) and that greater attention should be paid to this in the future rather than relying on overall FD rates.
Conclusion
Our study is an important step towards a better understanding of the surgical team’s capability to conquer the challenges arising from frequent breaks and disruptions. The intraoperative collaboration of human professional teams and modern robotic technology offers advancements in physical ergonomics and workflow but also introduces new spaces for equipment errors and requires adaptive adjustments to new ways of team communication and effective management of high-risk challenges. We are the first to explore self-developed OR team strategies to prevent FDs in high-risk episodes with comprehensive consideration of all OR professions. Therefore, we offer a contemporary example of the application of resilient actions in surgery. The OR team autonomously developed adaptive behaviours to respond to the higher demands of a high-risk surgical episode. We believe that the identified behavioural strategies serve as examples for surgical teams to improve risk management in highly demanding episodes in the OR. Based on our findings future research can translate the identified strategies to other specialities and interventions. Moreover, we hope that our findings enable new options in the process of further improving patient safety and care in modern surgery.
Supplemental Material
Download Zip (50.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data is available on request from the corresponding author.
Additional information
Funding
References
- Ahmed, Aadil, Mueen Ahmad, C Matthew Stewart, Howard W. Francis, and Nasir I. Bhatti. 2015. “Effect of Distractions on Operative Performance and Ability to Multitask–A Case for Deliberate Practice.” The Laryngoscope 125 (4): 837–841. doi:10.1002/lary.24856.
- Al-Hakim, L. 2011. “The Impact of Preventable Disruption on the Operative Time for Minimally Invasive Surgery.” Surgical Endoscopy 25 (10): 3385–3392. doi:10.1007/s00464-011-1735-9.
- Allers, Jenna C., Ahmed A. Hussein, Nabeeha Ahmad, Lora Cavuoto, Joseph F. Wing, Robin M. Hayes, Nobuyuki Hinata, Ann M. Bisantz, and Khurshid A. Guru. 2016. “Evaluation and Impact of Workflow Interruptions during Robot-Assisted Surgery.” Urology 92: 33–37. doi:10.1016/j.urology.2016.02.040.
- Antoniadis, Sophia, Stefanie Passauer-Baierl, Heiko Baschnegger, and Matthias Weigl. 2014. “Identification and Interference of Intraoperative Distractions and Interruptions in Operating Rooms.” The Journal of Surgical Research 188 (1): 21–29. doi:10.1016/j.jss.2013.12.002.
- Arnold-Forster, A. 2020. “Resilience in Surgery.” The British Journal of Surgery 107 (4): 332–333. doi:10.1002/bjs.11493.
- Arora, S., and N. Sevdalis. 2011. “A Systemic Analysis of Disruptions in the Operating Room: Reply.” World Journal of Surgery 35 (4): 931–932. doi:10.1007/s00268-010-0926-1.
- Atkinson, P.A., C.R. Martin, and J. Rankin. 2009. “Resilience Revisited.” Journal of Psychiatric and Mental Health Nursing 16 (2): 137–145. doi:10.1111/j.1365-2850.2008.01341.x.
- Ayas, Suzan, Bonnie A. Armstrong, Sherman Wong, Lauren Gordon, Teruko Kishibe, Teodor Grantcharov, and Birsen Donmez. 2022. “Mitigating Operating Room Distractions: A Systematic Review Assessing Intervention Effectiveness.” Human Factors in Healthcare 2: 100013. doi:10.1016/j.hfh.2022.100013.
- Bellandi, Tommaso, Alessandro Cerri, Giulia Carreras, Scott Walter, Cipriana Mengozzi, Sara Albolino, Eleonora Mastrominico, Fernando Renzetti, Riccardo Tartaglia, and Johanna Westbrook. 2018. “Interruptions and Multitasking in Surgery: A Multicentre Observational Study of the Daily Work Patterns of Doctors and Nurses.” Ergonomics 61 (1): 40–47. doi:10.1080/00140139.2017.1349934.
- Bretonnier, Maxime, Estelle Michinov, Xavier Morandi, and Laurent Riffaud. 2020. “Interruptions in Surgery: A Comprehensive Review.” The Journal of Surgical Research 247: 190–196. doi:10.1016/j.jss.2019.10.024.
- Broom, M.A., A.L. Capek, P. Carachi, M.A. Akeroyd, and G. Hilditch. 2011. “Critical Phase Distractions in Anaesthesia and the Sterile Cockpit Concept.” Anaesthesia 66 (3): 175–179. doi:10.1111/j.1365-2044.2011.06623.x.
- Bruun, B., J.L. Poulsen, P. Møhl, and L. Spanager. 2021. “Is Non-Stop Always Better? Examining Assumptions behind the Concept of Flow Disruptions in Studies of Robot-Assisted Surgery.” Journal of Robotic Surgery 16: 731–733. doi:10.1007/s11701-021-01275-8.
- Campbell, G., K. Arfanis, and A.F. Smith. 2012. “Distraction and Interruption in Anaesthetic Practice.” British Journal of Anaesthesia 109 (5): 707–715. doi:10.1093/bja/aes219.
- Catchpole, K., A. Mishra, A. Handa, and P. McCulloch. 2008. “Teamwork and Error in the Operating Room: Analysis of Skills and Roles.” Annals of Surgery 247 (4): 699–706. doi:10.1097/SLA.0b013e3181642ec8.
- Catchpole, K., C. Lusk, M. Weigl, J. Anger, and T. Cohen. 2021. “Addressing Misconceptions of Flow Disruption Studies in “Is Non-Stop Always Better? Examining Assumptions behind the Concept of Flow Disruptions in Studies of Robot-Assisted Surgery”.” Journal of Robotic Surgery 16 (4): 989–990. doi:10.1007/s11701-021-01318-0.
- Catchpole, Ken, Ann Bisantz, M. Susan Hallbeck, Matthias Weigl, Rebecca Randell, Merrick Kossack, and Jennifer T. Anger. 2019. “Human Factors in Robotic Assisted Surgery: Lessons from Studies ‘In the Wild’.” Applied Ergonomics 78: 270–276. doi:10.1016/j.apergo.2018.02.011.
- Catchpole, Ken, Colby Perkins, Catherine Bresee, M. Jonathon Solnik, Benjamin Sherman, John Fritch, Bruno Gross, Samantha Jagannathan, Niv Hakami-Majd, Raymund Avenido, and Jennifer T. Anger. 2016. “Safety, Efficiency and Learning Curves in Robotic Surgery: A Human Factors Analysis.” Surgical Endoscopy 30 (9): 3749–3761. doi:10.1007/s00464-015-4671-2.
- Clark, G.J. 2013. “Strategies for Preventing Distractions and Interruptions in the OR.” AORN Journal 97 (6): 702–707. doi:10.1016/j.aorn.2013.01.018.
- Cohen, Tara N., Douglas A. Wiegmann, Falisha F. Kanji, Myrtede Alfred, Jennifer T. Anger, and Ken R. Catchpole. 2022. “Using Flow Disruptions to Understand Healthcare System Safety: A Systematic Review of Observational Studies.” Applied Ergonomics 98: 103559. doi:10.1016/j.apergo.2021.103559.
- Dalsgaard, Torur, Morten D. Jensen, Dorthe Hartwell, Berit J. Mosgaard, Annemette Jørgensen, and Bente R. Jensen. 2020. “Robotic Surgery Is Less Physically Demanding Than Laparoscopic Surgery: Paired Cross Sectional Study.” Annals of Surgery 271 (1): 106–113. doi:10.1097/SLA.0000000000002845.
- Desai, Mihir M., Inderbir S. Gill, Jihad H. Kaouk, Surena F. Matin, and Andrew C. Novick. 2003. “Laparoscopic Partial Nephrectomy with Suture Repair of the Pelvicaliceal System.” Urology 61 (1): 99–104. doi:10.1016/s0090-4295(02)02012-5.
- Elo, S., and H. Kyngäs. 2008. “The Qualitative Content Analysis Process.” Journal of Advanced Nursing 62 (1): 107–115. doi:10.1111/j.1365-2648.2007.04569.x.
- Feuerbacher, Robin L., Kenneth H. Funk, Donn H. Spight, Brian S. Diggs, and John G. Hunter. 2012. “Realistic Distractions and Interruptions That Impair Simulated Surgical Performance by Novice Surgeons.” Archives of Surgery 147 (11): 1026–1030.
- Galvan, Cynthia, Emile A. Bacha, Julie Mohr, and Paul Barach. 2005. “A Human Factors Approach to Understanding Patient Safety during Pediatric Cardiac Surgery.” Progress in Pediatric Cardiology 20 (1): 13–20. doi:10.1016/j.ppedcard.2004.12.001.
- Gao, J., A.J. Rae, and S.W.A. Dekker. 2021. “Intervening in Interruptions: What Exactly Is the Risk We Are Trying to Manage?” Journal of Patient Safety 17 (7): e684–e688. doi:10.1097/PTS.0000000000000429.
- Gill, A., and R. Randell. 2016. “Robotic Surgery and Its Impact on Teamwork in the Operating Theatre.” Journal of Perioperative Practice 26 (3): 42–45. doi:10.1177/175045891602600303.
- Goldstraw, M.A., B.J. Challacombe, K. Patil, P. Amoroso, P. Dasgupta, and R.S. Kirby. 2012. “Overcoming the Challenges of Robot-Assisted Radical Prostatectomy.” Prostate Cancer and Prostatic Diseases 15 (1): 1–7. doi:10.1038/pcan.2011.37.
- Goodell, K.H., C.G.L. Cao, and S.D. Schwaitzberg. 2006. “Effects of Cognitive Distraction on Performance of Laparoscopic Surgical Tasks.” Journal of Laparoendoscopic & Advanced Surgical Techniques 16 (2): 94–98. doi:10.1089/lap.2006.16.94.
- Healey, A.N., N. Sevdalis, and C.A. Vincent. 2006. “Measuring Intra-Operative Interference from Distraction and Interruption Observed in the Operating Theatre.” Ergonomics 49 (5–6): 589–604. doi:10.1080/00140130600568899.
- Hollnagel, E., R.L. Wears, and J. Braithwaite. 2015. From Safety-I to Safety-II: A White Paper.
- Hsieh, H.-F., and S.E. Shannon. 2005. “Three Approaches to Qualitative Content Analysis.” Qualitative Health Research 15 (9): 1277–1288. doi:10.1177/1049732305276687.
- Iqbal, S.T., and B.P. Bailey. 2005. “Investigating the Effectiveness of Mental Workload as a Predictor of Opportune Moments for Interruption.” Extended Abstracts Proceedings of the 2005 Conference on Human Factors in Computing Systems, CHI 2005, Portland, OR, USA. doi:10.1145/1056808.1056948.
- Jung, J.J., J. Elfassy, and T. Grantcharov. 2020. “Factors Associated with Surgeon’s Perception of Distraction in the Operating Room.” Surgical Endoscopy 34 (7): 3169–3175. doi:10.1007/s00464-019-07088-z.
- Jung, James J., Peter Jüni, Gerald Lebovic, and Teodor Grantcharov. 2020. “First-Year Analysis of the Operating Room Black Box Study.” Annals of Surgery 271 (1): 122–127. doi:10.1097/SLA.0000000000002863.
- Katz, J.D. 2017. “Control of the Environment in the Operating Room.” Anesthesia and Analgesia 125 (4): 1214–1218. doi:10.1213/ANE.0000000000001626.
- Keller, Sandra, Steven Yule, Douglas S. Smink, Vivian Zagarese, Shawn Safford, and Sarah Henrickson Parker. 2020. “Episodes of Strain Experienced in the Operating Room: Impact of the Type of Surgery, the Profession and the Phase of the Operation.” BMC Surgery 20 (1): 318. doi:10.1186/s12893-020-00937-y.
- Koch, Amelie, Aljoscha Kullmann, Philipp Stefan, Tobias Weinmann, Sebastian F. Baumbach, Marc Lazarovici, and Matthias Weigl. 2022. “Intraoperative Dynamics of Workflow Disruptions and Surgeons’ Technical Performance Failures: Insights from a Simulated Operating Room.” Surgical Endoscopy 36 (6): 4452–4461. doi:10.1007/s00464-021-08797-0.
- Koch, Amelie, Jacob Burns, Ken Catchpole, and Matthias Weigl. 2020. “Associations of Workflow Disruptions in the Operating Room with Surgical Outcomes: A Systematic Review and Narrative Synthesis.” BMJ Quality & Safety 29 (12): 1033–1045. doi:10.1136/bmjqs-2019-010639.
- Kolodzey, Lauren, Patricia Trbovich, Arash Kashfi, and Teodor P. Grantcharov. 2020. “System Factors Affecting Intraoperative Risk and Resilience: Applying a Novel Integrated Approach to Study Surgical Performance and Patient Safety.” Annals of Surgery 272 (6): 1164–1170. doi:10.1097/SLA.0000000000003280.
- Law, Katherine E., Emily A. Hildebrand, Hunter J. Hawthorne, M Susan Hallbeck, Russell J. Branaghan, Sean C. Dowdy, and Renaldo C. Blocker. 2019. “A Pilot Study of Non-Routine Events in Gynecological Surgery: Type, Impact, and Effect.” Gynecologic Oncology 152 (2): 298–303. doi:10.1016/j.ygyno.2018.11.035.
- Leal Ghezzi, Tiago, and Oly Campos Corleta. 2016. “ 30 Years of Robotic Surgery.” World Journal of Surgery 40 (10): 2550–2557.
- Li, S.Y.W., F. Magrabi, and E. Coiera. 2012. “A Systematic Review of the Psychological Literature on Interruption and Its Patient Safety Implications.” Jamia 19 (1): 6–12.
- Makary, Martin A., J. Bryan Sexton, Julie A. Freischlag, E. Anne Millman, David Pryor, Christine Holzmueller, and Peter J. Pronovost. 2006. “Patient Safety in Surgery.” Annals of Surgery 243 (5): 628–635. doi:10.1097/01.sla.0000216410.74062.0f.
- Manuguerra, Anthony, Charles Mazeaud, Nicolas Hubert, Pascal Eschwège, Mathieu Roumiguié, Julia Salleron, and Jacques Hubert. 2021. “Non-Technical Skills in Robotic Surgery and Impact on near-Miss Events: A Multi-Center Study.” Surgical Endoscopy 35 (9): 5062–5071. doi:10.1007/s00464-020-07988-5.
- McCulloch, Peter, Lauren Morgan, Steve New, Ken Catchpole, Eleanor Roberston, Mohammed Hadi, Sharon Pickering, Gary Collins, and Damian Griffin. 2017. “Combining Systems and Teamwork Approaches to Enhance the Effectiveness of Safety Improvement Interventions in Surgery: The Safer Delivery of Surgical Services (S3) Program.” Annals of Surgery 265 (1): 90–96. doi:10.1097/SLA.0000000000001589.
- McMullan, R.D., R. Urwin, P. Gates, N. Sunderland, and J.I. Westbrook. 2021. “Are Operating Room Distractions, Interruptions, and Disruptions Associated with Performance and Patient Safety? A Systematic Review and Meta-Analysis.” International Journal of Quality in Health Care 33 (2): mzab068. doi:10.1093/intqhc/mzab068.
- Mentis, Helena M., Amine Chellali, Kelly Manser, Caroline G.L. Cao, and Steven D. Schwaitzberg. 2016. “A Systematic Review of the Effect of Distraction on Surgeon Performance: directions for Operating Room Policy and Surgical Training.” Surgical Endoscopy 30 (5): 1713–1724. doi:10.1007/s00464-015-4443-z.
- Merry, A.F., J.M. Weller, B.J. Robinson, G.R. Warman, E. Davies, J. Shaw, J.F. Cheeseman, and L.F. Wilson. 2008. “A Simulation Design for Research Evaluating Safety Innovations in Anaesthesia.” Anaesthesia 63 (12): 1349–1357. doi:10.1111/j.1365-2044.2008.05638.x.
- Murden, F., D. Bailey, F. Mackenzie, R.S. Oeppen, and P.A. Brennan. 2018. “The Impact and Effect of Emotional Resilience on Performance: an Overview for Surgeons and Other Healthcare Professionals.” The British Journal of Oral & Maxillofacial Surgery 56 (9): 786–790. doi:10.1016/j.bjoms.2018.08.012.
- Ng, Richard, Saad Chahine, Brent Lanting, and James Howard. 2019. “Unpacking the Literature on Stress and Resiliency: A Narrative Review Focused on Learners in the Operating Room.” Journal of Surgical Education 76 (2): 343–353.
- Palmer, Gary, James H. Abernathy, Greg Swinton, David Allison, Joel Greenstein, Scott Shappell, Kevin Juang, and Scott T. Reeves. 2013. “Realizing Improved Patient Care through Human-Centered Operating Room Design: A Human Factors Methodology for Observing Flow Disruptions in the Cardiothoracic Operating Room.” Anesthesiology 119 (5): 1066–1077. doi:10.1097/ALN.0b013e31829f68cf.
- Parush, Avi, Chelsea Kramer, Tara Foster-Hunt, Kathryn Momtahan, Aren Hunter, and Benjamin Sohmer. 2011. “Communication and Team Situation Awareness in the OR: Implications for Augmentative Information Display.” Journal of Biomedical Informatics 44 (3): 477–485. doi:10.1016/j.jbi.2010.04.002.
- Patel, A.R., and S.E. Eggener. 2011. “Warm Ischemia Less than 30 Minutes is Not Necessarily Safe during Partial Nephrectomy: Every Minute Matters.” Urologic Oncology 29 (6): 826–828. doi:10.1016/j.urolonc.2011.02.015.
- Persoon, Marjolein C., Hans J.H.P. Broos, J. Alfred Witjes, Ad J.M. Hendrikx, and Albert J.J.M. Scherpbier. 2011. “The Effect of Distractions in the Operating Room during Endourological Procedures.” Surgical Endoscopy 25 (2): 437–443. doi:10.1007/s00464-010-1186-8.
- Porpiglia, Francesco, Julien Renard, Michele Billia, Francesca Musso, Alessandro Volpe, Rodolfo Burruni, Carlo Terrone, Loredana Colla, Giorgina Piccoli, Valerio Podio, and Roberto Mario Scarpa. 2007. “Is Renal Warm Ischemia over 30 Minutes during Laparoscopic Partial Nephrectomy Possible? One-Year Results of a Prospective Study.” European Urology 52 (4): 1170–1178. doi:10.1016/j.eururo.2007.04.024.
- Rivera-Rodriguez, A.J., and B.-T. Karsh. 2010. “Interruptions and Distractions in Healthcare: Review and Reappraisal.” Quality & Safety in Health Care 19 (4): 304–312. doi:10.1136/qshc.2009.033282.
- Robertson, Helen D., Alison M. Elliott, Christopher Burton, Lisa Iversen, Peter Murchie, Terry Porteous, and Catriona Matheson. 2016. “Resilience of Primary Healthcare Professionals: A Systematic Review.” The British Journal of General Practice: The Journal of the Royal College of General Practitioners 66 (647): e423–e433. doi:10.3399/bjgp16X685261.
- Sanderson, P., T. McCurdie, and T. Grundgeiger. 2019. “Interruptions in Health Care: Assessing Their Connection With Error and Patient Harm.” Human Factors: The Journal of the Human Factors and Ergonomics Society 61 (7): 1025–1036. doi:10.1177/0018720819869115.
- Schraagen, Jan Maarten, Ton Schouten, Meike Smit, Felix Haas, Dolf van der Beek, Josine van de Ven, and Paul Barach. 2011. “A Prospective Study of Paediatric Cardiac Surgical Microsystems: assessing the Relationships between Non-Routine Events, Teamwork and Patient Outcomes.” BMJ Quality & Safety 20 (7): 599–603.
- Schreyer, Julia, Amelie Koch, Annika Herlemann, Armin Becker, Boris Schlenker, Ken Catchpole, and Matthias Weigl. 2022. “RAS-NOTECHS: Validity and Reliability of a Tool for Measuring Non-Technical Skills in Robotic-Assisted Surgery Settings.” Surgical Endoscopy 36 (3): 1916–1926. doi:10.1007/s00464-021-08474-2.
- Sevdalis, N., A.N. Healey, and C.A. Vincent. 2007. “Distracting Communications in the Operating Theatre.” Journal of Evaluation in Clinical Practice 13 (3): 390–394. doi:10.1111/j.1365-2753.2006.00712.x.
- Shouhed, Daniel, Bruce Gewertz, Doug Wiegmann, and Ken Catchpole. 2012. “Integrating Human Factors Research and Surgery: A Review.” Archives of Surgery 147 (12): 1141–1146. doi:10.1001/jamasurg.2013.596.
- Smith, A.F., and E. Plunkett. 2019. “People, Systems and Safety: resilience and Excellence in Healthcare Practice.” Anaesthesia 74 (4): 508–517. doi:10.1111/anae.14519.
- Sverdrup, T.E., V. Schei, and Ø.A. Tjølsen. 2017. “Expecting the Unexpected: Using Team Charters to Handle Disruptions and Facilitate Team Performance.” Group Dynamics: Theory, Research, and Practice 21 (1): 53–59. doi:10.1037/gdn0000059.
- Tiferes, Judith, Ahmed A. Hussein, Ann Bisantz, Justen D. Kozlowski, Mohamed A. Sharif, Nathalie M. Winder, Nabeeha Ahmad, Jenna Allers, Lora Cavuoto, and Khurshid A. Guru. 2016. “The Loud Surgeon Behind the Console: Understanding Team Activities During Robot-Assisted Surgery.” Journal of Surgical Education 73 (3): 504–512.
- Tschan, Franziska, Sandra Keller, Norbert K. Semmer, Eliane Timm-Holzer, Jasmin Zimmermann, Simon A. Huber, Simon Wrann, Martin Hübner, Vanessa Banz, Gian Andrea Prevost, Jonas Marschall, Daniel Candinas, Nicolas Demartines, Markus Weber, and Guido Beldi. 2021. “Effects of Structured Intraoperative Briefings on Patient Outcomes: Multicentre before-and-after Study.” The British Journal of Surgery 109 (1): 136–144. doi:10.1093/bjs/znab384.
- Vincent, Charles, Krishna Moorthy, Sudip K. Sarker, Avril Chang, and Ara W. Darzi. 2004. “Systems Approaches to Surgical Quality and Safety.” Annals of Surgery 239 (4): 475–482. doi:10.1097/01.sla.0000118753.22830.41.
- Wahlström, Mikael, Laura Seppänen, Leena Norros, Iina Aaltonen, and Jarno Riikonen. 2018. “Resilience through Interpretive Practice – A Study of Robotic Surgery.” Safety Science 108: 113–128. doi:10.1016/j.ssci.2018.04.010.
- Weber, Jeannette, Ken Catchpole, Armin J. Becker, Boris Schlenker, and Matthias Weigl. 2018. “Effects of Flow Disruptions on Mental Workload and Surgical Performance in Robotic-Assisted Surgery.” World Journal of Surgery 42 (11): 3599–3607.
- Weigl, Matthias, Jeannette Weber, Elyse Hallett, Michael Pfandler, Boris Schlenker, Armin Becker, and Ken Catchpole. 2018. “Associations of Intraoperative Flow Disruptions and Operating Room Teamwork During Robotic-Assisted Radical Prostatectomy.” Urology 114: 105–113. doi:10.1016/j.urology.2017.11.060.
- Weigl, Matthias, Ken Catchpole, Markus Wehler, and Anna Schneider. 2020. “Workflow Disruptions and Provider Situation Awareness in Acute Care: An Observational Study with Emergency Department Physicians and Nurses.” Applied Ergonomics 88: 103155. doi:10.1016/j.apergo.2020.103155.
- Werner, N.E., and R.J. Holden. 2015. “Interruptions in the Wild: Development of a Sociotechnical Systems Model of Interruptions in the Emergency Department through a Systematic Review.” Applied Ergonomics 51: 244–254. doi:10.1016/j.apergo.2015.05.010.
- Wheelock, Ana, Amna Suliman, Rupert Wharton, E.D. Babu, Louise Hull, Charles Vincent, Nick Sevdalis, and Sonal Arora. 2015. “The Impact of Operating Room Distractions on Stress, Workload, and Teamwork.” Annals of Surgery 261 (6): 1079–1084. doi:10.1097/SLA.0000000000001051.
- Widmer, Lukas W., Sandra Keller, Franziska Tschan, Norbert K. Semmer, Eliane Holzer, Daniel Candinas, and Guido Beldi. 2018. “More Than Talking About the Weekend: Content of Case-Irrelevant Communication Within the OR Team.” World Journal of Surgery 42 (7): 2011–2017. doi:10.1007/s00268-017-4442-4.
- Wiegmann, Douglas A., Andrew W. ElBardissi, Joseph A. Dearani, Richard C. Daly, and Thoralf M. Sundt. 2007. “Disruptions in Surgical Flow and Their Relationship to Surgical Errors: An Exploratory Investigation.” Surgery 142 (5): 658–665. doi:10.1016/j.surg.2007.07.034.
- Willett, Matthew, Orla Gillman, Esther Shin, Emma Sewart, Daniel Muller, Maud Nauta, and Wai Yoong. 2018. “The Impact of Distractions and Interruptions during Cesarean Sections: A Prospective Study in a London Teaching Hospital.” Archives of Gynecology and Obstetrics 298 (2): 313–318. doi:10.1007/s00404-018-4810-9.
