Abstract
Comfortable and well-fitting bras are necessary for good quality of life but hard to find for women who undergo reconstruction after breast cancer treatment. This study aimed to provide data to inform bra designs for breast cancer survivors. We measured anatomical distances used in bra design on 3D clinical photographs of patients who underwent unilateral and bilateral implant-based reconstruction to quantify changes after reconstruction relative to the measured values before the person underwent surgery. We performed additional assessments of symmetry before surgery and after reconstruction, and we used regression analyses to identify associations between the measurements and patient characteristics, such as BMI. Overall, almost all measurements changed significantly in implant-based reconstructed breasts relative to native breasts. We highlight several aspects of ergonomic bra design that will be impacted by the changes in anatomical distances.
Practitioner summary: Implant-based breast reconstruction surgery changes the breast so that off-the-rack bras are inadequate. This study provides designers with measurement data from women who underwent implant-based reconstruction to inform bra designs for this population. The key factor designers need to account for is the semi-spherical shape of the reconstructed breast.
1. Introduction
It is well-established that women often wear ill-fitting bras. Researchers have found that between 85 and 100% of their study participants wear the wrong size bra (White and Scurr Citation2012; Greenbaum et al. Citation2003; McGhee and Steele Citation2010; Chen, LaBat, and Bye Citation2011). Factors that lead to wearing ill-fitting bras include insufficient knowledge about how a bra should fit, a lack of standardisation in bra sizes among manufacturers, and inadequate bra design (McGhee and Steele Citation2020; Coltman, Steele, and McGhee Citation2018). Physical symptoms due to wearing ill-fitting bras include back pain, poor posture, and exercise-induced discomfort. Upper-limb neural symptoms and deep bra furrows can also be caused by excessive bra strap pressure (Coltman, Steele, and McGhee Citation2018; McGhee and Steele Citation2010; McGhee and Steele Citation2020; Coltman, McGhee, and Steele Citation2017; Coltman, McGhee, and Steele Citation2015).
Ill-fitting bras are especially burdensome for breast cancer survivors, whose breasts can be permanently and substantially changed by breast cancer and its treatment. Typically, specialised garments are needed during the acute postoperative phase or during radiation treatment. Many breast cancer patients temporarily use a surgical bra, a garment that the surgeon places on a woman immediately after breast surgery that is worn for ∼1 month postoperatively in lieu of an off-the-rack bra. Unfortunately, surgical bras are inadequate and medical staff often act as tailors to fit the generic bra to a specific patient’s body. Moreover, after the healing process is complete, many women desire to return to wearing bras similar to their preoperative garments. Unfortunately, off-the-rack bras are inadequate for breast cancer patients and survivors because of the breast changes that persist after treatment (Nicklaus et al. Citation2019).
Bra needs and preferences vary by type of breast cancer treatment (LaBat, Ryan, and Sanden-Will Citation2017). Those who have breast-conserving surgery may choose to wear an external prosthesis or search for bras that can accommodate a breast defect, such as a contour deformity (Fitch et al. Citation2012). Women who have mastectomy without reconstruction can use an external breast prosthesis or go flat. There is substantial variation in the bras used by women who have reconstruction following breast-conserving surgery or mastectomy, and some choose to not wear a bra (Nicklaus et al. Citation2020). It is important to note that while reconstruction can mitigate the appearance changes resulting from breast cancer and its treatment, even women who undergo reconstruction can still have substantial asymmetry between their breasts as well as breast shapes quite different from that of women who have not had breast cancer (Nicklaus et al. Citation2019; Gho et al. Citation2014).
In addition to the physical symptoms resulting from wearing an ill-fitting bra, many breast cancer survivors also experience psychological symptoms, such as restlessness and anxiousness about their bodily changes (Liu, Zheng, and Xu Citation2019). Moreover, the process of finding an acceptable ready-to-wear bra typically requires more time and effort for breast cancer survivors than for other women, leading to increased frustration and reminders of how breast cancer and its treatment have forever changed their bodies.
There has been limited research on how to improve the construction of bras for women who have undergone breast reconstruction. Most research on bras for breast cancer survivors focuses on the problems and needs of survivors who wear mastectomy bras (Leung et al. Citation2021; McGhee, Mikilewicz, and Steele Citation2020), i.e. bras containing pockets to hold breast prosthetics. 3D photography, especially body surface stereophotogrammetry, is a promising technology for bra design (Abtew et al. Citation2018; Amoozegar-Montero and Ramírez Citation2017) but has not been utilised for breast reconstruction patients. The patients who underwent implant-based reconstruction in LaBat et al. indicated that implants cause ‘comfort and appearance problems,’ but ‘few suggestions were offered for bra improvement’ (LaBat, Ryan, and Sanden-Will Citation2017). The goal of this study is to augment the previous qualitative studies of women’s post-reconstruction satisfaction with bras with quantitative information to determine what bra construction components lead to discomfort for patients who undergo implant-based reconstruction. We have previously developed a correspondence system between torso measurements typically used in bra design and torso measurements typically used to assess reconstruction surgery outcomes. In this study, we analyse torso measurements on 3D photographs of patients before and after unilateral and bilateral implant-based breast reconstruction and discuss implications for improving bra design for women who have undergone breast reconstruction.
2. Materials and methods
2.1. Participants
The participants in this analysis were selected from a study of 505 women who underwent breast reconstruction at The University of Texas MD Anderson Cancer Centre from 2011 to 2014. The 505 patients underwent a variety of reconstruction procedure types and entered the study at different phases in their reconstruction care. Medical record data and 3D photographs (surface scans) of the participants’ torsos were acquired at a baseline study visit and 3, 6, 9, 12, 18, and 18+ months after reconstruction. The 3D photographs were collected with a custom 3dMDTorso System (3dMD, Atlanta, GA, USA). Participants in this analysis were those who underwent bilateral or unilateral implant-based reconstruction and had both a baseline 3D photograph with two native breasts and a post-reconstruction 3D photograph at least 3 months after a final major surgery, such as tissue expander exchange to implant.
Ethics Statement: Participants provided informed consent under The University of Texas MD Anderson Cancer Centre Institutional Review Board protocol #2010-0321.
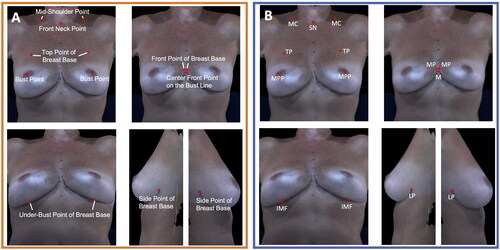
2.2. Clinical bra measurements
Previously, we identified eight measurements used in bra design that can be assessed on clinical 3D photographs of breast reconstruction patients (Nicklaus et al. Citation2017). The nine measurements included in this study are bust point distance, front neck point to bust point, front point of breast base to bust point, under-bust point of breast base to bust point, side point of breast base to bust point, top point of breast base to bust point, centre front point on bust line to bust point, mid-shoulder point to top point of breast base, and front point of breast base distance (shown in Results and Supplementary Figures). These measurements use the following anatomical fiducial points: most projecting point, lateral point, inframammary fold, medial point, midline, mid-clavicle, sternal notch, and transition point, visualised in . The most projecting point is used rather than the nipple since many women do not have nipples after mastectomy and reconstruction. We measured these properties on both breasts in the baseline pre-surgery and post-reconstruction 3D photographs by manually selecting the fiducial points using proprietary software. An experienced reconstructive surgeon (GPR) verified all fiducial point selections. We also calculated symmetry for all breast measurements, except for bust point distance and front point of breast base distance, as the ratio of the shorter measurement to the longer measurement.
Figure 1. (A) Anatomical landmarks used for bra fitting. (B) Anatomical fiducial points used in the clinical bra measurements. MPP: most projecting point; TP: transition point; MC: mid-clavicle; SN: sternal notch; MP: medial point; M: midline; IMF: inframammary fold; LP: lateral point.
2.3. Statistical analyses
Statistical analyses were performed separately for the patients who underwent unilateral implant-based reconstruction and the patients who underwent bilateral implant-based reconstruction. Descriptive statistics were calculated for the breast measurements, the symmetry of the measurements, and the percent change in the measurements between the pre-surgery baseline and post-reconstruction time points. The measurements and the symmetry of the measurements were statistically compared between the pre-surgery baseline and post-reconstruction time points using either the paired Students’ t-test or Wilcoxon signed-rank test, depending on the normality of the data. Normality was assessed using Q-Q plots and the Shapiro-Wilk test.
A linear regression analysis was performed to investigate associations between demographic variables, medical variables, and the post-reconstruction breast measurements for the patients who underwent bilateral reconstruction. A multiple linear mixed-effects model was fit for each breast measurement, with the post-reconstruction measurement as the dependent variable and baseline measurement as the independent variable. Patient effect was included as a random effect to account for the intracluster dependence for bilateral patients. Covariates included in the model were implant shape, body mass index (BMI), age, and recovery time (number of months since last major surgery). Residual plots were used to check the model fitting. Variance inflation factor (VIF) was used to measure the amount of multicollinearity. p-Values <0.05 were considered statistically significant. Analyses were conducted in R (R Core Team Citation2020).
3. Results
3.1. Participants
Thirty-three participants with bilateral implant-based reconstruction and 14 participants met the criteria with unilateral implant-based reconstruction met the selection criteria. Reasons participants were excluded from this analysis included undergoing a procedure other than bilateral or unilateral implant-based reconstruction, entering the study at an intermediate point in their reconstructive process, and missing 3D photographs at time points relevant to our analyses. All participants indicated female as their biological sex. The mean age of the participants was 46.7 ± 10.3 years, and mean BMI was 27.0 ± 5.6. Thirteen of the participants who underwent unilateral implant-based reconstruction also had contralateral symmetry procedures performed. Supplementary Table 1 contains a complete listing of participant demographics.
3.2. Unilateral participants clinical bra measurements
For the participants who underwent unilateral implant-based reconstruction, the reconstructed breasts were grouped for comparison to the contralateral breasts. Clinical bra measurements significantly changed in the reconstructed breast for the front neck point to bust point (), front point of breast base to bust point (), centre front point on the bust line to bust point (), and mid-shoulder point to top point of breast base measurements (). The inframammary fold point was not visible in 10/14 baseline photographs and 3/14 post-reconstruction photographs, which is typical due to natural breast ptosis. No measurement changed significantly for the contralateral breasts, despite most participants having contralateral symmetry procedures. (The bust point distance and front point of breast base distance measurements were each the same for the reconstructed and contralateral breasts since these measurements span both breasts.) Supplementary Tables 2 and 3 present the summary statistics and hypothesis testing results for the reconstructed and contralateral breasts, respectively. Supplementary Figures 1–5 show results for each of the non-statistically significant measurements.
Figure 2. The front neck point to bust point measurement (sternal notch to most projecting point) significantly decreased in the reconstructed breast after unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of the front neck point to bust point measurement at baseline and post-reconstruction (median and interquartile range). (B) The front neck point to bust point measurement on an exemplar patient at baseline. (C) The front neck point to bust point measurement on the same patient post-reconstruction.
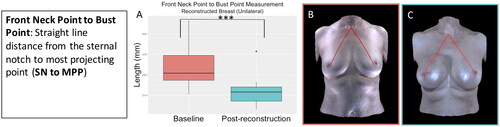
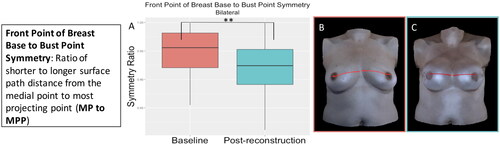
Figure 3. The front point of breast base to bust point measurement (medial point to most projecting point) significantly decreased in the reconstructed breast after unilateral implant-based reconstruction (p = 0.02). (A) Boxplot of the front point of breast base to bust point measurement at baseline and post-reconstruction (median and interquartile range). (B) The front point of breast base to bust point measurement on an exemplar patient at baseline. (C) The front point of breast base to bust point measurement on the same patient post-reconstruction.
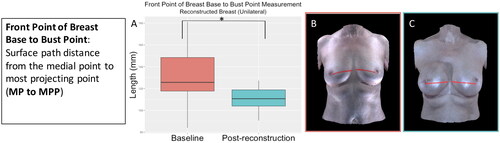
Figure 4. The centre front point on the bust line to bust point measurement (midline to most projecting point) significantly decreased in the reconstructed breast after unilateral implant-based reconstruction (p = 0.03). (A) Boxplot of the centre front point on the bust line to bust point measurement at baseline and post-reconstruction (median and interquartile range). (B) The centre front point on the bust line to bust point measurement on an exemplar patient at baseline. (C) The centre front point on the bust line to bust point measurement on the same patient post-reconstruction.
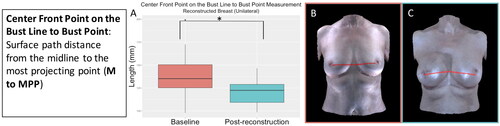
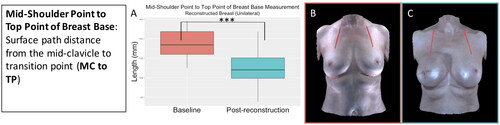
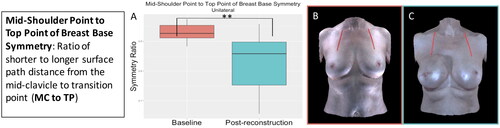
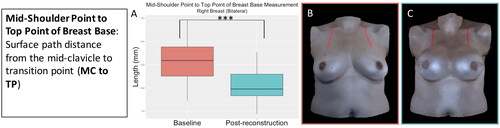
Figure 5. The mid-shoulder point to top point of breast base measurement (mid-clavicle to transition point) significantly decreased in the reconstructed breast after unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of the mid-shoulder point to top point of breast base measurement at baseline and post-reconstruction (median and interquartile range). (B) The mid-shoulder point to top point of breast base measurement on an exemplar patient at baseline. (C) The mid-shoulder point to top point of breast base measurement on the same patient post-reconstruction.
3.3. Unilateral participants’ symmetry measures
Symmetry significantly worsened (i.e. participants became more asymmetrical) for all measures except under-bust point of breast base to bust point (Supplementary Figure 6) and top point of breast base to bust point (Supplementary Figure 7) for the participants who underwent unilateral implant-based reconstruction. The statistically significant increase in asymmetry was expected for this cohort of participants owing to the inherent differences between the breast reconstructed with an implant and the revised native breast. show the symmetry measures that changed significantly for this group, and Supplementary Table 4 presents the summary statistics and results.
Figure 6. The front neck point to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The front neck point to bust point measurement on an exemplar patient. (C) The front neck point to bust point measurement on the same patient post-reconstruction.
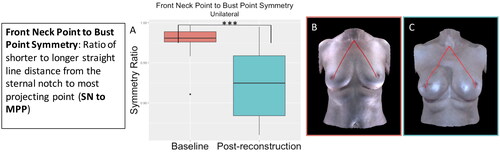
Figure 7. The front point of breast base to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The front point of breast base to bust point measurement on an exemplar patient. (C) The front point of breast base to bust point measurement on the same patient post-reconstruction.
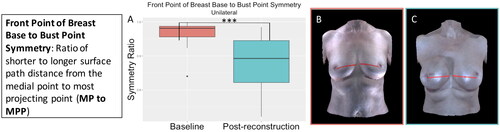
Figure 8. The side point of breast base to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p < 0.001). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The side point of breast base to bust point measurement on an exemplar patient. (C) The side point of breast base to bust point measurement on the same patient post-reconstruction.
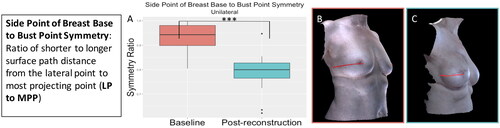
Figure 9. The centre front point on the bust line to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p = 0.01). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The centre front point on the bust line to bust point measurement on an exemplar patient. (C) The centre front point on the bust line to bust point measurement on the same patient post-reconstruction.
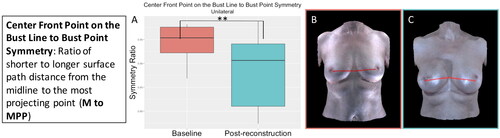
Figure 10. The mid-shoulder point to top point of breast base symmetry significantly decreased (became more asymmetrical) for the participants who underwent unilateral implant-based reconstruction (p = 0.002). (A) Boxplot of symmetry at baseline and post-reconstruction (median and interquartile range). (B) The mid-shoulder point to top point of breast base measurement on an exemplar patient. (C) The mid-shoulder point to top point of breast base measurement on the same patient post-reconstruction.
3.4. Bilateral participants clinical bra measurements
For the participants who underwent bilateral implant-based reconstruction, we grouped the breasts into left and right, as both breasts were reconstructed. All clinical bra measurements demonstrated significant change between baseline and post-reconstruction except side point of breast base to bust point measurement (Supplementary Figure 8), top point of breast base to bust point measurement (Supplementary Figure 9), and front point of breast base distance (Supplementary Figure 10). The results were consistent between the left and right breasts. The inframammary fold point was not visible in 20/33 baseline photographs owing to ptosis and missing data in the images. A few other measures were missing owing to missing data in the photographs. show the measurements that significantly changed for this group, and Supplementary Tables 5 and 6 contain the summary statistics and results for the right and left breasts, respectively.
Figure 11. The front neck point to bust point measurement (sternal notch to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly decreased in the reconstructed breast after implant-based reconstruction (right breast: p < 0.001, left breast: p < 0.001). (A) Boxplot (median and interquartile range) of the front neck point to bust point measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The front neck point to bust point measurement on an exemplar patient at baseline. (C) The front neck point to bust point measurement on the same patient post-reconstruction.
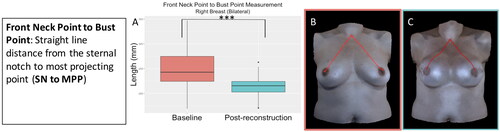
Figure 12. The bust point distance measurement (most projecting point to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly decreased after implant-based reconstruction (p = 0.003). (A) Boxplot of the bust point distance measurement at baseline and post-reconstruction (median and interquartile range). (B) The bust point distance measurement on an exemplar patient at baseline. (C) The bust point distance measurement on the same patient post-reconstruction.
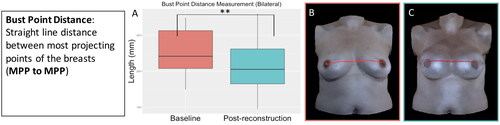
Figure 13. The front point of breast base to bust point measurement (medial point to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly decreased after implant-based reconstruction (right breast: p < 0.001, left breast: p < 0.001). (A) Boxplot (median and interquartile range) of the front point of breast base to bust point measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The front point of breast base to bust point measurement on an exemplar patient at baseline. (C) The front point of breast base to bust point measurement on the same patient post-reconstruction.
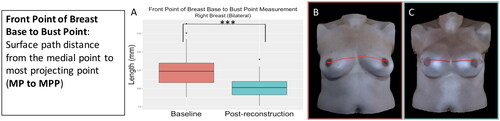
Figure 14. The under-bust point of breast base to bust point measurement (inframammary fold to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly increased after implant-based reconstruction (right breast: p = 0.03, left breast: p = 0.005). (A) Boxplot (median and interquartile range) of the under-bust point of breast base to bust point measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The under-bust point of breast base to bust point measurement on an exemplar patient at baseline. (C) The under-bust point of breast base to bust point measurement on the same patient post-reconstruction.
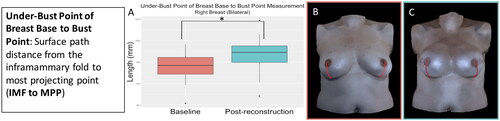
Figure 15. The centre front point on the bust line to bust point measurement (midline to most projecting point) for the participants who underwent bilateral implant-based reconstruction significantly decreased after implant-based reconstruction (right breast: p = 0.002, left breast: p = 0.003). (A) Boxplot (median and interquartile range) of the centre front point on the bust line to bust point measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The centre front point on the bust line to bust point measurement on an exemplar patient at baseline. (C) The centre front point on the bust line to bust point measurement on the same patient post-reconstruction.
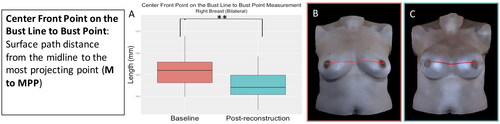
Figure 16. The mid-shoulder point to top point of breast base measurement (mid-clavicle to transition point) for the participants who underwent bilateral implant-based reconstruction significantly decreased after implant-based reconstruction (right breast: p < 0.001, left breast: p < 0.001). (A) Boxplot (median and interquartile range) of the mid-shoulder point to top point of breast base measurement at baseline and post-reconstruction for the right breast (left was similar). (B) The mid-shoulder point to top point of breast base measurement on an exemplar patient at baseline. (C) The mid-shoulder point to top point of breast base measurement on the same patient post-reconstruction.
3.5. Bilateral participants symmetry measures
Symmetry remained consistent between baseline and post-reconstruction for the participants who underwent bilateral implant-based reconstruction. The only symmetry measure that demonstrated a significant change was the front point of breast base to bust point symmetry, which decreased. demonstrates the front point of breast base to bust point symmetry change between baseline and post-reconstruction. Supplementary Table 7 contains the symmetry measure summary statistics and results for this group, and Supplementary Figures 11–16 show the remaining symmetry measures.
Figure 17. The front point of breast base to bust point symmetry significantly decreased (became more asymmetrical) for the participants who underwent bilateral implant-based reconstruction (p = 0.01). (A) Boxplot (median and interquartile range) of symmetry at baseline and post-reconstruction. (B) The front point of breast base to bust point measurement on an exemplar patient. (C) The front point of breast base to bust point measurement on the same patient post-reconstruction.
3.6. Regression analysis
We did not find any statistically significant associations between age, BMI, implant shape, or recovery time and the postoperative clinical bra measurements for the participants who underwent bilateral implant-based reconstruction (Supplementary Tables 8–16). On the other hand, the front neck point to bust point (Supplementary Table 8), side point of breast base to bust point (Supplementary Table 11), centre front point on the bust line to bust point (Supplementary Table 13), under-bust point to bust point (Supplementary Table 14), and bust point distance (Supplementary Table 16) revealed statistically significant associations between the postoperative measurement and baseline measurement.
4. Discussion
We discuss the implications of the breast measurement changes due to implant-based reconstruction on the design of bras intended for wear under a variety of tops, such as t-shirt bras. Bra designers and manufacturers will be able to use these measurement changes and the implications to bra components to customise bras for this patient population. As changes in one bra component can affect the fit of other bra components, all of the measurements need to be taken into consideration with each other to optimise fit. The key change that designers will have to account for is bra cup shape, which is discussed in section 4.4. We do not discuss implications for other types of bras, such as sports bras meant to be worn during exercise activities or aesthetic lingerie. Overall, this study is the first to analyse the difference in bra measurements before and after breast cancer treatment and implant-based reconstruction. These results can inform and inspire bra designers and manufacturers, mastectomy bra fitters, and others who counsel patients about bra fit after breast surgery.
4.1. Implications for bra design: bra strap design
The mid-shoulder point to top point of breast base measurement decreased significantly (), indicating that the reconstructed breasts are typically positioned higher on the chest wall than are native breasts. Likewise, the front neck point to bust point measurement also decreased (), reflecting the upward vertical movement of the bust point. These anatomical changes make sense from a surgical perspective. In an implant-based reconstruction, the implant is placed either under the skin or under the pectoralis muscle and surrounded by an acellular dermal matrix after the removal of native breast tissue. But, since an implant-reconstructed breast is more rigid than native breast tissue, the implant can’t deform to fit into small spaces. Often, the acellular matrix and pectoralis muscle limit the movement of the implant, forcing the implant to ride higher on the chest wall than the native tissue did.
While most bra straps are adjustable, our findings indicate that women with implant-based reconstructed breasts may need to be able to make more strap adjustments than other bra-wearers. Since the reconstructed breast is positioned higher on the chest wall, the shortest position of the bra strap may need to be shorter than for bra designs created for native breasts. In addition, the location of the bra cup where the bra strap is anchored may need to differ from the standard bra design to better support the implant-based reconstructed breast. In clothing design, patterns for bra straps position the sewing point on the outer edges of the expected apex of the breast (Coltman, McGhee, and Steele Citation2015).
4.2. Implications for bra design: bra bridge design
Overall, the change between baseline and post-reconstruction in the front point of breast base distance (medial point to medial point) (Supplementary Figures 5, 10) was not statistically significant in our study. However, we observed substantial patient variation in this measurement at both the baseline and post-reconstruction time points. For example, the range of the post-reconstruction front point of breast base distance measurement for patients who underwent bilateral reconstruction was 4.3–60.7 mm. Some patients experience more distance between the implants due to the lateral attachments of the breast tissue to the chest wall being removed during the mastectomy. Increased distance between the implants can also occur if the skin ‘pocket’ in which the implant sits on the chest wall is too large so that the implants can slide towards the sides of the body. In both scenarios, the implant moves laterally and inferior from the original breast position. Consequently, some patients exhibited large changes in the front point of breast base distance. The subset of patients whose front point of breast base distance was changed substantially by breast cancer and its treatment might benefit from undergarments customised to accommodate this particular anatomical change for a more ergonomic fit.
4.3. Implications for bra design: symmetry
Overall, symmetry for participants who underwent bilateral implant-based reconstruction was about the same post-operatively as pre-operatively, which is to be expected when implants of the same size and shape are used for both breasts. The front point of breast base to bust point symmetry () did significantly decrease, but the mean post-reconstruction symmetry for this measure was still 0.92, which is within the range of preoperative symmetry observed in this study.
On the other hand, symmetry is a major concern for people who undergo unilateral implant-based reconstruction. Even though most participants underwent additional procedures to improve symmetry, participants became significantly more asymmetrical for all symmetry measures except for the under-bust point of breast base to bust point and top point of breast base to bust point measures. Off-the-rack bras will not accommodate the significant shape and chest wall position asymmetry for these patients.
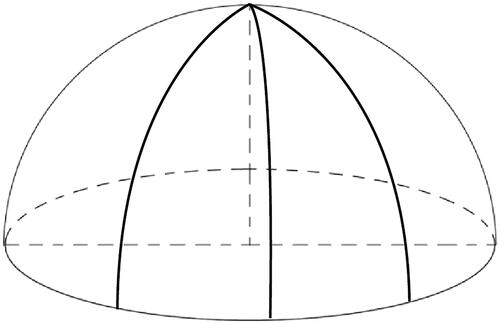
4.4. Implications for bra design: bra cup shape
Changes in four of the clinical bra measurements indicate a need to change the bra cup shape: the top point of breast base to bust point, front point of breast base to bust point, under-bust point of breast base to bust point, and side point of breast base to bust point. The base of an implant-based reconstructed breast is more circular than that of a native breast, and the breast shape is more semi-spherical. During mastectomy, oftentimes the nipple-areola complex tissue is removed, which contributes to creating the natural shape and projection of the breast. Without this tissue, the reconstructed breast shape is formed from the shape of the implant. This change causes the bust point or apex of the breast to be located more superior, medial, and posterior than its normal position on the native breast. The four measurements of the breast base change in conjunction with each other in reconstructed breasts. The under-bust point of breast base to bust point measurement (, Supplementary Figure 3) increased due to the upward shift in the location of the bust point and lack of ptosis. The front point of breast base to bust point measurement () decreased due to the medial movement of the bust point. The top point of breast base to bust point measurement (Supplementary Figures 2, 9) remained about the same for both the participants with unilateral reconstruction and participants with bilateral reconstruction. The path length remained about the same even though the bust point location shifted vertically because of the breast shape change such that the upper pole of the breast was fuller and more rounded. The side point of breast base to bust point distance remained about the same for the bilateral participants (Supplementary Figure 8) and decreased slightly (not statistically significantly) for the unilateral patients (Supplementary Figure 4). The lack of change in this measurement can be attributed to competing changes in the placement of the bust point, breast size, and lateral pole fullness. Thus, the bra cup design for implant-based reconstructed breasts needs to be adapted to smoothly cover the semi-spherical shape of the breast, especially over the upper pole of the breast, as shown in . These results concur with LaBat et al. who found patients complained their implants were ‘too rounded’ to find a bra that adequately fit (LaBat, Ryan, and Sanden-Will Citation2017). Since we found no associations between implant shape (round vs. anatomical) and post-reconstruction measurements, we believe a semi-spherical bra cup shape will serve the largest number of patients. Further research will be needed to determine whether a different design is necessary for patients with anatomically-shaped implants.
Figure 18. The semi-spherical shape of a bra cup for an implant-based reconstructed breast. The darts or the seams of the bra cup should be evenly distributed so that it will fit the semi-spherical shape of the implant-based reconstructed breast.
4.5. Study limitations
The limitations of this study include a modest sample size, only analysing patients who underwent implant-based reconstructions, and narrow scope to focus only on anatomical measurements. Bra designers and manufacturers will need to expand upon this work to develop a better fitting garment for this patient population and incorporate the work of other researchers who have performed qualitative studies to fully meet patients’ needs. The results in this study are not generalisable to women who undergo other forms of reconstruction after breast cancer treatment. These patients will require separate studies to develop appropriate undergarments for their needs since different forms of reconstruction have different impacts on breast size, shape, and symmetry.
4.6. Opportunities for future work
As demonstrates, conventional cutting and sewing patterns would require multiple seams to lie flat over the shape of the breast implant. Seams can irritate the skin (Seram and Senadheera Citation2020), which is a particular concern for breast cancer survivors who often experience reduced protective sensation of the breast skin due to nerve damage from breast cancer and its treatment (Lovelace, McDaniel, and Golden Citation2019). Different bra construction techniques, such as moulding, knitting, or weaving, could be explored to achieve the needed cup shape without seams. Rapid prototyping technologies may be investigated to create custom garments for women with extreme asymmetry, such as the patients who underwent unilateral reconstruction.
In addition, there are important properties of the reconstructed breast that cannot be assessed from imaging, such as the mechanical properties of the implant and loss of sensation, which need to be considered for the ideal bra design for reconstruction patients. These aspects can be studied qualitatively (LaBat, Ryan, and Sanden-Will Citation2017) and quantitatively (McGhee et al. Citation2013; Sun et al. Citation2019) and may impact bra design choices, such as fibre type and construction. In addition, advances in thermo-regulating fabrics (Prajapati and Kandasubramanian Citation2020), moisture-adaptive fabrics (Gorea, Baytar, and Sanders Citation2020), and pressure-sensitive fabrics (Zhou et al. Citation2017) could address some of the issues women face after breast surgery.
Our regression analysis results suggest that clinical variables, such as age and BMI may not be important factors in changes in the clinical bra measurements for patients who undergo implant-based reconstruction. However, for other types of reconstruction, such as autologous reconstruction, these factors may play more significant roles. Conducting similar analyses for other types of reconstruction is crucial for improving the quality of life of all patients who undergo breast reconstruction.
Little quantitative research has been performed to directly study the impact of a poor-fitting bra on breast cancer survivors and breast reconstruction patients, including psychosocial, physiological, and economical. Measuring these impacts could bring more attention to the need for improved bra designs for breast cancer survivors and determine whether new bra designs are effective in mitigating these effects.
Supplemental Material
Download Zip (11 MB)Acknowledgements
The manuscript was edited by Sarah Bronson, ELS, of the Research Medical Library at The University of Texas MD Anderson Cancer Center.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, MKM. The data are not publicly available due to their containing information that could compromise the privacy of research participants.
Additional information
Funding
References
- Abtew, Mulat Alubel, Pascal Bruniaux, François Boussu, Carmen Loghin, Irina Cristian, and Yan Chen. 2018. “Development of Comfortable and Well-Fitted Bra Pattern for Customized Female Soft Body Armor through 3D Design Process of Adaptive Bust on Virtual Mannequin.” Computers in Industry 100 (September): 7–20. doi:10.1016/j.compind.2018.04.004.
- Amoozegar-Montero, Ariya Xuxu, and Edgar Rodríguez Ramírez. 2017. Parametric Modelling for Better Bra Fit & Design. Vancouver: Modeling and Simulation Western Decision Sciences Institute (WDSI). doi:10.26686/wgtn.13012841.v1.
- Chen, Chin-Man, Karen LaBat, and Elizabeth Bye. 2011. “Bust Prominence Related to Bra Fit Problems.” International Journal of Consumer Studies 35 (6): 695–701. doi:10.1111/j.1470-6431.2010.00984.x.
- Coltman, Celeste E., Deirdre E. McGhee, and Julie R. Steele. 2015. “Bra Strap Orientations and Designs to Minimise Bra Strap Discomfort and Pressure during Sport and Exercise in Women with Large Breasts.” Sports Medicine-Open 1 (1): 21. doi:10.1186/s40798-015-0014-z.
- Coltman, Celeste E., Deirdre E. McGhee, and Julie R. Steele. 2017. “Three-Dimensional Scanning in Women with Large, Ptotic Breasts: Implications for Bra Cup Sizing and Design.” Ergonomics 60 (3): 439–445. doi:10.1080/00140139.2016.1176258.
- Coltman, Celeste E., Julie R. Steele, and Deirdre E. McGhee. 2018. “Which Bra Components Contribute to Incorrect Bra Fit in Women across a Range of Breast Sizes?” Clothing and Textiles Research Journal 36 (2): 78–90. doi:10.1177/0887302X17743814.
- Fitch, Margaret I., Alison McAndrew, Andrea Harris, Jim Anderson, Todd Kubon, and Jay McClennen. 2012. “Perspectives of Women about External Breast Prostheses.” Canadian Oncology Nursing Journal 22 (3): 162–174. doi:10.5737/1181912x223162167.
- Gho, Sheridan A., Bridget J. Munro, Sandra C. Jones, and Julie R. Steele. 2014. “Exercise Bra Discomfort is Associated with Insufficient Exercise Levels among Australian Women Treated for Breast Cancer.” Supportive Care in Cancer 22 (3): 721–729. doi:10.1007/s00520-013-2027-9.
- Gorea, Adriana, Fatma Baytar, and Eulanda A. Sanders. 2020. “Experimental Design and Evaluation of a Moisture Responsive Sports Bra.” Fashion and Textiles 7 (1): 20. doi:10.1186/s40691-020-00209-6.
- Greenbaum, A.R., T. Heslop, J. Morris, and K.W. Dunn. 2003. “An Investigation of the Suitability of Bra Fit in Women Referred for Reduction Mammaplasty.” British Journal of Plastic Surgery 56 (3): 230–236. doi:10.1016/S0007-1226(03)00122-X.
- LaBat, Karen L., Karen S. Ryan, and Sherry Sanden-Will. 2017. “Breast Cancer Survivors’ Wearable Product Needs and Wants: A Challenge to Designers.” International Journal of Fashion Design, Technology and Education 10 (3): 308–319. doi:10.1080/17543266.2016.1250289.
- Leung, Kaoru, Kristina Shin, Fred Han, and Jiao Jiao. 2021. “Ergonomic Mastectomy Bra Design: Effect on Core Body Temperature and Thermal Comfort Performance.” Applied Ergonomics 90 (January): 103249. doi:10.1016/j.apergo.2020.103249.
- Liu, Chi., Xueqing Zheng, and Bugao Xu. 2019. “Design Requirements of Mastectomy Bra for Formal Dress.” In Advances in Ergonomics in Design, Advances in Intelligent Systems and Computing, edited by Francisco Rebelo and Marcelo M. Soares, 172–182. Cham: Springer International Publishing. doi:10.1007/978-3-319-94706-8_20.
- Lovelace, Dawn L., Linda R. McDaniel, and Dwynn Golden. 2019. “Long-Term Effects of Breast Cancer Surgery, Treatment, and Survivor Care.” Journal of Midwifery & Women’s Health 64 (6): 713–724. doi:10.1111/jmwh.13012.
- McGhee, Deirdre E., Katelyn L. Mikilewicz, and Julie R. Steele. 2020. “Effect of External Breast Prosthesis Mass on Bra Strap Loading and Discomfort in Women with a Unilateral Mastectomy.” Clinical Biomechanics 73 (March): 86–91. doi:10.1016/j.clinbiomech.2019.12.027.
- McGhee, Deirdre E., and Julie R. Steele. 2010. “Optimising Breast Support in Female Patients through Correct Bra Fit. A Cross-Sectional Study.” Journal of Science and Medicine in Sport 13 (6): 568–572. doi:10.1016/j.jsams.2010.03.003.
- McGhee, Deirdre E., and Julie R. Steele. 2020. “Biomechanics of Breast Support for Active Women.” Exercise and Sport Sciences Reviews 48 (3): 99–109. doi:10.1249/JES.0000000000000221.
- McGhee, Deirdre E., Julie R. Steele, William J. Zealey, and George J. Takacs. 2013. “Bra–Breast Forces Generated in Women with Large Breasts While Standing and during Treadmill Running: Implications for Sports Bra Design.” Applied Ergonomics 44 (1): 112–118. doi:10.1016/j.apergo.2012.05.006.
- Nicklaus, Krista, Eloise Jewett, Chi Liu, Jun Liu, Gregory Reece, Summer Hanson, Fatima Merchant, and Mia K. Markey. 2019. “Trends in Breast Measurements of Unilateral Breast Reconstruction Patients to Inform Bra Design.” 10th International Conference and Exhibition on 3D Body Scanning and Processing Technologies, 272–279. doi:10.15221/19.272.
- Nicklaus, Krista M., Karen Bravo, Chi Liu, Deepti Chopra, Gregory P. Reece, Summer E. Hanson, and Mia K. Markey. 2020. “Undergarment Needs after Breast Cancer Surgery: A Key Survivorship Consideration.” Supportive Care in Cancer 28 (8): 3481–3484. doi:10.1007/s00520-020-05414-z.
- Nicklaus, Krista M., Jevon Chu, Chi Liu, Greg P. Reece, Fatima A. Merchant, Michelle C. Fingeret, and Mia K. Markey. 2017. “Correspondence of Breast Measurements for Bra Design after Reconstruction Surgery.” Proceedings of 3DBODY.TECH 2017 – 8th International Conference and Exhibition on 3D Body Scanning and Processing Technologies, Montreal QC, Canada, 11–12 October 2017, 106–112. Montreal: Hometrica Consulting-Dr. Nicola D’Apuzzo. doi:10.15221/17.106.
- Prajapati, Deepak G., and Balasubramanian Kandasubramanian. 2020. “A Review on Polymeric-Based Phase Change Material for Thermo-Regulating Fabric Application.” Polymer Reviews 60 (3): 389–419. doi:10.1080/15583724.2019.1677709.
- R Core Team. 2020. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing. https://www.R-project.org/
- Seram, Niromi C.K., and Malmi A.T. Senadheera. 2020. “Skin Issues Caused by Construction Techniques Used in Casual Garments: Survey of Female Consumers in Sri Lanka.” Conference Proceedings of the 2nd Asia International Conference on Multidisciplinary, Vol. 2, 65. https://www.aimr.tirdiconference.com/assets/images/portfolio/Conference-Proceeding-AIMR-20.pdf#page=71
- Sun, Yue., Kit-lun Yick, Winnie Yu, Lihua Chen, Newman Lau, Wanzhong Jiao, and Shichen Zhang. 2019. “3D Bra and Human Interactive Modeling Using Finite Element Method for Bra Design.” Computer-Aided Design 114 (September): 13–27. doi:10.1016/j.cad.2019.04.006.
- White, J., and J. Scurr. 2012. “Evaluation of Professional Bra Fitting Criteria for Bra Selection and Fitting in the UK.” Ergonomics 55 (6): 704–711. doi:10.1080/00140139.2011.647096.
- Zhou, Yuman, Jianxin He, Hongbo Wang, Kun Qi, Nan Nan, Xiaolu You, Weili Shao, Lidan Wang, Bin Ding, and Shizhong Cui. 2017. “Highly Sensitive, Self-Powered and Wearable Electronic Skin Based on Pressure-Sensitive Nanofiber Woven Fabric Sensor.” Scientific Reports 7 (1): 12949. doi:10.1038/s41598-017-13281-8.
