Abstract
Skin-to-skin contact between parents and preterm infants is recommended because it has proven to be valuable for the infants’ development and healing. However, it can be difficult to comply with this guideline and still ensure a good working environment for the staff.
This randomised controlled trial compared a new recliner developed in collaboration with parents and staff with a hospital bed for use in neonatal and maternity care using parents’ rating of own comfort/discomfort, self-reliance, and felt security, and the chair’s/bed’s functionality at two different days (Q1 and Q2) of hospitalisation. The physical work-environment was evaluated through a questionnaire to the staff.
Ninety-seven parents and 53 health professionals participated. Parents had significantly lower discomfort, in the recliner at Q1 compared to the hospital bed. The staff had to twist and/or bend their back significantly less often when working at the recliner as compared to the hospital bed.
Practitioner summary: Due to poor working environment, a participatory design project developed a new recliner that improved the possibility of infants having skin-to-skin contact with their parents. The recliner provided a better working-environment for the staff while focussing on improving comfort and self-reliance of the parents, as compared to a hospital bed.
Abbreviations: NICU: Neonatal Intensive Care Unit; VELA: Vermund Larsen
Introduction
The World Health Organisation recommends that premature infants have skin-to-skin contact with their parents. Skin-to-skin contact has proven to be valuable for preterm infants as it contributes to stabilising the infant’s temperature, pulse, and respiration, and improves weight gain and sleep patterns facilitating the parent–infant attachment process and lowering the parents’ stress (WHO Citation2022; Kostandy and Ludington-Hoe Citation2019; Ionio, Ciuffo, and Landoni Citation2021).
Nonetheless, there are barriers in implementing skin-to-skin contact. For example, parents’ anxiety about harming the infant while holding them in their arms, lack of attention from the staff, and deficiency of resources and space. Likewise, mothers have found hospital beds unsuitable for having skin-to-skin contact with their infants and have suggested that comfortable arm-chairs should be used instead (Jesney Citation2016; Seidman et al. Citation2015; Blomqvist et al. Citation2013; Benoit et al. Citation2016). For mothers, it is essential that skin-to-skin contact is easy to practice and still minimises postpartum pain (Jesney Citation2016; Seidman et al. Citation2015; Blomqvist et al. Citation2013; Lewis et al. Citation2019). Zhang and Helander found that among persons seated in a chair, the most important descriptions of the seat were ‘comfort’ and ‘discomfort’. Comfort is the feeling of well-being, relaxation, and relief, while discomfort is the feeling of restlessness, fatigue, tenderness, and pain (Helander Citation2003; Helander and Zhang Citation1997; Zhang, Helander, and Drury Citation1996).
Background
In Denmark, at least 20% of nurses reported that their physical working environment stressed their musculoskeletal system and forced them to twist their back during at least half of their working hours (Sørensen Citation2017). These findings corroborate international studies that reported a high prevalence of lower back pain related to nurses’ working-environment. This condition can become chronic and disabling (Adhikari and Dhakal Citation2014; Schlossmacher and Amaral Citation2012), and affects the well-being and productivity of the nurses, and the quality of care, as well as patient safety (Aiken et al., Citation2012; Albertsen, Jessen, and Nielsen Citation2015; Amaliyah and Tukimin Citation2021). A correlation has been found between patient satisfaction and nurses’ evaluation of their working environment, as well as between the working environment and quality of care: the better the working-environment, the better the healthcare and patient satisfaction (Aiken et al. Citation2012; Albertsen, Jessen, and Nielsen Citation2015). Also, strengthening the patients’ experience of self-control and self-reliance is important for the patients’ mental well-being. (Huisman et al. Citation2012). Being able to adjust the hospital bed by themselves is an example of being self-reliant.
The staff in the study neonatal intensive care unit (NICU) and maternity ward often complained of difficult working-environment as they had to stand, bend forward and had to twist their backs when guiding and supporting parents who were sitting with their infants in an arm-chair or hospital bed, putting the staff at risk of lumbar and back pain. In addition, the hospital’s biomedical laboratory scientists frequently complained of difficult working-conditions when taking blood sample from an infant being skin-to-skin with a parent. Therefore, the infants were often left in incubators or cradles while waiting for and while having blood samples taken. Even though, studies have shown that infants requiring a heel lance respond with less pain and crying when placed skin-to-skin with their parents (Johnston et al. Citation2017).
Parents were offered to sit in traditional arm-chairs with armrests and a high back that could be manually reclined to approximately 30 degrees in our study ward. The arm-chair was difficult to move and had a separate footrest. Hence, there were requests from parents to replace this arm-chair. However, no chair meeting the expressed needs of the parents and the staff at the NICU could be identified. Therefore, the Department of Paediatrics and Adolescent Medicine entered into a public–private innovation project with the aim of developing a new recliner. In a close collaboration between the parents of infants admitted to the NICU, interdisciplinary staff, the companies Vermund Larsen (VELA) and Design Concern A/S, a participatory design project was launched including field studies and workshops with parents, nurses, consultants, biomedical laboratory scientists, and cleaning staff. In addition, health and safety representatives and the hospital hygiene unit were involved in the process. As identified during this process the development of the new recliner focussed on comfort, self-reliance, security, and home-like appearance for the parents and improved working-environment and hygiene for the health professionals.
Several features of the new recliner were found to be crucial, e.g. that it could be reclined to give the best possible position for the mother when breastfeeding or sleeping; and that it could be raised and lowered to ensure an optimal working position for the staff without the parents feeling unsecure. These features could also allow the parents to see and touch their infants while resting in the incubator or cradle. As many parents sat with their infant skin-to-skin for longer periods, it had to be easy changing the settings of the recliner, such as adjusting the backrest, armrests, and footrest, without needing to ask the nurses for help. A stand-up lift feature helped parents when going from a sitting to a standing position while holding their infants. The recliner had a battery to ensure that it was easy to operate and move. These features also improved the work-environment of the staff (see a video and description of the final produced recliner VELA Neonatal Chair – For Neonatology Departments (vela-medical.com) (Vela Citation2022).
The aim of this study was to compare the newly developed recliner and a hospital bed for use in neonatal care with special focus on parents sitting skin-to-skin with their infants, both emphasising the comfort and self-reliance of the parents and the working environment of the nurses and other staff members.
Methods
Study design
This study was a randomised controlled trial carried out at Lillebaelt Hospital, University Hospital of Southern Denmark, at (1) A 22-bed level II NICU, annually treating around 600 ill newborn infants, including preterm infants with a gestational age of ≥28 weeks. Single, double, and quadruple patient rooms were available and a traditional arm-chair was provided at the incubator or cradle. Depending upon the availability of space in the NICU, a hospital bed could also be made available to the families. Parents and siblings had unrestricted access to stay with the infants and they were allowed to sleep in a patient hotel nearby.
(2) A 9-bed maternity unit with around 400 admissions of newborn infants with a gestational age of ≥ 35 weeks needing special care. Usually, the length of admission was between one and three days. One or both parents stayed with the infant in a family room, where a non-adjustable bed and a traditional arm-chair were available. The study was prepared and reported along with CONSORT checklist.
Participants
Infants admitted to the NICU from 15 August 2017, to 31 December 2017, and to the maternity ward from 16 November 2017, to 31 January 2018, were assessed for eligibility. Inclusion criteria: The infants’ parents understood verbal and written Danish (). Exclusion criteria: (a) infants discharged in ≤ 3 days; (b) critical illness of the mother or infant; (c) parents with social or psychological problems, and (d) infants admitted from home.
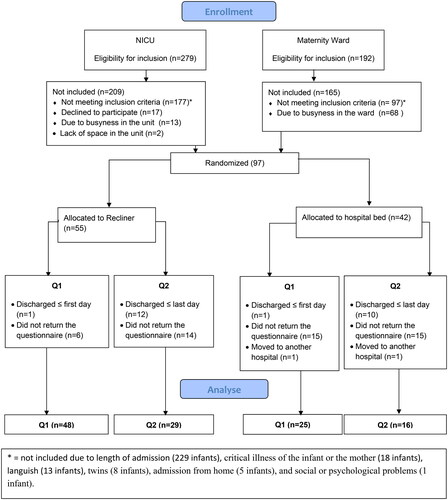
Figure 1. Flow-chart.
The nurses in the two study wards informed parents of infants who met the inclusion criteria. If they agreed to participate, the parents drew a sealed envelope determining whether the infant was randomised to test the recliner or the hospital bed. As birth method could have an impact on the seat comfort of the mothers, the infants at the NICU were stratified by block-randomisation according to birth method, either vaginal or caesarean section. Each block contained 10 sealed envelopes, five for each arm of the trial. For twins and triplets only the first-born infant was randomised.
All nurses, social assistants and doctors working in the NICU and the nurses and midwives working in the maternity ward during the inclusion periods were asked to complete a questionnaire in December 2017 and March 2018, respectively.
Measurement
Inspired by the questionnaire Chair Evaluation Checklist (Helander and Zhang Citation1997) the parents’ evaluation of the recliner and the hospital bed was sampled in two comfort and one discomfort scores. Comfort 1 consisted of five items (‘I feel relaxed’, ‘I feel refreshed’, ‘I feel comfortable’, ‘I do not feel restless’, and ‘I like the recliner/hospital bed’). Comfort 2 consisted of four items (‘The recliner/hospital bed is spacious’, ‘I do not feel cramped’, ‘I have enough support from the seat base or the seat back’, and ‘The recliner/hospital bed feels soft’). Discomfort included five items (‘I have sore muscles’, ‘I have heavy legs’, ‘I feel stiff’,, ‘I feel tired’, and ‘I feel uncomfortable’). The answers were rated on a 9-point Likert scale ranging from one (not at all) to nine (extremely).
In addition, the parents were asked to fill in a questionnaire regarding the functionality of the new recliner/hospital bed and their sense of self-reliance and safety (six items: ‘Easy to adjust’, ‘Safe to sit in’, ‘Support arms while giving tube feeding’, ‘Supports arms while bottle feeding’, ‘Supports arms while breast feeding’, and ‘Ensures self-reliance’). Furthermore, they were asked eight items on background information (see ) and finally to provide comments and suggestions for changes and improvements.
Table 1. Characteristics of the infants and the parents responding to the questionnaire.
The questionnaire regarding comfort/discomfort was forward-translated from English into Danish by two Danish-native speakers fluent in English, and then back-translated into English by an independent translator to provide quality control of the translation. The whole questionnaire was content validated by 10 parents and 10 staff members at two NICUs.
In the maternity ward, the father or the mother having skin-to-skin contact with the infant was asked to answer the first questionnaire (Q1) on day one. Parents admitted to the NICU were troubled and we didn’t expect them to being able to prioritise filling in a questionnaire right away. Therefore, they were asked to fill in their first questionnaire on the second day only. Due to this difference and as the admissions tended to be shorter in the maternity ward, the parents in the maternity ward having skin-to-skin contact were asked to fill in the last questionnaire (Q2) on the 3rd day, but only on the 5th day in the NICU. This was considered sufficient time for giving the parents an opportunity to gain experience with the functions of the recliner or the hospital bed.
To evaluate the physical working-environment of the staff, a questionnaire inspired by one developed for a Danish study among workers who had repetitive monotonous workflows (Det nationale forskningscenter for arbejdsmiljø Citation1994) was used after being content validated by 10 staff members at two NICUs. The questionnaire consisted of questions regarding the recliner and the hospital bed. It contained (a) five items on background – ‘Profession’, ‘Do you have had symptoms from your neck, lower back, shoulder and/or back during the past six month’; if confirmative, have any of the symptoms lasted for more than one month’, ‘Have you had pain and/or discomfort within the last month’ (answer options: yes and no), and ‘Your experience with the recliner and hospital-bed’ (answer options: no, little, some, and much), (b) seven items on working-environment – ‘It is easy to adjust to a satisfactory working height’, ‘I have a good working position’, ‘I twist my back’, ‘My back is heavily bent’, ‘My neck is heavily bent over’, ‘I adjust the working height for the specific task’, ‘I adjust the working height for having a conversation’ (answer options: never, rarely, sometimes, and often), and (c) an open-ended question for comments and suggestions for changes and improvements).
Both questionnaires were electronic and were given out using SurveyXact (http://www.surveyxact.com/).
Outcomes
The primary outcome was the difference in parents’ experience of comfort/discomfort in the recliner group compared to the hospital bed group at Q1 and Q2, respectively. Secondary outcomes were the differences between the recliner group and hospital bed group at Q1 and Q2 in parents’ experience of self-reliance, and in terms of staff members’ experience of their physical working environment.
Data analysis
The differences in comfort/discomfort-scores, experience of self-reliance, and working environment between the recliner and hospital bed groups were analysed in Stata statistical software, using a t-test and two-sample Wilcoxon rank-sum (Mann–Whitney) test.
Sub-analyses were performed to evaluate whether the comfort- and discomfort-scores of the recliner and hospital bed differed by sex, body height, or birth method.
As experience could be a factor in the evaluation of the physical working environment, the staff members were only included in the analysis of the results from the recliner and the hospital bed if they had had experience with the equipment in question.
Ethics
In accordance with the Danish law, the study did not need to be reviewed by an ethics committee but was approved by the Danish Data Protection Agency on 18 August 2017 (approval-number 20/53345). The participants were informed about the study in writing and orally before they agreed to participate. Participation was voluntary, and the participants could withdraw at any time. For all questionnaires, only the researcher knew the coding, and confidentiality and anonymity were guaranteed. The procedures followed were in accordance with the Helsinki Declaration.
Results
Participants
During the study period, 471 infants were assessed for eligibility. Of the 374 not included 274 did not meet the inclusion criteria mainly due to short admission periods, (less than five days in the NICU and three days in the maternity ward) and 18 because of either severe illness of the infant or the mother. Moreover, 81 were not randomised due to busyness at the wards, and, finally did lack of space in the NICU not allow two families to be randomised ().
Of the 97 infants included, 55 were randomised to the recliner and 42 to the hospital bed (). A total of 73 infants were included in the analysis at Q1 and 45 at Q2. The characteristics of the infants and their parents are shown in .
Thirty-nine of 42 (93%) staff members at the NICU (33 nurses, two social assistants, and four neonatologists) and 14 of 19 (74%) staff members at the maternity ward (12 nurses and two midwives) answered the questionnaire related to their working-environment. Of these staff members six (11%) had a lot of experience and 39 (74%) had little or some experience with the recliner. As for the hospital bed 40 (75%) had a lot of experience, and 11 (21%) had little or some experience.
Parents’ experience
Parents in the recliner group had a significantly lower discomfort-score at Q1 compared to parents in the hospital bed group (3.94 vs. 5.48, p = 0.02) (); when analysed by gender, this difference was statistically significant only for the mothers (4.16 vs 6.15, p = 0.01) and not for the fathers (3.20 vs 2.80, p = 0.08). Both mothers having given birth vaginally and by caesarean section rated the discomfort-score at Q1 lowest for the recliner (vaginal: 4.29 vs 6.00, p = 0.06 and caesarean: 3.00 vs 5.75, p = 0.07), although not statistically significant (data not shown). The lower discomfort in the recliner group was commented by a mother who had used the possibility of changing the position of the recliner because ‘The same position causes pain in my backsides, because the sitting comfort is not so good in the long run’. Another mother commented the stand-up lift function as it minimised her pain after giving birth by caesarean section ‘Love the stand-up lift function that helps me sit down after surgery’.
Table 2. The parents’ scores on comfort/discomfort of the recliner and the hospital bed at Q1 and Q2.
No significant differences were found in discomfort-scores at Q2 neither overall nor when analysed by gender or birth method (data not shown).
A tendency for lower comfort-scores at Q1 and a tendency for higher scores at Q2 were found for the recliner group as compared to the hospital bed group (). The same tendencies were also found when sub-analyzing by gender and by birth method (data not shown). Parents were divided into two sub-groups according to height (<166 cm and ≥166 cm), and no significant differences were found between these sub-groups neither in the recliner group nor in the hospital bed group (data not shown). However, two mothers of low height made the following comments:
The backrest seems too long for me, and the headrest is difficult to use, since it does not support the neck’ and ‘I am not that tall and could not get far enough back in the seat to get lumbar support.
Significantly higher comfort-, and discomfort-scores were found at Q1 than at Q2 in both study groups () (p < 0.02 for all comparisons).
Both at Q1 and Q2, more parents stated that the recliner supported their arms better than the hospital bed both while tube feeding (16/25 vs. 1/18, p = 0.01 and 10/19 vs 1/15, p = 0.01), breast-feeding (18/29 vs 0/14, p = 0.01, 9/17 vs 1/10, p = 0.04), and bottle feeding (8/11 vs 0/5, p = 0.03 and 2/7 vs 0/8, p = 0.2), though the difference at Q2 for bottle feeding was not statistically significant. The recliner ensured parents’ self-reliance significantly more often as compared to the hospital bed at Q1 (29/34 vs 9/20, p = 0.01), though, the difference was not statistically significant at Q2 (16/21 s 4/10, p = 0.11).
Mothers mentioned a situation that had given them a feeling of confidence and self-reliance as,
‘I think it’s great that you can adjust the chair to a forward sloping position. Therefore, when you express milk, you do not need to sit bend forward for the milk to run down. In the chair, you can sit with your back straight and then adjust it into the right inclination. I avoided getting back pain’. Another mother commented; ‘Nice to be able to adjust the back and footstool to rest position when I breastfeed’.
No differences were found between the recliner and the hospital bed when the parents were asked whether they found it easy to adjust and whether they felt secure while being seated skin-to-skin with their infants. (data not shown).
Experience of the physical working-environment
Twenty-six of the 53 (49%) interdisciplinary staff had had pain and discomfort in the neck, shoulder, and/or lower back in the past six months and of these 12 (23%) reported the pain to have lasted for at least one month.
Out of the 53 staff members, significantly more indicated that they only rarely had to twist their back (22/45 (49%) vs. 12/51 (24%), p = 0.01) or rarely had to bend their back heavily (24/45 (53%) vs. 14/51 (27%), p = 0.01) when working with the recliner as compared to working with the hospital bed.
In addition, though the difference was not statistically significant, the staff answered ‘rarely’ more often to the question ‘My neck is heavily bent over’, (17/45 (38%) vs 28/51 (55%), p = 0.09) and indicated more frequently that they often had a good working position (33/45 (73%) vs. 28/51 (55%), p = 0.06) when working with the recliner as compared to the hospital bed.
For the three questions on functionality (‘It is easy to adjust to a satisfactory working height’, ‘I adjust the working height for the specific task’, and ‘I adjust the working height when talking with the parent’), no differences between the recliner and the hospital bed were found (data not shown). Different explanations were given for not adjusting the recliner; time-consuming, not necessary, not prioritised, and lack of experience. Illustrated with the following comments:
If the time is scarce or the assistance/the conversation is brief, it is not a priority to adjust the recliner.
However, I think I can be content with the recliner’s many features when I get a little more experience.
Discussion
At neonatal wards, it is important to offer parents the best conditions when they handle and care for their premature and/or sick newborn infants, including optimising the possibility to have skin-to-skin contact with the infant, for its many benefits (Kostandy and Ludington-Hoe Citation2019; Ionio, Ciuffo, and Landoni Citation2021). Parents and infants often need assistance and care when sitting skin-to-skin. Therefore, their position and the possibilities for adjustments significantly affect the work environment of neonatal nurses and other health professionals (Schlossmacher and Amaral Citation2012). Given the high frequency of musculoskeletal complaints from nurses, any changes and improvements for the infants and the parents should also consider how to ensure the best working postures for the staff.
Not being able to identify a chair that meets all the requirements of the parents and staff, the NICU participated in the development of an improved recliner involving all stakeholders. This recliner was used in the present study to compare its comfort functionality, self-reliance and its impact on the working-environment with that of a hospital bed.
In the first questionnaire after admission, the parents in the recliner group had a lower discomfort-score than parents in the hospital bed group, following both caesarean section and vaginal delivery. This lower discomfort may be due to the functionality of the rest-chair, e.g. the stand-up lift function, and the parents’ experience of higher self-reliance since they could easily change the position by themselves. This might also explain that the difference had almost disappeared in the follow-up questionnaire, when the mothers were less troubled by the consequences of having given birth.
It was expected that the parents would get accustomed to the features of the recliner and the hospital bed after some days and that this would increase the comfort score; however, the comfort-scores decreased from the first questionnaire to the day of follow-up. An explanation could be that mothers often received pain medication during the first few days after giving birth. When pain medication was discontinued, they might have experienced the signals of their body more intensely (Lilliesköld et al. Citation2022).
Fathers are very concerned about both their newborn infants and the infants’ mothers when admitted to an NICU, a fact that could affect the awareness of their own comfort/discomfort initially (Lilliesköld et al. Citation2022; Fegran, Helseth, and Fagermoen Citation2008). As the situation around their family gets more stable, they might allow themselves to feel their body and to be aware of their own well-being.
Corroborating the results of other studies, (Adhikari and Dhakal Citation2014; Schlossmacher and Amaral Citation2012) this study found that the staff members often had musculoskeletal-related symptoms, resulting in pain and discomfort. It could be expected that these complaints would decrease when using the new recliner, as the staff rated their working positions as being less cumbersome.
Despite the positive evaluations of the recliner, both parents and staff members suggested improvements: the seat should be softer, the headrest should be easier to adjust, the ear-flaps should be padded, and the back should be more reclinable for sleeping or for a reclined position while breastfeeding.
Using the hospital-bed, approximately 75% of the staff, most of these nurses, reported that they often had to twist or heavily bend their back as compared to 50% when using the recliner. The suggested improvements and becoming more familiar and experienced with the recliner hopefully will help to reduce the high proportion health issues among staff experiencing unsatisfactory working positions.
Strengths and limitations
A strength of this study was that the new recliner was developed within a participatory design where parents and staff co-operated with the company and designers. Likewise, the recliner was compared to the hospital bed in real-life clinical practice by both staff and parents. The study design was strengthened by randomisation of the infants, so that the nurses could not choose whether a specific family should be offered the recliner or the traditional hospital bed. The variations in participants’ characteristics strengthened the results. Participants were both mothers and fathers, with different heights, as well as mothers who had given birth vaginally or by caesarean section. Although nurses comprised the majority of the staff participant group, a strength of the study was that we included interdisciplinary staff members.
However, this study had some limitations. The sample size was small and more participants in the recliner arm answered the questionnaire, which could weaken the results. The newly developed recliner might have motivated the parents to answer the questionnaire more often compared to those who were testing the well-known hospital bed. Furthermore, the fact that 18 of the participants in the maternity ward were randomised to the recliner compared to only four randomised to the hospital bed could have biased the results. The main limitation was the low response rate by the parents. This is probably due to the parents being concerned about their newborn infant and therefore not having focussed on the questionnaires for the study.
Sub analyses by gender and birth methods were carried out despite the small sample size as both parents are important caregivers (Fisher et al. Citation2018) and because mothers who have given birth vaginally and by caesarean section have different problems when sitting skin-to-skin with their children.
As the length of the test period for the parents was short, they might not have had enough time to become familiar with the functionalities of the recliner. Instead, a pair-wise comparison of both the recliner and the hospital bed could have strengthen the result, but due to the relative short admission periods, it was not feasible to have such a pair-wise comparison.
However, the short period was acceptable, as a previous study found that comfort and discomfort were immediately noticed and did not change over time, which means that a person testing a chair is able to evaluate it, straightaway (Helander Citation2003). Nevertheless, by extending the test period, staff members could have gained more experience with the recliner. A larger sample would have enabled us to explore the results of the parents with greater statistical precision. Furthermore, many infants were unable to breastfeed because of their health status, which meant that only a few evaluations about breastfeeding were obtained.
Conclusion
Using a recliner created in a participatory design process involving parents and staff members, the study showed that the recliner diminished the discomfort of the parents after birth of the infant and slightly increased the comfort on follow-up. Furthermore, the nurses and other interdisciplinary staff members evaluated their work-environment as being better, when a parent was sitting skin-to-skin with the infant in the recliner as compared to being in the hospital bed.
Implication for future research and practice. The participating staff members and parents made several suggestions for improvements of the recliner to achieve even better care of infants and parents and to obtain better working-environments for the nurses and other staff members. The willingness of parents, neonatal nurses, and other health professionals to give inputs for improvements and the creativity and enthusiasm shown, would make an ongoing development and improvement process involving all stakeholders from the initial process useful and exciting to organise. Furthermore, the experience of using participatory design processes can potentially be useful in other areas, too, not only for future research concerning skin-to-skin contact, parent comfort, and health care professionals’ working-environment
Relevance to clinical practice
In many countries, parents do not have the possibility to room-in with their infants when they are admitted to an NICU, and lack of space is often a problem.
To our knowledge, this study is the first that uses a participatory design involving parents and interdisciplinary staff members in developing a recliner that meet the physical needs of parents when sitting skin-to-skin with their infants.
While developing the recliner, all relevant stakeholders ensured that high priority be given to ensure good working postures in health care professionals in order to prevent having low back injury and pain at work.
Clinical trial registration
Given the nature of the study reporting on the process of designing and testing a recliner, the study was not found appropriate for registration at a register as e.g. Clinical Trails.
Acknowledgments
Thanks to parents, staff, and managers for taking part in this study. We are grateful for the support received by The Market Development Fund, Denmark.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Adhikari, S., and G. Dhakal. 2014. “Prevalent Causes of Low Back Pain and Its Impact among Nurses Working in Sahid Gangalal National Heart Centre.” Journal of Nepal Health Research Council 12 (28): 167–171.
- Aiken, Linda H., Walter Sermeus, Koen Van den Heede, Douglas M. Sloane, Reinhard Busse, Martin McKee, Luk Bruyneel, Anne Marie Rafferty, Peter Griffiths, Maria Teresa Moreno-Casbas, Carol Tishelman, Anne Scott, Tomasz Brzostek, Juha Kinnunen, Rene Schwendimann, Maud Heinen, Dimitris Zikos, Ingeborg Strømseng Sjetne, Herbert L. Smith, and Ann Kutney-Lee. 2012. “Patient Safety, Satisfaction, and Quality of Hospital Care: Cross Sectional Surveys of Nurses and Patients in 12 Countries in Europe and the United States.” BMJ (Clinical Research Ed.) 344: e1717. doi:10.1136/bmj.e1717.
- Albertsen, K.W.I.-M., J. Jessen, and C. Nielsen. 2015. “Kvalitet af sygeplejen og arbejdsmiljø i sundhedssektoren Dokumentationsrapport nr 2.” https://dsr.dk/sites/default/files/24/dsr_dokumentationsrapport_2015_0.pdf
- Amaliyah, E., and S. Tukimin. 2021. “The Relationship between Working Environment and Quality of Nursing Care: An Integrative Literature Review.” British Journal of Healthcare Management 27 (7): 194–200. doi:10.12968/bjhc.2020.0043.
- Benoit, B., M. Campbell-Yeo, C. Johnston, M. Latimer, K. Caddell, and T. Orr. 2016. “Staff Nurse Utilization of Kangaroo Care as an Intervention for Procedural Pain in Preterm Infants.” Advances in Neonatal Care 16 (3): 229–238. doi:10.1097/ANC.0000000000000262.
- Blomqvist, Y.T., L. Frolund, C. Rubertsson, and K.H. Nyqvist. 2013. “Provision of Kangaroo Mother Care: supportive Factors and Barriers Perceived by Parents.” Scandinavian journal of Caring Sciences 27 (2): 345–353. doi:10.1111/j.1471-6712.2012.01040.x.
- Det nationale forskningscenter for arbejdsmiljø. 1994. "PRIM reseach." https://nfa.dk/
- Fegran, L., S. Helseth, and M. Fagermoen. 2008. “A Comparison of Mothers’ and Fathers’ Experiences of the Attachment Process in a Neonatal Intensive Care Unit.” Journal of Clinical Nursing 17 (6): 810–816. doi:10.1111/j.1365-2702.2007.02125.x.
- Fisher, D., M. Khashu, E.A. Adama, N. Feeley, C.F. Garfield, J. Ireland, F. Koliouli, B. Lindberg, B. Nørgaard, L. Provenzi, F. Thomson-Salo, and E. Teijlingenl. 2018. “Fathers in Neonatal Units: Improving Infant Health by Supporting the Baby-Father Bond and Mother-Father Coparenting.” Journal of Neonatal Nursing 24 (6): 306–312. doi:10.1016/j.jnn.2018.08.007.
- Helander, M. 2003. “Forget about Ergonomics in Chair Design? Focus on Aesthetics and Comfort!.” Ergonomics 46 (13–14): 1306–1319. doi:10.1080/00140130310001610847.
- Helander, M.G., and L. Zhang. 1997. “Field studies of Comfort and Discomfort in Sitting.” Ergonomics 40 (9): 895–915. doi:10.1080/001401397187739.
- Huisman, E.R.C.M., E. Morales, J. van Hoof, and H.S.M. Kort. 2012. “Healing environment: A Review of the Impact of Physical Environmental Factors on Users.” Building and Environment 58: 70–80. doi:10.1016/j.buildenv.2012.06.016.
- Ionio, C., G. Ciuffo, and M. Landoni. 2021. “Parent-Infant Skin-to-Skin Contact and Stress Regulation: A Systematic Review of the Literature.” International Journal of Environmental Research and Public Health. 18 (9): 4695.
- Jesney, S. 2016. “A Critical Analysis of the Role of the Nurse in the Implementation of Skin-to-Skin on the Neonatal Unit.” Journal of Neonatal Nursing 22 (2): 68–73. doi:10.1016/j.jnn.2015.04.008.
- Johnston, C., M. Campbell‐Yeo, T. Disher, B. Benoit, A. Fernandes, D. Streiner., et al. 2017. “Skin‐to‐Skin Care for Procedural Pain in Neonates.” Cochrane Database of Systematic Reviews 2017 (2): CD008435. doi:10.1002/14651858.CD008435.pub3.
- Kostandy, R.R., and S.M. Ludington-Hoe. 2019. “The Evolution of the Science of Kangaroo (Mother) Care (Skin-to-Skin Contact).” Birth Defects Research 111 (15): 1032–1043. doi:10.1002/bdr2.1565.
- Lewis, Todd P., Kathryn G. Andrews, Elyse Shenberger, Theresa S. Betancourt, Günther Fink, Sunita Pereira, and Margaret McConnell. 2019. “Caregiving can Be Costly: A Qualitative Study of Barriers and Facilitators to Conducting Kangaroo Mother Care in a US Tertiary Hospital Neonatal Intensive Care Unit.” BMC Pregnancy and Childbirth 19 (1): 227. doi:10.1186/s12884-019-2363-y.
- Lilliesköld, S., S. Zwedberg, A. Linnér, and W. Jonas. 2022. “Parents’ Experiences of Immediate Skin-to-Skin Contact After the Birth of Their Very Preterm Neonates.” Journal of Obstetric, Gynecologic, and Neonatal Nursing 51 (1): 53–64. doi:10.1016/j.jogn.2021.10.002.
- Schlossmacher, R., and F.G. Amaral. 2012. “Low Back Injuries Related to Nursing Professionals Working Conditions: A Systematic Review.” Work 41 (Suppl 1): 5737–5738. doi:10.3233/WOR-2012-0935-5737.
- Seidman, Gabriel, Shalini Unnikrishnan, Emma Kenny, Scott Myslinski, Sarah Cairns-Smith, Brian Mulligan, and Cyril Engmann. 2015. “Barriers and Enablers of Kangaroo Mother Care Practice: A Systematic Review.” PLoS One 10 (5): e0125643. doi:10.1371/journal.pone.0125643.
- Sørensen, K.L. 2017. "NOTAT Sygeplejerskers fysiske arbejdsmiljø.” https://dsr.dk/sites/default/files/24/notat_sygeplejerskers_fysiske_arbejdsmiljoe_2017.pdf
- Vela, M. 2022. "Rest-chair for Neonatal Unit.” https://vela-medicalcom/chair/vela-neonatal-chair/. Accessed 23 February 2022.
- WHO. 2022. “Kangaroo Mother Care.” Accessed 26 September 2022. https://wwwwhoint/news/item/26-05-2021-kangaroo-mother-care-started-immediately-after-birth-critical-for-saving-lives-new-research-shows.
- Zhang, L., M.G. Helander, and C.G. Drury. 1996. “Identifying Factors of Comfort and Discomfort in Sitting.” Human Factors 38 (3): 377–389. doi:10.1518/001872096778701962.
