Abstract
As the global population ages there is an imperative to enhance labour participation of older workers in ways that support good physical and psychological health. However, there is limited guidance for organisations on how to do this effectively. This systematic review examined literature identified through four databases and a targeted web-search, yielding 39 PRISMA records (32 scholarly, seven grey literature) reporting workplace interventions aimed at improving the injury outcomes of older workers. The review revealed that organisational and composite interventions may be most effective, although an absence of robust research in this area and a scarcity of empirical evidence-based interventions known to improve injury outcomes for older workers was noted. Responding to these shortcomings, this article presents ‘A future research agenda for older worker health, safety and well-being interventions.’ This systems-based approach has a dual focus on organisational and composite interventions combined with robust research design.
Practitioner summary: We conducted a systematic literature review of studies focussed on workplace interventions to improve the physical and psychological safety of older workers. Within the existing literature, evidence for effective interventions and guidance for organisations is weak. We present a future research agenda with a systems approach to address these gaps.
1. Introduction
Globally, the population is ageing (World Health Organisation 2015), with considerable impacts on labour supplies, financial sustainability of pension schemes, health systems and organisations (Avendano and Cylus Citation2019; Stynen, Jansen, and Kant Citation2017). Improved working conditions and technological advances, coupled with increases in the retirement or superannuation age, have led to many workers remaining longer in the workforce (Beers and Butler, Citation2012; Delloiacono Citation2015, Horton et al. Citation2018; Leime and Ogg Citation2019; Poscia et al. Citation2016). This change to workforce demographics has necessitated governments and businesses to focus resources towards creating physically and psychologically safe work environments for older workers. While many jurisdictions have stated goals to enhance the labour participation of older workers (Stynen, Jansen, and Kant Citation2017), there is a paucity of research evidence to guide the interventions needed to meet these goals.
The goals of ergonomics and human factors (E/HF) are to improve both human performance and well-being through effective integration of the physical, organisational and social sub-systems by designing environments to fit the people that use them (Dul et al. Citation2012). Considering the needs and capabilities of people is central to this, including the changes in capabilities and preferences that occur as people age (Elton and Nicolle Citation2015). Yet, workforce ageing has been the focus of only limited E/HF attention (e.g. Bentley et al. Citation2021; Costa and Sartori Citation2007; Dul et al. Citation2012; Kumashiro Citation2000). Aligned with an E/HF approach, this systematic literature review sought to examine interventions reported within the scholarly and grey literature that aimed to reduce the risk of physical and psychological injury amongst older workers through changes to the organisation of work, work design, and the work environment. The review also captured individual-level interventions that focussed on the worker as these often included a work design or organisational component.
1.1. Defining older workers
Defining a chronological age range for older workers is problematic as it assumes that chronology is a valid proxy for behaviour when, in practical terms, it may be only loosely associated with function (World Health Organisation 2015). There is no accepted definition in Australia of the age at which someone is classified as an ‘older worker’, although health begins to decline at age 55, according to the Queensland Government’s Office of Industrial Relations (2019). Generally, older worker studies include people 45 years-of-age and older and a focus range of age is often defined for the purposes of specific reports. For example, a 1993 WHO (World Health Organisation 1993) report defined an older worker as over 45 years-of-age, while a UK based study specified 50 and over (National Institute of Economic and Social Research Citation2017). The studies included in this review adopted various definitions for an older worker, although these typically fell within the 40–65 years-of-age range.
1.2. Work-related musculoskeletal disorders, psychological injuries and older workers
While a growing body of research has focussed on identifying and assessing the extent and nature of health and safety risks to older workers (Delloiacono Citation2015), the literature does not deal specifically with interventions to prevent and manage work-related musculoskeletal disorders (WMSD) and psychological injury. These conditions have complex aetiologies arising from exposure to physical and psychosocial hazards in the workplace (Caponecchia et al. Citation2020; Robertson, Jayne, and Oakman Citation2021). International research indicates older workers experience a high prevalence of WMSD (Delloiacono Citation2015; Tugman Citation2013), carry a high-cost burden and contribute to early retirement (Oakman, Clune, and Stuckey Citation2019). The role of psychological stress in the development of WMSD is widely acknowledged (for example, Gerr et al. Citation2014; Lang et al. Citation2012; Macdonald and Evans Citation2006). For older workers, psychological injury exacerbated by the impact of WMSD may lead to functional decline, loss of employment and early retirement (Oakman, Clune, and Stuckey Citation2019).
The extant literature highlights the fact that psychosocial risks, such as high demands, role conflict, lack of managerial or co-worker support, stress, bullying and discrimination in the work environment, are detrimental to both health and well-being of older workers and can also increase the probability of early retirement (Beehr et al. Citation2000; Bentley et al. Citation2019; Bibby Citation2008; Chiu et al. Citation2001; Nilsson Citation2016). Indeed, studies indicate that where the work is intrinsically stressful, such as for police officers (Gershon, Lin, and Li Citation2002) and nurses (Santos et al. Citation2003), older workers are more likely to have significant mental health problems. In line with this research, Nilsson (Citation2016) found that a poor work environment and associated stress and mental disorders were associated with early retirement amongst older workers, especially in highly demanding work environments (Johnston and Lee Citation2009). Research also indicates that older workers may need more rest and recovery time between periods of work, are less able to sustain long work hours and high work-pace (Nilsson Citation2016) and may be negatively impacted by shift work (Blok and de Looze Citation2011). However, other research evidence suggests that older workers may be more resilient to some work demands, including work-family conflict and stress (Mauno, Ruokolainen, and Kinnunen Citation2013), as well as exposure to workplace bullying (Personal Communication).
1.3. Interventions for older worker physical and psychological injury
As people work into older age, work tasks, systems, and equipment need to adapt in order to continue to reduce risk, prevent injury and enhance well-being (EU-OSHA 2016). Strategies used to deal with the challenge of ageing workforces often focus on individuals rather than taking a systems approach (Robertson, Jayne, and Oakman Citation2021). For example, exercise programs for older workers focus on improving individual capacity rather than considering the design of work systems and tasks to fit the capabilities and needs of older workers. However, the literature offers growing empirical evidence for the role of organisations in supporting the health and well-being of older workers through design and management systems initiatives tailored specifically for this population. These include mature-age job design and management practices such as recognition, support and flexible work opportunities which have been found to increase older workers’ well-being and satisfaction with work (Bentley et al. Citation2017; Kooij et al. Citation2010; Raab Citation2020; Teo et al. Citation2022). Vanajan, Bültmann, and Henkens (Citation2020) found perceived access to flexible working hours and a psychologically safe work climate to be associated with improvements in workability amongst older workers with chronic health conditions. Moreover, the improved well-being of older workers associated with mature-age management practices were explained by inclusive leadership and feelings of being recognised and valued (Teo et al. Citation2022), while Bentley et al. (Citation2017) found perceptions of changes in job design and positive work environment promoted well-being and positive engagement. These studies indicate that it is the design and organisation of work and work environments, rather than the age-related factors per se, that are the more important influences on older workers’ well-being (Guglielmi et al. Citation2016; Raab Citation2020; Thorsen, Jensen, and Bjørner Citation2016).
This review aimed to identify, from the scholarly and grey literature, interventions used to address older worker health, safety and well-being and examine the evidence of their effectiveness (Bentley et al. Citation2022). This paper provides a summary of those results, reflecting the current knowledge and research in this area. Drawing on this, we present an E/HF research agenda for older worker health, safety and well-being.
2. Method
2.1. Scholarly literature search strategy
Search strategies were developed for the scholarly literature by the research team in consultation with a university librarian. The search terms for the scholarly literature are shown in and were applied to the CINAHL, PsychINFO, ProQuest Business and Scopus databases. These databases were selected as the most appropriate in terms of coverage of the relevant content (allied health, psychology, business and citation databases) and with the maximum coverage of listed peer reviewed articles. Limits placed on the search included: English language; published from 2000; journal articles, literature reviews, or conference proceedings. Limiting the search to articles published from the year 2000 was agreed in the co-design process for the study with the project funder as being broadly consistent with the start of a growth in research interest in the field while still capturing relatively contemporary approaches to prevention, including technological interventions. The search was conducted in July 2021.
Table 1. Search terms for the scholarly databases.
2.1.1. Exclusion and inclusion criteria
At screening, included articles needed to have a focus on work, older workers currently participating in work, and include interventions for older workers. Reasons for exclusion included domains other than work (e.g. medical treatment for clinical populations); matters other than interventions (e.g. experimental work); returning older people to the workforce (e.g. retirees, the unemployed); finding new work opportunities for older people so that they can participate in employment; removing discrimination or stigma around hiring older people; and theoretical contributions that did not implement or evaluate interventions.
2.1.2. Screening protocol
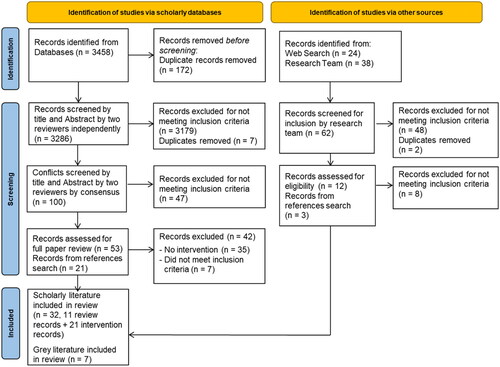
Using the PRISMA protocol for systematic literature reviews (Page et al., Citation2021), the search initially identified 3458 records for review (). After the removal of 172 duplicates, the resultant records were entered into Covidence software to facilitate the screening and selection process. The PRISMA 2020 Checklist was used to guide the review (Page et al. Citation2021) and while the risk of bias cannot be eliminated, the researchers (co-authors to this paper) developed protocols to minimise the risk and improve consistency. The protocols were tested by two project researchers before being agreed on by the remainder of the research team. Next, the researchers independently screened the title and abstract of the records, two researchers for each record, to determine relevance for the scope and focus of the review based on the inclusion criteria. In cases where the two co-authors did not agree on whether to include the article, the screening was marked as a conflict and a third researcher reviewed the conflicts to resolve them by consensus. Fifty-three papers were included for a full paper review and an additional 21 records were identified from the references examined and subjected to the same full paper screening process. The full paper reviews were conducted by four members of the research team who assessed each paper for inclusion in the study. Forty-two papers were subsequently excluded; 35 did not include interventions and seven did not meet other inclusion criteria. This resulted in a total 32 scholarly records being included in the review. Eleven were reviews and 21 were intervention records.
Figure 1. PRISMA flowchart of the literature search.
2.2. Grey literature
The grey literature was identified by searching websites of key organisations, government bodies and enterprises with potential interest in workplace health and safety, older workers, and well-being at work. Documents containing information on evidence-based interventions or strategies designed for older workers were included. The grey literature website search identified 24 documents, together with a further 38 that were provided by the co-authors for a total of 62 documents. Each document was allocated to a member of the research team to determine whether the document met the inclusion criteria. Fifty documents were removed (two were duplicates and 48 did not meet the inclusion criteria) and three records were added through examining the references of the scholarly records. The remaining 15 documents were read in-depth by co-authors (AV, VH, LO) and eight excluded for not focussing on older workers or being informative for workplace interventions. A total of seven records from the grey literature were included in the review ().
2.3. Data extraction and synthesis
The resultant records were considered separately as review articles, intervention articles and grey records, as they can describe heterogenous information, for example multiple interventions across a range of industries. The information extracted from records during full-text analysis is shown in .
Table 2. Data extracted from the full-text reviews.
2.4. Ethical statement
Not applicable.
3. Results
3.1. Full-text review
A total of 39 articles (11 review articles, 21 intervention papers and 7 grey literature documents) from the scholarly literature and grey literature met the review criteria and were included in the full-text review. Generally, the number, scope and quality of the studies reviewed were limited, suggesting a significant gap in knowledge related to which interventions are most effective in tackling older worker injuries. Grouped by document type, the details of the retained papers are discussed next.
3.2. Review articles
shows a summary of the type of review articles, their focus and the interventions examined (more detail is included in Supplementary Appendix 1).
Table 3. Review article summary.
3.2.1. Study characteristics
Where stated, the age-range addressed within the review papers was between 40-65 years or had a focus across all working age ranges but included specific content on older workers (e.g. Pieper, Schröer, and Eilerts Citation2019). The reviews concerned older workers generally, rather than focussing on specific industries, though Nilsson (Citation2016) focussed on agriculture and Denton, Evans, and Xu (Citation2021) on nursing and midwifery. The reviews explored a range of older worker outcomes, extending beyond worker health, safety and well-being, to include related issues of workability, performance and retention. None focussed specifically on WMSD or psychological injury, although several papers included studies focussed on either WMSD or employee well-being or work stress (e.g. Roper and Yeh Citation2007; Pieper, Schröer, and Eilerts Citation2019).
3.2.2. Intervention foci
The review papers mostly included multiple interventions for older worker health, safety, well-being and workability. Some addressed specific intervention categories such as workplace physical activity interventions (Merom et al. Citation2021) and workplace health promotion campaigns (Nilsson Citation2016). The foci of the remaining review papers were across a wide range of interventions including those related to physical aspects (e.g. design and equipment, engineering improvements, safety equipment); individual approaches (e.g. stress management, exercise, education programs); and organisational improvements (e.g. work environment, administrative changes).
3.2.3. Intervention effectiveness
Positive findings on intervention effectiveness were reported for multi-component interventions (Pieper, Schröer, and Eilerts Citation2019), and integrated approaches as systematic solutions for complex problems (Cooklin et al. Citation2017). These studies typically included both organisational and individual-level interventions, for example a combination of exercise, education and equipment in reducing musculoskeletal pain (Pieper, Schröer, and Eilerts Citation2019). Evidence for the effectiveness of single component interventions for enhancing older worker health, safety, well-being or workability was mixed. Job stress management training and workstation adjustments as single approaches were found to have no effect on WMSD outcomes (Pieper, Schröer, and Eilerts Citation2019), while another review reported moderate effects of stress management training on stress reduction, although there was no evidence for the sustainability of this approach (Pieper, Schröer, and Eilerts Citation2019). Workplace health promotion programs failed to improve the workability, productivity or job retention of older workers (Poscia et al. Citation2016). There was limited evidence that individual-level interventions such as health promotion, exercise, web-based programs and training have positive outcomes for older workers (Merom et al. Citation2021; Poscia et al. Citation2016), although almost all the reviews reported methodological weaknesses that limited the value of the research studies. There was some evidence of effectiveness for multi-component interventions including a mix of organisational and individual-level interventions) (Pieper, Schröer, and Eilerts Citation2019).
3.3. Intervention articles
A summary of the interventions examined in the full-text review and the main findings of each of the 21 intervention articles is included in Supplementary Appendix 2.
3.3.1. Outcome measures
A wide range of subjective and objective outcome measures related to aspects of older worker health, safety, well-being and workability were used in the articles. Some specifically targeted improvements in WMSD, including aspects of posture or workstation improvement, or work stress/mental health outcomes. However, many records assessed other specific health, e.g. balance (Granacher et al. Citation2011), diet (Cook et al. Citation2015), or general health outcomes such as workability (De Boer et al. Citation2004) or absenteeism (Hesselink, de Leede, and Goudswaard Citation2010). Other studies targeted improvements to aspects of work design that would be expected to result in a reduction in exposure to WMSD and psychosocial risk factors (e.g. Weichel et al. Citation2010; Härmä et al. Citation2006).
3.3.2. Study design and intervention types
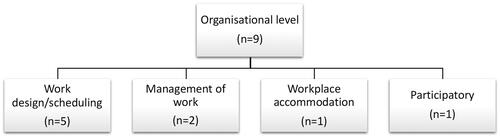
Approximately one-half (n = 11) of the records reported using randomised-controlled trial (RCT) or case-controlled evaluation designs. Two studies appear to have used no control group. The interventions can be broadly divided into individual-level interventions (n = 9; ) and organisational level interventions (n = 9; ). Three records included both individual and organisational interventions, which we have termed ‘composite’ interventions.
Figure 2. Individual-level interventions reported in the older worker literature.
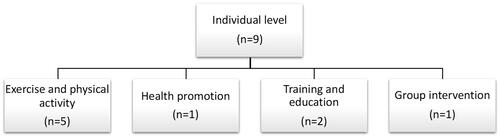
Figure 3. Organisational-level interventions reported in the older worker literature.
Individual-level interventions most frequently included physical activity, reported in conjunction with training interventions in two cases. There was some overlap between some of the intervention records involving exercise, diet, health promotion and training.
Organisational-level interventions () included the design/scheduling and management of work and workplace accommodation. As such, they were designed to reduce exposure to the risk factors associated with injury and health risks to older workers, rather than acting on the individual to increase fitness to avoid injury, resilience to injury or aid coping.
3.3.3. Intervention effectiveness
3.3.3.1. Physical activity and exercise
The most applied intervention category was physical activity and exercise. Evidence of effectiveness was mixed, and relatively inconclusive as different components were more or less effective, and studies did not provide longer-term evaluations. One study included a mix of yoga, workout sessions, aerobic exercise, and free fruit (Strijk et al. Citation2012), and although the program had some positive effects on sports participation and fruit intake, it did not show benefits for aerobic capacity or mental health. Another RCT involved a Tai Chi wellness program (Palumbo et al. Citation2012), showing work stress reduction and some non-significant improvements in general and mental health for the Tai Chi group. An RCT of a web-based health promotion (Cook et al. Citation2015) showed some improvements in dietary and exercise practices of older workers after three months, particularly for women. Cirla et al. (Citation2005) utilised a training intervention of six simple exercises during work time for older sedentary office workers. Musculoskeletal complaints were improved for 21 of the 56 workers participating in the trial, although the strength and duration of effectiveness was unclear.
3.3.3.2. Training
The evidence for effectiveness of training interventions on older worker health-related outcomes was also mixed, with inconsistencies in study design making determining the adequacy of specific solutions to address older worker injury problematic. Taieb-Maimon et al. (Citation2012) compared an office training group (personal ergonomics training and workstation adjustments), a photo-training group (office training and self-modelling photos of participants’ postures), and a control group. Both training methods resulted in posture improvement during the first 12 days of the intervention, but sustained improvement (at six weeks) was seen only with the photo-training method. The intervention had greatest benefit to older workers, females, and those suffering most musculoskeletal pain. Another study examined the effectiveness of an ergonomics and health training program (including physical exercise, skills training and self-experience) on work interest, workability (i.e. ability to work) and health in older urban transport drivers (Karazman et al. Citation2000). The findings of the study suggested improvements in workability and health and positive trends for ergonomics and relationships at work.
3.3.3.3. Work scheduling
Papers reporting interventions that focussed on aspects of work and shift scheduling (n = 3) targeted a range of health and well-being outcomes. All found particularly strong positive effects for older workers on the outcomes targeted. The interventions focussed on altering the shift rotations with a view to improve health and absenteeism rates. Härmä et al. (Citation2006) examined the impact of changes to a rapid, forward-rotating shift system on sleep duration of younger (<45 years) and older (45+ years) shift workers. The authors found older workers were positively affected, with improvements in sleep, well-being and alertness following night shift. A case-controlled study by Hesselink, de Leede, and Goudswaard (Citation2010) examined a number of roster changes on health, injury and absence of all workers in a steel production site. Changes included more days off after night shifts, backward to forward rotating and slow to fast rotating shifts. Older workers particularly benefitted from these new arrangements, including improvement in fatigue and musculoskeletal problems. A study by Piszczek and Pimputkar (Citation2021) found flexible schedules to benefit older workers in terms of sick days and health perceptions.
3.3.3.4. Work design
Aspects of work design have been considered in the classifications that reflect the study’s key focus (e.g. work scheduling) while other studies included work design as part of composite interventions. May et al. (Citation2004), in a quasi-experimental longitudinal field study, examined the impact of workstation ergonomics design improvements on municipal workers’ perceptions of workstation qualities, musculoskeletal complaints, and satisfaction. Findings suggested the experimental groups had superior outcomes to those of controls, although this effect was weaker for older workers. A study by Weichel et al. (Citation2010) examined the impact of task rotation on health and performance outcomes of equipment manufacture workers in the automobile industry. While older workers rotated tasks less, and therefore had less variety in their work, greater rotation was associated with lower absenteeism and improvements to health. However, the study sample size was small, did not incorporate a control group and there were few older workers in the workplace.
3.3.3.5. Management of work
The two management of work/worker reviews (Skoglund and SkoglundCitation2005; Morelock, McNamara, and James Citation2017) used training and other means to develop the capabilities and skills of managers to manage older workers and maintain a safe and healthy work environment. As managers can strongly influence the work experience of older workers this approach would seem to have merit, though only one of the studies found a beneficial effect. Skoglund and Skoglund (Citation2005), implemented a one-year training program for managers of municipal workers. The interventions were detailed, involving a mix of policy reviews, interviews, seminars, support and mentorship. The program was evaluated using a quasi-experimental design, finding that managers’ knowledge about ageing and workability was improved, with skills developed that enabled them to assess the needs of older workers and use the knowledge in practice. Morelock, McNamara, and James (Citation2017) implemented a management of work initiative in the health care sector. The intervention focussed on flexible work options and communication between managers and workers on the best practice for the design and implementation of work arrangements. The intervention had only a low effect size, with improvements most evident for those older workers approaching retirement with low workability.
3.3.3.6. Composite interventions
Avendano and Cylus (Citation2019) suggest that multi-factorial interventions are more likely to address the complexity associated with workplace problems and injury risk though just two composite studies were identified in the review. De Boer et al. (Citation2004), examined the effectiveness of a program that combined discussions with managers about workplace changes to suit older workers and health promotion components. The RCT found that workers in the treatment group were less likely to retire early and took fewer sick days. Furthermore, after six-months, older workers had greater workability and less burnout, although no differences were detected after two-years. In addition, a quasi-experimental study by Andersson-Felé (Citation2005), examined the role of a combined training and workplace change intervention on workload, workplace ergonomics, psychosocial ‘troubles’ and stress. They found an improvement in each of these outcomes, alongside greater reported joy and stimulation from work although no differences were observed in sick days or work duration.
One example of a participatory intervention was identified in the review. Hengel et al. (Citation2011) used an intervention mapping process to design a three-component intervention (workload reduction, rest break tool, empowerment training) for construction workers. The intervention resulted in improvements in satisfaction with workplace design and better insights into older workers, however, no robust effectiveness evaluation was reported in the article. While participatory interventions are suggested as best practice for organisational intervention (e.g. Eurofound and EU-OSHA Citation2014; EU-OSHA Citation2018; Leka, Van Wassenhove, and Jain Citation2015; Nielsen and Christensen Citation2021), these approaches are difficult to evaluate.
3.4. Grey literature documents
The seven pieces of grey literature included in the full-text review comprised guidance material (n = 2), reports (n = 3), conference proceedings (n = 1) and a book chapter (n = 1). The records are relatively old; only one was published post-2010. Supplementary Appendix 3 provides a detailed summary of these records while their foci is described next.
3.4.1. Record foci
A European Union (EU) guide (Crawford et al. Citation2016) highlights the need for good quality working conditions, appropriate work-life balance, employment security, and lifelong learning. These concepts are considered the basis for sustainable work and the guide argues that creating sustainable work requires an understanding of the aged-related issues affecting hazard exposure and workability. The WorkSafe (Citation2010) guidance focusses on control measures and raising awareness about older workers’ health and safety without reviewing interventions. Recommendations for creating a healthy and safe work environment for older workers focus on organisational-level interventions, including aspects of job design, reducing work demands, scheduling of work, flexibility and autonomy, improvements to the physical work environment and reducing postural demands. The strongest guidance evidence is found in Crawford et al. (Citation2009) as it incorporates a systematic review of the health, safety and health promotion needs of older workers. However, the body of work upon which the review drew was limited, of low quality and is now dated. The control measures recommended in the guide include job design to reduce demands and consideration of E/HF principles in shift scheduling. The proceedings from the Healthy Ageing for a Sustainable Workforce conference (AOEC and CSOEH 2009) focussed on construction and healthcare industries and called for research that evaluates the effectiveness of policies, practices, and interventions (e.g. job design, workplace accommodations, training) that are effective in promoting health and safety in older workers. Finally, a Europe-based report (Morschhäuser and Sochert Citation2006) described a stress management and fitness program for older drivers and a shift change intervention for textile workers. While improvements to health, well-being and absenteeism were observed, few details of evaluation were provided.
3.5. Quality considerations
Overall, the quality of the records included in the full-text review was mixed. A number of the review papers reported studies which did not use controls or use robust evaluation designs. Problems with intervention design and evaluation quality also limited the value of several of the intervention studies reviewed. This included a lack of implemented and evaluated interventions (Nilsson Citation2016), inadequate description of interventions implemented thus reducing their reproducibility (Merom et al. Citation2021), low-quality evaluation methodologies (Merom et al. Citation2021), small sample sizes (Poscia et al. Citation2016), and limited implementation and/or evaluation period (Andersson-Felé Citation2005; Poscia et al. Citation2016). The very small number of grey literature records had limited value due to the lack of evidence of the effective strategies and the age of the materials. The lack of process evaluation for most studies also limited the ability of researchers to understand how effective the implementation process was and identify barriers and facilitators of the intervention’s success (Neilsen and Abildgaard, Citation2013). A common theme amongst review papers was the paucity in the body of research on intervention to control risks to older workers, and evaluated interventions in particular (e.g. Crawford et al. Citation2010; McDermott et al. Citation2010; Pieper, Schröer, and Eilerts Citation2019). Indeed, a number of the records conclude that higher-quality evidence from future intervention research for older workers is needed including longitudinal studies (Crawford et al. Citation2009) as there is currently insufficient evidence to recommend specific interventions (Pieper, Schröer, and Eilerts Citation2019).
4. Discussion
This review of interventions to improve older worker health, safety and well-being at work examined a comprehensive range of literature, including literature reviews, primary research records, and grey literature. The paucity in the quality and scope of documented evidence for what works in preventing older worker injuries identified in this review suggests the need for a future research agenda that combines robust evidence-based intervention, implementation and evaluation methodologies with appropriate intervention designs. Furthermore, future research will need to have a specific focus on interventions that are effective in preventing the two most frequent and overwhelmingly costly injury types: WMSD and psychological injury. In most of the interventions reviewed, the role of industry or workplace context was not well addressed. Yet we argue that context is a fundamental consideration in the design and implementation of interventions to reduce physical and psychological injury in older workers (Cox et al. Citation2000; Safe Work Australia (Citation2020). More broadly still, many future of work trends are impacting how, where, when and with whom we work (Bentley et al. Citation2021), and it is vital that these changes are considered in research on the design of work and interventions to promote health and safety for older workers. The future research agenda set out in responds to some of the shortcomings in the extant literature and is discussed further below.
Figure 4. A future research agenda for older worker health, safety and well-being interventions.
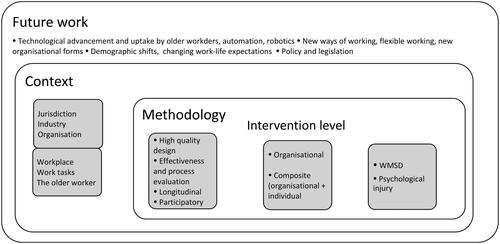
4.1. Future of work
Many of the intervention studies identified in this review were undertaken in the 2000–2016 period, meaning most were not cognisant of the more recent, and substantial, demographic and technological shifts that have reshaped the older worker landscape (Bentley et al. Citation2021). With so few recent, replicated (or expanded) studies looking at interventions on older workers, there is a significant gap in knowledge. Indeed, technology was largely ignored in the interventions, despite the promise for adopting technological measures to reduce excessive physical and psychological demands on older workers (Anders Citation2015; Horton et al. Citation2018). Indeed, factors influencing the adoption and use of new technologies by older workers need to be considered. Undoubtedly, greater understanding of contemporary issues and challenges that older workers face will benefit from research that focuses on identifying and understanding potential hazards related to psychological health and WMSD in this new work environment. Such research would provide greater insight into how to better integrate older workers into work settings now and into the future in a way that prevents psychological injuries and WMSD. The way we work is evolving at a very rapid pace, therefore, a framework for preventing psychological injury and WMSD among older workers that relies on the modest literature available could already be outdated. Hence, there is a need to take the current rapidly evolving work environment into account when devising intervention strategies for older workers. Since the scientific literature has not caught up with recent changes in the world of work, any intervention strategies put forward will have to rely on a strong theoretical framework to guide their development. Given these omissions, future research should examine the role of technological advancements, including automation, robotics/co-bots, and assistive technologies to enhance work and health outcomes including longevity for older workers. Similarly, the role of new ways of working, notably flexible work arrangements (Bentley et al. Citation2017; Green et al. Citation2020) should also be considered given the indications of their increasing application in the post-COVID-19 world of work.
4.2. The role of context
Many of the records included in this review did not address the issue of context in any depth, with an assumption of homogeneity in the design and implementation of interventions. While the organisational or industry context was mentioned in 17 of the 21 intervention studies reviewed, there was a lack of elaboration on why the intervention design was related to the specific context of its application. For example, while a number of intervention records dealt with high-risk industry sectors for older workers, including construction (Hengel et al. Citation2011), agriculture (Nilsson Citation2016) and health (Andersson-Felé Citation2005; Maatouk et al. Citation2018; Palumbo et al. Citation2012; Strijk et al. Citation2012), this context did not appear to form a key part of the rationale for the choice of intervention, nor for the interpretation and implications of findings. Furthermore, different work contexts such as larger or smaller workplaces, knowledge workers and skilled workers, white and blue collar, flexible workers and office-based workers were not well addressed, yet older workers in each context will respond differently to a given intervention, and interventions may be more or less effective in different contexts or settings. Additionally, because of the age of the records reviewed, nothing was learned about the context of COVID-19 and the pandemic’s restrictions on work. Indeed, impacts of the current COVID-19 context include increased mental health concerns for socially isolated workers, sedentary work, changes to physical activity, flexible working, prolonged screen time, and so on. In addition, early predictions suggest population changes due to the impact of COVID-19 on migration (Centre for Population Australian Government Citation2020) and this will have long-term effects for the longevity of the workforce. Clearly, future research needs to be designed to meet the health and safety needs of older workers and contemporary organisational workplaces. Moreover, future research should address these wider issues of context to understand what approach works best in different settings and when designing interventions for older workers.
4.3. Culture, climate and leadership
Two of the included interventions studies noted that workplace culture, climate and leadership were key enablers of healthy and active ageing for employees (Skoglund and Skoglund Citation2005; Hengel et al. Citation2011). In both studies, the authors noted that effective leadership, at both the senior and line level, as well as an inclusive workplace climate, was key to facilitating dialogue between older workers and other cohorts about workplace health. The role of leadership and climate in advancing a psychologically safe environment within an organisation is well established, but the two papers implied that management considerations can have much broader implications for setting an agenda around stigma and ageing, WMSD prevention and physical activity at work, as well as mental health considerations. Future research may seek to develop a more nuanced understanding regarding how workplace culture, climate and leadership can shape (or reshape) foundational values about the role of older workers and track the direct and indirect effect of management support on health, engagement, longevity and well-being outcomes for older workers.
4.4. Participatory interventions
Just one study in the intervention records reported a participatory intervention (Hengel et al. Citation2011); moreover, the study only reported on the co-design of an intervention and not its implementation. This is a concern given the importance placed on participatory approaches to organisational interventions involving end-users, employees, managers and others in intervention and implementation design (Eurofound and EU-OSHA Citation2014; EU-OSHA Citation2018; Leka, Van Wassenhove, and Jain Citation2015; Nielsen and Christensen Citation2021). Indeed, participatory approaches are favoured for intervention to prevent WMSD (Oakman, Macdonald, and Wells Citation2014) and psychosocial risks (Leka, Van Wassenhove, and Jain Citation2015; Neilsen et al. Citation2010) to provide subject matter expertise and ownership of interventions and workplace context to ensure a good fit for the cohort (Piszczek and Pimputkar Citation2021). Future research is needed to explore participatory interventions in organisations that might help shift stigma that inhibits longevity for older workers, irrespective of their physical health and mental resilience. The need for work design and the work environment to be improved in a coordinated fashion would appear essential to creating healthier older workers.
4.5. The primacy of organisational and composite approaches to intervention
While the intervention records provided support for organisational intervention, study designs and evaluation methodologies were often of low quality and the majority did not provide longitudinal evidence to support the effectiveness of these approaches. While this is a major limitation in the body of work reviewed, an organisational approach is supported by research on the wider workforce and reflects the legislative requirements in most jurisdictions to provide a safe place of work and to manage hazards that can impact worker health, safety and well-being. While organisational intervention is desirable as it addresses the risks closest to the source of harm, individual-level interventions were examined in approximately one-half of the intervention records reviewed. These studies tended to use higher quality evaluation designs (i.e. RCT), but on the whole failed to find longer-term support for the effectiveness of interventions to influence health, safety and workability outcomes. The review records provided very limited evidence that individual-level interventions such as health promotion, exercise, web-based programs and training can have positive outcomes for older workers (Merom et al. Citation2021; Poscia et al. Citation2016), while the intervention records offered evidence of only short-term improvements for the most common approaches, including physical activity and training (Cook et al. Citation2015). Indeed, in some cases, no significant effect was observed for older workers for specific interventions, including workstation ergonomics enhancements (May et al. Citation2004), and the opportunity for flexible work (Piszcsek and Pimputkar Citation2020).
The most promising, effective approaches in the literature for health, safety and workability outcomes were composite interventions. These integrated approaches can be considered systematic solutions for complex problems (Cooklin et al. Citation2017) and seem to be more effective than unidimensional approaches (Avendano and Cylus Citation2019). While these approaches make identification of the more effective elements of a composite intervention difficult if not impossible to determine, they reflect the complexity of occupational injury prevention and support a systems approach to intervention. The studies focussed on promoting older worker health and safety through changes to both work environment (fitting the work to the person) and improvements to the employee’s ability to maintain well-being, performance and longevity in work. At the same time, no identified study tracked the impact of any one intervention on enabling an employee’s likelihood to remain engaged in the workforce for a longer time. Future studies need to look specifically at the outcome of ‘engaged longevity’ (remaining in the workforce, healthily, and for longer) of older workers, to meet the growing and pernicious demographic challenges.
4.6. Limitations
This literature review was limited in that it did not examine interventions that were not originally intended for older workers, but that could have been applied or re-purposed for an older worker context. This means that some relevant material may have been overlooked. Further, the review was restricted to peer-reviewed and grey literature published since 2000 due to the funder’s requirement to focus on relatively recent research on intervention to prevent injury in older workers, meaning earlier work of relevance was excluded. Furthermore, the quality of intervention and/or evaluation descriptions provided in a small number of the outputs included in our review were limited, meaning some details were unavailable to the review. Finally, a protocol, guided by PRISMA, was implemented to minimise researcher bias and to provide broad quality checks (e.g. peer-reviewed was a baseline quality check for scholarly literature). In addition, informal discussions occurred within the research team about the selected literature during review; however, due to the type and range of literature included in the review, formal reviewer reliability checks were not conducted. Therefore, the findings should be considered in respect to this limitation.
5. Conclusion
The existing literature examining interventions provides some evidence that composite and organisational interventions are most effective in improving physical and psychological injury outcomes amongst older workers. Interventions that focus on the individual appear less effective when used as the sole approach to prevention, although appear to be more effective when coupled with organisational interventions. These findings are limited, however, as there are only a small number of high-quality intervention studies published, with limited evaluation and a lack of participatory approaches. Little attention has been paid to context and the changing landscape of work. These concerns should be addressed through a future research agenda considering the future of work, context, high quality methodology, intervention levels and a focus on WMSD and psychological injuries of older workers.
Supplemental Material
Download Zip (152.4 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Anders, G. 2015. “Aging Workers, New Technology.” MIT Technology Review. Accessed 8 September 2021. https://www.technologyreview.com/2015/09/28/166065/aging-workers-new-technology/.
- Andersson-Felé, L. 2005. “Age Related Workload—A Work Environment Intervention with a Life Course Perspective.” In International Congress Series 1280: 341–346. doi:10.1016/j.ics.2005.01.017.
- Association of Occupational and Environmental Clinics and Society of Occupational and Environmental Health (AOEC & CSOEH). 2009. “Healthy Aging for a Sustainable Workforce: A Conference Report.” Accessed 9 September 2021. https://www.cpwr.com/wp-content/uploads/publications/Aging-Workers-Workshop-Report_11-09_Final.pdf.
- Avendano, M., and J. Cylus. 2019. Working at Older Ages. Copenhagen: WHO Regional Office for Europe.
- Beehr, T. A., S. Glazer, N. L. Nielson, and S. J. Farmer. 2000. “Work and Nonwork Predictors of Employees’ Retirement Ages.” Journal of Vocational Behavior 57 (2): 206–225. doi:10.1006/jvbe.1999.1736.
- Beers, H. & Butler, C. 2012. “Age related changes and safety critical work: Identification of tools and a review of the literature” Health and Safety Executive Research Report RR946.
- Bentley, T., C. Caponecchia, L. A. Onnis, B. Farr-Wharton, A. Vassiley, S. O'Neill, C. Andrew, A. De Almeida Neto, and V. Huron. 2022. “The Healthy Older Worker: A Systematic Review of Literature on Work Health and Safety Interventions for Older Worker: Industry Summary.” Report,//www.centreforwhs.nsw.gov.au/__data/assets/pdf_file/0020/1114256/Centre-for-Work-Health-and-Safety-The-HOW-toolkit-Literature-Review-Industry-Summary.pdf.
- Bentley, T., K. Blackwood, B. Catley, M. P. O'Driscoll, M. Roche, S. Teo, and L. Twiname. 2017. “The Role of Human Resource Practices and Other Factors Influencing the Continuing Work Participation of Older Workers in New Zealand.” In The Aging Workforce Handbook: Individual, Organizational, and Societal Challenges, edited by A. Antoniou, R. J. Burke, and C. L. Cooper, 213–239. Bingley: Emerald Group Publishing Limited.
- Bentley, T., N. Green, D. Tappin, and R. Haslam. 2021. “State of Science: The Future of Work – Ergonomics and Human Factors Contributions to the Field.” Ergonomics 64 (4): 427–439. doi:10.1080/00140139.2020.1841308.
- Bentley, T. A., T. T. Teo, B. Catley, K. Blackwood, M. Roche, and M. P. O’Driscoll. 2019. “Factors Influencing Leave Intentions among Older Workers: A Moderated-Mediation Model.” Personnel Review 48 (4): 898–914. doi:10.1108/PR-03-2018-0095.
- Bibby, C. 2008. “Should I Stay or Should I Leave? Perceptions of Age Discrimination, Organizational Justice, and Employee Attitudes on Intentions to Leave.” Journal of Applied Management and Entrepreneurship 13 (2): 63–86.
- Blok, M. M., and M. P. de Looze. 2011. “What is the Evidence for Less Shift Work Tolerance in Older Workers?” Ergonomics 54 (3): 221–232. doi:10.1080/00140139.2010.548876.
- Caponecchia, C., R. L. Coman, V. Gopaldasani, E. C. Mayland, and L. Campbell. 2020. “Musculoskeletal Disorders in Aged Care Workers: A Systematic Review of Contributing Factors and Interventions.” International Journal of Nursing Studies 110: 103715.
- Centre for Population, Australian Government. 2020. “Population Statement.” Accessed 13 September 2021. Retrieved from December 2020. https://population.gov.au/docs/population_statement_2020.pdf.
- Chiu, W.C., A.W. Chan, E. Snape, and T. Redman. 2001. “Age Stereotypes and Discriminatory Attitudes towards Older Workers: An East-West Comparison.” Human Relations 54 (5): 629–661. doi:10.1177/0018726701545004.
- Cirla, A. M., R. Fazioli, F. Santini, and P. E. Cirla. 2005. “Prevention of Musculo-Skeletal Disorders in Sedentary Ageing Workers by Ergomotricity.” International Congress Series 1280: 166–171. doi:10.1016/j.ics.2005.02.084.
- Cook, R. F., R. K. Hersch, D. Schlossberg, and S. L. Leaf. 2015. “A Web-Based Health Promotion Program for Older Workers: Randomized Controlled Trial.” Journal of Medical Internet Research 17 (3): e3399. doi:10.2196/jmir.3399.
- Cooklin, A., N. Joss, E. Husser, and B. Oldenburg. 2017. “Integrated Approaches to Occupational Health and Safety: A Systematic Review.” American Journal of Health Promotion 31 (5): 401–412. doi:10.4278/ajhp.141027-LIT-542.
- Costa, G., and S. Sartori. 2007. “Ageing, Working Hours and Work Ability.” Ergonomics 50 (11): 1914–1930. doi:10.1080/00140130701676054.
- Cox, T., A. Griffiths, C. Barlowe, R. Randall, L. Thomson, and E. Rial-Gonzalez. 2000. “Organisational Interventions for Work Stress, A risk Management Approach, HSE Contract Research Report 286/2000.” https://www.hse.gov.uk/research/crr_pdf/2000/crr00286a.pdf/.
- Crawford, J. O., Davis, A., Cowie, H., Dixon, K., Mikkelsen, S. H., Bongers, P., Graveling, R., Beline , and Dupont, C. 2016. The Ageing Workforce: Implications for Occupational Safety and Health. Luxumberg, Belgium: European Agency for Safety and Health at Work (EU-OSHA).
- Crawford, J. O., R. A. Graveling, H. A. Cowie, and K. Dixon. 2010. “The Health Safety and Health Promotion Needs of Older Workers.” Occupational Medicine 60 (3): 184–192. doi:10.1093/occmed/kqq028.
- Crawford, J. O., R. A. Graveling, H. Cowie, K. Dixon, and L. MacCalman. 2009. The Health, Safety and Health Promotion Needs of Older Workers, an Evidence-Based Review and Guidance. UK: IOSH.
- De Boer, A. G. E. M., J. C. Van Beek, J. Durinck, J. H. A. M. Verbeek, and F. J. H. Van Dijk. 2004. “An Occupational Health Intervention Programme for Workers at Risk for Early Retirement; a Randomised Controlled Trial.” Occupational and Environmental Medicine 61 (11): 924–929. doi:10.1136/oem.2003.009746.
- Delloiacono, N. 2015. “Musculoskeletal Safety for Older Adults in the Workplace: Review of Current Best Practice Evidence.” Workplace Health & Safety 63 (2): 48–53. doi:10.1177/2165079915570299.
- Denton, J., D. Evans, and Q. Xu. 2021. “Older Nurses and Midwives in the Workplace: A Scoping Review.” Collegian 28 (2): 222–229. doi:10.1016/j.colegn.2020.06.004.
- Dul, J., R. Bruder, P. Buckle, P. Carayon, P. Falzon, W. S. Marras, J. R. Wilson, and B. van der Doelen. 2012. “A Strategy for Human Factors/Ergonomics: developing the Discipline and Profession.” Ergonomics 55 (4): 377–395. doi:10.1080/00140139.2012.661087.
- Elton, E., and C. Nicolle. 2015. “Inclusive Design and Design for Special Populations.” In Evaluation of Human Work, edited by J. Wilson and S. Sharples, 4th ed., 299–329. Boca Raton: CRC Press.
- EU-OSHA. 2018. Management of Psychosocial Risks in European Workplaces – Evidence from the Second European Survey of Enterprises on New and Emerging Risks (ESENER-2). Luxembourg: European Agency for Safety and Health at Work.
- Eurofound and EU-OSHA. 2014. Psychosocial Risks in Europe: Prevalence and Strategies for Prevention. Luxembourg: European Agency for Safety and Health at Work.
- European Agency for Safety and Health at Work (EU-OSHA). 2007. Expert Forecast on Emerging Psychosocial Risks Related to Occupational Safety and Health. Luxembourg, Belgium: European Agency for Safety and Health at Work.
- Gerr, F., N. B. Fethke, D. Anton, L. Merlino, J. Rosecrance, M. Marcus, and M. P. Jones. 2014. “A Prospective Study of Musculoskeletal Outcomes among Manufacturing Workers: II. Effects of Psychosocial Stress and Work Organization Factors.” Human Factors 56 (1): 178–190. doi:10.1177/0018720813487201.
- Gershon, R. R., S. Lin, and X. Li. 2002. “Work Stress in Aging Police Officers.” Journal of Occupational and Environmental Medicine 44 (2): 160–167. doi:10.1097/00043764-200202000-00011.
- Granacher, U., C. Wick, N. Rueck, C. Esposito, R. Roth, and L. Zahner. 2011. “Promoting Balance and Strength in the Middle-Aged Workforce.” International Journal of Sports Medicine 32 (1): 35–44. doi:10.1055/s-0030-1267214.
- Green, N., D. Tappin, and T. Bentley. 2020. “Working from home before, during and after the Covid-19 pandemic: implications for workers and organisations.” New Zealand Journal of Employment Relations 45 (2): 5–16.
- Guglielmi, D., L. Avanzi, R. Chiesa, M. G. Mariani, I. Bruni, and M. Depolo. 2016. “Positive Aging in Demanding Workplaces: The Gain Cycle Between Job Satisfaction and Work Engagement.” Frontiers in Psychology 7: 1224. doi:10.3389/fpsyg.2016.01224.
- Härmä, M., H. Tarja, K. Irja, S. Mikael, V. Jussi, B. Anne, and M. Pertti. 2006. “A Controlled Intervention Study on the Effects of a Very Rapidly Forward Rotating Shift System on Sleep–Wakefulness and Well-Being among Young and Elderly Shift Workers.” International Journal of Psychophysiology 59 (1): 70–79. doi:10.1016/j.ijpsycho.2005.08.005.
- Hengel, K. M. O., C. I. Joling, K. I. Proper, H. F. Van Der Molen, and P. M. Bongers. 2011. “Intervention Mapping as a Framework for Developing an Intervention at the Worksite for Older Construction Workers.” American Journal of Health Promotion 26 (1): E1–10. doi:10.4278/ajhp.100326-QUAL-88.
- Hesselink, J. K., J. de Leede, and A. Goudswaard. 2010. “Effects of the New Fast Forward Rotating Five-Shift Roster at a Dutch Steel Company.” Ergonomics 53 (6): 727–738. doi:10.1080/00140139.2010.489651.
- Horton, J., A. Cameron, D. Devaraj, R. T. Hanson, and S. A. Hajkowicz. 2018. Workplace Safety Futures: The Impact of Emerging Technologies and Platforms on Work Health and Safety and Workers’ Compensation over the Next 20 Years. Canberra: CSIRO.
- Institute of Medicine. 2004. Health and Safety Needs of Older Workers. Washington, DC: The National Academies Press.
- Johnston, D. W., and W. S. Lee. 2009. “Retiring to the Good Life? The Short-Term Effects of Retirement on Health.” Economics Letters 103 (1): 8–11. doi:10.1016/j.econlet.2009.01.015.
- Karazman, R., I. Kloimüller, H. Geissler, and I. Karazman-Morawetz. 2000. “Effects of Ergonomic and Health Training on Work Interest, Work Ability and Health in Elderly Public Urban Transport Drivers.” International Journal of Industrial Ergonomics 25 (5): 503–511. doi:10.1016/S0169-8141(99)00037-2.
- Kooij, D. T. A. M., P. G. W. Jansen, J. S. E. Dikkers, and A. H. De Lange. 2010. “The Influence of Age on the Associations between HR Practices and Both Affective Commitment and Job Satisfaction: A Meta-Analysis.” Journal of Organizational Behavior 31 (8): 1111–1136. doi:10.1002/job.666.
- Kumashiro, M. 2000. “Ergonomics Strategies and Actions for Achieving Productive Use of an Ageing Work-Force.” Ergonomics 43 (7): 1007–1018. doi:10.1080/001401300409189.
- Lang, J., E. Ochsmann, T. Kraus, and J. W. B. Lang. 2012. “Psychosocial Work Stressors as Antecedents of Musculoskeletal Problems: A Systematic Review and Meta-Analysis of Stability-Adjusted Longitudinal Studies.” Social Science & Medicine 75 (7): 1163–1174. doi:10.1016/j.socscimed.2012.04.015.
- Leka, S., W. Van Wassenhove, and A. Jain. 2015. “Is Psychosocial Risk Prevention Possible? Deconstructing Common Presumptions.” Safety Science 71: 61–67. doi:10.1016/j.ssci.2014.03.014.
- Léime, Á. N., and J. Ogg. 2019. “Gendered impacts of extended working life on the health and economic wellbeing of older workers.” Ageing & Society 39 (10): 2163–2169.
- Maatouk, I., A. Müller, P. Angerer, R. Schmook, C. Nikendei, K. Herbst, M. Gantner, W. Herzog, and H. Gündel. 2018. “Healthy Ageing at work- Efficacy of Group Interventions on the Mental Health of Nurses Aged 45 and Older: Results of a Randomised, Controlled Trial.” PLOS One 13 (1): e0191000. doi:10.1371/journal.pone.0191000.
- Macdonald, W., and O. Evans. 2006. Research on the Prevention of Work-Related Musculoskeletal Disorders: Stage 1: Literature Review. Canberra: Safe Work Australia.
- Mauno, S., M. Ruokolainen, and U. Kinnunen. 2013. “Does Aging Make Employees More Resilient to Job Stress? Age as a Moderator in the Job Stressor–Well-Being Relationship in Three Finnish Occupational Samples.” Aging & Mental Health 17 (4): 411–422. doi:10.1080/13607863.2012.747077.
- May, D. R., C. E. Schwoerer, K. Reed, and P. Potter. 2004. “Ergonomic Office Design and Aging: A Quasi-Experimental Field Study of Employee Reactions to an Ergonomics Intervention Program.” Journal of Occupational Health Psychology 9 (2): 123–135. doi:10.1037/1076-8998.9.2.123.
- McDermott, H. J., A. Kazi, F. Munir, and C. Haslam. 2010. “Developing Occupational Health Services for Active Age Management.” Occupational Medicine 60 (3): 193–204. doi:10.1093/occmed/kqq026.
- Merom, D., F. Stanaway, K. Gebel, J. Sweeting, A. Tiedemann, S. Mumu, and D. Ding. 2021. “Supporting Active Ageing before Retirement: A Systematic Review and Meta-Analysis of Workplace Physical Activity Interventions Targeting Older Employees.” BMJ Open 11 (6): e045818. doi:10.1136/bmjopen-2020-045818.
- Morelock, J. C., T. K. McNamara, and J. B. James. 2017. “Workability and Requests for Flexible Work Arrangements among Older Adults: The Role of a Time and Place Management Intervention.” Journal of Applied Gerontology 36 (11): 1370–1392. doi:10.1177/0733464815624149.
- Morschhäuser, M., and R. Sochert. 2006. Healthy Work in an Ageing Europe, Strategies and Instruments for Prolonging Working Life. Essen, Germany: Federal Association of Company Health Insurance Funds.
- National Institute of Economic and Social Research. 2017. “Older Workers and the Workplace: Evidence from the Workplace Employment Relations Survey, Research Report No 939.” https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/584727/older-workers-and-the-workplace.pdf.
- Nielsen, K., and J. S. Abildgaard. 2013. “Organizational interventions: A research-based framework for the evaluation of both process and effects.” Work & Stress 27 (3): 278–297.
- Nielsen, K., R. Randall, A. L. Holten, and E. R. Schmook. 2010. “Conducting organizational-level occupational health interventions: What works?” Work & Stress 24 (3): 234–259.
- Nielsen, K., and M. Christensen. 2021. “Positive Participatory Organizational Interventions: A Multilevel Approach for Creating Healthy Workplaces.” Frontiers in Psychology 12: 696245. doi:10.3389/fpsyg.2021.696245.
- Nilsson, K. 2016. “Interventions to Reduce Injuries among Older Workers in Agriculture: A Review of Evaluated Intervention Projects.” Work 55 (2): 471–480. doi:10.3233/WOR-162407.
- Oakman, J., S. Clune, and R. Stuckey. 2019. Work-Related Musculoskeletal Disorders in Australia. Canberra: Safe Work Australia.
- Oakman, J., W. Macdonald, and Y. Wells. 2014. “Developing a Comprehensive Approach to Risk Management of Musculoskeletal Disorders in Non-Nursing Health Care Sector Employees.” Applied Ergonomics 45 (6): 1634–1640. doi:10.1016/j.apergo.2014.05.016.
- Page, M. J., J. E. McKenzie, P. M. Bossuyt, I. Boutron, T. C. Hoffmann, C. D. Mulrow, L. Shamseer, J. M. Tetzlaff, E. A. Akl, S. E. Brennan, R. Chou, J. Glanville, J. M. Grimshaw, A. Hróbjartsson, M. M. Lalu, T. Li, E. W. Loder, E. Mayo-Wilson, S. McDonald, L. A. McGuinness, L. A. Stewart, J. Thomas, A. C. Tricco, V. A. Welch, P. Whiting, and D. Moher. 2021. “The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews.” BMJ 372: n71. doi:10.1136/bmj.n71P.
- Palumbo, M. V., G. Wu, H. Shaner-McRae, B. Rambur, and B. McIntosh. 2012. “Tai Chi for Older Nurses: A Workplace Wellness Pilot Study.” Applied Nursing Research 25 (1): 54–59. doi:10.1016/j.apnr.2010.01.002.
- Pieper, C., S. Schröer, and A. L. Eilerts. 2019. “Evidence of Workplace Interventions-A Systematic Review of Systematic Reviews.” International Journal of Environmental Research and Public Health 16 (19): 3553. doi:10.3390/ijerph16193553.
- Piszczek, M. M., and A. S. Pimputkar. 2021. “Flexible Schedules across Working Lives: Age-Specific Effects on Well-Being and Work.” The Journal of Applied Psychology 106 (12): 1907–1920. doi:10.1037/apl0000844.
- Poscia, A., U. Moscato, D. I. La Milia, S. Milovanovic, J. Stojanovic, A. Borghini, A. Collamati, W. Ricciardi, and N. Magnavita. 2016. “Workplace Health Promotion for Older Workers: A Systematic Literature Review.” BMC Health Services Research 16 (S5): 415–428. doi:10.1186/s12913-016-1518-z.
- Queensland Government, Office of Industrial Relations. 2019. “Ageing Workforce Report: Employer Readiness to Support the Needs of Australia’s Ageing Workforce.” https://www.worksafe.qld.gov.au/__data/assets/pdf_file/0016/22156/australias-ageing-workforce-report-2019.pdf.
- Raab, R. 2020. “Workplace Perception and Job Satisfaction of Older Workers.” Journal of Happiness Studies 21 (3): 943–963. doi:10.1007/s10902-019-00109-7.
- Robertson, J., C. Jayne, and J. Oakman. 2021. “Work-Related Musculoskeletal and Mental Health Disorders: Are Workplace Policies and Practices Based on Contemporary Evidence?” Safety Science 138: 105098. doi:10.1016/j.ssci.2020.105098.
- Roper, K. O., and D. C. Yeh. 2007. “Ergonomic Solutions for an Aging Workforce.” Journal of Facilities Management 5 (3): 172–178. doi:10.1108/14725960710775054.
- Safe Work Australia. 2020. “Principles-Good-Work-Design: A Work Health and Safety Handbook.” https://www.safeworkaustralia.gov.au/system/files/documents/1702/good-work-design-handbook.pdf.
- Santos, S. R., C. A. Carroll, K. S. Cox, S. L. Teasley, S. D. Simon, L. Bainbridge, M. Cunningham, and L. Ott. 2003. “Baby Boomer Nurses Bearing the Burden of Care: A Four-Site Study of Stress, Strain, and Coping for Inpatient Registered Nurses.” The Journal of Nursing Administration 33 (4): 243–250. doi:10.1097/00005110-200304000-00010.
- Skoglund, B., and C. Skoglund. 2005. “Can Age Management Promote Work Ability among Older Workers?” In International Congress Series 1280: 392–396. doi:10.1016/j.ics.2005.02.049.
- Söderbacka, T., L. Nyholm, and L. Fagerström. 2020. “Workplace Interventions That Support Older Employees’ Health and Work ability – A Scoping Review.” BMC Health Services Research 20 (1): 1–9. doi:10.1186/s12913-020-05323-1.
- Strijk, J. E., K. I. Proper, A. J. Van der Beek, and W. van Mechelen. 2012. “A Worksite Vitality Intervention to Improve Older Workers’ Lifestyle and Vitality-Related Outcomes: Results of a Randomised Controlled Trial.” Journal of Epidemiology and Community Health 66 (11): 1071–1078. doi:10.1136/jech-2011-200626.
- Stynen, D., N. W. H. Jansen, and I. Kant. 2017. “The Impact of Work-Related and Personal Resources on Older Workers’ Fatigue, Work Enjoyment and Retirement Intentions over Time.” Ergonomics 60 (12): 1692–1707. doi:10.1080/00140139.2017.1334094.
- Taieb-Maimon, M., J. Cwikel, B. Shapira, and I. Orenstein. 2012. “The Effectiveness of a Training Method Using Self-Modeling Webcam Photos for Reducing Musculoskeletal Risk among Office Workers Using Computers.” Applied Ergonomics 43 (2): 376–385. doi:10.1016/j.apergo.2011.05.015.
- Teo, S. T., T. A. Bentley, D. Nguyen, K. Blackwood, and B. Catley. 2022. “Inclusive Leadership, Matured-Age HRM Practices and Older Worker Well-Being.” Asia Pacific Journal of Human Resources 60 (2): 323–341. doi:10.1111/1744-7941.12304.
- Thorsen, S. V., P. H. Jensen, and J. B. Bjørner. 2016. “Psychosocial Work Environment and Retirement Age: A Prospective Study of 1876 Senior Employees.” International Archives of Occupational and Environmental Health 89 (6): 891–900. doi:10.1007/s00420-016-1125-7.
- Tugman, K. 2013. “Aging Workforce Update.” Professional Case Management 18 (3): 155–157. doi:10.1097/NCM.0b013e31828ad597.
- Vanajan, A., U. Bültmann, and K. Henkens. 2020. “Health-Related Work Limitations among Older workers – The Role of Flexible Work Arrangements and Organizational Climate.” The Gerontologist 60 (3): 450–459. doi:10.1093/geront/gnz073.
- Varianou-Mikellidou, C., G. Boustras, C. Dimopoulos, J. L. Wybo, F. W. Guldenmund, O. Nicolaidou, and I. Anyfantis. 2019. “Occupational Health and Safety Management in the Context of an Ageing Workforce.” Safety Science 116: 231–244. doi:10.1016/j.ssci.2019.03.009.
- Weichel, J., S. Stanic, J. A. Enriquez Diaz, and E. Frieling. 2010. “Job Rotation – Implications for Old and Impaired Assembly Line Workers.” Occupational Ergonomics 9 (2): 67–74. doi:10.3233/OER-2010-0172.
- WorkSafe, WA. 2010. “Understanding the Safety and Health Needs of Your Workplace Older Workers and Safety.” https://www.commerce.wa.gov.au/sites/default/files/atoms/files/older_workers_guide_.pdf.
- World Health Organization. 1993. Aging and Working Capacity: Report of a WHO Study Group. Geneva: World Health Organization.
- World Health Organization. 2015. World Report on Ageing and Health. Geneva: WHO.
