Abstract
Background
Many governments have introduced health insurance schemes for the poor sections of society to save them from catastrophic health expenditure. Private hospitals play a key role in India, as they are in significant number in secondary and tertiary care services. Private hospitals have to fund their infrastructure, staff salaries from the revenue of previous year. In this study, we compared money received by a private medical college hospital bed through government insurance scheme patient and private paying patient.
Methods
Observational study, comparing money reimbursed for top ten procedures treated in private medical college hospitals by Ayushman Bharat (AB) fund and the price offered by a paying patient in similar bed.
Results
On average 600 patients received medical care through the AB scheme per month at our tertiary care super-specialty hospital. Highest numbers were seen in specialties like cardiovascular, and cancer treatments and infectious diseases under general medicine specialty. The costs considered were surgeon’s cost, medicines, devices, and hospitalization costs. The laparoscopic procedures were incurring a loss of 130%, knee replacements about 50%, coronary bypass grafting thankfully due to controlling of prices by central government is incurring a loss of 10%. The package amount offered accounts to 26–52% only of the costs incurred by the private hospitals.
Conclusion
The private academic hospitals need 25% to 50% more than current prices offered, across various procedures.
Introduction
Universal health coverage schemes are ambitiously launched in developing countries to reduce catastrophic healthcare expenditure proportion by economically weaker sections of society., As per National Health accounts estimates data for 2015–16 year, The Total Health Expenditure (THE) in India was Rs. 5,28,484 crores out of which government health expenditure (GHE) is 30.6% of THE (Rs. 1, 61, 863 Crore, at the time of this study $ 1 = Rs. 74.40) and household expenditure (HHE) amounts to 60.4% of THE (Rs. 3,20,211 crore) mainly through Out-of-pocket expenditure (OOPE) THE would be 3.84% of total GDP, at Rs. 4116 per capita spending, GHE would be 1.18% and HHE at 2.3% of GDP. Over the last decade (2011–2020), the Indian population has increased by 13% to 160 crores, during same period, the government healthcare expenditure has increased only by 0.39% (National Health Systems Resource Centre Citation2018). To pay for medical care and treatments, rural households depend primarily on their household income/savings (68%) and on borrowings (25%) whereas urban households relied more on their income/saving (75%) for financing expenditure on hospitalization, and lesser on borrowings (only 18%) (Andargie Citation2008). Hence, government health insurance schemes are the best available option for rural households.
Government insurance as a way of financing healthcare expenditure of low income groups is present since 2005 in India, under the flagship schemes like Rastriya Swasthya Bima Yojana (RSBY) by federal government, later in 2009, 2011 successive schemes were introduced by few state governments in South India under the names of Yeshasvini scheme, Arogyashree schemes. The challenges they faced were low population coverage of upto 12% of urban and 13% of the rural population, low sum assured in a year for a family of four – INR 30000 in RSBY, in other two schemes upto INR 150,000 to INR 200,000. The health coverage offered was for few illnesses, only elective surgeries, no emergency surgical and medical conditions were covered, higher waiting time for pre-authorization approvals, documentation and claim submissions hassles. To mitigate the above challenges through new scheme, the current federal government embarked on a journey creating an umbrella scheme called Ayushman Bharat scheme aiming to cover 40% of the population (National Health Authority Citationn.d.). The sum assured has been raised to INR 500,000 per year with 1400 procedures covered for a family of four, both emergency and elective procedures at tertiary care and secondary care level, better administration through nodal officers at district level, Arogyamitra as a coordinator of patients at every hospital, for claim submissions and approvals dedicated office at the state headquarters.
To make the insurance benefits reachable to community, support from both government owned hospitals and private hospitals is needed in India. Government hospitals are funded and owned by government. Private hospitals are started by proprietors and partners who invest large capital on real estate, buildings, equipment, payrolls of manpower, expensive diagnostic and therapeutic equipment. A specialty hospital has to procure specialized diagnostic and therapeutic equipment, medical technology, and skilled experts to provide service (Jaffrolet and Jumle Citation2020). All these resources need large capital to start a tertiary care public or a private hospital. Tertiary care and secondary care hospitals should have advanced radio-imaging modalities to identify and treat complex cases (Frija, et al. Citation2021), which only All India Institutes of Medical sciences managed by central government type of institutions among government institutions can afford to have. These institutions are less in number, one per state.
Many district hospitals and state-run medical college hospitals will lack sufficient equipment and their maintenance budgets. Government hospitals are lacking funds to provide medicines, precise and continuously working diagnostic armamentarium (Chatterjee, Levin, and Laxminarayan Citation2013). There are about 5649 community health centers, 1200 sub divisional hospitals, 810 district hospitals, 300 medical colleges run by government in India (NHM Citation2023). To achieve healthcare services accessibility to the vast populations, the private sector hospitals have to pitch in with their empanelment. And for Ayushman Bharat to achieve its goal, it has to welcome private hospitals enroll to the panel for accepting patients. There is a shortfall of them in catering to the large population. Private hospitals have to play a key role in the implementation of government sponsored health insurance schemes (GSHIS) in India (National Institute of Public Finance and Policy Citation2019). The costs incurred for extended stay of patients, higher antibiotics, cannulas will have to be levied on to end users, but hospitals are not allowed to collect extra expenses from GSHIS patients. It’s going to impact private hospitals with coming to terms with pricing that government schemes offer. Equating private hospitals to provide procedures at low bundled prices to patients is not ideal.
There were independent studies conducted by two nonprofit, non-government organizations on the rates charged by private nonacademic hospitals. These organizations were FICCI (called as Federation of Indian Chambers of Commerce and Industry, a non-government, not-for-profit organization, acting as voice of India’s business and industry, engages with policy makers and civil society equally) (FICCI Citation2017) and IMA-TN (Indian Medical Association, Tamilnadu unit – IMA is a voluntary, national organization of 0.33 million doctors which works toward upholding medical profession interests) (IMA Citation2021). These reports did not mention the methodology of costs calculation. In their joint study (FICCI Citation2021), it has been mentioned that average cost of treatment in a private hospital is Rs. 25,850/- as compared to INR 6,120 charged in a public hospital. The highest expenditure was recorded for treatment of cancer cycles (INR 56,712), followed by that for cardiovascular diseases (INR 31,647). Average medical expenditure per non-hospitalization case was INR 509 in rural India and INR 639 in urban India. Incidentally, 86% of rural and 82% of urban population are not covered under any scheme of health expenditure support (Naveen et al. Citation2014).
In India, private hospitals procedure prices and the length of stays are not capped, there are no upper tariff limits. It varies based on urban-rural location, based on consultation fee charges, based on profit margin perceived by owners, no standardized treatment protocols between two Unit of Consultants and medicine protocols. The medical college hospitals in India to accommodate patients for teaching and learning purposes of students operate at minimal profit margins (5%) when compared to opulent private hospitals in urban centers. The motive behind this study is to show case prices that can be offered by two private medical college hospitals which are relatively lesser when compared with city based hospitals. Most of the other private academic institutions will charge higher to patients. Government hospitals provide free of cost treatment. They were excluded from study. Hence, this study was conducted with the below mentioned aims and objectives.
Aim of the Study
To compare the costs incurred by the private medical college hospitals vis a vis the bundled packages offered by government sponsored scheme in India.
Objectives
To collect the price of ten most common procedures done as bundled packages in tertiary care hospitals under PMJAY-AB (Prime Minister Jan Arogya Yojana – Ayushman Bharat) scheme patients.
Identify the price difference between out of pocket payment patients and scheme patients.
Methods
Study Design
A qualitative, observational study was done comparing the hospital prices for top commonly done procedures under AB-ArK scheme and price incurred by self-paying patients.
Sample
Primary data is amount paid by paying patients collected from two tertiary care private medical college hospitals who were willing to share financial information. Secondary data collected from a report published from data of ten urban private hospitals were considered in the study. More academic hospitals were not included in sample size, as prices offered by other colleges for paying patients are higher and price information is deemed sensitive by management of hospitals. Study Variables
The top ten procedures in previous six months got referred from district hospitals under government insurance scheme (AB-ArK) were chosen from both hospitals, the amount paid by the scheme to hospital and the prices charged to self-paying patients of general ward category were compared. The amounts were taken from billing codes created in hospital billing department. When a patient gets treated, these procedures codes are applied and patient pays before discharge. The hospitals bills were covering – procedure costs, material costs, hospital room costs, nursing and doctor consultation costs, surgeon’s and anesthetists operating fees.
Duration of Study
6 months, January to June 2021.
Results
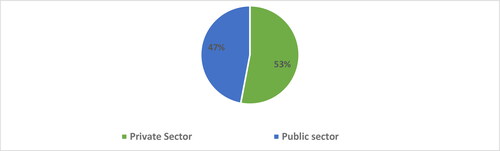
In India, hospitals are defined by public health authorities as “licensed establishments that are primarily engaged in providing inpatient and outpatient health services that include physician, nursing, diagnostic and other allied health services.” (National Health Systems Resource Centre Citation2018) As per national health mission portal estimates, in India there are about 15 lakh beds in secondary and tertiary care. Out of which 800,000 are there in private sector which accounts to major share of about 53%, as shown in .
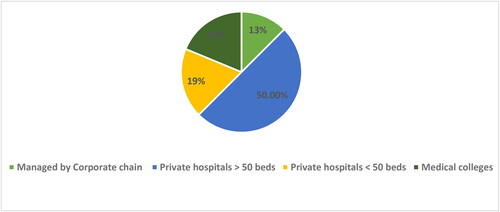
A National Sample Survey Office (NSSO) survey report done in 2013–14, found that 72% of the rural and 79% of the urban Indian population rely on private hospitals for treatment, represented in (National Health Authority Citationn.d.).
We considered the compilation of Registry of Hospitals in Network of Insurance (ROHINI) database published by Insurance Information Bureau (IIB) of India, carrying a repertoire of empaneled private hospitals by third party administrators to insurance companies. Hospitals enroll on a voluntary basis. IIB works in close association with government and other stakeholders equally. The hospitals thus shown can provide hospitalization services under private insurance schemes and also government-sponsored insurance schemes.
Out of 43,486 private hospitals, 450 private hospitals are empaneled for secondary or tertiary care in Karnataka. The administrator for government insurance scheme is called as Suvarna Arogya Karnataka Ayushman Bharat Trust. Apart from private hospitals, 2300 government hospitals also accept Ayushman Bharat patients for “simple procedure” and “wellness procedures” in this state. Around 15 of these government hospitals per district are catering to specialty care and tertiary care. The district hospitals which do not have requisite tertiary specialty refer their patients to private hospitals where this study was conducted. In the study, our hospitals accept on an average 600 patients per month, under the scheme. Out of which maximum cases are being seen in General medicine department, Cardiology specialty, Cancer care services. Patients visit hospitals from 6 districts around. Clinicians are eager to conduct procedures, as doctors get paid over and above fixed salaries as regular faculty under the college. Hence, the admission of patients happen under consultant in specialty under general ward beds and the bed charge is Rs. 900 per day with food and nursing charges included. shows the prices offered by a paying patient in general category (Column B) versus the price offered by Ayushman Bharat scheme patient. (Column A)
Table 1. Comparing bundled prices offered by Karnataka Ayushman Bharat scheme and average bill paid by the general category paying patient in private medical college hospital.
data infers that we incur a difference in loss between package amount offered under UHS and out of pocket payment patient, with both having similar length of stays. Laparoscopic Appendicectomy cost varies based on the mesh used to seal the gap along herniated space. As the implants and stent prices were capped by central government in year 2017, hospitals could incur lesser costs for PTCA procedure, which were more a decade back. LSCS (Lower segment Cesarean Section) incurs a huge loss, because volumes admitted under paying category also are high in our hospital, if we are going to think that to a medical college referral of UHS cases will be high in numbers, we have to allot more beds to UHS patients. For this package if price can be increased by 100% it would be exceptionally good.
We have used costs in this study for the materials and brands of stents as approved by government agencies, mentioned by ABArK packages, which were price capped and supplied by government approved suppliers, hence, the difference of loss comes to minimal. When, we compare the same prices with studies published by FICCI and IMA, it shows difference in highest ranges as in .
Table 2. Comparing bundled prices offered by Suvarna Karnataka Ayushman Bharat scheme and average cost incurred by the private nonacademic hospitals (Reported by FICCI and IMA).
FICCI and IMA studies (FICCI Citation2021) doesn’t mention the type of stents used, brand of knee replacement disks used, hence, we observe that the difference of cost is shown in higher ranges. These hospitals accept less number of patients through government schemes compared to academic hospitals. These hospitals are extending their hospitals to government scheme patients in sub-urban areas of cities, providing services in low cost settings. People have to spend on transportation to reach such facilities. Documentation work is another grouse that doctors have about scheme patients, which includes taking a photograph pre and post-surgery. Bill amount monitoring has to be done, as scheme patient is not going to pay, it will be shown as loss under the specialty consultant. Hospitals have to increase their manpower in the Billing departments who need to be allocated for Pre-authorization and post-treatment discharge documentation work. Many records will be held at billing desks and these personnel have to follow up with doctors for deficiency in medical records. As government agencies are taking pro-active decisions in monitoring the prices of supplies to hospitals, we are able to provide universal health coverage to the approved list of beneficiaries in large numbers at private medical college hospitals.
Discussion
Both private medical colleges in this study had similar prices offered to self-paying patients. The AB-ArK prices offered to all institutions are one and the same. By comparing these procedure codes prices between self-paying patient and AB-ArK codes, we can infer that on an average amount lost by the private hospitals is around 2 to 4 times, which results in non-acceptance of the empanelment by private institutions who are major health providers in India at secondary and tertiary care. Referring to data in and , the laparoscopic procedures are having more price difference, and such low priced packages can put quality of service and patient’s safety at stake (Jaffrolet and Jumle Citation2020). With the present prices it raises the question of sustainability of the hospital. A reduction of operating costs by 30–35% by private hospitals to treat patients will be able to accept at least 30% more of the Ayushman Bharat patients, and the occupancy rates can be increased to 85% so that the beds get utilized, achieving a reasonable return on capital employed (National Institute of Public Finance and Policy Citation2019).
From our study, it’s clear that UHC scheme is providing package amount for procedures which accounts to 26–52% of the costs incurred by the private hospitals which can lead to lesser acceptance of the scheme by private hospitals, who are the major health providers in India. We propose a hike of 25% in overall prices offered. The cost to private hospitals in running the day to day operations includes fixed cost like building, rental or lease values, licensing costs, variable costs like medicines and devices, electricity charges, salaries of doctors, transportation. Without upgraded healthcare technology in diagnostics, information technology hospitals cannot become tertiary care, quaternary care centers and cannot become world class. It’s not so easily possible for private hospitals to provide the quality of care at the amount which even does not cover the incurred cost. In one study conducted in India on equipment planning of 250 bed private hospital with all broad specialties, about INR 45 crore has to be kept aside for equipment budget, which would be about 28% of project cost (Naveen et al. Citation2014).
As government healthcare spending in India is only 1.18% of GDP which is far below the other developing countries (WorldBank Citation2022), it can compel the healthcare sector to compromise on the treatment facilities. Tax concessions in the form of exemptions, depreciation margins on equipment, reduced import taxation on equipment can be extended to private institutions at federal government level. State governments at local level should extend support to private hospitals in terms of state taxation exemptions. It is our opinion that, healthcare services that India can provide are directly related to percentage of GDP on India, earmarked for spending on health. More taxes we pay, better is the healthcare. Harvard Gazette published on February 22, 2016 states that money = quality of healthcare. Health inequality based on income is a part of American life (Powell Citation2019). Systematic review of 61 studies yielded results that 34% of studies clearly established positive association between money and the quality of care (Hussey, Wertheimer, and Mehrotra Citation2013). It applies to all countries.
Limitations of the Study
More academic hospitals are not included in study sample, as prices for paying patients offered by these two colleges is lowest in South India.
Price information is deemed sensitive by management of hospitals, hence, more hospitals cannot be studied.
Conclusion
Private hospitals and medical colleges benefit with more footfalls through insurance schemes, but they incur loss due to huge fixed costs and operating expenses to start and sustain with operations. Hospitals are happy to provide care to private insurance companies’ clientele, but, unhappy with the government scheme package prices. A capital-intensive private hospital establishment will find it difficult to provide tertiary care to both paying and scheme population. Support from governments in the form of price hike ranging from 25% to 100% over the current package rates, tax exemptions and price capping of medicines, materials and medical devices will improve operating margins to private establishments. The healthcare financing system exhibits a classical tradeoff between equity and efficiency which must be balanced for it to be successful (Rajesh Kumar and Sheela Prasad Citation2021).
Disclosure Statement
No potential conflict of interest was reported by the author(s)
Additional information
Funding
References
- Andargie, G. 2008. Lecture Notes, 73–74. https://www.cartercenter.org/resources/pdfs/health/ephti/library/lecture_notes/health_science_students/ln_intro_to_health_economics_final.pdf
- Chatterjee, S., C. Levin, and R. Laxminarayan. 2013. Unit cost of medical services at different hospitals in India. PLoS One 8 (7):e69728. Jul 23 doi: 10.1371/journal.pone.0069728.
- FICCI. 2017. https://ficci.in/about-us.asp. Last Accessed October 2021.
- FICCI. 2021. https://ficci.in/ficci-in-news-page.asp?nid=18344. Last updated 18 August 2019. Last Accessed 10 November 2021.
- Frija, G. et al. 2021. How to improve access to medical imaging in low- and middle-income countries? eClinicalMedicine. 38:101034. doi: 10.1016/j.eclinm.2021.101034.
- Hussey, P. S., S. Wertheimer, and A. Mehrotra. 2013. The association between health care quality and cost: A systematic review. Annals of Internal Medicine 158 (1):27–34. doi: 10.7326/0003-4819-158-1-201301010-00006.
- IMA. 2021. https://www.ima-india.org/ima/free-way-page.php?pid=2 Last Updated 18 October 2021. Last Accessed 10 November 2021.
- Jaffrolet, C. and V. Jumle. 2020. Private Healthcare in India: Boons and Banes. November. https://www.institutmontaigne.org/en/analysis/private-healthcare-india-boons-and-banes
- National Health Authority. n.d. Official website of PM-JAY. https://pmjay.gov.in/about/pmjay
- National Health Systems Resource Centre. 2018. National Health Accounts Estimates for India (2015–16). New Delhi, Ministry of Health and Family Welfare, Government of India, 20. https://main.mohfw.gov.in/sites/default/files/NHA_Estimates_Report_2015-16_0.pdf. Published November 2018. Accessed 11 November 2021.
- National Institute of Public Finance and Policy. 2019. Private Hospitals in Health Insurance Network in India: A Reflection for Implementation of Ayushman Bharat, Mita Choudhury and Pritam Datta, National Institute of Public Finance and Policy New Delhi, NIPFP Working paper series No. 254, 19 February.
- Naveen, P. K., H. P. Godhia, N. J. Srinivas, et al. 2014. Insights into equipment planning of a 250-bed hospital project. International Journal of Health Sciences and Research 4 (10):311–21.
- NHM. 2023. https://nhm.gov.in/index1.php?lang=1&level=2&sublinkid=1220&lid=190#:∼:text=There%20are%2010453%20PHCs%20that,24X7%20facilities%20as%20on%2031.12. Last updated February 24.
- Powell, A. 2019. The costs of inequality: Money = quality health care = longer life. [online] Harvard Gazette. https://news.harvard.edu/gazette/story/2016/02/money-quality-health-care-longer-life/. Last Accessed 17 October 2019.
- Rajesh Kumar, S., and J. Sheela Prasad. 2021. Health insurance – Ministry of Health and Family Welfare estimates on health insurance on National Health Accounts data 2013-14. https://www.mohfw.nic.in/sites/default/files/6691590451489562855.pdf Last Accessed on September 19.
- WorldBank. 2022. https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS?locations=IN. Published January 30. Last Accessed August 20, 2022.