Abstract
Blockchain technology enables supply chains to share and distribute data in secured and decentralised environments through validators who trust and validate transactions. The use of blockchain was crucial in the context of the healthcare supply chain (HCSC) during COVID-19, where transactions were secure, and links throughout the supply chain were physically disrupted. Current research has focused on the blockchain application in industry, reviewing its architecture and the mechanisms involved. However, limited empirical studies consider HCSCs and the associated implementation challenges. In this sense, our case study of Indian hospitals has engaged with various stakeholders of the HCSC including clinicians, nurses, doctors, hospital managers, and digital healthcare equipment companies to explore the context to answer the following research questions: (i) What is the impact of the blockchain technology in the HCSC context? and (ii) What are the challenges faced in utilising blockchain technologies in the HCSC? Our findings indicate that the challenges blockchain implementation faced were based on variations in patients’ treatment needs, data storage and privacy, interoperability, digital transformation, technology resistance, training and skills development, resource restraints and capabilities, and supply chain-wide collaboration. The study emphasises challenges for Blockchain in HCSC setting that both practitioners and academics need to be cognisant of.
1. Introduction
Supply chains involve members from initial raw material suppliers to the end customers, while establishing coordination, and collaboration as well as rewiring trust between its partners to compete and withstand disruptions. In order to run a smooth healthcare supply chain (HCSC), the operation adaption of new technologies has become paramount. As each of the supply chain members can serve a multitude of supply chains with varied goals, it becomes difficult to align the supply chain (Bak Citation2016). In this sense, blockchain technology has been viewed as a potential solution by the healthcare providers, as it provides three key benefits: (i) the potential to improve productivity and quality, (ii) increased transparency among parties, and (iii) potential venues for product and process innovation (World Economic Forum Citation2019). Blockchain technology enables supply chains to share and distribute data in a secured and decentralised environment through validators who trust and validate transactions Recently, the COVID-19 pandemic has generated an environment where HCSCs needed to evaluate and address the inefficiencies of the supply chain and find ways to address, improve, and respond to current and potential future disruptions in a rapid manner (Senna et al. Citation2021). With blockchain technology, the resilience of the HCSC can be established, as supply chain-wide data can be accessed to understand the inefficiencies throughout the end-to-end supply chain and to develop, monitor, and innovate strategies to mitigate or tackle the inefficiencies (Sim, Zhang, and Chang Citation2022). Especially within the context of HCSC, this has become imperative, as the disruptions in demand and supply may lead to unintended consequences, such as danger to human life, and would require rapid adjustments by the hospital managers (Riley et al. Citation2016).
Despite the recorded advantages of the worldwide use of blockchain in diverse industrial settings (Li, Lee, and Gharehgozli Citation2023; Van Nguyen et al. Citation2023), Min (Citation2019, 36) stated that ‘many firms are still either sceptical about blockchain’s face value or unfamiliar with its inner workings and application potential.’ Research has mainly focused on the successful application of Blockchain in the context of financial transactions as well as cryptocurrency (Attaran Citation2020; Huang et al. Citation2021; Min Citation2019). Attaran (Citation2020, 1) notes that current research on blockchain in use ‘by the healthcare industry does not adequately address these requirements due to limitations related to privacy, security, and full ecosystem interoperability’ and with the limited implementation calls for assessing the challenges faced in HCSC. Ghadge et al. (Citation2023, 6646) similarly noted that ‘there are concerns that Blockchain interoperability in the healthcare/pharmaceutical system may be challenging’. Current research on the use of blockchain in HCSCs has addressed the decision-making process (Fusco et al. Citation2020; Huang et al. Citation2021); focusing on the use of electronic medical records with clinical data on a large scale (Fusco et al. Citation2020; Khan et al. Citation2021) and the creation of partnerships with pharmacies (Pouye Citation2021) whilst elucidating the implications of blockchain technologies on performance (Park and Li Citation2021) and barriers for blockchain adaption (Saberi et al. Citation2019). Tandon et al. (Citation2020) reviewed for their structured literature review 42 studies that highlighted the need for blockchain implementation in healthcare setting, not only focusing on the platform and its performance but rather holistic implementation of blockchain and its use in healthcare. Similarly, Hermes et al. (Citation2020) focused on the platform as well as the associated digital transformation in the healthcare context. Hence as discussed previously, the assessment of blockchain technology challenges in a healthcare supply chain (HCSC) context extant literature is limited (Hermes et al. Citation2020; Karakas, Acar, and Kucukaltan Citation2021; Riley et al. Citation2016; Sim, Zhang, and Chang Citation2022; Tandon et al. Citation2020) and lacks the implementation in a healthcare setting (Hermes et al. Citation2020; Tandon et al. Citation2020). Our study aims to contribute to the extant literature are threefold: (1) to contribute to the existing body of literature by comprehensively addressing blockchain challenges. Unlike previous works such as Sim, Zhang, and Chang (Citation2022) and Riley et al. (Citation2016), we aim to provide an exhaustive list of challenges, which we will elaborate on in greater detail; (2) to develop a robust conceptual framework for assessing the challenges associated with the implementation of blockchain technology. This endeavour aligns with the recommendations made by Saberi et al. (Citation2019) and Hermes et al. (Citation2020); (3) to bridge a gap in the current literature by conducting an in-depth case study focused on healthcare supply chain challenges. This particular aspect has been relatively underrepresented in the literature, as noted by Attaran (Citation2020) and Hermes et al. (Citation2020). With this aim, the next section will introduce the concept of blockchain technology and its context, followed by the developments in HCSC in terms of blockchain technology usage. We then present the methodology used and a case study from the supply chain of private Indian healthcare providers. We conclude by presenting our findings and indicating directions for future research.
2. Blockchain application in healthcare supply chain context
Hasselgren et al. (Citation2020) stated that the HCSC operations is based upon the triage of health related problem-solving, clinical decision-making, and the realisation and assessment of knowledge-based care provided by a multidisciplinary team for diverse patient needs. The potential to keep and use patients’ lifetime data and electronic record sharing is of interest to healthcare providers (Halamka, Lippman, and Ekblaw Citation2017). Hence, using blockchain, according to Gordon and Catalini (Citation2018, 224), has the potential to improve and reduce the operational time for healthcare providers through ‘five mechanisms: (1) digital access rules, (2) data aggregation, (3) data liquidity, (4) patient identity, and (5) data immutability.’ However, the implementation challenges have not been discussed within healthcare nor its supply chain context (Riley et al. Citation2016; Sim, Zhang, and Chang Citation2022), which has been noted in the literature independently. We argue that the implementation of blockchain in the supply chain context faces the following challenges.
2.1. Challenge 1: variations in patients’ diagnostic needs
Hasselgreen et al. (Citation2020) noted that at its core, healthcare is based upon the patient’s treatment, which can present variations across patients and over time. The challenge is that a patient’s records are kept depending on the time and, thus, can show a variance across time based on the progress in the patient’s health. Moreover, depending on changes in the patient’s health status, the records provide input only across a time period. The size and volume of data and its interpretation across time can also be a challenge for blockchain implementation (Justinia Citation2019), which provides variation across time and across healthcare providers. Hence, we propose the following:
Proposition 1a: Challenges stemming from patients’ individual treatment needs affect blockchain implementation.
Proposition 1b: Challenges stemming from patients’ continuous health changes across time affect blockchain implementation.
2.2. Challenge 2: data storage and privacy
The operations in healthcare revolve around the storage of the data of individual patients, and privacy and trust between supply chain members is important (Hasselgren et al. Citation2020; Martins et al. Citation2019). According to Gordon and Catalini, ‘The first way blockchain technology could improve patient-driven interoperability is through management of digital access rules’ (Gordon and Catalini Citation2018, 227). Blockchain principles can provide increased efficiency in terms of data retrieval, usage, and collaborative work; however, the concern regarding the issues of privacy and data ownership becomes more complex in a supply chain context (Kleinaki et al. Citation2018). A smart contract established with blockchain partners in the supply chain (Hasan et al., Citation2023; Prause and Boevsky Citation2019) provides the opportunity for self-execution, meaning that it creates the conditions for trust and transparency through the supply chain via the process of consolidation, validation, and confirmation (Chang et al. Citation2019; Cole et al. Citation2019). As Govindan et al. (Citation2023, 3513) noted ‘[s]ince blockchain has an open and transparent nature, it can create a climate of trust among the healthcare applications’. This, in turn, improves the data sharing, allays concerns regarding privacy, and allows more streamlined services, such as the automation of payments and an improved cashflow cycle (Prause and Boevsky Citation2019). However, within healthcare, the discussion about privacy and data sharing has been rather problematic. The use of data, data sharing, and data interoperability has given rise to significant concerns not only among the patients but also among members of the HCSC (Justinia Citation2019). Hence, we propose the following:
Proposition 2: Challenges to data storage and privacy have a negative impact on blockchain implementation.
2.3. Challenge 3: system interoperability
The interoperability of systems permits data sharing, which helps improve the accuracy of diagnostics across diverse medical settings from doctors to lab technicians, pharmacies etc. (Zhang et al. Citation2018). The interoperability of the systems allows the accuracy of patients’ diagnostics as well as their treatment (Hussien et al. Citation2019). Considering that blockchain is a distributed technology which is capable to address challenges of data standardisation and system interoperability, and safe electronic health-records accessibility to provide a patient-driven healthcare information systems and technology (Jabbar et al. Citation2020). Therefore, the use of blockchain technology can ease the sharing of information between, for instance, cancer specialists with different expertise to liaise, discuss, and explore treatment options as well as set up plans for treatments (Xie et al. Citation2021). According to Zhang et al. (Citation2018), there are several interoperability-related challenges, one being the use of incompatible software and/or systems, access restrictions in electronic health records (EHR), or the use of multiple platforms ranging from mobile devices to clinic based internal firewall protected environments.
Proposition 3: Challenges stemming from system interoperability may affect blockchain implementation.
2.4. Challenge 4: digital transformation (DT)
Digital transformation refers to ‘a process that aims to improve an entity by triggering significant changes to its properties through combinations of information, computing, communication, and connectivity technologies’ (Hermes et al. Citation2020, 1034). According to Sebastian et al. (Citation2017, 198), ‘Most big old companies’ digital transformations are at an early stage – in most industries, the vast majority of established companies’ revenues still come from traditional products and services.’ In the HCSC digital transformation indicated positive impact upon the operations performance as well as efficient workflow processes (Kraus et al. Citation2021).
Despite the positive outcomes, one of the challenges of system implementation stems from the associated cost and uncertainties involved in costing; as Sunmola et al. (Citation2021, 514) stated, ‘Critical barriers … for digital transformations of supply chains [can] include financial factors’, which are associated also with the level of process reengineering that is needed within the supply chain (Bak Citation2016).
Proposition 4a: Financial constraints can affect blockchain digital transformation.
Proposition 4b: Challenges stemming from process engineering may affect blockchain implementation.
2.5. Challenge 5: technology resistance
Technology resistance has been seen as one of the major supply chain challenges due to issues with the implementation of new technology (Bak Citation2016). Teixeira et al.’s (Citation2023) findings reported that within the HCSCs, staff reluctance is one of the challenges in blockchain implementation. Similarly, the HCSC literature has indicated that inadequate healthcare staff support for the blockchain technology can lead to technology resistance, which can be one of the main implementation challenges (Chong, Blut, and Zheng Citation2022; Kim et al. Citation2023; Oliveira-Dias, Maqueira, and Moyano-Fuentes Citation2022). The technology resistance in the blockchain context also stemmed from the notion that the HCSCs will be relying on third-party providers, where there will be a lack of trust between the supply chain members and the third-party providers (Bak and Papalexi Citation2022; Kassab et al. Citation2019). Especially the technology resistance also may stem from the reported high cost of the systems and the unwillingness of the healthcare provider to cover such a cost (Kassab et al. Citation2019).
Proposition 5: Challenges stemming from technology resistance can affect blockchain implementation.
2.6. Challenge 6: training and skills development
Skills and training are important to any organisation; however, in terms of blockchain, the digital skills seem to be a common dominator requiring the further training of healthcare professionals as well as administrators etc. Although these challenges remain currently, there are more educational settings providing
Blockchain training programs have been increasing recently and are now being offered by some of the nation’s leading universities, including MIT, Princeton, and Stanford. Many blockchain vendors such as Consensys, Blockapps, the Ethereum Foundation, and Hyperledger also provide training programs and certificates. (Kassab et al. Citation2021, 53).
Proposition 6: Challenges with skills and training can affect blockchain implementation in HCSCs.
2.7. Challenge 7: resource restraints and capabilities
One of the challenges faced by blockchain implementation is resource restraints and capabilities (Jiang et al. Citation2018; Kamalahmadi and Parast Citation2016). Similarly, Shukla et al. (Citation2020, 169) noted that supply chain members may refrain from IT investments due to ‘perceived high costs and unclear return on investments’, especially where healthcare providers may have limited resources (Dagher et al. Citation2018; Hasselgren et al. Citation2020). The resource limitations can be based on staff, equipment, and finance, which hinders the development of the necessary capabilities (Bak and Papalexi Citation2022). Similarly, according to Xanthopoulou (Citation2022, 558) ‘the lack of equipment, had a great impact on the adoption and the successful integration of blockchain in the Greek public administration.’ Steele et al.’s (Citation2020) findings indicated especially that in low- to middle-income countries, the technology and its implementation required to be tailored based on the consumption needs, availability of equipment, as well as finances. Hence, we propose the following:
Proposition7a: Challenges with equipment availability can affect blockchain implementation.
Proposition7b: Challenges with staff constraints and capabilities can affect blockchain implementation.
Proposition7c: Challenges with finance can affect blockchain implementation.
2.8. Challenge 8: supply chain wide collaboration
Omar et al. (Citation2021, 37397) noted that ‘HCSC suffers from highly fragmented structures, obsolete processes and systems, and disconnectedness in information sharing among stakeholders’. As the complexity involved is fragmented, it is difficult to generate for blockchain the required degree of collaboration at every level (Bak and Papalexi Citation2022). For example, there are several structures in terms of purchasing, where 90% of US hospitals are members of (Omar et al. Citation2021), creating another layer of complexity. The system’s supply chain-wide collaboration is also dependent upon government regulations as well as the supply chain contextual setting, such as private and public organisation settings (Dagher et al. Citation2018; Hasselgren et al. Citation2020; Omar et al. Citation2021).
Proposition 8: Challenges of supply chain wide collaboration affect blockchain implementation.
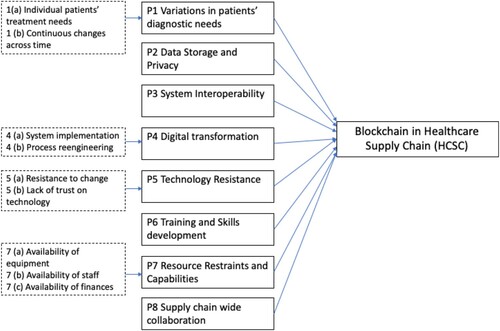
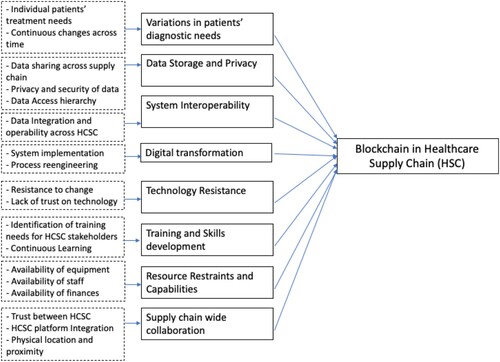
Drawing upon the propositions developed above, we created a conceptual model to represent the effects of challenges on the implementation of blockchain in HCSCs. This is shown in Figure .
3. Case study
This research utilises a case study. According to Yin (Citation2009, 18), ‘A case study is an empirical inquiry that investigates a contemporary phenomenon within its real–life context, especially when the boundaries between phenomenon and context are not clearly evident’. The case study design in this study allowed us the much sought-after in-depth understanding of the challenges supply chain blockchain faces in HCSCs (Senna et al. Citation2021). The case study enabled the empirical grounding for providing an explanation whereby the quality of the research design and the construct validity have been established with multiple sources of evidence (Eisenhardt Citation1989; Voss et al. Citation2002). Within this case study, in-depth interviews with medical consultants, intensive care doctors, and nurses with diverse responsibilities and decision support roles were undertaken, allowing us to evaluate the blockchain challenges from diverse angles (see Table ). Prior to collecting data, full ethical approval was sought and received from the university’s Research Ethics Committee. At the start of each interview, it was confirmed that the interview would be kept anonymous, and during the interview process, the utmost effort was made to create a high degree of trust with the interviewee. A case study was developed based on the emergency centre in Indian private hospitals’ supply chain. To explore the context of blockchain technologies during COVID-19, we propose two research questions: (i) What is the impact of blockchain technology in the HCSC context? and (ii) What are the challenges faced in utilising blockchain technologies in HCSCs? To explore the research questions, focus group discussions and semi-structured interviews were utilised in addition to access to hospital data and government reports.
Table 1. Interviewee roles.
The main steps of conducting the fieldwork in our study can be summarised as follows:
Initial meetings: Meetings were set up with our India project partners, including clinicians, medical doctors, hospital managers, and digital ICU equipment providers, for the delivery of digitally driven ICU services in India to gain access to hospital data and government reports.
Data collection: Researchers spent two and half years collecting data via face-to-face focus groups and interviews on site in India before the start of the pandemic in 2019 and via MS Teams during the pandemic. Data collection strategies included observation in meetings, interviews, and taking notes during focus group discussions with healthcare systems and medical equipment providers and deriving data from documents and from various online sources (e.g. official websites of healthcare (ICU) providers, digital ICU equipment providers, and India’s Ministry of Health & Family Welfare).
The selected cases and interviewees (clinicians, medical doctors, hospital managers, and digital ICU equipment providers) were recommended by our project collaborators. Most of the interviews with clinicians and medical doctors were carried out in 2021 via MS Teams.
In total, we conducted two focus groups with providers of healthcare systems and medical equipment (three managers and directors) and 14 in-depth interviews with ICU clinicians and doctors. In addition, two focus group discussions with digital healthcare equipment companies were carried out. Each interview lasted between 30 and 60 min. It was very challenging to contact and set up interview meetings with ICU doctors, as they are normally extremely busy and were especially busy during the pandemic period. As evident in Table below, our interviewees encompass a diverse spectrum of expertise, ranging from nurses to internists, intensive care specialists, anaesthesiologists, and medical doctors. Their cumulative experience spans a wide range, from 5 to 30 years, providing a comprehensive understanding of the challenges associated with the implementation of blockchain in healthcare. At the initiation of each interview, we assured our interviewees of strict anonymity. Throughout the interview process, we placed paramount importance on establishing a high level of trust with each participant, with a commitment to safeguarding their anonymity and the confidentiality of the interview content.
The Blockchain technology used in the private hospital setting has several layers and helps with the decentralised distribution of information that can be used across the healthcare supply chain (see Figure ). Here the HCSC includes patients (e.g. inpatients, outpatients, and their EHRs), medical team members (e.g. consultants, doctors, nurses, diverse departmental administrators, and insurers), diverse hospitals and laboratories, governmental and regulatory bodies, and blockchain intermediary firms and third-party providers (Fichman, Kohli, and Krishnan Citation2011; Shukla et al. Citation2020).
Figure 2. A figure of Blockchain within the Indian case study HCSC provider setting framework exploring the Blockchain implementation.
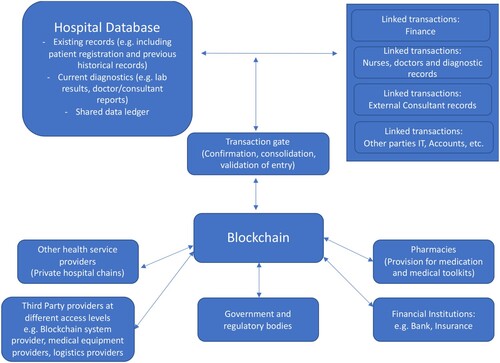
The blockchain technology used in the private hospital setting has several layers, and this helps with the decentralised distribution of information that can be used across the HCSC including the link to payments via bank transfer, the link to pharmacies for prescriptions, the use of patients’ existing EHRs, validation of the diagnostic and critical care including records of nurses, consultants (internal and external), as well as other HCSC parties.
4. Findings and analysis
The blockchain implementation in the Indian healthcare provider was initially attributed to several benefits, such as.
ease of access to data – whereby one interviewee noted, ‘That'll be very helpful in case even if we are shifting the patient from one place to one place, which we are going to CT scan or, like for an MRI or scan and on the way somebody wants to see the patient details … . access about the patient details anywhere’;
the verification process, which provides another layer of security, as each entry will have a time stamp – ‘There is no way of tampering [with] these documents because it comes with a date and time, so it's a record. Once recorded, it is a permanent record, lifelong, so that has made life very much easier for us’;
reduction of processes – one interviewee noted, ‘We had to look into, say, lab investigations or imaging the packs and all that – those who are located in the nursing station. So, every time it was like a back-and-forth from the patient’s bedside to the nursing station. But now I've been able to do away with that because we have a computer on wheels.’ Another interviewee noted that the systems in place can ease the data collection: ‘ … and the data automatically flows into the … our [patients’ records], hospital information systems well – then the nurses need not duplicate the work. Now they, for example, they write on the chart. In addition to that, they must go and enter the notes. All the values you know … .’.
These three main benefits described by the interviewees allow the HCSC operationalisation based upon the triage of health-related problem-solving, clinical decision-making, and realisation and assessment (Hasselgren et al. Citation2020). The blockchain technology used in the private hospital setting has several layers, and this helps with the decentralised distribution of information that can be used across the HCSC including the link to payments via bank transfer, the link to pharmacies for prescriptions, the use of patients existing EHRs, validation of diagnostic and critical care including records of nurses, consultants (internal and external) as well as other HCSC parties (see Figure ). Within the case setting based on our analysis, the following challenges were observed.
4.1. Challenge 1: variations in patients’ diagnostic needs
Proposition 1a: Challenges stemming from patients’ individual treatment needs affect blockchain implementation.
The patient's treatment can present variations due to patients requiring individual treatment involving several supply chain members, which may be different when compared to other patients (Hasselgreen et al. Citation2020). In the case study, the variations of individual patients’ needs resulted in an additional layer of complexity, as the patients’ needs, particularly in ICU, may range from patients that require ‘isolation like infectious patients and protective isolation – patients will be posted in other ICU, like, separate cubicles … . [a]nd other patients who are OK to be like in the main ICU’. The complexity involved in the variations of patients needs can generate a new layer of complexity, Bak and Papalexi (Citation2022) mentioned that fragmentation and complexity involved may create difficulty in generating the required level of collaboration for blockchain at every level.
Proposition 1b: Challenges stemming from patients’ continuous changes across time affect blockchain implementation.
This indicates that variations at a given time can exist between patients’ needs, and thus it also brings a level of unpredictability (Hasselgreen et al. Citation2020). Also, although very helpful in diverse ways, the trends in the use of blockchain technology need to be observed over a time period due to the changing condition of patients’ needs. Similarly, an interviewee noted that some diagnostic tools, such as charts, were difficult to use solely in the digital environment:
We tried getting it onto the electronic medical records because this is the most important part of any ICU because when I go to check on a patient, I need to know how the trend has been over the last couple of hours or the last few days … this capture of the flow chart has not been possible for various reasons.
4.2. Challenge 2: data storage and privacy
Proposition 2: Challenges with data storage and privacy have a negative impact on blockchain implementation.
According to Gordon and Catalini (Citation2018, 227), ‘The first way blockchain technology could improve patient-driven interoperability is through management of digital access rules’. As mentioned earlier, smart contracts established with blockchain partners in the supply chain (Hasan et al., Citation2023; Prause and Boevsky Citation2019) improve data sharing and allay concerns regarding privacy. In addition, they allow more streamlined services, such as the automation of payments, and improve the cash flow cycle (Prause and Boevsky Citation2019). In this case study, the system generated large data sets and detailed records, which are crucially important yet also confidential. However, in the healthcare supply chain in the case study, the interviewees reported that the data was shared across hospitals (including in the private chain) in terms of reference to patient diagnostic and treatment history, financial data etc. This does also provide the opportunity for trust and transparency through the process of consolidation, validation, and confirmation of data as noted by Chang et al. (Citation2019) and Cole et al. (Citation2019). Similarly, the interviewee noted the importance of trust in the system security noting that taking it further to other tools may be beneficial stating that ‘If I were able to have some sort of a secure system that could relay data or the interface itself directly onto my mobile, that would be great’. However, within the healthcare case study, the discussion of privacy and data interoperability has been portrayed as a challenge across HCSC. This finding is also aligned with Peng, Chen, and Wang (Citation2023, 4511) study in which they iterated‘ [i]t is worth examining how stakeholders’ perceived levels of information security affect their willingness to share information via a blockchain application’.
4.3. Challenge 3: system interoperability
Proposition 3: Challenges stemming from system interoperability may affect blockchain implementation.
Data integration and interoperability were available for the provider with individual and departmental access restrictions; this meant availability was limited, with access to levels in some cases requiring internal permission. Another interviewee noted the limitation and use of other technologies that were not embedded in the blockchain: ‘Even if I'm at home, I should be able to monitor the ventilator interface or the hemodynamic interface of all of these patients’. Although it is beneficial to have systems that encourage transparency as highlighted by the interviewee ‘[t]here is no way of tampering [with] these documents … .[o]nce recorded, it is a permanent record, lifelong, so that has made life very much easier for us’ however as seen in the case study this can be a challenge as noted by the interviewee
[w]e … .take calls, so, even when I'm away from the hospital, like, we … I have defined days when I'm on call, so it's usually the registrar who calls me and gives me the, you know, information over the phone. Or sometimes he puts on his WhatsApp video and shows me a couple of things, which is, again, not the ideal thing to be doing.
4.4. Challenge 4: digital transformation (DT)
Proposition 4a: System implementation constraints can affect blockchain digital transformation.
The hospital selected for the case study was a private organisation. In this context, one interviewee noted that there is a difference between the HCSCs in India, stating that there is
the private healthcare sectors, and there is a government sector as well. So, the private healthcare sectors in Bangalore, that is, corporate hospitals, work completely differently compared to the government setups. The care is the same, but the ancillary things are very different.
Proposition 4b: Challenges stemming from process engineering may affect blockchain implementation.
Regarding the move from physical to digital recordings, one interviewee described it as follows:
[Formerly], there was no electronic recording, and all the reports used to be hard copy like X- rays and CT scans - all those things used to be the hard copies, which we keep near the patient’s bedside. Like whenever they come for the rounds, they can take it out and see.
4.5. Challenge 5: technology resistance
Proposition 5: Challenges stemming from technology resistance can affect blockchain implementation.
The technology resistance challenge has been identified as one of the issues for blockchain implementation in HCSCs (Bak and Papalexi Citation2022; Chong, Blut, and Zheng Citation2022; Kim et al. Citation2023; Oliveira-Dias, Maqueira, and Moyano-Fuentes Citation2022). In this case study, although the interviewees acknowledged the benefits of the system, they noted that human interaction is paramount within the HCSC, ‘We can stay without technology. But we can't stay without working hands’. This is also partially because the paper is still used alongside the system. As an interviewee noted,
That is, we are not paperless yet. Of course, in my hospital, the outpatient system is paperless, but the inpatient is sort of a hybrid. There are certain things which we tried making paperless, but we always had a tough time. So, there is paper, and there is digital as well.
I don’t know if everyone is comfortable with that either. There are some people who are having … for that matter, even I feel I am more comfortable with paper quite often. I know things must change; it’s more the attitude, behaviour.
So … we started giving a charge port at the bedside and maybe the computer on wheels next to the patients, so they try to enter all the notes and order entries there, but still, they are reluctant to sit there and do the work. Still, they come to, you know, the main nursing station to do that.
4.6. Challenge 6: training and skills development
In this case study in the context of the Indian setting, IT skills have been seen as the most developed. The interviewee noted,
Some of the time, people [the public] will not be aware of, like, handling computers, but almost all educated staff [such as] … nursing, doctors and the like, those communities might be quite skilful, but … sometimes, there are people who come from the rural areas like the countryside, where even the teaching in nursing education is not computerized in a few of the colleges; it’s like they won't be getting proper access to the computers, or they will not be advanced. Technology depends on … which place … which colleges [we] study at or which area we belong to. Because some will be skilful in handling the computers or advanced technology and gadgets, and somewhere … some … maybe [need to] study.
Proposition 6: Challenges with skills and training affect blockchain implementation in HCSCs.
4.7. Challenge 7: resource restraints and capabilities
Proposition 7a: Challenges with equipment availability affect blockchain implementation.
Our findings suggest the actual systems seem to work well, as reported by the interviewees. However, issues regarding the availability of some equipment were observed, such as the limited availability of laptops. For example, one interviewee noted that other than desktops, there were only four laptops available for the ward rounds, which made the resource allocation when doing the rounds difficult. Also, another issue was system- and software-related challenges, which required updates as well as maintenance. One interviewee commented, ‘They [maintenance and software team] will help us out … in case of any power disconnections or we need any power cords or extra connections’. Another interviewee noted that sometimes downtimes to connectivity can happen: ‘And there is always a central downtime. You know, for various reasons, there is a server downtime and things like that. So, when that happens, like, you're blocked.’ This also highlights that equipment availability needs to be revisited based on consumption needs in HCSCs, which supports the findings of Steele et al. (Citation2020).
Proposition 7b: Challenges with staff constraints and capabilities affect blockchain implementation.
One of the challenges that faced by blockchain implementation is the restraints of resources and capabilities (Jiang et al. Citation2018; Kamalahmadi and Parast Citation2016). This is also highlighted within this case study setting. There seem to be several tasks assigned to the nurses that require the nurses to be able to move swiftly through several supply chain operations relevant to the patients’ needs. Despite the use of the systems, the nurses’ station is seen as the central monitoring desk. One interviewee had observed why this was the case and provided a description of a critical incident:
We had [a specific brand] monitors, for which we had pagers … the alarm goes off when something goes wrong with patients in case saturation comes down, … . It's like there will be an escalation system, like, if we don't respond, it will alert the next level manager, like, maybe nursing staff, then the charge nurse, and then the doctor; like, the three-alarm system needs to be there.
the system entry is set so that the nurse must leave the patient’s side and go through the system and then she has to enter the data, like, whatever we will need to do. So that, maybe, in case the system is quite far away from the patient, it will be quite a hard task for us to leave the bedside and go.
Proposition 7c: Challenges with finance restraints and capabilities affect blockchain implementation.
Steele et al.’s (Citation2020, 78) findings indicated that in low- to middle-income countries, ‘Technology needs to be tailored to the skills and consumption needs’. However, as the case study setting was a private hospital, the finance capabilities of its supply chain for investing technologies were present. Nonetheless, based on the case study, there seems to be a variance between hospitals, as stated by one interviewee: ‘Right now, I'm working in the hospital where we have electronic records and most advanced technologies … right now, like. But there are lots of differences … where some (hospitals) are technologically more advanced than others.’ The interviewees highlighted a distinct contrast between private and public hospitals, emphasising that the adoption and operation of the system were primarily confined to private healthcare institutions. This discrepancy resonates with findings from a study conducted in Greek public administration, where Xanthopoulou (Citation2022, 558) underscored a related concern, stating, ‘The deficiency of equipment significantly impeded the adoption and effective integration of blockchain in the Greek public administration.’
4.8. Challenge 8: supply chain-wide collaboration
Proposition 8: Challenges of supply chain-wide collaboration affect blockchain implementation.
Omar et al. (Citation2021, 37397) noted that ‘HCSC suffers from highly fragmented structures, obsolete processes and systems, and disconnectedness in information sharing among stakeholders’. For example, in this case study, although the technology provided integration across the healthcare providers’ supply chain and eased the critical share of information, sometimes there were still coordination problems within the supply chain. One interviewee noted,
Sometimes the pharmacy might delay medicines. It won't happen routinely, but sometimes they will be short-staffed or something. But we have to give medicines within a specific time limit, so it will be stressed that we have to see, we have to send staff to the pharmacy to get medicines, so such things are quite challenging
There is a central team which considers all of these things, and they are the ones who probably will be directly responsible. So, we are the end-users; we just must state what we want and what our requirements would be. So that gets discussed at a higher level and then we get to see whether it is being implemented or not.
Let's say I'll just … I'll use the ultrasound machine, for example. OK, so this has this Bluetooth device tagged on to it, and then there's a central monitoring system which identifies the movement of this device. So, every time the moment of this device towards a particular bed is identified, it then realizes that the machine is lodged there for a couple of hours or whatever. It is sort of a billing - happens automatically now.
The conceptual framework (Figure ) and the findings and analysis of the propositions presented in the former sections have indicated some additional challenges. Based on these propositions, we devised an updated conceptual framework (see Figure below) for blockchain technology implementation in HCSCs. Our framework introduces new areas of challenges investigated through our analysis to inform HCSC stakeholders. Nevertheless, the updated conceptual framework drawn from theory and the data provides an insight into the complex challenges for blockchain technology implementation in HCSCs (Table ).
Table 2. Summary of findings from the case study.
5. Conclusion
In this paper, we studied and discussed the implementation challenges of blockchain technology in the context of HCSCs in India. A conceptual framework based on eight areas with relevant stakeholders in the HCSC is developed based on our findings. The eight areas of blockchain technology challenges are depicted as variations in patients’ treatment needs, data storage and privacy, interoperability, digital transformation, technology resistance, training and skills development, resource restraints and capabilities, and supply chain-wide collaboration. This study contributed by evaluating the blockchain challenges addressed in the extant literature providing an exhaustive list of challenges which are not fully elaborated upon as addressed by Sim, Zhang, and Chang (Citation2022) as well as Riley et al. (Citation2016); in developing a conceptual framework that highlights the assessment of the challenges of blockchain technology implementation as also suggested by Saberi et al. (Citation2019) as well as Hermes et al. (Citation2020) and lastly by providing an in-depth case study to explore the healthcare supply chain challenges that are currently lacking in the literature (Attaran Citation2020; Hermes et al. Citation2020). Aligned with the three main contributions the theoretical and managerial contributions of the study have been included in detail below.
5.1. Theoretical contribution
The academic literature on blockchain in HCSC has focused on the decision-making process (Fusco et al. Citation2020; Huang et al. Citation2021), the use of electronic medical records with clinical data on a large scale (Fusco et al. Citation2020; Khan et al. Citation2021), and the creation of partnerships with pharmacies (Pouye Citation2021) whilst focusing on the implications of blockchain technologies on performance (Park and Li Citation2021) and barriers for blockchain adaption (Saberi et al. Citation2019) However, this case study examines the context for and assessment of blockchain technology, and identifies the challenges in an HCSC, addresses the contextual setting and the implications thereof, as this was limited in the existing literature (Hermes et al. Citation2020; Riley et al. Citation2016; Sim, Zhang, and Chang Citation2022; Tandon et al. Citation2020). Furthermore, we identified and presented issues that may affect the implementation of blockchain technology in the HCSC context. Our key findings and recommendations include the following:
Blockchain challenges were evident in eight distinctive arenas of the HCSC; however, the challenges were specific and varied across the HCSC. For example, staffing had a particular impact in terms of nurses as the resource. The data access and sharing between hospital and pharmacy had a system-based relevant impact. Hence, adopting a stakeholder-based assessment may be valuable for responding to each challenge.
The development of blockchain technology needs to be aligned with the current existing operation process and needs to address the grey areas, such as the use of non-integrated or recorded tools, including WhatsApp or telephone conversations. This will help HCSC members develop solutions to improve the process of reengineering.
Blockchain technology is affected by the governance structure of hospitals, in this context, public and private HCSCs. It would be interesting to investigate whether other areas of challenges are present in the context of the supply chain of public hospitals.
5.2. Managerial contribution
Our research addresses the Blockchain implementation challenges in the healthcare supply chain (HCSC) in India and provides insights into the policy implications of blockchain adoption in the healthcare sector. In this research context three practical issues have been highlighted for the policy makers which were; (1) Data distribution, security and transparency draw attention to privacy needs and establishment of regulation across the HCSC (Van Dijck et al. Citation2018), (2) In the case of any supply chain disruption (i.e. pandemic) in the HCSCs the benefits and disadvantages of health-relevant data needs to be considered not at the local, national level but also at the international level to enhance healthcare supply chain resilience, (3) lastly there is a concern of data’s validity and reliability and whether an audit trail needs to be embedded at stages needs to be discussed, perhaps not at the HCSC level but specific areas of the supply chain for accurate data collection.
Our findings suggest that blockchain implementation challenges faced were based on variations in patients’ treatment needs; data storage and privacy; interoperability; digital transformation; technology resistance; training and skills development; resource restraints and capabilities; and supply chain-wide collaboration. The Blockchain in HCSC has addressed the decision-making process (Fusco et al. Citation2020; Huang et al. Citation2021); focusing on the use of electronic medical records with clinical data on a large scale (Fusco et al. Citation2020; Khan et al. Citation2021) and creation of partnerships with pharmacies (Pouye Citation2021) whilst these issues are important, the impact of the identified challenges identified in our study need to be assessed on elucidating implications for supply chain resilience across different in the healthcare sector. Hence future studies need to address how the HCSC utilises mechanisms and tools to become more resilient, as resilience has been shown to be a major disrupter in the operation of healthcare as seen in the case of COVID-19.
Acknowledgements
We would like to acknowledge the support of British Council and Indian SPARC (Scheme for Promotion of Academic and Research Collaboration) Impact of Artificial Intelligence on Productivity, Employability and Business Models in Health Care Services.
Data availability statement
The participants of this study did not give written consent for their data to be shared publicly, so due to the sensitive nature of the research supporting data is not available.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors

Ozlem Bak
Ozlem Bak, is a Senior Lecturer in Operations Management at Brunel Business School, UK. Her academic activities are underpinned by industrial and commercial background including experience in the automotive industry for companies such as DaimlerChrysler and Hyundai. Her current research interests lies in supply chain management, particularly organisational transformation, supply chain resilience and e-business implementations in supply chains.
Ashley Braganza
Ashley Braganza, is Dean of Brunel Business School and holds the Chair for Organizational Transformation and co-Director of Brunel’s Centre for AI. His research interests encompass artificial intelligence, big data, change management, strategy implementation, process and knowledge management. His research has been published in academic and practitioner journals. Professor Braganza is the Founder of the British Academy of Management Special Interest Group in Transformation, Change and Development. He has carried out over 50 consultancy assignments with large global organisations.

Weifeng Chen
Weifeng Chen, is a reader in Innovation Management at Brunel Business School. He specialises in technology adoption, business models innovation, digitalisation, and social transformation. His current research focuses on the impact of disruptive technologies such as Artificial Intelligence and Blockchain Technology on innovation related to new business models and ecosystem co-creation in global value chains. He is one of the founding members of the Brunel Centre for AI.
References
- Attaran, M. 2020. “Digital Technology Enablers and their Implications for Supply Chain Management.” In Supply Chain Forum: An International Journal. Vol. 21, No. 3, 158–172. Taylor & Francis.
- Bak, O. 2016. “An Application of the BPCM Model in an e-business Driven Transformation Agenda: Assessing Resource Implications for a European Automotive Multinational Corporation (MNC).” Information Technology & People 29 (2): 334–353. https://doi.org/10.1108/ITP-12-2013-0212.
- Bak, O., and M. Papalexi. 2022. “Understanding the Impact of Covid-19 on Blockchain and upon Sustainable supply chains.” In Proceedings of the 29th International Annual Euroma Conference, Berlin, Germany, 3–6 July, 1–4.
- Chang, S. E., Y. C. Chen, and M. F. Lu. 2019. “Supply Chain Re-Engineering Using Blockchain Technology: A Case of Smart Contract Based Tracking Process.” Technological Forecasting and Social Change 144: 1–11.
- Chong, A. Y. L., M. Blut, and S. Zheng. 2022. “Factors Influencing the Acceptance of Healthcare Information Technologies: A Meta-analysis.” Information & Management 59 (3): 103604. https://doi.org/10.1016/j.im.2022.103604.
- Cole, R., M. Stevenson, and J. Aitken. 2019. “Blockchain Technology: Implications for Operations and Supply Chain Management.” Supply Chain Management: An International Journal 24 (4): 469–483.
- Dagher, G. G., J. Mohler, M. Milojkovic, and P. B. Marella. 2018. “Ancile: Privacy-Preserving Framework for Access Control and Interoperability of Electronic Health Records Using Blockchain Technology.” Sustainable Cities and Society 39:283–297. https://doi.org/10.1016/j.scs.2018.02.014.
- Eisenhardt, K. M. 1989. “Building Theory from Case Study Research.” Academy of Management Review 14 (4): 532–550.
- Farooque, M., V. Jain, A. Zhang, and Z. Li. 2020. “Fuzzy DEMATEL Analysis of Barriers to Blockchain-Based Life Cycle Assessment in China.” Computers & Industrial Engineering 147: 106684.
- Fichman, R. G., R. Kohli, and R. Krishnan, eds. 2011. “Editorial Overview—The Role of Information Systems in Healthcare: Current Research and Future Trends.” Information Systems Research 22 (3): 419–428. https://doi.org/10.1287/isre.1110.0382.
- Fusco, A., G. Dicuonzo, V. Dell’Atti, and M. Tatullo. 2020. “Blockchain in Healthcare: Insights on COVID-19.” International Journal of Environmental Research and Public Health 17 (19): 7167.
- Ghadge, A., M. Bourlakis, S. Kamble, and S. Seuring. 2023. “Blockchain Implementation in Pharmaceutical Supply Chains: A Review and Conceptual Framework.” International Journal of Production Research 61 (19): 6633–6651. https://doi.org/10.1080/00207543.2022.2125595.
- Gordon, W. J., and C. Catalini. 2018. “Blockchain Technology for Healthcare: Facilitating the Transition to Patient-Driven Interoperability.” Computational and Structural Biotechnology Journal 16:224–230. https://doi.org/10.1016/j.csbj.2018.06.003.
- Govindan, K., A. K. Nasr, M. Saeed Heidary, S. Nosrati-Abarghooee, and H. Mina. 2023. “Prioritizing Adoption Barriers of Platforms Based on Blockchain Technology from Balanced Scorecard Perspectives in Healthcare Industry: A Structural Approach.” International Journal of Production Research 61 (11): 3512–3526. https://doi.org/10.1080/00207543.2021.2013560.
- Halamka, J. D., A. Lippman, and A. Ekblaw. 2017. “The Potential for Blockchain to Transform Electronic Health Records.” Harvard Business Review 3 (3): 2–5.
- Hasan, I., M. M. Habib, Z. Mohamed, and V. Tewari. 2023. “Integrated Agri-Food Supply Chain Model: An Application of IoT and Blockchain.” American Journal of Industrial and Business Management 13 (2): 29–45.
- Hasselgren, A., K. Kralevska, D. Gligoroski, S. A. Pedersen, and A. Faxvaag. 2020. “Blockchain in Healthcare and Health Sciences—A Scoping Review.” International Journal of Medical Informatics 134: 104040.
- Hermes, S., T. Riasanow, E. K. Clemons, M. Böhm, and H. Krcmar. 2020. “The Digital Transformation of the Healthcare Industry: Exploring the Rise of Emerging Platform Ecosystems and Their Influence on the Role of Patients.” Business Research 13 (3): 1033–1069. https://doi.org/10.1007/s40685-020-00125-x.
- Huang, S., J. Yang, S. Fong, and Q. Zhao. 2021. “Artificial Intelligence in the Diagnosis of COVID-19: Challenges and Perspectives.” International Journal of Biological Sciences, 17 (6), 1581–1587. https://doi.org/10.7150/ijbs.58855.
- Hussien, H. M., S. M. Yasin, S. N. I. Udzir, A. A. Zaidan, and B. B. Zaidan. 2019. “A Systematic Review for Enabling of Develop a Blockchain Technology in Healthcare Application: Taxonomy, Substantially Analysis, Motivations, Challenges, Recommendations and Future Direction.” Journal of Medical Systems 43 (10): 1–35. https://doi.org/10.1007/s10916-019-1445-8.
- Jabbar, R., N. Fetais, M. Krichen, and K. Barkaoui. 2020. “Blockchain Technology for Healthcare: Enhancing Shared Electronic Health Record Interoperability and integrity.” In 2020 IEEE International Conference on Informatics, IoT, and Enabling Technologies (ICIoT), 310–317. IEEE.
- Jiang, S., J. Cao, H. Wu, Y. Yang, M. Ma, and J. He. 2018. “Blochie: A Blockchain-Based Platform for Healthcare Information Exchange.” In 2018 IEEE International Conference on Smart Computing (Smartcomp), 49–56. IEEE. https://doi.org/10.1109/SMARTCOMP.2018.00073.
- Justinia, T. 2019. “Blockchain Technologies: Opportunities for Solving Real-world Problems in Healthcare and Biomedical Sciences.” Acta Informatica Medica 27 (4): 284. https://doi.org/10.5455/aim.2019.27.284-291.
- Kamalahmadi, M., and M. M. Parast. 2016. “A Review of the Literature on the Principles of Enterprise and Supply Chain Resilience: Major Findings and Directions for Future Research.” International Journal of Production Economics 171:116–133. https://doi.org/10.1016/j.ijpe.2015.10.023.
- Karakas, S., A. Z. Acar, and B. Kucukaltan. 2021. “Blockchain Adoption in Logistics and Supply Chain: A Literature Review and Research Agenda.” International Journal of Production Research, 1–24. https://doi.org/10.1080/00207543.2021.2012613.
- Kassab, M., J. DeFranco, T. Malas, V. V. G. Neto, and G. Destefanis. 2019, May. “Blockchain: A Panacea for Electronic Health Records?” In 2019 IEEE/ACM 1st International Workshop on Software Engineering for Healthcare (SEH), 21–24. IEEE. https://doi.org/10.1109/SEH.2019.00011.
- Kassab, M., G. Destefanis, J. DeFranco, and P. Pranav. 2021. “Blockchain-Engineers Wanted: An Empirical Analysis on Required Skills, Education and Experience.” In 2021 IEEE/ACM 4th International Workshop on Emerging Trends in Software Engineering for Blockchain (WETSEB), 49–55. IEEE.
- Kaur, P., M. Sharma, and M. Mittal. 2018. “Big Data and Machine Learning Based Secure Healthcare Framework.” Procedia Computer Science 132: 1049–1059.
- Khan, H., K. K. Kushwah, S. Singh, H. Urkude, M. R. Maurya, and K. K. Sadasivuni. 2021. “Smart Technologies Driven Approaches to Tackle COVID-19 Pandemic: A Review.” 3 Biotech 11 (2): 11–50https://doi.org/10.1007/s13205-020-02581-y.
- Kim, E. D., K. K. Kuan, M. R. Vaghasiya, J. Penm, N. Gunja, R. El Amrani, and S. K. Poon. 2023. “Passive Resistance to Health Information Technology Implementation: The Case of Electronic Medication Management Systems.” Behaviour & Information Technology 42 (13): 1–22.
- Kleinaki, A. S., P. Mytis-Gkometh, G. Drosatos, P. S. Efraimidis, and E. Kaldoudi. 2018. “A Blockchain-Based Notarization Service for Biomedical Knowledge Retrieval.” Computational and Structural Biotechnology Journal 16:288–297. https://doi.org/10.1016/j.csbj.2018.08.002.
- Koh, L., A. Dolgui, and J. Sarkis. 2020. “Blockchain in Transport and Logistics–Paradigms and Transitions.” International Journal of Production Research 58 (7): 2054–2062. https://doi.org/10.1080/00207543.2020.1736428.
- Kraus, S., P. Jones, N. Kailer, A. Weinmann, N. Chaparro-Banegas, and N. Roig-Tierno. 2021. “Digital Transformation: An Overview of the Current State of the Art of Research.” Sage Open 11 (3): 21582440211047576.
- Li, K., J. Y. Lee, and A. Gharehgozli. 2023. “Blockchain in Food Supply Chains: A Literature Review and Synthesis Analysis of Platforms, Benefits and Challenges.” International Journal of Production Research 61 (11): 3527–3546. https://doi.org/10.1080/00207543.2021.1970849.
- Martins, G. D., R. F. Gonçalves, and B. C. Petroni. 2019. “Blockchain in Manufacturing Revolution Based on Machine to Machine Transaction: A Systematic Review.” Brazilian Journal of Operations & Production Management 16 (2): 294–302.
- Min, H. 2019. “Blockchain Technology for Enhancing Supply Chain Resilience.” Business Horizons 62 (1): 35–45. https://doi.org/10.1016/j.bushor.2018.08.012.
- Munene, D., A. A. Egwar, and J. Nabukenya. 2020. Towards a Digital Health Curriculum for Health Workforce for the African region: A Scoping Review. Last accessed 09.03.2023. https://www.researchgate.net/profile/Andrew-AlunyuEgwar/publication/344769369_Towards_a_Digital_Health_Curriculum_for_Health_Workforce_for_the_African_Region_A_Scoping_Review/links/5f8ea1f4299bf1b53e3488ff/Towards-a-Digital-Health-Curriculum-for-Health-Workforce-for-the-African-Region-A-Scoping-Review.pdf.
- Nunes, P., M. Antunes, and C. Silva. 2021. “Evaluating Cybersecurity Attitudes and Behaviors in Portuguese Healthcare Institutions.” Procedia Computer Science 181: 173–181.
- Oliveira-Dias, D., J. M. Maqueira, and J. Moyano-Fuentes. 2022. “The Link Between Information and Digital Technologies of Industry 4.0 and Agile Supply Chain: Mapping Current Research and Establishing New Research Avenues.” Computers & Industrial Engineering 108000: 1–20.
- Omar, I. A., R. Jayaraman, M. S. Debe, K. Salah, I. Yaqoob, and M. Omar. 2021. “Automating Procurement Contracts in the Healthcare Supply Chain Using Blockchain Smart Contracts.” IEEE Access 9: 37397–37409.
- Park, A., and H. Li. 2021. “The Effect of Blockchain Technology on Supply Chain Sustainability Performances.” Sustainability 13 (4): 1726.
- Patan, R., R. M. Parizi, M. Dorodchi, S. Pouriyeh, and A. Rorrer. 2023. Blockchain Education: Current State, Limitations, Career Scope, Challenges, and Future Directions. Preprint, arXiv:2301.07889.
- Peng, Y., X. Chen, and X. Wang. 2023. “Enhancing Supply Chain Flows Through Blockchain: A Comprehensive Literature Review.” International Journal of Production Research 61 (13): 4503–4524. https://doi.org/10.1080/00207543.2022.2157064.
- Pouye, M. B. 2021. “The Covid-19 Impact on Digital & E-commerce.” Journal of Economics Bibliography 8 (2): 82.
- Prause, G., and I. Boevsky. 2019. “Smart Contracts for Smart Rural Supply Chains.” Bulgarian Journal of Agricultural Science 25 (3).
- Riley, J. M., R. Klein, J. Miller, and V. Sridharan. 2016. “How Internal Integration, Information Sharing, and Training Affect Supply Chain Risk Management Capabilities.” International Journal of Physical Distribution & Logistics Management 46 (10): 953–943. https://doi.org/10.1108/IJPDLM-10-2015-0246.
- Saberi, S., M. Kouhizadeh, J. Sarkis, and L. Shen. 2019. “Blockchain Technology and Its Relationships to Sustainable Supply Chain Management.” International Journal of Production Research 57 (7): 2117–2135. https://doi.org/10.1080/00207543.2018.1533261.
- Sebastian, I. M., J. W. Ross, C. Beath, M. Mocker, K. G. Moloney, and N. O. Fonstad. 2017, September. “How Big Old Companies Navigate Digital Transformation.” MIS Quarterly Executive 16 (3): 197–213.
- Senna, P., A. Reis, A. Dias, O. Coelho, J. Guimaraes, and S. Eliana. 2021. “Healthcare Supply Chain Resilience Framework: Antecedents, Mediators, Consequents.” Production Planning & Control 34 (3): 1–15.
- Shukla, R. G., A. Agarwal, and S. Shukla. 2020. “Blockchain-Powered Smart Healthcare System.” In Handbook of Research on Blockchain Technology, 245–270. Academic Press.
- Sim, C., H. Zhang, and M. L. Chang. 2022. “Improving End-to-end Traceability and Pharma Supply Chain Resilience with Blockchain.” Blockchain in Healthcare Today 5 (231): 1–10.
- Steele, P., Tolani, F., & Subramanian, L. (2020). Aligning Health Supply Chain Maturity with Technology Transfer in Low-and-Middle-Income Countries. Acta Scientific Pharmaceutical Sciences, 4(1). (ISSN: 2581-5423)
- Sunmola, F. T., P. Burgess, and A. Tan. 2021. “Building Blocks for Blockchain Adoption in Digital Transformation of Sustainable Supply Chains.” Procedia Manufacturing 55: 513–520.
- Tandon, A., A. Dhir, A. N. Islam, and M. Mäntymäki. 2020. “Blockchain in Healthcare: A Systematic Literature Review, Synthesizing Framework and Future Research Agenda.” Computers in Industry 122:103290. https://doi.org/10.1016/j.compind.2020.103290.
- Teixeira, L., I. Cardoso, J. Oliveira e Sá, and F. Madeira. 2023. “Are Health Information Systems Ready for the Digital Transformation in Portugal?” Challenges and Future Perspectives. in Healthcare 11 (5): 712.
- Van Dijk, N., A. Tanas, K. Rommetveit, and C. Raab. 2018. “Right Engineering? The Redesign of Privacy and Personal Data Protection.” International Review of Law, Computers & Technology 32 (2-3): 230–256.
- Van Nguyen, T., H. Cong Pham, M. Nhat Nguyen, L. Zhou, and M. Akbari. 2023. “Data-Driven Review of Blockchain Applications in Supply Chain Management: Key Research Themes and Future Directions.” International Journal of Production Research, 1–23. https://doi.org/10.1080/00207543.2023.2253475.
- Voss, C., N. Tsikriktsis, and M. Frohlich. 2002. “Case Research in Operations Management.” International Journal of Operations & Production Management 22 (2): 195–219.
- World Economic Forum. 2019. Building Value with Blockchain Technology: Is Blockchain Worth the Investment? In collaboration with Accenture, Whitepaper. Last access date 02.01.2023. https://www.accenture.com/_acnmedia/pdf-105/accenture-blockchain-value-report.pdf.
- Xanthopoulou, P. 2022. “Blockchain and the Digital Transformation of the Public Sector: The Greek Experience.” Technium Social Sciences Journal 32:558.
- Xie, M., Y. Wei, and Y. Wang. 2021. “Research on Application of Blockchains in Supply Chain Risk Management.” In 2021 2nd International Conference on Computer Science and Management Technology (ICCSMT), 504–509. IEEE.
- Yin, R. K. 2009. Case Study Research: Design and Methods. London: Sage.
- Zhang, P., J. White, D. C. Schmidt, G. Lenz, and S. T. Rosenbloom. 2018. “FHIRChain: Applying Blockchain to Securely and Scalable Share Clinical Data.” Computational and Structural Biotechnology Journal 16:267–278. https://doi.org/10.1016/j.csbj.2018.07.004.