 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
The aim is to examine how mental health is affected by cohabitation and marriage. Individual fixed-effects models are estimated from Norwegian register data containing information about consultations with a general practitioner because of mental health conditions in 2006–19. Mental health, as indicated by annual number of consultations, improves over several years before cohabitation. For those marrying their cohabiting partner, there is a weak further reduction in consultations until the wedding, but no decline afterwards. In other words, formalization of the union does not seem to confer additional mental health benefits. However, marriage may be considered a marker of favourable earlier development in mental health. In contrast, there is further improvement after direct marriage, as well as stronger improvement over the years just preceding direct marriage. Patterns are quite similar for women and men. Overall, the results suggest that the mental health benefits of cohabitation and marriage are similar.
Supplementary material for this article is available at: https://dx.doi.org/10.1080/00324728.2022.2063933. Note: numbers in brackets refer to supplementary notes that can be found at the end of the supplementary material.
Introduction
It is well established that all-cause mortality is higher among the non-married than the married, and in some countries increasingly higher (Kravdal et al. Citation2018). Marriage is also linked to lower mortality from many specific causes (Franke and Kulu Citation2018) and better disease survival (Kravdal Citation2013). Advantages with respect to health, especially mental health, have been documented too (Umberson et al. Citation2013). These relationships likely reflect both causal pathways and uncontrolled joint determinants of marital status and health/mortality (Lillard and Panis Citation1996; Brockmann and Klein Citation2004).
Over the last half century, age at marriage has risen in many countries, along with an increase in the proportions never marrying. At the same time, consensual unions—which tend to be less stable—have become more common (Sobotka and Toulemon Citation2008; Sassler and Lichter Citation2020). We would expect consensual unions to affect health and mortality through the same mechanisms as marriage, although perhaps not as strongly. However, comparisons between those who are cohabiting and those who have married—directly or after cohabitation—have shown quite mixed results, and the observed differences are difficult to interpret because they are partly a result of selection, like the differences between formal marital status groups.
The goal of this study is to provide a more detailed picture of the link between cohabitation, marriage, and mental health than in earlier research. The analysis is, like some other recent studies, based on individual fixed-effects models. Thus, unobserved time-invariant individual characteristics that may affect the choice of living arrangement as well as health are controlled for. Register data for the entire Norwegian population from 2006 to 2019 are used, and the outcome variable is the annual number of consultations with a general practitioner (GP) where a mental health condition is one of the reported diagnoses. With such a large data set, it is possible not only to study differences in mental health between married and cohabiting individuals, but also to examine in detail how mental health varies over time, before and after entry into cohabitation or marriage. The analysis is structured as follows: First, we describe the trends in mental health before cohabitation (when a romantic relationship is established). This has not been done previously, although a few studies have covered trends in well-being before marriage. We distinguish between individuals who later marry and those who do not. The development in mental health between entry into cohabitation and marriage, as well as after marriage, is then analysed. Finally, we compare the patterns before and after marriages preceded by cohabitation with those before and after direct marriages (which are less common these days). The differences between these types of marriages have received little attention in earlier fixed-effects investigations. We focus largely on first unions and distinguish between marriages that remain intact and those ending in separation, divorce, or spousal death. Given the possibility that the health effects of intimate relationships vary by sex (e.g. Simon Citation2002; Roelfs Citation2011; Shor et al. Citation2012a, Citation2012b), the analysis is sex stratified.
The Norwegian setting
The trend towards a lower proportion married and a higher age at marriage has been particularly strong in Nordic countries but has to a large extent been set off against a rise in consensual unions (Prioux Citation2006; Sobotka and Toulemon Citation2008; Sánchez Gassen and Perelli-Harris Citation2015; Härkönen et al. Citation2021). The latter are less stable (Liefbroer and Dourleijn, Citation2006; Poortman and Lyngstad Citation2007; Musick and Michelmore Citation2018), and many Nordic couples have children while living in such unions (Perelli-Harris et al. Citation2010). In 2017–19, 37 per cent of Norwegians aged 30–34 years were cohabiting and 37 per cent were married (Statistics Norway Citation2021a). The corresponding proportions at age 45–49 were 21 and 57 per cent, respectively. In comparison, in 1993–95, 24 per cent of 30–34-year-olds were cohabiting and 53 per cent married, while at age 45–49, 8 per cent were cohabiting and 77 per cent married. Only 65 per cent of 40–49-year-olds in 2021 had ever married, as opposed to 92 per cent in 1986 (Statistics Norway Citation2021b).
People who perceive the gains from living in a union as relatively small are, of course, also less likely to form a union, and if they do, they may prefer an informal one that is easier to dissolve and felt to be less of a commitment (Kravdal Citation1999). Thus, the particularly pronounced shift away from marriage in Nordic countries may be a result of factors that make partnership less important, including a generous welfare state (Baran et al. Citation2014). Another key argument in couples’ decision-making may be whether cohabitation also provides other advantages compared with marriage or is at least clearly not disadvantageous. According to that perspective, the observed patterns may fit well with Nordic cohabitants’ notion of their partnership being almost the same as marriage (Hiekel et al. Citation2014), perhaps partly because of the relatively small difference in legal rights (Sánchez Gassen and Perelli-Harris Citation2015). Finally, the generally liberal values in the region may have contributed to making consensual unions common.
If cohabitation is more similar to marriage in Nordic countries than elsewhere, it may also be particularly unlikely that the married enjoy a health advantage compared with cohabitants. In support, Soons and Kalmijn (Citation2009) found the smallest differences in well-being between married and cohabiting couples in Nordic and other countries where cohabitation is common and widely accepted.
The current state of knowledge
Marriage, health, and mortality
The well-documented health and survival advantages for the married probably result partly from various protective effects of having a spouse. For example, there may be economic benefits because of scale advantages or (more relevant in the past) specialization (Hahn Citation1993; Ross Citation1995; Wilmoth and Koso Citation2002). Spouses also exert control over each other’s behaviour (Lewis and Butterfield Citation2007), with implications for several lifestyle factors (Lee et al. Citation2004; Duncan et al. Citation2006; Ali and Ajilore Citation2011; Averett et al. Citation2013). Additionally, spouses typically provide companionship and practical and emotional support (Ross Citation1995). This may also contribute to a healthy lifestyle, in addition to making it easier to recover from disease. Furthermore, research has suggested that emotional closeness not only has these kinds of practical implications but has even more direct physiological effects (Kiecolt-Glaser Citation2018; Uchino Citation2018). Another possible benefit from marriage is that a spouse may help to increase the social network. However, marriage may also be burdening, not least if the partner is in poor health or the relationship quality is low. The latter would likely weaken the social control and support and also have other adverse effects (Robles et al. Citation2014).
The married are also more likely than the non-married to have children, who can influence their parents’ lives both favourably and adversely through various social mechanisms (Umberson et al. Citation2010; Kravdal et al. Citation2012). Additionally, for women, there are positive as well as negative physiological effects of childbearing (Kravdal et al. Citation2020a, Citation2020b).[1]
As mentioned, the observed relationships between marital status and health/mortality reflect both selection and causal effects (Lillard and Panis Citation1996; Brockmann and Klein Citation2004). For example, health, education, income, and lifestyle preferences have impacts on individuals’ chances of marrying and remaining married and also affect their later health and mortality. In practice, it is very difficult to control well for this.
Possible reasons for different effects of cohabitation and marriage on health
Cohabitants may, like the married, benefit from a partner’s support and social control over health behaviour, and from economies of scale. However, the advantages may be smaller if cohabitants live more separate lives and/or their relationship quality is lower. The latter—which may be both a reason for not marrying and a result of smaller investments in the relationship—has been suggested in some investigations (Wiik et al. Citation2012; Brown et al. Citation2017). Consistent with this idea of lower quality, it has been reported that people tend to think of consensual unions as less of a commitment and less stable than marriages (Brown Citation2000; Perelli-Harris et al. Citation2014; Stanley et al. Citation2004), and it has been documented that the dissolution rate is considerably higher for cohabiting couples, even when couples with children are compared. With respect to the related issue of separate lives, some authors have shown that cohabitants pool incomes to a lesser extent than the married (Lyngstad et al. Citation2011; Eickmeyer et al. Citation2019; Pepin Citation2019), less often own a house jointly (Thomas and Mulder Citation2016), and receive less support from each other and from broader family (Eggebeen Citation2005; Marcussen Citation2005), although there is also evidence suggesting no differences in social support (Ross Citation1995). A lower level of social control among cohabitants because of more separate lives may lie behind the smaller impact of cohabitation than marriage on risky health behaviour reported in some studies (Horwitz and White Citation1998; Marcussen Citation2005; Duncan et al. Citation2006; Joutsenniemi et al. Citation2007; Ali and Ajilore Citation2011).
To the extent that cohabitation involves less pronounced economies of scale and less social control and support than marriage—with potential implications for health and mortality—marrying directly rather than entering cohabitation may provide health advantages, and it may also be favourable for cohabitants to marry. However, the health outcomes for cohabitants who marry will not necessarily be the same as for those marrying directly. Outcomes will depend on whether the aforementioned factors, such as the inclination to live separate lives, are affected not only by current cohabitation but also by earlier cohabitation experience, of which there is little knowledge. They will also depend on the extent to which individuals’ health during years spent cohabiting rather than single has implications for their later health.
In any case, observed differences in lifestyle, health, and mortality between cohabitants and the married do not only reflect causal effects of the choice of living arrangement: low education, a poor economic situation, not having a child, individual values, social norms, and several other factors may steer people into cohabitation (Kravdal Citation1999; Sassler and Lichter Citation2020)—through relationship quality or other channels [2]—and also affect lifestyle, health, and mortality.[3] In this investigation, we take constant unobserved factors (such as aspects of people’s value orientations) into account through the fixed-effects approach, while explicitly controlling for some time-varying factors (in parts of the analysis).
Existing evidence of differences in health
As expected, most studies have indeed shown lower mortality for married than cohabiting individuals, at least in some population groups (Koskinen et al. Citation2007; Drefahl Citation2012; Liu and Reczek Citation2012).[4] When the focus is instead on health or well-being, some investigations have shown no marriage advantage when social background factors are controlled for (Mastekaasa Citation1995; Perelli-Harris et al. Citation2018; Perelli-Harris and Styrc 2018), while the advantage survives such controls in others (Kim and McKenry Citation2002; Marcussen Citation2005; Hansen et al. Citation2007; Soons and Kalmijn Citation2009; Perelli-Harris et al. Citation2019).[5] In some investigations, there are no differences between married and cohabiting people even according to the simplest models (Ross Citation1995; Joutsenniemi et al. Citation2006). A few authors have compared those who marry after cohabitation and those who marry directly, with mixed conclusions. For example, while Lamb et al. (Citation2003) found better outcomes for the latter, Horwitz and White (Citation1998) did not see any difference.
In some of these studies, the selection into cohabitation or marriage was dealt with by controlling for earlier measurements of the outcome variables (Horwitz and White Citation1998; Brown Citation2000; Kim and McKenry Citation2002; Lamb et al. Citation2003). Other investigations addressing the difference between married and cohabiting people have instead been based on individual fixed-effects analysis, also with varying conclusions. For example, some authors have found that cohabitation and marriage (directly or via cohabitation) have largely the same favourable impact on health or well-being—although with some variation across outcomes or social groups (Wade and Pevalin Citation2004 [mental health, UK]; Zimmermann and Easterlin Citation2006 [well-being, Germany]; Musick and Bumpass Citation2012 [mental and physical health and well-being, United States]; Kohn and Averett Citation2014 [general health, UK]; Næss et al. Citation2015 [well-being, Norway]; van Hedel et al. Citation2018 [mental health, Finland]).[6] The results in other investigations tilt towards a marriage advantage (Stutzer and Frey Citation2006 [well-being, Germany]; Soons et al. Citation2009 [well-being, the Netherlands]; Blekesaune Citation2018 [well-being, UK]; Chen and van Ours Citation2018 [well-being, the Netherlands]), at least for some of the outcomes (Kalmijn Citation2017 [mental and physical health and well-being, Switzerland]). Some authors have explicitly compared the directly married with those marrying after a period of cohabitation and concluded that the effect of these two types of transitions is the same (Soons et al. Citation2009; Musick and Bumpass Citation2012). In a study of health outcomes and health behaviour in Canada, Averett et al. (Citation2013) found that cohabitation tended to be less beneficial than marriage, but also—in some cases where marriage appeared to be disadvantageous—less harmful. Wu and Hart (Citation2002), who estimated difference models that corresponded to fixed-effects analysis, concluded that there was no effect of either marriage or cohabitation on mental and physical health in Canada. In a study of the transition from cohabitation to marriage in Germany, Gattig and Minkus (Citation2021) found a higher level of well-being associated with marriage.
Although these fixed-effects analyses are very valuable, they also have weaknesses. For example, some were based on only two observations two or six years apart (Wu and Hart Citation2002; Musick and Bumpass Citation2012) or on few individuals (Musick and Bumpass Citation2012). In other studies, no distinction was made between direct marriage and marriage after cohabitation or between cohabitation that led to marriage and cohabitation that did not (Wu and Hart Citation2002; Wade and Pevalin Citation2004; Stutzer and Frey Citation2006; Kohn and Averett Citation2014; Næss et al. Citation2015; Kalmijn Citation2017; Blekesaune Citation2018; Chen and van Ours Citation2018; van Hedel et al. Citation2018).
The importance of time since entry into cohabitation or marriage has been addressed in some fixed-effects investigations, which suggest adverse development in health or well-being with increasing time in the relationship (in line with the ‘set point theory’ about adaptation back to the earlier level; Diener et al. Citation2006) rather than a lasting accumulation of advantages. However, the effect of time since union formation or marriage has in most cases been assumed to be linear or log-linear (Soons et al. Citation2009; Kalmijn Citation2017), or there has been only a crude distinction between 0–3 vs 4–6 years (Musick and Bumpass Citation2012) or one vs two or more years (Zimmermann and Easterlin Citation2006). Furthermore, most research has not checked whether time since cohabitation and time since marriage have different effects (Soons et al. Citation2009; Musick and Bumpass Citation2012; Kalmijn Citation2017). An exception is the analysis by Blekesaune (Citation2018), which included a dummy for the first year and two slopes for the subsequent years, as well as interactions with type of union.
A few authors have considered the development in health or well-being before marriage (over quite a short period or in little detail) and interpreted the improvement as an impact of being in a relationship [7] or even a consensual union (Lucas et al. Citation2003; Stutzer and Frey Citation2006; Frijters et al. Citation2011; Quari et al. Citation2014; Tao et al. Citation2019). If there is a steady improvement over several years before marriage but some of these years are pooled together as a ‘premarital’ reference period, the estimated effect of marriage will depend on the number of years chosen (Quari et al. Citation2014; Grover and Helliwell Citation2019). The period up to a union of any type (marriage/cohabitation) has also been analysed (Blekesaune Citation2008), but changes specifically over the pre-cohabitation years were not examined. Doing so would capture the potential health effect of being in a romantic relationship that leads to a consensual union (and perhaps marriage) and thus would provide a more complete picture of the benefits associated with cohabitation.
Norwegian studies
The variation in findings is, of course, partly a result of differences in analytical approach. Additionally, it may reflect the different settings and we might expect the advantage of marriage compared with cohabitation to be smaller in Norway than in many other countries. However, the few studies carried out in Norway do not provide clear indication of this; the evidence is as mixed as that from other countries: one cross-sectional analysis showed an advantage for the (first-time) married (Hansen et al. Citation2007), while another showed no such pattern (Mastekaasa Citation1995). Similarly, one of the fixed-effects analyses pointed towards a marriage advantage (Blekesaune Citation2018), while another concluded that cohabiting women (but not men) were actually in better health than the married (Næss et al. Citation2015). Studies from other Nordic countries also vary: some suggest a health advantage for the married (Koskinen et al. Citation2007; Drefahl Citation2012), while no advantage appears in others (Joutsenniemi et al. Citation2006; van Hedel et al. Citation2018).
Data and methods
Data sources
Our key data sources are the Norwegian Population Register and the KUHR register (the Norwegian Control and Distribution of Health Reimbursement Database), the latter with information about primary healthcare usage reported by GPs since 2006 so they can be reimbursed by the state.[8] The data extractions made for this analysis cover the period up to 2019.
All individuals who have lived in Norway for some time after 1964 are included in the Population Register and assigned a personal identification number (PIN) that is also used in other registers. The Population Register contains information about individuals’ marital and cohabitation status on 1 January each year, from 2005 onwards (Falnes-Dalheim Citation2009). For earlier years, back to 1975, the register includes information only about marital status. PINs of spouses and cohabiting partners are also included. Additionally, there is annual information on whether the person lived in Norway on 1 January and, for the cohorts included in this study, the number of children a person has had at any point in time.[9]
The outcome variable in this study is the annual number of face-to-face GP consultations between 2006 and 2019 where a mental health condition (codes P70–P99 in the ICPC-2 system) was recorded as a diagnosis. We restrict the analysis to adults aged 18–59 [10], so only data for those born between 1947 and 2001 were extracted from the registers.[11] The analysis includes a series of annual observations for each person in these cohorts. This series (or study period) runs from the ‘first year of observation’ (FYO) to the ‘last year of observation’ (LYO). FYO is 2006 (the first year with information on GP consultations) or, if the person did not live in Norway on 1 January 2006, the first year after 2006 with residence in Norway on 1 January. LYO is 2019 (the last year covered by the data) or the last year after FYO before the first occurrence of 1 January when the person no longer lived in Norway.
In addition to the information from these two registers, some of the analysis is based on annual information from Statistics Norway on income (sum of labour income, entrepreneurial income, capital income, pensions, and some benefits, minus tax-deductible amounts), school enrolment, and highest educational level achieved.
Details about the partnership transitions
Most of the investigation focuses on three transitions among individuals for whom no earlier dissolution is reported in the data (note, however, that the data do not include information about dissolutions of consensual unions before 2005). Without such a limitation to first unions, the cohabitants might include relatively many with dissolution experience (De Jong Gierveld Citation2004), which is itself linked with poorer health and higher mortality (Hughes and Waite Citation2009; Sweeney Citation2010; Berntsen and Kravdal Citation2012). However, some models are also estimated separately for those we know have dissolved an earlier relationship.
The first transition is from single to living in a consensual union (and is referred to as SC); the number of years since union entry is the time variable. The analysis of this transition includes all individuals who made the transition between FYO and the year before LYO (note that there is insufficient information about transitions in LYO because the status in the next year is unknown) or in 2005 if FYO is 2006 and the person lived in Norway on 1 January 2005 (the first year with information on both cohabitation and marital status).[12] Special analysis is done for the subgroups whose union dissolved later in the study period (except in LYO) or who married their cohabiting partner. (For simplicity, this period excluding LYO is also referred to as the study period in some parts of the text.)
The second transition is from cohabitation to marriage (SCM), and the analysis includes those in the SC analysis who married during the study period (except in LYO). The time variable is years since marriage. Separate analysis covers those whose marriage remained intact until at least the beginning of LYO and those who experienced separation, divorce, or spousal death. Models are also estimated separately according to the interval between entries into consensual union and marriage.
The third transition is from single to married (SM), and years since marriage is the time variable. This analysis includes those who married directly during the study period (except in LYO) or in 2005 if FYO is 2006 and the person lived in Norway on 1 January 2005.[13] Some of the analysis is conditional on whether the individual remained married until at least the beginning of LYO.
Details about how the transitions are identified from marriage and cohabitation histories as well as the partner’s PIN can be found in the supplementary material (Appendix 1).
Statistical model
The goal is to assess the effects of being married or cohabiting on a health outcome (Y), but let us now simply assume that the interest is in the effect of being (ever-)married rather than never-married (M). In a cross-sectional analysis, a model would typically be estimated based on one measurement of marital status for each individual, with controls for factors suspected to be joint determinants of Y and M. The data needed for perfect control will in practice never be available. An alternative would be to undertake a fixed-effects analysis and thus control at least for all unobserved time-constant factors. More specifically, the following model could be estimated for those who are never-married at the beginning of the observation period but marry in a later year:
(1)
(1) where Yit is the outcome for person i in year t, Mit is a dummy variable for married vs never-married, νi are individual fixed effects, and ϵit are individual- and year-specific error terms. Time-varying control variables can also be included, but we ignore them for now. With such a model, the estimate of the effect of marriage comes from comparing outcomes before and after marriage for the same person, assuming that the period before marriage represents the counterfactual (i.e. the outcome for the person if they had not married). This effect of marriage among those who have married, sometimes referred to as a ‘treatment effect on the treated’, is not necessarily the same effect as marriage would have had if those who did not marry had done so. This issue is returned to later.
In this study, a model such as (1) is estimated but with several extensions. Instead of a marriage variable that distinguishes between married and never-married, we include a multi-category variable representing time since marriage (in the SCM and SM analyses) or since entry into cohabitation (in the SC analysis). More specifically, there are 20 dummies, , corresponding to year k since marriage or start of cohabitation, where k (in most of the analysis) runs from ≤−10 to −1 years before the transition and from 1 to ≥10 after it.[14] The transition year is the reference category (i.e.
= 0). Additionally, a vector of age dummies for one-year age categories, Ait, is included to take into account that: (1) individuals tend to be older after marriage or cohabitation than before; and (2) the number of GP consultations in a certain year is likely influenced by age in that year.
Thus, the model is:
(2)
(2) However, in such models, where both current age and variables for time since marriage or start of cohabitation are included (e.g. as in Kalmijn Citation2017), a linear dependence problem arises: current age minus time since transition equals age at transition. This is the same for all observations and can be seen as part of the individual fixed effect. As in corresponding analyses by Blekesaune (Citation2008) and Anusic et al. (Citation2014), we deal with this problem by estimating model (2) from data for those who made the transition (as described in the previous subsection) plus one-year observations for each year from FYO to LYO for those who were single on 1 January each of these years. All the M dummies for time since the event are set to zero for the latter, who are referred to as the ‘age control group’ and contribute only to the estimation of the age effect. The underlying assumption is that the age effect is the same in the age control group as among those experiencing the event. More detailed explanations of the linear dependence problem are given in the supplementary material (Appendix 2).
In a final step, the following time-varying variables (referring to the individual under study, not the couple) are added to the model: number of children, whether enrolled in education on 1 October the previous year, educational level at that time, and income for the previous year. The variables are allowed to have different effects for those who experienced the transition and those who remained single.[15] However, the causal direction of the links between cohabitation/marriage and these variables is ambiguous: they may affect the chance of being in a romantic relationship and forming a union but may also be influenced by this process, partly via each other. Therefore, it is not obvious whether the results from such a model (presumably involving ‘over-controlling’) are more useful than those from a model where they are not included (‘under-controlling’). In this case, the results are quite similar, which makes the choice between the two alternatives less important. The estimates from the simpler model are (quite arbitrarily) given most attention and presented in the main text, while the estimates from the more complex model are presented in the supplementary material.
Model estimation is carried out using the xtreg command in Stata, with robust standard errors clustered at the individual level.
Even though the fixed-effects analysis is widely regarded as a good approach for this kind of investigation, there are remaining problems. One of them is that the estimated effects may partly reflect effects of health on union formation. This has been ignored in most earlier studies, where a common argument is that the individual fixed effects capture people’s general health or satisfaction. However, health and satisfaction vary over time, making reverse causality a relevant concern even when fixed effects are included. Given the lack of attention to this issue, we illustrate, through a simulation experiment, how reverse causality may produce bias (supplementary material, Appendix 3). This occurs not only when time since entry into cohabitation or marriage is considered, as here, but also when simply distinguishing between cohabiting/married or not. In particular, we show that a decline in mental health consultations until the start of cohabitation, according to a fixed-effects model, may be partly a result of reverse causality. We also explain that a good idea of the magnitude of reverse causality bias cannot be obtained by estimating a model for how mental health influences the chances of entering cohabitation or marriage (as in Chen and van Ours Citation2018) and that the reverse causality problem is not solved by just adding the outcome in a previous year to the fixed-effects model for mental health (as in Grover and Helliwell Citation2019).[16] Nor can the reverse causality problem be solved by estimating a multiprocess model with a set of equations for entry into cohabitation or marriage and one equation for mental health (e.g. models such as used by Steele et al. Citation2009; Mikolai and Kulu Citation2018).[17]
Results
The numbers of observations in all analyses are shown in . The distribution over the time variable is shown for the SC analysis (as an example) in the supplementary material (Appendix 4), along with the variation in the average number of GP consultations across all independent variables in the SC, SCM, and SM analyses.
Table 1 Numbers of observations in the different analyses for individuals with no earlier dissolution experience: Norway, 2006–19
Entry into cohabitation (SC)
The number of annual GP visits falls for both women and men during a period of about seven years before the start of a consensual union that is (as far as we can tell) the first such union (solid line, , where the scales are different for women and men; Tables A2.1 and A5.1, supplementary material). There is no further decline after union entry. The downward trend is particularly sharp among women, and that is also the case if we take into account that women generally consult GPs for mental health conditions more often than men (by dividing the outcome variable by the sex-specific average or standard deviation across all observations in the SC analysis, including the age control group (not shown)).
Figure 1 Effects of time since entry into consensual union on annual number of GP visits because of mental health conditions: women and men with no earlier dissolution experience who entered a consensual union within the study period, Norway, 2006–19
Note: GP visits on the y-axis is the difference in annual number of GP visits compared with the year when cohabitation started. Vertical bars show 95 per cent confidence intervals.
Source: Authors’ analysis of data from Norwegian Population Register and KUHR register.
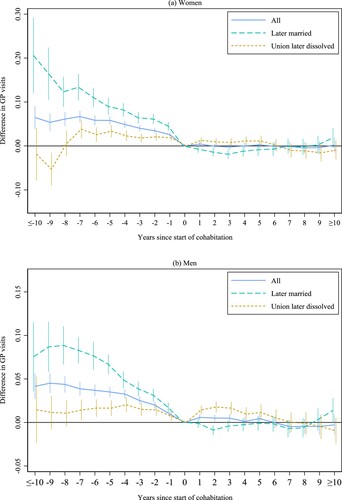
If only the relatively large proportion of the unions that later dissolve are considered (short-dashed line, ), the reduction in GP visits before cohabitation is much weaker, and there is an upturn afterwards, reflecting the relatively large number of GP visits for some years before and after a dissolution (discussed further later). The trend is quite different for those who later marry their cohabiting partner (long-dashed line): a particularly sharp reduction in GP visits before the start of cohabitation is followed by a small further reduction for a couple of years, and then a slight increase.[18]
Further analysis of marriage among cohabitants (SCM)
The next step is to consider cohabitants who marry but to change the key variable to time since marriage (to learn more about the changes around marriage and compare with direct marriage). As we would expect, given the analysis just reported, the number of GP visits declines over many years before marriage, although—especially for women—somewhat less markedly during the last couple of years than further back in time (solid line, ; Table A5.2, supplementary material). When a similar analysis is done for those who marry one, two, three, four, five, or six years after the start of cohabitation (, with circles marking the start of cohabitation), there are only a few examples of significant decline in GP visits from union entry to marriage. However, the point estimates suggest a downward trend or in some cases (among women and especially those with several years between the two transitions) a U shape.[19]
Figure 2 Effects of time since marriage on annual number of GP visits because of mental health conditions: women and men with no earlier dissolution experience who entered a consensual union and then married their cohabiting partner within the study period or who married directly, Norway, 2006–19
Note: GP visits on the y-axis is the difference in annual number of GP visits compared with the year when marriage started. Vertical bars show 95 per cent confidence intervals.
Source: As for .
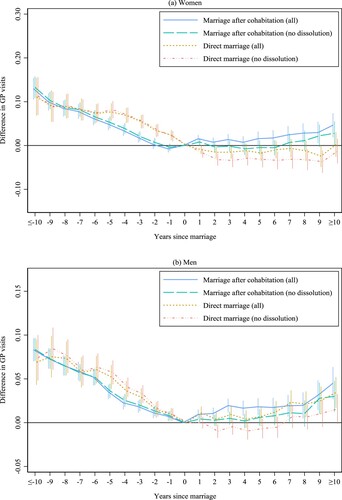
Figure 3 Effects of time since entry into marriage on annual number of GP visits because of mental health conditions: women and men with no earlier dissolution experience who entered a consensual union and then married their cohabiting partner within the study period, Norway, 2006–19
Note: GP visits on the y-axis is the difference in annual number of GP visits compared with the year when marriage started. Vertical bars show 95 per cent confidence intervals. Circles mark start of cohabitation.
Source: As for .
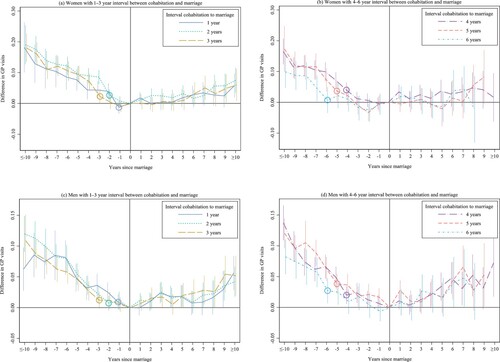
An increase in GP visits appears after marriage when all individuals are pooled together regardless of the timing of the events (solid line, ) and, on the whole, the estimates point in the same direction when models are estimated separately for those who marry after one, two, three, four, five, or six years (). If the analysis is conditioned on remaining married throughout the study period (long-dashed line, ), there is a less clear upturn after marriage as expected; a significant increase appears only at the end of the study period (when some marriages may be troubled and later dissolve).
Among those whose marriage dissolve later in the study period, there is a sharp increase in GP visits immediately after marriage and little evidence of premarital decline (Figure A4, supplementary material). Stated differently, a less favourable development in mental health before marriage appears to be predictive of marital dissolution (largely separation or divorce, not spousal death, at the ages considered here).[20] This is itself an interesting finding, but not dealt with further in this paper.
Let us now return to the decline in GP visits between entry into cohabitation and marriage and find out whether people who marry after, say, two or four years of cohabitation then have experienced a greater decline since the start of cohabitation than those who are still cohabiting after two or four years. To do so, we need to consider again time since start of cohabitation (rather than marriage). According to the point estimates, women—but not men—who marry two or four years after starting to cohabit experience a decline in GP visits over those years that is larger than among those who are still cohabiting after two or four years, although the differences are not significant (). A similar pattern appears with other durations of cohabitation before marriage among women (not shown). Furthermore, and as expected from , those who marry after two or four years (), or after another period (not shown), experience a more favourable development before cohabitation than those who are still cohabiting at that time.[21] However, those who marry do not seem to experience greater decline or less increase in GP visits later.[22]
Table 2 Effects of time since entry into consensual union on annual number of GP visits for mental health conditions, among individuals with no known earlier dissolution experience who entered a consensual union within the study period (SC and SCM groups): Norway, 2006–19
Direct marriage (SM)
The decline in GP visits is sharper in the last few years before a direct marriage than before a marriage preceded by cohabitation (; Table A5.3, supplementary material). This is seen most clearly among women. Women marrying directly also experience further decline for a couple of years after marriage, in contrast to the increase among those marrying after cohabitation. Among men who marry directly, there is a delayed upturn afterwards compared with those who marry after cohabitation. Comparison of the trend over several years before and after marriage suggests that those who proceed directly from single to married, especially women, experience a larger decline in GP visits in the long run than those who marry via cohabitation.
These patterns are not a result of different dissolution risks, because similar patterns are seen when the focus is on those who remain married throughout the study period, who generally experience slightly more decline in GP visits before marriage and less increase or more decline afterwards (). Also in this group, the development is more favourable before and after a direct marriage than around a marriage preceded by cohabitation (and a decline in GP visits after direct marriage is seen also among men, not only women).
For those whose direct marriage dissolves, there is no premarital decline in GP visits, and among men there are actually indications of increase; after marriage there is a clear upward trend (Figure A4, supplementary material).
Robustness checks
The point estimates from the SCM analysis suggest a decline in GP visits from the year when cohabitation starts to the year of marriage, but significance is not always attained. In an alternative analysis (not shown), the series of observations starts the year after entry into cohabitation, rather than FYO, and individuals who are already cohabiting at FYO (whose start of cohabitation is in most cases unknown) are also included but with FYO as the starting year. The age control group is changed to individuals who are already cohabiting at FYO or start cohabiting during the study period and remain cohabitants. The series of observations for these individuals starts at FYO (or the year after start of cohabitation) and ends at LYO. This analysis provides even less evidence of a decline in GP visits between cohabitation and marriage, but as in the SCM analysis, there is an increase after marriage.
Furthermore, supplementary SC, SCM, and SM analyses restricted to individuals born in Norway show the same patterns as reported earlier, but the effects are slightly stronger. This fits well with the generally larger number of GP consultations among the Norwegian born (according to our calculations). Another set of analyses shows that the use of a dichotomous outcome variable (no vs one or more GP consultations) does not change the main conclusions.
Adding other socio-demographic variables
When number of children, school enrolment, educational level, and income are added to the SC, SCM, and SM analyses, with no conditioning on subsequent events, the estimated effects of time since entry into cohabitation or marriage change little (Tables A5.1–A5.3, supplementary material). There is a somewhat weaker downward trend in GP visits before cohabitation or marriage (especially in the SC and SCM analyses) and a slightly less declining or more strongly increasing trend afterwards. See Appendix 6 (supplementary material) for a brief summary of the effects of the socio-demographic variables.
Dissolution of consensual unions and marriages, and subsequent union formation
The effects of union dissolution are not the focus of this study, but are reported (still with restriction to ages <60) for comparison. As we would expect, there is an increase in GP visits up to the time of dissolution, and especially during the last two years (Appendix 7, supplementary material). An immediate but slower decline takes place after the dissolution. On the whole, the increases in GP visits before a marital dissolution are about three times larger than the decreases around marriage and start of cohabitation.
Three transitions are analysed for individuals who have experienced previous dissolution: SC, SCM, and SM, without conditioning on subsequent events. There is less decline in GP visits before these transitions than observed for those who have not experienced dissolution—if a decline at all—and an immediate and sharp increase afterwards (Appendix 8, supplementary material). The same patterns are found if those whose marriage later dissolves are excluded from the analysis (not shown).
Conclusions
Our aim was to analyse the trends in GP consultations for mental health conditions before and after marriage or start of cohabitation in more detail than in other investigations, by using an exceptionally large data set and a method that controls for constant unobserved individual characteristics (as in several recent studies) and age (not always adequately controlled for previously). More specifically, one goal was to examine the development in the pre-cohabitation period, which has so far attracted little interest. Another goal was to study the changes between entry into cohabitation and marriage, as well as after marriage, and to compare these with trajectories among the directly married. Only a few earlier studies of this type have distinguished between direct marriage and marriage after cohabitation. Most of our analysis has focused on individuals who have not previously experienced union dissolution.
There are four main messages. First, it is important to consider the period before entry into cohabitation or direct marriage. The number of GP visits falls for several years before these events, which may partly reflect the benefits of romantic involvement (which may last on average not more than a couple of years but much longer for some (Dommermuth et al. Citation2009; Sassler et al. Citation2018)). It seems reasonable to consider these dating benefits as an inherent part of the rewards from union formation. Studies that compare the situation after couples have moved in together with the situation immediately or only a few years earlier do not give a complete picture of the advantages associated with being in a union. Additionally, the decline before union formation may reflect couples having started to live together earlier than suggested by the data. Unfortunately, there are no Norwegian data that can shed light on this. Moreover, the decline may be a result of effects of health on the chance of forming a union. While widely accepted as the best approach for this kind of research, the fixed-effects model does not solve this reverse causality problem (Appendix 3, supplementary material). This limitation appears to be insufficiently acknowledged in the literature.
Attention to the changes in mental health before cohabitation or marriage is even more important in light of the moderate changes afterwards, which brings us to the second and third main messages. The second is that while there is indication of some further decline in GP visits after entry into cohabitation for those who formalize their relationship by marrying (on average a couple of years later), this decline lasts only until the marriage. This is noteworthy, because a marriage is in some respects different from a consensual union, on the whole being seen as a better living arrangement among those who choose to marry (as they would otherwise typically not take this step). As argued earlier, it would not be unreasonable to expect the different nature of a marriage to produce some health benefits, although previous studies—including fixed-effects analyses—have provided mixed evidence. However, marriage may at least be considered as a marker of relatively favourable development in mental health before the consensual union is formed, and perhaps also after union entry, compared with cohabitation not (yet) followed by marriage.
The third main message is that the trend in mental health is more favourable after direct marriage than after a marriage preceded by cohabitation: among women, the number of GP visits continues to decline for a couple of years after direct marriage (as opposed to the increase after marriage via cohabitation), and among men there is less post-marital increase if the marriage is direct. Furthermore, there is a stronger decline in GP visits in the last few years before direct marriage, especially among women. This pattern may reflect the fact that at the time of marriage, the intimate relationship has been ongoing for a shorter period for the directly married. Additionally, a more favourable development on the whole is indicated for the directly married. It is not obvious theoretically that this should be expected, and earlier fixed-effects investigations have not suggested special health advantages from this transition. One possible explanation (relevant even when we compare across fixed-effects analyses) might be that those who marry directly tend to hold more traditional family values, which may also lead to larger benefits from marriage.
The fourth, and far from surprising, main message is that the development in mental health varies strongly according to whether it is conditioned on later union stability. Among those who experience disruption, the number of GP visits increases shortly after the start of cohabitation (without later marriage) or marriage. This fits, of course, with the sharp increases in GP visits over some years before a union disruption. In fact, the increase before separation, divorce, or spousal death is about three times stronger than the changes around entry into cohabitation or marriage, as also reported by Kalmijn (Citation2017), whereas disruption of consensual unions appears to be less harmful. According to some estimates, there is an upturn in GP visits some years after marriage even among those who do not experience dissolution within the study period, but there may be a separation or divorce later, and the relationship quality may deteriorate anyway. Earlier studies have also shown post-marital deterioration in health or well-being. Furthermore, the development in mental health appears to be less favourable even before cohabitation or marriage among those who experience dissolution later, which makes good sense theoretically.
While the patterns are similar for women and men, with a few small exceptions, the magnitudes of the changes are not always the same. In particular, women experience a somewhat stronger decline in the number of consultations before the start of cohabitation than men, even when the generally higher tendency of women to consult GPs about mental health conditions is taken into account.
We might have expected changes in mental health before and after entry into cohabitation or marriage to be partly a result of having a child, leaving school, attaining higher educational levels, or earning more money, because in addition to being of likely importance for mental health, these factors probably influence the chance of being in a relationship and forming a union and are also affected by this process. However, while they are indeed linked to the number of GP visits, including them in the models has quite a small impact on the estimated effects of the key variable. In other words, if there are causal effects of cohabitation and marriage on mental health—which we cannot be sure about (see next subsection)—these effects must be a result of other mechanisms.
Among those who have experienced dissolution earlier, there is much less evidence of mental health benefits from cohabitation and marriage. It is, of course, possible that these relationships are of lower quality, even if analyses are restricted to marriages that remain intact throughout the study period. This would accord with ideas in the literature about special challenges in second or higher-order relationships (Hughes and Waite Citation2009; Sweeney Citation2010; Berntsen and Kravdal Citation2012). Surely, some individuals who are recorded in our analysis as not having experienced earlier dissolution have actually experienced it before the first year covered by the data. Therefore, those who are truly in their first relationship may enjoy even larger advantages from dating, cohabitation, and marriage than indicated by the patterns in .[23]
Overall, the results for Norway suggest that the mental health benefits of cohabitation and marriage are quite similar. The conclusion might, of course, be different if the analysis were repeated for another country with different laws and a different welfare system and normative climate.
Limitations
A weakness of this study is that the outcome variable reflects a combination of two outcomes: experiencing a mental health condition and seeking help from a GP (or not). Very serious conditions may not be adequately captured, as GPs typically refer these cases to specialized healthcare providers, and many individuals (especially with milder conditions) may not consult a physician and receive a diagnosis.[24] To the extent that a person’s inclination to seek professional help is constant, it is controlled for through the fixed-effects approach, but there are likely to be variations over time in this inclination, and if these variations are linked to cohabitation or marriage, they should be taken into account when interpreting the results. For example, we might suspect that experiencing a change in income on starting cohabitation or marrying, or becoming a parent after forming a union, could affect the tendency to seek help. (Parents may have less time to see a physician or even, in extreme cases, be afraid that they could lose custody of the child if they present with a mental health condition (Anderson et al. Citation2006)). However, GP consultations are heavily subsidized in Norway and inclusion of such socio-demographic variables has little impact on the estimated effects of cohabitation or marriage. Another possibility is that people are less likely to seek help for mental health when they are partnered, because of embarrassment, although it seems more likely that they would be more inclined to seek help because they are pushed or encouraged by their partner. If the latter were true, cohabitation or marriage (or prior dating) would have a more beneficial health effect than indicated by the estimates.
Another limitation is that some couples may have started living together earlier than suggested by the data, and some who are recorded as not having cohabited may actually have done so. One or both partners may, for example, be formally registered as still living with parents (particularly students). Consequently, it is possible that some of the reduction in GP visits before cohabitation or direct marriage may be a result of earlier cohabitation with the same partner, and if some of the directly married actually cohabited previously, the development for those who do marry directly may be more different from that for couples who marry after cohabitation than indicated by the estimates. Also, the difference in the pattern between those who experience earlier disruption and others may in reality be larger than suggested.
Note also that, for simplicity, we did not explore interactions, although the importance of marriage and cohabitation may well differ between, for example, parents and non-parents (Brown Citation2000; van Hedel et al. Citation2018), by the age when the transition is made, or by socio-economic status (Drefahl Citation2012; Sigle and Goisis Citation2019), including the degree of socio-economic homogamy. Furthermore, our perspective was purely individual, in the sense that the possibility of effects of one partner’s health on the other’s health (Gustavson et al. Citation2016) was ignored.
We should, of course, be careful in interpreting the reported estimates causally. First, time-varying life circumstances not captured by the included variables may both affect mental health and increase a person’s chance of entering a romantic relationship, consensual union, or marriage. A related issue is the possible effect of health on union formation. Such reverse causality is a general problem in this type of research, even in studies that distinguish only between before and after cohabitation/marriage, where there are two related additional concerns: results depending on the length of the chosen pre-transition period, and much of the effect of dating being ignored if this period is short. Second, the estimates tell us only how marriage and the steps leading up to it affect mental health among those who do marry (and similarly for cohabitation): that is, their health situation compared with how it would have been if they had not married. This effect of marriage ‘among the treated’ may be different from what would happen if those who do not marry, hypothetically, do so. Presumably, this latter group would experience less of an advantage, because it is typically those who expect the largest benefits from a certain family transition who make that transition, and their expected benefits likely accord to a considerable extent with the actual ones.[25] Another potential problem is the assumption about the same age effect among those who experience the transition under study as in the age control group. If, for example, those who marry/cohabit are a group with a more favourable underlying trend in mental health (less increase in GP visits over age), there would be fewer benefits of marriage/cohabitation than indicated by the estimates.[26] This is difficult to test because of the linear dependence between current age and time since transition. It is reassuring, however, that some key patterns in the estimates remain when the age control group is excluded, meaning that the age effect is estimated from the variations in GP consultations during the periods 10 or more years before or after the transition, under the assumption that time since the transition itself has no impact at that stage (Appendix 2, supplementary material).
These concerns about causality—relevant also in earlier studies—should be taken into account by politicians who might be tempted to use results from such investigations as justification for policies aimed at encouraging certain family behaviours. The same caveat is relevant for individuals making decisions about partnership, typically based on expectations about various types of implications for themselves. In such a situation, many might like to know what the health consequences of different relationship transitions are on average in a population, but we cannot claim that such causal effects have been identified in this study. However, our analysis is at least a step towards a better understanding of how people tend to be affected in terms of mental health by these milestones in life; it also feeds into the general discussion about whether and how cohabitation differs from marriage.
Supplementary Material
Download PDF (368.6 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Notes
1 Øystein Kravdal, Jonathan Wörn, and Bjørn-Atle Reme are all based at the Centre for Fertility and Health, Norwegian Institute of Public Health. Øystein Kravdal is also based at the Department of Economics, University of Oslo, Norway.
2 Please address all correspondence to Øystein Kravdal, Centre for Fertility and Health, Norwegian Institute of Public Health, PO Box 222 Skøyen, 0213 Oslo, Norway; or by E-mail: [email protected]
3 The work has been funded by the Research Council of Norway through its Centres of Excellence funding scheme, project number 262700.
4 Helpful comments from two reviewers and Wendy Sigle are greatly appreciated.
References
- Ali, M. M. and O. Ajilore. 2011. Can marriage reduce risky health behavior for African-Americans?, Journal of Family and Economic Issues 32(2): 191–203. https://doi.org/10.1007/s10834-010-9242-z
- Anderson, C. M., C. S. Robins, C. G. Greeno, H. Cahalane, V. C. Copeland, and R. M. Andrews. 2006. Why lower income mothers do not engage with the formal mental health care system: Perceived barriers to care, Qualitative Health Research 16(7): 926–943. https://doi.org/10.1177/1049732306289224
- Anusic, I., S. C. Yap, and R. E. Lucas. 2014. Testing set-point theory in a Swiss national sample: Reaction and adaptation to major life events, Social Indicators Research 119(3): 1265–1288. https://doi.org/10.1007/s11205-013-0541-2
- Averett, S. L., L. M. Argys, and J. Sorkin. 2013. In sickness and in health: An examination of relationship status and health using data from the Canadian National Public Health Survey, Review of Economics of the Household 11(4): 599–633. https://doi.org/10.1007/s11150-012-9143-z
- Baran, M. L., E. E. Diehnelt, and J. E. Jones. 2014. Family policies in Norway, in M. Robila (ed), Handbook of Family Policies Across the Globe. New York: Springer, pp. 77–90.
- Berntsen, K. N. and Ø. Kravdal. 2012. The relationship between mortality and time since divorce, widowhood or remarriage in Norway, Social Science & Medicine 75(12): 2267–2274. https://doi.org/10.1016/j.socscimed.2012.08.028
- Blekesaune, M. 2008. Partnership transitions and mental distress: Investigating temporal order, Journal of Marriage and Family 70(4): 879–890. https://doi.org/10.1111/j.1741-3737.2008.00533.x
- Blekesaune, M. 2018. Is cohabitation as good as marriage for people’s subjective well-being? Longitudinal evidence on happiness and life satisfaction in the British household panel survey, Journal of Happiness Studies 19(2): 505–520. https://doi.org/10.1007/s10902-016-9834-x
- Brockmann, H. and T. Klein. 2004. Love and death in Germany: The marital biography and its effect on mortality, Journal of Marriage and Family 66(3): 567–581. https://doi.org/10.1111/j.0022-2445.2004.00038.x
- Brown, S. L. 2000. The effect of union type on psychological well-being: Depression among cohabitors versus marrieds, Journal of Health and Social Behavior 41(3): 241–255. https://doi.org/10.2307/2676319
- Brown, S. L., W. D. Manning, and K. K. Payne. 2017. Relationship quality among cohabiting versus married couples, Journal of Family Issues 38(12): 1730–1753. https://doi.org/10.1177/0192513X15622236
- Chen, S. and J. C. van Ours. 2018. Subjective well-being and partnership dynamics: Are same-sex relationships different?, Demography 55(6): 2299–2320. https://doi.org/10.1007/s13524-018-0725-0
- De Jong Gierveld, J. 2004. Remarriage, unmarried cohabitation, living apart together: Partner relationships following bereavement or divorce, Journal of Marriage and Family 66(1): 236–243. https://doi.org/10.1111/j.0022-2445.2004.00015.x
- Diener, E., R. E. Lucas, and C. N. Scollon. 2006. Beyond the hedonic treadmill: Revising the adaptation theory of well-being, American Psychologist 61: 305–314. https://doi.org/10.1037/0003-066X.61.4.305
- Dommermuth, L., K. Aa. Wiik, and T. Noack. 2009. Gift, samboer eller “bare” kjærester. [Married, cohabiting or «only» romantic partners.] Samfunnsspeilet 2009/1. Statistics Norway. Oslo-Kongsvinger. Available at: www.ssb.no/befolkning/artikler-og-publikasjoner/gift-samboer-eller-bare-kjaereste
- Drefahl, S. 2012. Do the married really live longer? The role of cohabitation and socioeconomic status, Journal of Marriage and Family 74(3): 462–475. https://doi.org/10.1111/j.1741-3737.2012.00968.x
- Duncan, G. J., B. Wilkerson, and P. England. 2006. Cleaning up their act: The effects of marriage and cohabitation on licit and illicit drug use, Demography 43(4): 691–710. https://doi.org/10.1353/dem.2006.0032
- Eggebeen, D. J. 2005. Cohabitation and exchanges of support, Social Forces 83(3): 1097–1110. https://doi.org/10.1353/sof.2005.0027
- Eickmeyer, K. J., W. D. Manning, and S. L. Brown. 2019. What’s mine is ours? Income pooling in American families, Journal of Marriage and Family 81(4): 968–978. https://doi.org/10.1111/jomf.12565
- Falnes-Dalheim, A. 2009. Dokumentasjon av registerbasert familie- og husholdningsstatistikk. Årlig statistikk f.o.m. 2005, basert på folkeregistrert adresse per 1. januar [Documentation of register based family and household statistics. Annual statistics from 2005, based on addresses in the Population Register as of 1 January]. Notater 2009/54. Oslo/Kongsvinger: Statistics Norway.
- Franke, S. and H. Kulu. 2018. Cause-specific mortality by partnership status: Simultaneous analysis using longitudinal data from England and Wales, Journal of Epidemiology and Community Health 72(9): 838–844. https://doi.org/10.1136/jech-2017-210339
- Frijters, P., D. W. Johnston, and M. A. Shields. 2011. Life satisfaction dynamics with quarterly life event data, Scandinavian Journal of Economics 113(1): 190–211. https://doi.org/10.1111/j.1467-9442.2010.01638.x
- Gattig, A. and L. Minkus. 2021. Does marriage increase couples’ life satisfaction?, Comparative Population Studies 46: 123–148. https://doi.org/10.12765/CPoS-2021-05
- Grover, S. and J. F. Helliwell. 2019. How’s life at home? New evidence on marriage and the set point for happiness, Journal of Happiness Studies 20(2): 373–390. https://doi.org/10.1007/s10902-017-9941-3
- Gustavson, K., E. Røysamb, I. Borren, F. A. Torvik, and E. Karevold. 2016. Life satisfaction in close relationships: Findings from a longitudinal study, Journal of Happiness Studies 17(3): 1293–1311. https://doi.org/10.1007/s10902-015-9643-7
- Hahn, B. A. 1993. Marital status and women’s health: The effect of economic marital acquisitions, Journal of Marriage and the Family 55(2): 495. https://doi.org/10.2307/352818
- Hansen, T., T. Moum, and A. Shapiro. 2007. Relational and individual well-being among cohabiters and married individuals in midlife: Recent trends from Norway, Journal of Family Issues 28(7): 910–933. https://doi.org/10.1177/0192513X07299610
- Härkönen, J., M. D. Brons, and J. Dronkers. 2021. Family forerunners? Parental separation and partnership formation in 16 countries, Journal of Marriage and Family 83(1): 119–136. https://doi.org/10.1111/jomf.12682
- Hiekel, N., A. C. Liefbroer, and A. R. Poortman. 2014. Understanding diversity in the meaning of cohabitation across Europe, European Journal of Population 30(4): 391–410. https://doi.org/10.1007/s10680-014-9321-1
- Horwitz, A. V. and H. R. White. 1998. The relationship of cohabitation and mental health: A study of a young adult cohort, Journal of Marriage and the Family 60(2): 505–514. https://doi.org/10.2307/353865
- Hughes, M. E. and L. J. Waite. 2009. Marital biography and health at mid-life, Journal of Health and Social Behavior 50(3): 344–358. https://doi.org/10.1177/002214650905000307
- Joutsenniemi, K., T. Martelin, P. Martikainen, S. Pirkola, and S. Koskinen. 2006. Living arrangements and mental health in Finland, Journal of Epidemiology & Community Health 60(6): 468–475. https://doi.org/10.1136/jech.2005.040741
- Joutsenniemi, K., T. Martelin, L. Kestilä, P. Martikainen, S. Pirkola, and S. Koskinen. 2007. Living arrangements, heavy drinking and alcohol dependence, Alcohol and Alcoholism 42(5): 480–491. https://doi.org/10.1093/alcalc/agm011
- Kalmijn, M. 2017. The ambiguous link between marriage and health: A dynamic reanalysis of loss and gain effects, Social Forces 95(4): 1607–1636. https://doi.org/10.1093/sf/sox015
- Kiecolt-Glaser, J. K. 2018. Marriage, divorce, and the immune system, American Psychologist 73(9): 1098–1108. https://doi.org/10.1037/amp0000388
- Kim, H. K. and P. C. McKenry. 2002. The relationship between marriage and psychological well-being: A longitudinal analysis, Journal of Family Issues 23(8): 885–911. https://doi.org/10.1177/019251302237296
- Kohn, J. L. and S. L. Averett. 2014. Can’t we just live together? New evidence on the effect of relationship status on health, Journal of Family and Economic Issues 35(3): 295–312. https://doi.org/10.1007/s10834-013-9371-2
- Koskinen, S., K. Joutsenniemi, T. Martelin, and P. Martikainen. 2007. Mortality differences according to living arrangements, International Journal of Epidemiology 36(6): 1255–1264. https://doi.org/10.1093/ije/dym212
- Kravdal, Ø. 1999. Does marriage require a stronger economic underpinning than informal cohabitation?, Population Studies 53: 63–80. https://doi.org/10.1080/00324720308067
- Kravdal, Ø., E. Grundy, T. Lyngstad, and K. Aa. Wiik. 2012. Family life history and late mid-life mortality in Norway. Population and Development Review 38 (2): 237–257.
- Kravdal, Ø. 2013. The poorer cancer survival among the unmarried in Norway: Is much explained by comorbidities?, Social Science & Medicine 81: 42–52. https://doi.org/10.1016/j.socscimed.2013.01.012
- Kravdal, Ø., E. Grundy, and K. Keenan. 2018. The increasing mortality advantage of the married: The role played by education. Demographic Research 38 (20): 471–512.
- Kravdal, Ø., Aa. Tverdal, and E. Grundy. 2020a. The association between parity, CVD mortality, and CVD risk factors among Norwegian women and men, European Journal of Public Health 30(6): 1133–1139. https://doi.org/10.1093/eurpub/ckz235
- Kravdal, Ø., P. Magnus, B. Moum, and M. L. Høivik. 2020b. Association of childbearing with a short-term reduced risk of Crohn disease in mothers, American Journal of Epidemiology 189(4): 294–304. https://doi.org/10.1093/aje/kwz285
- Lamb, K. A., G. R. Lee, and A. DeMaris. 2003. Union formation and depression: Selection and relationship effects, Journal of Marriage and Family 65(4): 953–962. https://doi.org/10.1111/j.1741-3737.2003.00953.x
- Lee, S., E. Cho, F. Grodstein, I. Kawachi, F. B. Hu, and G. A. Colditz. 2004. Effects of marital transitions on changes in dietary and other health behaviours in US women, International Journal of Epidemiology 34(1): 69–78. https://doi.org/10.1093/ije/dyh258
- Lewis, M. A. and R. M. and Butterfield. 2007. Social control in marital relationships: Effect of one's partner on health behaviors, Journal of Applied Social Psychology 37(2): 298–319. https://doi.org/10.1111/j.0021-9029.2007.00161.x
- Liefbroer, A. C. and E. Dourleijn. 2006. Unmarried cohabitation and union stability: Testing the role of diffusion using data from 16 European countries, Demography 43(2): 203–221. https://doi.org/10.1353/dem.2006.0018
- Lillard, L. A. and C. W. Panis. 1996. Marital status and mortality: The role of health, Demography 33(3): 313–327. https://doi.org/10.2307/2061764
- Liu, H. and C. Reczek. 2012. Cohabitation and U.S. adult mortality: An examination by gender and race, Journal of Marriage and Family 74(4): 794–811. https://doi.org/10.1111/j.1741-3737.2012.00983.x
- Lucas, R. E., A. E. Clark, Y. Georgellis, and E. Diener. 2003. Re-examining adaptation and the set point model of happiness: Reactions to changes in marital status, Journal of Personality and Social Psychology 84(3): 527–539. https://doi.org/10.1037/0022-3514.84.3.527
- Lyngstad, T. H., T. Noack, and P. A. Tufte. 2011. Pooling of economic resources: A comparison of Norwegian married and cohabiting couples, European Sociological Review 27(5): 624–635. https://doi.org/10.1093/esr/jcq028
- Marcussen, K. 2005. Explaining differences in mental health between married and cohabiting individuals, Social Psychology Quarterly 68(3): 239–257. https://doi.org/10.1177/019027250506800304
- Mastekaasa, A. 1995. Age variations in the suicide rates and self-reported subjective well-being of married and never married persons, Journal of Community & Applied Social Psychology 5(1): 21–39. https://doi.org/10.1002/casp.2450050103
- Mikolai, J. and H. Kulu. 2018. Divorce, separation, and housing changes: A multiprocess analysis of longitudinal data from England and Wales, Demography 55: 83–106. https://doi.org/10.1007/s13524-017-0640-9
- Musick, K. and L. Bumpass. 2012. Reexamining the case for marriage: Union formation and changes in well-being, Journal of Marriage and Family 74(1): 1–18. https://doi.org/10.1111/j.1741-3737.2011.00873.x
- Musick, K. and K. Michelmore. 2018. Cross-national comparisons of union stability in cohabiting and married families with children, Demography 55(4): 1389–1421. https://doi.org/10.1007/s13524-018-0683-6
- Næss, S., M. Blekesaune, and N. Jakobsson. 2015. Marital transitions and life satisfaction: Evidence from longitudinal data from Norway, Acta Sociologica 58(1): 63–78. https://doi.org/10.1177/0001699314563841
- Pepin, J. R. 2019. Beliefs about money in families: Balancing unity, autonomy, and gender equality, Journal of Marriage and Family 81(2): 361–379. https://doi.org/10.1111/jomf.12554
- Perelli-Harris, B., W. Sigle-Rushton, M. Kreyenfeld, T. Lappegård, R. Keizer, and C. Berghammer. 2010. The educational gradient of childbearing within cohabitation in Europe, Population and Development Review 36(4): 775–801. https://doi.org/10.1111/j.1728-4457.2010.00357.x
- Perelli-Harris, B., M. Mynarska, A. Berrington, C. Berghammer, A. Evans, O. Isupova, and D. Vignoli. 2014. Towards a new understanding of cohabitation: Insights from focus group research across Europe and Australia, Demographic Research 31: 1043–1078. https://doi.org/10.4054/DemRes.2014.31.34
- Perelli-Harris, B., S. Hoherz, F. Addo, T. Lappegård, A. Evans, S. Sassler, and M. Styrc. 2018. Do marriage and cohabitation provide benefits to health in mid-life? The role of childhood selection mechanisms and partnership characteristics across countries, Population Research and Policy Review 37(5): 703–728. https://doi.org/10.1007/s11113-018-9467-3
- Perelli-Harris, B. and M. Styrc. 2018. Mental well-being differences in cohabitation and marriage: The role of childhood selection, Journal of Marriage and Family 80(1): 239–255. https://doi.org/10.1111/jomf.12431
- Perelli-Harris, B., S. Hoherz, T. Lappegård, and A. Evans. 2019. Mind the “happiness” gap: The relationship between cohabitation, marriage, and subjective well-being in the United Kingdom, Australia, Germany, and Norway, Demography 56(4): 1219–1246. https://doi.org/10.1007/s13524-019-00792-4
- Poortman, A. R. and T. H. Lyngstad. 2007. Dissolution risks in first and higher order marital and cohabiting unions, Social Science Research 36(4): 1431–1446. https://doi.org/10.1016/j.ssresearch.2007.02.005
- Prioux, F. 2006. Cohabitation, marriage and separation: Contrasts in Europe, Population & Societies 422: 1. https://doi.org/10.3917/popsoc.422.0001
- Quari, S. 2014. Marriage, adaptation and happiness: Are there long-lasting gains to marriage?, Journal of Behavioral and Experimental Economics 50: 29–39. https://doi.org/10.1016/j.socec.2014.01.003
- Robles, T. F., R. B. Slatcher, J. M. Trombello, and M. M. McGinn. 2014. Marital quality and health: A meta-analytic review, Psychological Bulletin 140(1): 140–187. https://doi.org/10.1037/a0031859
- Roelfs, D. J., E. Shor, R. Kalish, and T. Yogev. 2011. The rising relative risk of mortality for singles: Meta-analysis and metaregression, American Journal of Epidemiology 174(4): 379–389. https://doi.org/10.1093/aje/kwr111
- Ross, C. E. 1995. Reconceptualizing marital status as a continuum of social attachment, Journal of Marriage and the Family 57(1): 12–140. https://doi.org/10.2307/353822
- Sánchez Gassen, N. and B. Perelli-Harris. 2015. The increase in cohabitation and the role of union status in family policies: A comparison of 12 European countries, Journal of European Social Policy 25(4): 431–449. https://doi.org/10.1177/0958928715594561
- Sassler, S., K. Michelmore, and Z. Qian. 2018. Transitions from sexual relationships into cohabitation and beyond, Demography 55(2): 511–534. https://doi.org/10.1007/s13524-018-0649-8
- Sassler, S. and D. T. Lichter. 2020. Cohabitation and marriage: Complexity and diversity in union-formation patterns, Journal of Marriage and Family 82(1): 35–61. https://doi.org/10.1111/jomf.12617
- Shor, E., D. J. Roelfs, P. Bugyi, and J. E. Schwartz. 2012a. Meta-analysis of marital dissolution and mortality: Reevaluating the intersection of gender and age, Social Science & Medicine 75(1): 46–59. https://doi.org/10.1016/j.socscimed.2012.03.010
- Shor, E., D. J. Roelfs, M. Curreli, L. Clemow, M. M. Burg, and J. E. Schwartz. 2012b. Widowhood and mortality: A meta-analysis and meta-regression, Demography 49(2): 575–606. https://doi.org/10.1007/s13524-012-0096-x
- Sigle, W. and A. Goisis. 2019. Mind the gap: The health advantages that accompany parental marriage vary by maternal nativity, Population Studies 73(3): 369–386. https://doi.org/10.1080/00324728.2019.1654613
- Simon, R. W. 2002. Revisiting the relationships among gender, marital status, and mental health, American Journal of Sociology 107(4): 1065–1096. https://doi.org/10.1086/339225
- Sobotka, T. and L. Toulemon. 2008. Changing family and partnership behaviour: Common trends and persistent diversity across Europe, Demographic Research 19(6): 85–138. https://doi.org/10.4054/DemRes.2008.19.6
- Soons, J. P. and M. Kalmijn. 2009. Is marriage more than cohabitation? Well-being differences in 30 European countries, Journal of Marriage and Family 71(5): 1141–1157. https://doi.org/10.1111/j.1741-3737.2009.00660.x
- Soons, J. P., A. C. Liefbroer, and M. Kalmijn. 2009. The long-term consequences of relationship formation for subjective well-being, Journal of Marriage and Family 71(5): 1254–1270. https://doi.org/10.1111/j.1741-3737.2009.00667.x
- Stanley, S. M., S. W. Whitton, and H. J. Markman. 2004. Maybe I do: Interpersonal commitment and premarital or nonmarital cohabitation, Journal of Family Issues 25(4): 496–519. https://doi.org/10.1177/0192513X03257797
- Statistics Norway. 2021a. Cohabitants, married, and single, by age group. www.ssb.no/en/statbank/table/06854/
- Statistics Norway. 2021b. Population, by sex, age and marital status. www.ssb.no/en/statbank/table/03031/
- Steele, F., W. Sigle-Rushton, and Ø. Kravdal. 2009. Consequences of family disruption on children’s educational outcomes in Norway, Demography 46(3): 553–574. https://doi.org/10.1353/dem.0.0063
- Stutzer, A. and B. S. Frey. 2006. Does marriage make people happy, or do happy people get married?, The Journal of Socio-Economics 35(2): 326–347. https://doi.org/10.1016/j.socec.2005.11.043
- Sweeney, M. M. 2010. Remarriage and stepfamilies: Strategic sites for family scholarship in the 21st century, Journal of Marriage and Family 72(3): 667–684. https://doi.org/10.1111/j.1741-3737.2010.00724.x
- Tao, H. L. 2019. Marriage and happiness: Evidence from Taiwan, Journal of Happiness Studies 20(6): 1843–1861. https://doi.org/10.1007/s10902-018-0029-5
- Thomas, M. J. and C. H. Mulder. 2016. Partnership patterns and homeownership: A cross-country comparison of Germany, the Netherlands and the United Kingdom, Housing Studies 31(8): 935–963. https://doi.org/10.1080/02673037.2016.1164832
- Uchino, B. N., K. Bowen, R. K. de Grey, J. Mikel, and E. B. Fisher. 2018. Social support and physical health: Models, mechanisms, and opportunities, in E. B. Fisher, L. D. Cameron, A. J. Christensen, U. Ehlert, Y. Guo, and B. Oldenburg (eds), Principles and Concepts of Behavioral Medicine. New York, NY: Springer, pp. 341–372.
- Umberson, D., T. Pudrovska, and C. Reczek. 2010. Parenthood, childlessness, and well-being: A life course perspective, Journal of Marriage and Family 72(3): 612–629. https://doi.org/10.1111/j.1741-3737.2010.00721.x
- Umberson, D., M. B. Thomeer, and K. Williams. 2013. Family status and mental health: Recent advances and future directions, in C. S. Aneshensel, J.C. Phelan, and A. Bierman (eds), Handbook of the Sociology of Mental Health. Dordrecht: Springer, pp. 405–431.
- Van Hedel, K., P. Martikainen, H. Moustgaard, and M. Myrskylä. 2018. Cohabitation and mental health: Is psychotropic medication use more common in cohabitation than marriage?, SSM - Population Health 4: 244–253. https://doi.org/10.1016/j.ssmph.2018.01.001
- Wade, T. J. and D. Pevalin. 2004. Marital transitions and mental health, Journal of Health and Social Behavior 45(2): 155–170. https://doi.org/10.1177/002214650404500203
- Wu, Z. and R. Hart. 2002. The effects of marital and nonmarital union transition on health, Journal of Marriage and Family 64(2): 420–432. https://doi.org/10.1111/j.1741-3737.2002.00420.x
- Wiik, K. Aa., R. Keizer, and T. Lappegård. 2012. Relationship quality in marital and cohabiting unions across Europe, Journal of Marriage and Family 74(3): 389–398. https://doi.org/10.1111/j.1741-3737.2012.00967.x
- Wilmoth, J. and G. Koso. 2002. Does marital history matter? Marital status and wealth outcomes among preretirement adults, Journal of Marriage and Family 64(1): 254–268. https://doi.org/10.1111/j.1741-3737.2002.00254.x
- Zimmermann, A. C. and R. A. Easterlin. 2006. Happily ever after? Cohabitation, marriage, divorce, and happiness in Germany, Population and Development Review 32(3): 511–528. https://doi.org/10.1111/j.1728-4457.2006.00135.x
