ABSTRACT
Objective: Our aim was to explore how differing attitudes, expectations, and experiences among people with obesity (PwO) and healthcare providers (HCPs) might have an impact on effectively implementing current obesity treatment guidelines.
Methods: Online surveys were conducted among 3,008 adult PwO (BMI≥30 by self-reported height and weight) and 606 HCPs.
Results: PwO with weight loss ≥ 10% during the previous three years were more likely to have been diagnosed with obesity and to have discussed a weight loss plan with an HCP. However, only 21% believe HCPs have a responsibility to actively contribute to their obesity treatment. Further, HCPs tend not to effectively communicate the diagnosis of obesity, its nature as a serious and chronic disease, the full range of treatment options, and obesity’s implications for health and quality of life.
Regarding treatment goals, HCPs more often focus on BMI reduction, while PwO’s goals focus on improved functioning, energy, and appearance. HCPs also tend to underestimate their patients’ motivation to address their obesity. Twenty-eight percent of HCPs ‘completely agreed’ that losing weight was a high priority for PwO, whereas more than half of PwO ‘completely agreed’ that losing weight was a high priority for them. When asked how their HCP could better support them, PwO most often expressed a desire for helpful resources, as well as assistance with specific and realistic goal-setting to improve health.
Conclusions: HCPs can more effectively implement obesity treatment guidelines by more clearly and proactively communicating with PwO about their diagnosis, health implications of obesity, desired treatment goals, and the full range of treatment options. HCPs should understand that most PwO believe that managing their disease is solely their own responsibility. HCPs can also encourage more effective conversations by better appreciating their patients’ motivation and treatment goals.
Trial registration: ClinicalTrials.gov identifier: NCT03223493.
Introduction
Obesity is a chronic, serious, and progressive disease associated with adverse health, social, and economic consequences [Citation1–Citation8]; however, several potential barriers to effectively treating obesity exist. People with obesity (PwO) are often associated with undesirable attitudes and stereotypes which have far-reaching adverse effects, including discrimination and prejudice in employment and educational settings, in close relationships, and during patient and healthcare provider (HCP) interactions [Citation9–Citation15]. This weight stigma is present even in health care settings where it affects quality of care through shorter appointment times, less discussion with patients, and fewer interventions [Citation16,Citation17]. Several studies show that patients with obesity are less likely to receive preventive services and exams including mammograms and pelvic exams and have increased missed diagnoses [Citation18,Citation19]. Weight bias may affect the quality of their obesity management as well; many PwO do not receive the diagnosis of obesity even after visiting their HCP [Citation20,Citation21]. Stigma in the healthcare setting can negatively impact patients’ weight loss experiences by reinforcing an internal sense of failure, encouraging avoidance of visits for treatment due to embarrassment, and leading to a reactive treatment plan that assumes noncompliance [Citation11,Citation15]. Perceptions of lack of motivation or desire to lose weight can also be a barrier, particularly when these beliefs about PwO are held by HCPs. According to a recent survey, HCPs believe patients with obesity are not very engaged in addressing their weight and that lack of patient perception of obesity as a health issue is one of the major barriers to patient engagement in obesity treatment [Citation22].
Although clinical guidelines developed by various professional organizations including the American Heart Association (AHA), American College of Cardiology (ACC), and The Obesity Society (TOS) [Citation23], the American Association of Clinical Endocrinologists and the American College of Endocrinology (AACE/ACE) [Citation24] and the Obesity Medicine Association (OMA) [Citation25], describe strategies for identifying and treating patients with obesity, many health care providers are not well-versed in the recommendations [Citation26]. These guidelines include several steps in obesity management, summarized as: (1) identifying patients for obesity management by screening for BMI, comorbid conditions, and complications of obesity; (2) communicating the benefits of treating obesity through weight loss including the value of sustained weight loss of 5–10%; (3) providing dietary therapy for weight loss with a plan based on the patient’s preferences and health status; (4) providing lifestyle and behavioral counseling, preferably comprehensive weight loss interventions utilizing motivational interviewing; and (5) recommending pharmacotherapy and/or bariatric surgery for patients who meet appropriate BMI and/or comorbidity criteria. To effectively manage obesity, the treatment guidelines should be combined with the communication elements from the chronic disease management models, and broaching the topic of obesity is a critical first step [Citation27]. The 2015 Milan Declaration can provide additional guidance on how to specifically consider the patient’s perspective in addressing obesity and its management [Citation28].
The ACTION (Awareness, Care, and Treatment In Obesity management) study examined perceptions, attitudes, behaviors, and potential barriers to effective obesity care across three respondent groups: PwO, HCPs, and employer representatives (ERs) [Citation29]. Results of the ERs have been previously reported [Citation29,Citation30]. The aim of this paper is to explore how differing attitudes, expectations, and experiences among PwO and HCPs might have an impact on effectively implementing current treatment guidelines for obesity.
Material and methods
This study, sponsored by Novo Nordisk Inc., was approved by an Institutional Review Board [Citation31]. This study is registered with ClinicalTrials.gov, number NCT03223493. Separate surveys were used for each audience to measure obesity-related perceptions, behaviors, and potential barriers. The study samples were independent, i.e. PwO and HCPs surveyed were not matched pairs. A detailed methodological description has been previously presented [Citation29].
Data were collected from 29 October to 12 November 2015 via online surveys using a cross-sectional, US-based stratified sample design. PwO inclusion criteria were: age ≥18 years, living in the US, and body mass index (BMI) of ≥30 kg/m2 based on self-reported height and weight. We selected a BMI ≥30 to minimize the effects of self-reported weight and height (studies support the conclusion that self-reported height and weight underestimate BMI [Citation32–Citation34]). Thus, with the inclusion criterion of BMI ≥30 calculated from self-reported height and weight, the actual BMIs of subjects enrolled in this study are likely to skew somewhat higher across the study population. PwO were categorized into those who self-reported a weight loss of ≥10% in the past three years and maintained that weight loss for at least one year, and those who self-reported weight loss of <10% in the past three years or reported a weight loss of ≥10% but did not keep the weight off for at least one year. PwO were also categorized by obesity class (Class I: BMI 30- < 35, Class II: BMI 35- < 40, Class III: BMI≥40) for analysis purposes [Citation35].
HCP inclusion criteria included: employment in a U.S. facility (except Vermont to comply with Sunshine reporting requirements), spending a minimum of 70% of professional time in patient care, seeing ≥100 patients during the previous month with ≥10 patients in need of weight management, and practicing 2–35 years in their current role; board certification was additionally required of physicians. To reduce potential selection bias, respondent-level, individual weighting was applied to the PwO sample. Using an established weighting methodology [Citation36], final data were weighted to representative demographic targets for age, household income, ethnicity, race, Hispanic descent, gender, and U.S. region based on the 2010 U.S. Census [Citation37]. Participant characteristics are reported for the final unweighted sample. All other results are weighted unless otherwise specified.
The PwO survey covered a wide range of topics on obesity including information on PwO weight history, weight management attempts and experiences, weight management goals, motivators to lose weight, barriers to weight loss, obesity awareness and perceptions, attitudes towards obesity, tools and resources helpful in weight management efforts, support structure, employer wellness programs, and societal perspectives on obesity. Another key survey topic was the interaction and discussion that PwO have with their HCP. As not all of the PwO in our study had discussed weight with an HCP in the past five years, those who did not have a conversation with their HCP were asked questions related to what they would like their HCP to do regarding their weight and weight management. PwO were asked to identify the type of HCP with whom they discussed their weight most often in the past 5 years (or would most like to discuss weight for those who have not had a discussion). Respondents chose from a list of physician specialties, nurse, nurse practitioner, physician assistant, registered dietician, diabetes educator, social worker/psychologist, nutritionist, and were also able to write in another type of HCP; PwO were then asked questions about the interaction with this HCP. The HCP survey covered similar topics and were asked about their interactions and discussions with their patients who had a BMI greater than 27 and at least 1 comorbidity or a BMI greater than 30 with or without comorbidities. Five-point end-anchored Likert scales assessed agreement, where ‘1’ meant ‘do not agree at all,’ and ‘5’ meant ‘completely agree.’ Responses of 4 or 5 were coded and reported as ‘agree’ unless otherwise noted.
Statistical analysis
Descriptive statistical analysis (means, frequencies) was performed using SPSS 15.0.1 [Citation38]. Tests of differences (chi square, t-tests) within respondent types were performed using SPSS tables; additional analyses were performed using Stata/IC 14.1 [Citation39]. Statistical significance was set at p < 0.05, using 2-tailed tests. Multiple test corrections were not applied to statistical tests, as this research was exploratory and descriptive in nature.
Results
Description of PwO and HCP samples
Characteristics for PwO (n = 3,008) and HCP (n = 606) are displayed in .
Table 1. Sample characteristics (unweighted).
Attitudes toward weight loss by HCPs and PwO
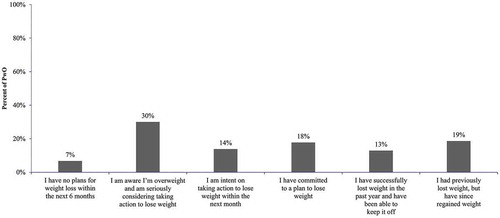
More than half of PwO ‘completely agreed’ that losing weight is a high priority for them compared to only 28% of HCPs who believed the same regarding their patients (). PwO were also more motivated to lose weight than HCPs perceived (). PwO appeared to be interested in treating their obesity as the majority (62%) reported they were seriously considering taking action to lose weight, intent on taking action to lose weight within the next month, or had committed to a plan to lose weight (). When asked about the factors that have the greatest influence on their desire to lose weight, PwO were most likely to cite wanting to feel better physically (71%), wanting to be in better shape (71%), and general health concerns (53%). HCPs were presented with the same list of factors and asked what they believed most motivated patients to lose weight; PwO were less motivated than HCPs believed by a specific medical event (13% PwO vs. 79% HCPs), wanting to stop taking medication for a weight-related health condition (25% PwO vs. 54% HCPs), an upcoming social occasion or event (13% PwO vs. 62% HCPs), and financial incentives such as lower co-pays or insurance premiums (5% PwO vs. 26% HCPs).
Figure 1. Attitudes Towards Weight Loss. All PwO (n = 3,008), All HCPs (n = 606); PwO = People with Obesity, HCP = Healthcare Provider.
Most PwO (82%) believed that weight management is completely their responsibility, as previously reported [Citation29]. Only 19% of PwO reported that ‘encouragement, support and recommendations from an HCP’ influenced their desire to lose weight, which may be related to thinking that weight is completely within their control, a belief shared by almost half of PwO (47%). Many PwO believed they could lose weight if they set their mind to it (), but only about half (56%) agreed they know how to lose weight. Less than one quarter of PwO (21%) agreed their HCP has a responsibility to actively contribute to a successful weight loss effort.
Clinical guidelines for effective obesity care – evaluation, diagnosis, and communication
Because PwO tended to underestimate their weight, with the majority of Obesity Class I identifying themselves as ‘overweight’ (), it is important for HCPs to directly address patients’ weight status. Although PwO may not recognize their obesity status, they are dissatisfied with their weight – PwO were more likely to disagree that they were happy with their current weight than HCPs reported regarding their own patients (80% PwO vs. 55% HCPs). Most PwO (85%) were at least ‘somewhat’ worried about the effect of their weight on their future health.
Table 2. Perception of current weight compared to obesity class.
PwO with ≥10% maintained weight loss for at least one year were more likely to report having ever been diagnosed as ‘overweight,’ ‘obese,’ or both rather than being given no diagnosis or being unsure of a diagnosis (68% vs. 31%). Those reporting being diagnosed were significantly more likely than those not diagnosed to report a greater percentage of weight loss from their maximum weight three years ago (6.7% vs. 5.1%).
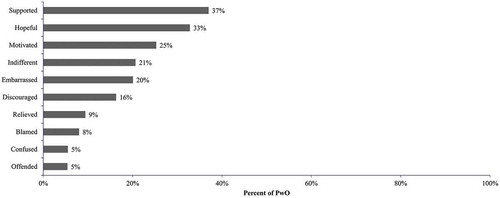
More than two-thirds of HCPs (67%) were ‘very’ or ‘extremely’ comfortable discussing weight management with their patients and the majority of PwO who had discussed their weight with their HCP agreed they feel comfortable talking to their HCP about their weight (62%). At least half of these PwO agreed their HCP listens carefully to what they say about their weight, listens to their concerns, and understands the difficulties of weight management (). PwO who had discussed weight with their HCP felt supported (37%), hopeful (33%), and motivated (25%) after these discussions (). Among those who had not discussed their weight with their HCP in the past five years, the main reason reported by PwO for not seeking assistance from their HCP is a belief that it is their own responsibility to manage their weight (44%). Embarrassment and lack of motivation to lose weight were infrequently reported as barriers (15% and 21%, respectively), which is contrary to the perception of HCPs in our study as previously reported [Citation29]. However, about half of those who have not discussed weight with an HCP (52%) reported that they would like their HCP to bring up their weight during appointments and agreed they would feel comfortable talking to their HCP about their weight (57%).
Figure 3. PwO Attitudes toward Weight Discussions with HCPs. All PwO who have discussed being overweight/losing weight with their provider (n = 2,185); PwO = People with Obesity, HCP = Healthcare Provider.
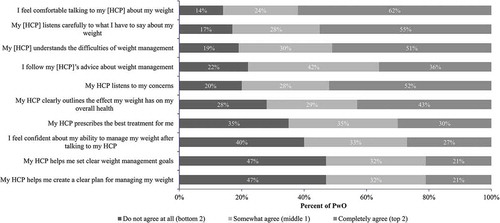
Figure 4. Feelings After Discussion about Weight with HCP. All PwO who have discussed being overweight/losing weight with their provider (n = 2,185); PwO = People with Obesity, HCP = Healthcare Provider.
Approximately half of PwO (54%) reported speaking to an HCP about their weight in relation to their health within the past 6 months, but just over 4 in 10 agreed their HCP clearly outlines the effect their weight has on their overall health. On average, HCPs reported discussing the impact of overweight/obesity on their patients’ health at 62% of appointments with patients in need of weight management and that these discussions comprised 24% of a typical wellness visit for these patients. Despite these conversations, just over half (55%) of PwO reported being formally diagnosed by their HCP as ‘obese.’
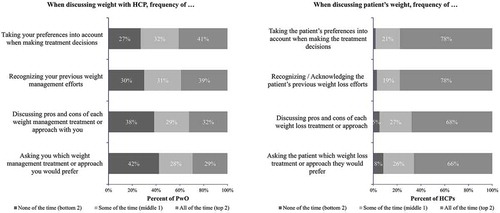
While almost all HCPs (95%) reported discussing trended weight with their patients, less than half of PwO who have discussed weight with their HCP (47% with Class I obesity, 40% with Class II obesity, and 41% with Class III obesity) reported their HCP discussing their recorded weight over time. Among HCPs who discussed trended weight with their patients with obesity, weight history was most often discussed verbally (64%). Fewer HCPs used a visual aid when discussing weight history with their patients; only 42% showed weight history on the computer screen, and an even smaller 18% provided a printed graph or chart. Less than one-third of HCPs (30%) asked their patients to share their history of weight gains and losses over time. Although HCPs claimed to recognize their patients’ previous weight loss efforts ‘all of the time’ (78%), only 39% of PwO reported their HCP recognizing their previous efforts this frequently ().
Figure 5. How Weight is Discussed. All PwO who have discussed being overweight/losing weight with their provider (n = 2,185) and All HCPs (n = 606); PwO = People with Obesity, HCP = Healthcare Provider.
When asked how their HCP could better support them in achieving a healthy weight, PwO most often selected ‘provide me with helpful resources,’ ‘help me set specific goals to improve my health,’ and ‘help me to set more realistic goals to improve my health.’ PwO reported that setting realistic goals which seem possible to reach (51%), having a customized weight loss/management plan (34%), support from their HCP (29%), and a better understanding of the physiology of obesity (23%) would improve their chances for success in their weight management efforts.
Clinical guidelines for effective obesity care – interventions
Current obesity management guidelines outline treatment approaches including dietary therapy in line with patient preferences, lifestyle and behavioral counseling, and pharmacotherapy and/or bariatric surgery for appropriate patients. However, few PwO (21%) agreed their HCP helped them set clear weight management goals or create a clear plan for managing their weight. This is an important step as those with substantial weight loss were significantly more likely to report having spoken to their HCP about a weight loss plan (45% vs. 37%).
Although few PwO indicated that losing a specific percentage of their body weight was important to achieve as part of their weight management, many (40%) reported being satisfied only if they could lose more than 20% of their body weight, and only 22% would be satisfied with losing up to 10% of their body weight. General improvements in diet and exercise are the predominant strategies HCPs recommended for their patients in need of weight management, including general improvement in eating habits/reducing calories (58%) and generally being more active/increase in physical activity (57%). Fewer HCPs reported recommending specific diets or diet programs (27%), visits to a dietitian/nutritionist (27%), or a formal exercise program/gym membership/personal trainer (23%). HCPs were least likely to recommend prescription (11%) or over-the-counter (4%) weight loss medications or visiting a non-surgical weight loss specialist or clinic (9%). PwO who discussed their weight with their HCP reported conversations similarly; few reported discussing specific diet or exercise programs or other interventions such as counseling, pharmacotherapy, or weight loss surgery ().
Figure 6. Treatments Discussed with HCPs. All PwO who have discussed being overweight/losing weight with their provider (n = 2,185); PwO = People with Obesity.
Despite the similarities in approaches reported by HCPs and PwO, the two groups had different perceptions of these treatment discussions – more than two-thirds of HCPs reported discussing the pros and cons of each treatment frequently, while only about one-third of PwO reported that their HCP often does so. Almost all HCPs said they asked their patients which weight loss treatment or approach they prefer and took their patients’ preferences into account when making treatment decisions at least some of the time with 78% saying they did this ‘all of the time’; however, only 41% of PwO felt their HCP did this ‘all of the time’ (). Some PwO (15%) reported their HCP did not provide any weight management suggestions at all after their most recent discussion and few PwO (24%) reported that their HCP scheduled a follow-up appointment related to their weight after their last visit.
When weight management plans were implemented, HCPs tended to predominately monitor the effectiveness of their patients’ weight management strategies using metrics of less importance to PwO. Although changes/improvements in comorbidities or other illnesses were commonly used by HCPs to measure the success of weight management strategies (63%), they were most likely to measure their patients’ success through a reduction in BMI (81%) and amount of weight lost in pounds (72%); less than half (46%) reported using improvement in patient functioning to monitor effectiveness. This approach is in contrast with the important outcomes reported by PwO including improving or preventing health conditions (63% and 70%, respectively), having more energy (64%), and improving their appearance (60%).
Discussion
Vital to the effective implementation of treatment guidelines for obesity is better understanding the attitudes, expectations, and experiences of the key stakeholder, PwO, and how they differ from those of their HCPs. The ACTION study explored these factors from the perspective of PwO and HCPs and identified key areas in which HCPs can better support PwOs within current obesity management guidelines.
Despite recognition as a serious and chronic disease, obesity management often does not follow a chronic disease management model as recommended by AACE/ACE and AHA/ACC/TOS in the organizations’ treatment guidelines [Citation24,Citation40]. This model has been used successfully to treat obesity in a primary care setting [Citation41]. Applying this approach would take advantage of missed opportunities to improve the quality of the obesity management dialogue between HCPs and PwO. Despite HCPs reporting being comfortable discussing weight management and doing so regularly with their patients with obesity, there is a lack of concordance between HCPs and PwO in the quality of weight management conversations. The way HCPs communicate with their patients can be an important factor in effectively managing obesity [Citation12,Citation42,Citation43].
Obesity management guidelines convey the importance of communicating the adverse health effects of overweight and obesity, and the benefits of modest and sustained weight loss, but HCPs are not effectively communicating their patients’ weight status and its health implications. Obesity is a disease and the first step in management of any chronic disease is making the diagnosis, and, very importantly, clearly communicating the diagnosis to the patient. This study shows that PwO tend to underestimate their weight status and the health implications. Formally diagnosing obesity and clearly communicating the diagnosis is an important first step in treating obesity as a serious and chronic disease requiring long-term management following clinical treatment guidelines. Therefore, screening all patients for BMI, complications of obesity, and comorbid conditions is critical in identifying patients needing obesity management. PwO in our study who were diagnosed with obesity were more likely to be successful in their weight loss efforts.
One barrier to engaging patients in discussion about obesity may be the widespread assumption that PwO lack the motivation to lose weight. HCPs may not formally or informally evaluate their patients’ readiness to change as part of their obesity management discussions despite most PwO reporting several attempts to lose weight. This lack of individual evaluation may lead to incorrect assumptions and misinterpretation of patients’ motivations, which differ among individuals.
Another key barrier to PwO receiving support from their HCP may be the belief held by most PwO that weight management is completely their responsibility and not the responsibility of their HCP. The ACTION study and others have demonstrated that while the majority of PwO have an intent to lose weight, they tend to not seek treatment for obesity from HCPs [Citation44], yet are receptive to having weight and weight loss discussions. Because discussions with HCPs, regardless of the message or guidance provided, were well-received by PwO, having conversations with patients that specifically focus on obesity guideline recommendations has the potential to improve obesity management success.
Shared decision-making may provide another opportunity for more effective weight management discussions between PwO and HCPs – a key component of the chronic disease management model that is currently underutilized in these discussions. A lack of clear, attainable weight loss goals is a barrier perceived by many PwO who are not aligned with HCPs on their goals and definitions of success. The most common goals of PwO are general improvement in health and functioning and any amount of weight loss. HCPs tend to set goals related to reduction in BMI or pounds/percentages of weight loss but are less likely to set ‘SMART’ goals (Specific, Measurable, Attainable, Relevant and Timely) that are most pertinent to their patients and thus more likely to result in successful weight management. Weight loss goals PwO set for themselves may be difficult to attain, with many wanting to lose more than 20% of their body weight. Helping PwO understand the health benefits of a 5–10% weight loss goal based on guidelines may be one way HCPs can help PwO set more achievable goals for long-term maintenance [Citation45,Citation46], yet only 4 in 10 had a discussion about the effect of their weight on their overall health. Many PwO feel that their HCP can be a great resource on their weight management journey, but that their preferences may not always be considered in treatment decisions. Better alignment on what goals are appropriate and attainable for each individual patient may support patient success [Citation47].
Clinical practice guidelines encourage a variety of therapeutic approaches to obesity management; however, most treatment recommendations by HCPs are based on general lifestyle improvements – more intensive treatments such as referral to a dietary or weight loss specialist, pharmacotherapy, and bariatric surgery are recommended for very few patients. Using established counseling methods to develop customized obesity management plans for patients based on their own motivations, goals, and preferences may help HCPs better support obesity management efforts [Citation48,Citation49]. By tracking changes in weight over time, acknowledging the results of past weight loss efforts, and soliciting patient feedback, HCPs can alter these treatment plans as needed to optimize each patient’s outcomes. These modifications may include intensifying lifestyle changes beyond healthy diet and increased physical activity, referral to a specialist, pharmacotherapy, and referral to a bariatric surgeon. Carefully listening to and considering PwO’s individual needs and goals related to weight management and helping PwO set clear plans and goals could lead to better outcomes [Citation50]. Scheduling follow-up appointments for the chronic disease of obesity to alter treatment plans based on results and soliciting patient feedback after implementing weight loss strategies rather than assuming the patient did not follow advice may help identify areas for further discussion and alternative solutions.
The present study has some limitations, as previously reported [Citation29]. Additionally, causality of the relationships between obesity management strategies and outcomes cannot be inferred from the data. The PwO and HCP respondents were sampled independently. Because the PwO and HCP samples were not matched, differences in perceptions between the two groups could be related to differences in the PwO surveyed and patients managed by the HCPs surveyed. The clinical guidelines continue to evolve; information on the current treatment guidelines and advocacy organizations can be found in the Obesity Treatment Guidelines and Resource Guide ().
Table 3. Obesity treatment guidelines and resource guide.
Conclusion
The results from the ACTION study demonstrate the need for treating obesity as a chronic and serious disease and according to the current treatment guidelines. Identifying PwO in need of obesity management, providing a diagnosis, and ensuring the diagnosis is understood are necessary precursors to initiating the discussion with PwO about the disease, its impacts, and its treatment. Bringing up obesity is essential as PwO tend to view their condition as one that they are responsible for managing on their own; however, as with most other chronic conditions, the primary care provider can best guide the disease and treatment conversation. Although HCPs may think obesity is a sensitive topic for their patients, PwO are motivated to address their obesity and are comfortable discussing it. Setting appropriate expectations with PwO and managing obesity with a focus on outcomes important to PwO in addition to addressing comorbid conditions may be a successful approach as PwO were focused on the general health benefits of weight loss. Making follow-up appointments for obesity management allows for more adequate time to address this complex disease and will likely convey a sense of importance to patients. Helping PwO set weight loss goals outlined in the guidelines and providing individualized treatment plans including lifestyle and behavioral modifications, as well as pharmacotherapy and referrals for bariatric surgery as appropriate should help increase the chances of effective obesity management. Directions for future research include studying pairs of PwO and HCPs for a more direct comparison and evaluation of the effectiveness of educational/training programs for HCPs specializing in obesity care regarding the implementation of current guidelines.
Declaration of interest
M Look reports receipt of an honorarium from Novo Nordisk as part of the ACTION study steering committee as well as speakers’ fees as part of Novo Nordisk speakers’ bureau. RL Kolotkin reports consulting fees from Novo Nordisk during the conduct of this study and consulting fees form Novo Nordisk outside the submitted work. NV Dhurandhar reports personal fees from Novo Nordisk during the conduct of the study and personal fees from Novo Nordisk outside the submitted work. A Golden reports personal fees from Novo Nordisk as part of the ACTION study steering committee as well as speaker’s fees as part of Novo Nordisk speakers’ bureau, from Takeda as part of its speakers’ bureau, and from Sanofi as a consultant. J Nadglowski is an employee of the Obesity Action Coalition which is supported by Novo Nordisk. Dr. Stevenin is an employee of Novo Nordisk. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US Adults, 1999-2010. Jama. 2012 2012/02/01/;307(5):491–497.
- Flegal KM, Kruszon-Moran D, Carroll MD, et al. Trends in Obesity Among Adults in the United States, 2005 to 2014. Jama. 2016 2016/06/07/;315(21):2284–2291.
- Wang YC, McPherson K, Marsh T, et al. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011 2011/09/02/;378(9793):815–825.
- Withrow D, Alter DA. The economic burden of obesity worldwide: a systematic review of the direct costs of obesity. en Obesity Rev. 2011 2011/02/01/;122:131–141.
- Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J Health Econ. 2012 2012/01//;31(1):219–230.
- Finkelstein EA, Trogdon JG, Cohen JW, et al. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff. 2009 2009/09/01/;28(5):w822–w831. en.
- Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes. 2017 Oct;7(5):273–289. PubMed PMID: 28695722; PubMed Central PMCID: PMCPMC5600094. eng.
- Jastreboff AM, Kotz CM, Kahan S, et al. Obesity as a disease: The Obesity Society 2018 position statement. Obesity. 2019 Jan;27(1):7–9.
- Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 20092009/05/01/;175:941–964. en.
- Puhl RM, Heuer CA. Obesity Stigma: important Considerations for Public Health. Am J Public Health. 20102010/06/01/;100(6):1019–1028.
- Kirk SFL, Price SL, Penney TL, et al. Blame, Shame, and Lack of Support: A Multilevel Study on Obesity Management. Qual Health Res. 20142014/06/01/;246:790–800. en.
- Moorhead SA, Coates VE, Gallagher AM, et al. Obesity communication among patients by health professionals: findings from the Weight Care Project. Health. 2013 2013/08/13/;2013. en. 10.4236/health.2013.58A3015
- Potter MB, Vu JD, Croughan-Minihane M. Weight management: what patients want from their primary care physicians. J Fam Pract. 2001;50(6):513–518.
- Puhl RM, Moss-Racusin CA, Schwartz MB, et al. Weight stigmatization and bias reduction: perspectives of overweight and obese adults. Health Educ Res. 2008 2008/04/01/;23(2):347–358.
- Phelan SM, Burgess DJ, Yeazel MW, et al. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obesity Rev. 2015;16(4):319–326. PubMed PMID: PMC4381543.
- Bertakis KD, Azari R. The Impact of Obesity on Primary Care Visits. en Obes Res. 20052005/09/01/;139:1615–1623.
- Hebl MR, Xu J. Weighing the care: physicians’ reactions to the size of a patient. Int J Obes Relat Metab Disord. 2001 Aug;25(8):1246–1252. . PubMed PMID: 11477511; eng.
- Østbye T, Taylor DH Jr, Yancy WS Jr, et al. Associations between obesity and receipt of screening mammography, papanicolaou tests, and influenza vaccination: results from the Health and Retirement Study (HRS) and the Asset and Health Dynamics Among the Oldest Old (AHEAD) Study. Am J Public Health. 2005;95(9):1623–1630. PubMed PMID: 16051935.
- Aldrich T, Hackley B. The impact of obesity on gynecologic cancer screening: an integrative literature review. J Midwifery Women’s Health. 2010 Jul-Aug;55(4):344–356. . PubMed PMID: 20630361; eng.
- Ma J, Xiao L, Stafford RS. Adult Obesity and Office-based Quality of Care in the United States. Obesity. 2009;17(5):1077–1085.
- Bleich SN, Pickett-Blakely O, Cooper LA. Physician practice patterns of obesity diagnosis and weight-related counseling. Patient Educ Couns. 2011;821:123–129. PubMed PMID: 20303691.
- Volpp KG, Mohta NS. Patient Engagement Survey: the Failure of Obesity Efforts and the Collective Nature of Solutions. NEJM Catal. 2018. https://catalyst.nejm.org/failure-obesity-efforts-collective/
- Jensen MD, Ryan DH, Apovian CM, et al. AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2013 2014 Jun 24;129(25Suppl 2):S102–38. PubMed PMID: 24222017; eng.
- Garvey WT, Mechanick JI, Brett EM, et al. American Association of Clinical Endocrinologists and American College Of Endocrinology comprehensive clinical practice guidelines for medical care of patients with obesity. Endocr Pract. 2016 2016/05/24/;22(Supplement 3):1–203.
- Bays HE S J, Primack C, Long J, et al. Obesity Algorithm, presented by the Obesity Medicine Association. 2017-2018 [cited 2018 May 9]. Available from: www.obesityalgorithm.org
- Turner M, Jannah N, Kahan S, et al. Current knowledge of obesity treatment guidelines by health care professionals. Obesity (Silver Spring, Md). 2018 Apr;26(4):665–671. PubMed PMID: 29570250; eng.
- Kushner RF. Clinical assessment and management of adult obesity. Circulation. 2012 Dec 11;126(24):2870–2877. PubMed PMID: 23230316; eng.
- Frühbeck G, Sbraccia P, Nisoli E, et al. 2015 Milan Declaration: A Call to Action on Obesity - an EASO Position Statement on the Occasion of the 2015 EXPO. Obes Facts. 2016;9(4):296–298. PubMed PMID: 27577870; eng.
- Kaplan LM, Golden A, Jinnett K, et al. Perceptions of Barriers to Effective Obesity Care: results from the National ACTION Study. Obesity (Silver Spring). 2018 Jan;26(1):61–69. PubMed PMID: 29086529.
- Jinnett K, Kyle T, Parry T, et al. Insights into the role of employers supporting obesity management in people with obesity: results of the National ACTION Study. Popul Health Manag. 2018 Oct 31; PubMed PMID: 30383482; eng. 10.1089/pop.2018.0133.
- Copernicus Group Independent Review Board [cited September 2015]. Available from: http://www.cgirb.com/
- Stommel M, Schoenborn CA. Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001-2006. BMC Public Health. 2009;9:421. PubMed PMID: 19922675; eng.
- Akhtar-Danesh N, Dehghan M, Merchant AT, et al. Validity of self-reported height and weight for measuring prevalence of obesity. Open Med. 2008;2(3):e83–e88. PubMed PMID: 21602953; eng.
- Krul AJ, Daanen HAM, Choi H. Self-reported and measured weight, height and body mass index (BMI) in Italy, the Netherlands and North America. Eur J Public Health. 2010;21(4):414–419.
- World Health O. Obesity: preventing and managing the global epidemic: report of a WHO consultation. Geneva: World Health Organization; 2000. ( English).
- Kalton G. Introduction to Survey Sampling. First ed. SAGE University Paper series on Quantitative Applications in the Social Sciences, series no. 07-035. Beverly Hills and London: SAGE Publications, Inc.; 1983.
- United States Census Bureau. Summary File. 2007 – 2011 American Community Survey [Internet]. U.S. Census Bureau’s American Community Survey Office 2013. [cited 2015 Sept]. Available from: http://ftp2.census.gov/.
- SPSS. SPSS Statistics for Windows, Version 15.0.1. 15.0.1. Chicago IL: SPSS; 2008. Available from: http://www-01.ibm.com/support/docview.wss?uid=swg21476197
- StataCorp. Stata statistical software release: IC 14.1. College Station TX: StataCorp LP; 2015.
- Jensen MD, Ryan DH, Apovian CM, et al. AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the obesity society. J Am Coll Cardiol. 2014 2014/07/01/;63(25, Part B):2985–3023. 2013.
- Ely AC, Befort CA, Duncan AB, et al. A chronic care model program incorporating group office visits for obesity treatment in primary care. Kans J Med. 2011 2011-11-23;4(4):87–98.
- Jebb SA, Lang R, Penrose A. Improving communication to tackle obesity in the UK. Proc Nutr Soc. 2007;62(3):577–581.
- Durant NH, Bartman B, Person SD, et al. Patient provider communication about the health effects of obesity. Patient Educ Couns. 2009;75(1):53–57.
- Stokes A, Collins JM, Grant BF, et al. Prevalence and determinants of engagement with obesity care in the United States. Obesity. 2018. DOI: 10.1002/oby.22173.
- Foster GD, Makris AP, Bailer BA. Behavioral treatment of obesity. Am J Clin Nutr. 2005;82(1):230S–235S.
- Foster GD, Wadden TA, Vogt RA, et al. What is a reasonable weight loss? Patients’ expectations and evaluations of obesity treatment outcomes. English J Consult Clin Psychol. 19971997;651:79–85.
- Matthews SM, Peden AR, Rowles GD. Patient-provider communication: understanding diabetes management among adult females. Patient Educ Couns. 2009 Jul;76(1):31–37. . PubMed PMID: 19157762; eng.
- Fitzpatrick SL, Wischenka D, Appelhans BM, et al. An evidence-based guide for obesity treatment in primary care. Am J Med. 2016 Jan;129(1):115.e1-7. PubMed PMID: 26239092; PubMed Central PMCID: PMCPmc5988348. eng.
- Gutnick D, Reims K, Davis C, et al. Brief action planning to facilitate behavior change and support patient self-management. Journal of Clinical Outcomes Management. 2014;21(1):17–29.
- Fitzpatrick SL, Wischenka D, Appelhans BM, et al. An evidence-based guide for obesity treatment in primary care. Am J Med. 2015;129(1):115.e1-115.e7.