ABSTRACT
Objectives: We examined the relationship between the initial treatment of acute lower and upper tract respiratory infections with phytopharmaceuticals and the duration of the disease as well as between the initial treatment and the use of antibiotics in the further course of the disease.
Method: Outpatients from the IMS® Disease Analyzer database with diagnoses of acute respiratory infections between January 2015 and March 2019 were observed for 30 days. Patients who had been prescribed phytopharmaceuticals on the day of their diagnosis were matched with controls who had not received such prescriptions by treating practice, diagnosis, age, sex, insurance status, index year, and Charlson comorbidity score. Patients antibiotic precriptions on the day of diagnosis were excluded. Logistic regression was used to investigate the relationship between phytopharmaceutical prescription, antibiotic prescription in the further course of the disease, and duration of sick leave.
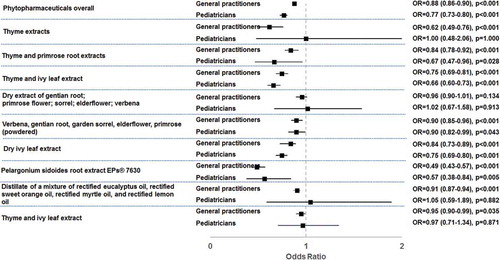
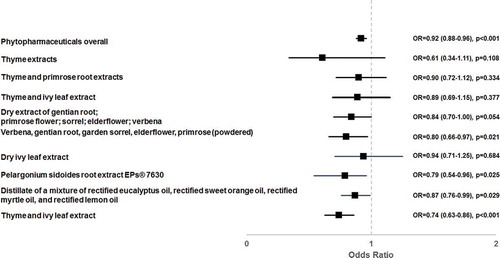
Results: A total of 117,182 patients who had been prescribed phytopharmaceuticals and an equal number of controls were available for analysis. Phytotherapeutics were associated with fewer antibiotic prescriptions. Extract of Pelargonium sidoides root (odds ratio (OR) 0.49 [0.43–0.57]) and thyme extract (OR 0.62 [0.49–0.76]) exhibited the strongest effect among patients treated by general practitioners, while Pelargonium sidoides root extract (OR 0.57 [0.38–0.84]), thyme and ivy extract (OR 0.66 [0.60–0.73]), and thyme and primrose root extract (OR 0.67 [0.47–0.96]) proved most effective in pediatric patients. Patients receiving phytopharmaceuticals had a significantly lower risk of prolonged periods of sick leave. The risk of sick leave durations of >7 days was most markedly reduced in patients taking cineole (OR 0.74 [0.63–0.86]) and Pelargonium root extract (OR 0.79 [0.54–0.96]).
Conclusion: The use of selected phytopharmaceuticals for acute respiratory infections is associated with a significantly reduced need for antibiotic prescriptions in the further course of the disease, as well as significantly shorter sick leaves.
Introduction
Acute lower and upper tract respiratory infections are among the most frequent reasons for visits to general and pediatric practices as well as for sick leave [Citation1,Citation2]. Many patients expect their physician to prescribe them an antibiotic [Citation3,Citation4]. Often, antibiotics are indeed prescribed, even though the conditions are mostly viral and self-limiting [Citation5,Citation6]. These prescriptions comply with current recommendations in only 25% of cases [Citation5–8]. Inappropriate prescriptions of antibiotics are ineffective, wasteful, cause side effects, and contribute to increasing bacterial resistance to antibiotics [Citation9]. Therefore, strategies are urgently needed to reduce the use of antibiotics in primary care [Citation10,Citation11].
Various phytopharmaceuticals have been approved in different countries including Germany for the treatment of acute lower and upper tract respiratory infections. Their efficacy and safety have been demonstrated in placebo-controlled clinical trials [Citation12–16]. The use of such phytopharmaceuticals could contribute to a reduction in the number of inappropriate antibiotic prescriptions for lower and upper tract respiratory infections, but further evidence is needed to corroborate this [Citation17].
Therefore, we systematically examined whether the prescription of the most commonly used phytopharmaceuticals to treat acute lower and upper tract respiratory infections is associated with lower antibiotic use as the disease progresses. Since the duration of the disease is a common reason for prescribing antibiotics [Citation18,Citation19], we also examined the effects of the use of phytopharmaceuticals on the duration of the disease.
Methods
The present retrospective analysis was carried out using the IMS® Disease Analyzer database, which contains case-related information such as demographic patient data, diagnoses, drug prescriptions, sick days, and referrals to hospitals made available by physicians in private practice in Germany. The database covers about 3% of all practices (approx. 3,000 practices), and its representativeness and validity has been demonstrated in the past [Citation20].
The analysis included all outpatients of general practitioners, pediatricians, and ENTs who had received at least one diagnosis of an acute lower and upper tract respiratory infection (see eSupplement for relevant ICD-10 diagnoses-) between 1 January 2015 and 31 March 2019. The first diagnosis documented during this period was defined as the index date. Only patients who had been observed for a period of at least 12 months prior to the index date were included. Patients with a prescription for antibiotics (ATC code: J01) at the index date or in the 90 days prior to the index date and patients diagnosed with a bacterial infection (see eSupplement for relevant ICD-10 diagnoses) in the 90 days prior to the index date were excluded from the study.
The endpoints of the study were as follows: at least one antibiotic prescription (ATC- code: J01) in the course of the disease (days 2–30 after the index date) and duration of sick leave. In addition, we investigated newly documented bacterial infections (see eSupplement for relevant ICD-10 diagnoses) in the course of the disease.
The most common approved (ATC codes R01 to R05) and prescribed (> 5,000 prescriptions) phytopharmaceuticals according to the IMS® Disease Analyzer database were selected and grouped by the active ingredient mentioned in the prescribing information. In the ATC code list, cineole is classified as R04AX04 and R05CA13 and thus not as a phytopharmaceutical. However, we included it in the analysis because, according to the prescribing information, the active ingredient is derived from eucalyptus oil.
Each patient who had been prescribed a phytopharmaceuticals at the index date was matched (full matching) 1:1 with a randomly selected patient without such a prescription, using the following variables: age, sex, insurance status, index year, treating practice, cold diagnosis, and Charlson Comorbidity Index score [Citation21].
We calculated descriptive statistics following the propensity score matching and tested group differences (phytopharmaceutical vs. no phytopharmaceutical) using the Wilcoxon test and McNemar’s test.
We investigated the association between the prescription of phytopharmaceuticals and a subsequent prescription of an antibiotic by means of univariate logistics regression models and provided the results as an odds ratio (OR), stratified separately for each medical specialty by active plant-based ingredients. We compared patients treated with each individual active ingredient with their own matched pairs.
We included only patients of general practitioners between the ages of 20 and 60 years in the examination of the duration of sick leave and excluded retirees. Since the sick leave duration was not normally distributed and the most frequent sick leave duration was three days, we used univariate logistic regression models to assess the association between the use of phytopharmaceuticals and the duration of sick leave as binary variables (longer than 3, 7, 10, 14, 18, 21, or 28 days).
We considered a p-value of < 0.05 statistically significant. All analyses were carried out on the basis of a pre-established study protocol, using SAS Version 9.4.
The analysis was funded by Dr. Willmar Schwabe GmbH & Co. KG, 76227 Karlsruhe, Germany.
German law allows the use of anonymous electronic medical records for research purposes under certain conditions. According to this legislation, it is not necessary to obtain informed consent from patients or approval from a medical ethics committee for this type of observational study that contains no directly identifiable data. Because patients were only queried as aggregates and no protected health information was available for queries, no IRB approval was required for the use of this database or the completion of this study.
Results
Selection of study patients
Of 3,671,077 patients diagnosed with a cold, antibiotics were prescribed on the day of diagnosis in 417,153 (25.7%) of 1,625,000 patients with at least one year of prior observation. A total of 1,169,168 patients met all inclusion criteria, 173,226 (14.8%) of whom received a prescription for a phytopharmaceutical on the day of diagnosis. After matching, 117,182 patients who had received phytopharmaceutical prescriptions and the same number of controls were available for analysis (). The 1:1 matching procedure resulted in the loss of approximately 30% of the original patient population, since a match with the same variable manifestation was not found for each patient.
The majority of study patients were treated by general practitioners (67%) and pediatricians (28%). ENT physicians treated only 5.5% of patients and were therefore not considered in subsequent analyses.
Characteristics of study patients
After 1:1 matching, patients with and without phytopharmaceutical prescriptions did not differ with regard to demographics and diagnoses. Patients of general practitioners were on average 43 years old, 9.4% of them were children or adolescents, and 56.1% of them were female. The only common diagnosis, affecting 49.5% of patients, was ICD-10: J06 (Acute upper respiratory infections of multiple and unspecified sites) (). Pediatric patients were on average 7.2 years old, and 49.3% were female. Again, the only common diagnosis, affecting 53.9% of them was ICD-10: J06 (Acute upper respiratory infections of multiple and unspecified sites).
Table 2. Basic characteristics of study patients by physician group
shows the prescribed phytopharmaceuticals, usually combination preparations. General practitioners most often prescribed the distillate of a mixture of rectified eucalyptus oil, rectified sweet orange oil, rectified myrtle oil, and rectified lemon oil (27.7%), followed by extract of dried gentian root, primrose flower, sorrel, elderflower, and verbena (14.1%), as well as a powdered drug blend of verbena, gentian root, garden sorrel, elderflower, and primrose flower (12.7%). Pediatricians most frequently prescribed dried ivy leaf extract (46.7%), followed by thyme and ivy leaf extract (25.0%) and the powdered drug blend (20.0%).
Table 1. Phytopharmaceuticals prescribed on the day of diagnosis
Antibiotic therapy in patients with and without phytopharmaceutical prescriptions
Extract of Pelargonium sidoides root (odds ratio (OR) 0.49 [95% CI: 0.43–0.57]) and thyme extract (OR 0.62 [0.49–0.76]) exhibited the strongest effect among patients treated by general practitioners, while Pelargonium sidoides root extract (OR 0.57 [0.38–0.84]), thyme and ivy extract (OR 0.66 [0.60–0.73]), and thyme and primrose root extract (OR 0.67 [0.47–0.96]) proved most effective in pediatric patients ()
Duration of sick leave in patients with and without phytopharmaceutical prescriptions
Phytopharmaceutical prescription on the day of diagnosis was significantly associated with fewer long sick leaves (>7 days: OR 0.92, p < 0.001; >10 days: OR 0.88, p < 0.001; >14 days: OR 0.84, p < 0.001; >18 days: OR 0.82, p < 0.001; >21 days: OR 0.83, p < 0.001). The effect on a sick leave period of more than 7 days was significant for several phytopharmaceuticals (). The strongest associations were found for cineole (OR 0.74 [0.63–0.86]) and the Pelargonium root extract EPs® 7630 (OR 0.79 [0.54–0.96]).
Documented diagnoses of bacterial infections in patients with and without phytopharmaceutical prescriptions
Additional bacterial infections, as a complication of the lower and upper tract respiratory tract infection, were only rarely documented in the further course of the disease. Only 225 patients treated by general practitioners and 782 patients treated by pediatricians were diagnosed with such infections. There were no significant differences in the proportions of patients with bacterial infections between patients with and patients without phytopharmaceutical prescriptions (0.14% of the phytopharmaceutical cohort versus 0.15% of the control cohort in general practices and 1.16% versus 1.16% in pediatric practices).
Discussion
This retrospective study, based on a large national sample of more than 230,000 patients, resulted in important findings regarding the use of phytopharmaceuticals in the treatment of patients with acute lower and upper tract respiratory infections. Phytotherapeutic prescriptions were significantly associated with reduced antibiotic use in the further course of the disease and with shorter sick leave duration.
These findings are not unexpected, since the efficacy of the phytopharmaceuticals examined in this study had already been demonstrated in placebo-controlled clinical trials [Citation12–16] and has now been confirmed by data from actual practices. In vitro anti-infective effects have been described for various active herbal ingredients [Citation22–25]. A possible explanation for the reduced antibiotic use following phytotherapeutic prescriptions could therefore be the occurrence of fewer bacterial sequelae of respiratory tract infections. While we were unable to confirm this hypothesis based on our data, bacterial sequelae were coded by the treating physicians in only 0.9% of cases. Other cohort studies have also only rarely found bacterial complications of acute respiratory infections [Citation26,Citation27]. The rate of bacterial complications, therefore, is not a suitable parameter for measuring the potential anti-infective effect of phytopharmaceuticals. Disease duration may be a better suited parameter for the purpose.
Depending on the active ingredient, phytopharmaceuticals have mucolytic, antiviral, antibacterial, secretolytic, anti-inflammatory, or immunomodulating properties. Complex mechanisms mediate mucolytic effects, a decrease in mucus viscosity, as well as a decrease in the intensity and frequency of the cough. They also promote relaxation of the bronchial musculature [Citation12–16].
The duration of the disease is a frequent reason for the prescription of antibiotics by general practitioners [Citation18]. The fact that fewer antibiotics were prescribed in the phytopharmaceutical group could thus be due to a faster improvement of cold symptoms, as previously described in placebo-controlled studies: Fischer & Dethlefsen reported that the symptoms of bronchitis patients improved significantly faster under treatment with cineole than in the placebo group [Citation28]. The same has been demonstrated for Pelargonium root extract EPs® 7630 [Citation12]. Faster improvement of symptoms has also been demonstrated for the treatment of sinusitis with extract of dry gentian root, primrose flower, sorrel, elderflower, and verbena [Citation14].
The above hypothesis is supported by the fact that, in our study, the prescription of phytopharmaceuticals was significantly associated with a reduced risk of sick leave of more than 7, 10, 14, 18, and 21 days, which is also consistent with the results of placebo-controlled studies. In a meta-analysis, adults treated with Pelargonium root extract EPs® 7630 were significantly more likely to be able to go back to work on day seven, and children and adolescents had a two to four times greater chance of returning to school or kindergarten on day seven [Citation12].
General practitioners often prescribe antibiotics because they cannot reliably distinguish between bacterial and viral infections in everyday practice and they want to prevent serious bacterial complications [Citation29]. Our finding that bacterial complications were not diagnosed more frequently in patients treated with phytotherapeutics than in the control group, although fewer antibiotics were prescribed, may provide reassurance that even initial treatment with a phytopharmaceutical does not increase the risk for already very rare bacterial complications.
Retrospective database analyses pertaining to primary care are generally limited by the validity and completeness of the data on which they are based. The following limitations of the IMS® Disease Analyzer database should be considered when interpreting the data:
Phytopharmaceuticals are available over the counter in Germany. It can thus be assumed that many patients self-medicate with phytopharmaceuticals. The comparison group can clearly be defined as consisting of patients who did not receive phytopharmaceutical prescriptions, but we cannot say with certainty that they did not use phytopharmaceuticals anyway. All diagnoses are based on the routine documentation entered by the treating physician, who used nonspecific ICD-10 codes in most cases. A certain vagueness of the coded diagnoses can therefore be assumed. Due to the anonymity of the database, we cannot rule out that patients received diagnoses or prescriptions from other physicians.
Above all, we do not know why the same physician prescribed phytopharmaceuticals for one patient but not for a comparable patient. There may have been differences in symptoms, severity, and/or duration of the disease or with regard to undocumented risk factors [Citation17]. Patient preferences may have also played a role. However, this information is not available in the database. Therefore, based on the data available to us, we cannot make conclusive statements as to the extent to which the observed differences in the use of antibiotics and the duration of the disease are due to the active ingredients used or to differences in the patients treated. However, since the efficacy of all active ingredients that showed a positive association in our study was demonstrated in placebo-controlled clinical trials, we believe that pharmacological effects contributed to the differences [Citation12–16].
Conclusion
The use of selected phytopharmaceuticals in acute lower and upper tract respiratory tract infections can significantly reduce the need for antibiotic prescriptions in the further course of the disease as well as the duration of sick leave. Phytopharmaceuticals should be used to reduce the use of antibiotics in primary care.
Declaration of interest
DM, MK, CCA declare that they have no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. KK is an employee of IQVIA.
Reviewers disclosure
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Supplemental Material
Download MS Word (12.9 KB)Supplementary Material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Kordt M. DAK-Gesundheit. DAK-Gesundheitsreport 2015. [cited 2019 Sep 20]. Available from: http://www.dak.de/dak/download/Vollstaendiger_bundesweiter_Gesundheitsreport_2015-1585948.pdf
- Gesundheitsberichterstattung des Bundes: Häufigste Diagnosen in Prozent der Behandlungsfälle in Arztpraxen in Nordrhein (Rang und Anteil). Gliederungsmerkmale: Jahre, Nordrhein, Geschlecht, ICD10, Arztgruppe. [cited 2019 Sept 20]. Available from: www.gbe-bund.de
- Coenen S, Francis N, Kelly M, et al. Are patient views about antibiotics related to clinician perceptions, management and outcome? A multi-country study in outpatients with acute cough. PLoS One. 2013;8(10):e76691.
- O’Connor R, O’Doherty J, O’Regan A, et al. Medical management of acute upper respiratory infections in an urban primary care out-of-hours facility: cross-sectional study of patient presentations and expectations. BMJ Open. 2019;9(2):e025396.
- Zweigner J, Meyer E, Gastmeier P, et al. Rate of antibiotic prescriptions in German outpatient care - are the guidelines followed or are they still exceeded? GMS Hyg Infect Control. 2018;13:Doc04.
- Ostermaier A, Barth N, Schneider A, et al. On the edges of medicine - a qualitative study on the function of complementary, alternative, and non-specific therapies in handling therapeutically indeterminate situations. BMC Fam Pract. 2019;20(1):55.
- Kraus EM, Pelzl S, Szecsenyi J, et al. Antibiotic prescribing for acute lower respiratory tract infections (LRTI) - guideline adherence in the German primary care setting: an analysis of routine data. PLoS One. 2017;12(3):e0174584.
- Linde K, Atmann O, Meer K, et al. How often do general practitioners use placebos and non-specific interventions? Systematic review and meta-analysis of surveys. PLoS One. 2018;13(8):e0202211.
- Bätzing-Feigenbaum J, Schulz M, Schulz M, et al. Outpatient antibiotic prescription: a population-based study on regional age-related use of cephalosporins and fluoroquinolones in Germany. Dtsch Arztebl Int. 2016;113:454–459.
- Salm F, Kramer T, Gastmeier P. Hausärzte müssen das Thema Antibiotika-Resistenzen angehen. MMW Fortschr Med. 2017;25:159–164.
- Richter-Kuhlmann E. Kampf gegen Antibiotikaresistenzen: Global und interdisziplinär. Dtsch Arztebl. 2017;114(5):A-210/B-190/C-190.
- Matthys H, Lehmacher W, Zimmermann A, et al. EPs 7630 in acute respiratory tract infections - a systematic review and meta-analysis of randomized clinical trials. J Lung Pulm Respir Res. 2016;3(1):415.
- Mousa HA. Prevention and treatment of influenza, influenza-like illness, and common cold by herbal, complementary, and natural therapies. J Evid Based Complementary Altern Med. 2017;22(1):166–174.
- Jund R, Mondigler M, Stammer H, et al. Herbal drug BNO 1016 is safe and effective in the treatment of acute viral rhinosinusitis. Acta Otolaryngol. 2015;135(1):42–50.
- Anheyer D, Cramer H, Lauche R, et al. Herbal medicine in children with respiratory tract infection: systematic review and meta-analysis. Acad Pediatr. 2018;18(1):8–19.
- Griffin AS, Cabot P, Wallwork B, et al. Alternative therapies for chronic rhinosinusitis: a review. Ear Nose Throat J. 2018;97(3):E25–E33.
- Baars EW, Zoen EB, Breitkreuz T, et al. The contribution of complementary and alternative medicine to reduce antibiotic use: a narrative review of health concepts, prevention, and treatment strategies. Evid Based Complement Alternat Med. 2019:5365608.
- Lum EPM, Page K, Whitty JA, et al. Antibiotic prescribing in primary healthcare: dominant factors and trade-offs in decision-making. Infect Dis Health. 2018;23:74–86.
- Salm F, Schneider S, Schmücker K, et al.; RAI-Study Group. Antibiotic prescribing behavior among general practitioners - a questionnaire-based study in Germany. BMC Infect Dis 2018;18(1):208.
- Rathmann W, Bongaerts B, Carius HJ, et al. Basic characteristics and representativeness of the German disease analyzer database. Int J Clin Pharmacol Ther. 2018;56(10):459–466.
- Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139.
- Tariq S, Wani S, Rasool W, et al. A comprehensive review of the antibacterial, antifungal and antiviral potential of essential oils and their chemical constituents against drug-resistant microbial pathogens. Microb Pathog. 2019;134:103580.
- Roth M, Fang L, Stolz D, et al. Pelargonium sidoides radix extract EPs 7630 reduces rhinovirus infection through modulation of viral binding proteins on human bronchial epithelial cells. PLoS One. 2019;14(2):e0210702.
- Glatthaar-Saalmüller B, Rauchhaus U, Rode S, et al. Antiviral activity in vitro of two preparations of the herbal medicinal product Sinupret® against viruses causing respiratory infections. Phytomedicine. 2011;19(1):1–7.
- Seibel J, Kryshen K, Pongrácz JE, et al. In vivo and in vitro investigation of anti-inflammatory and mucus-regulatory activities of a fixed combination of thyme and primula extracts. Pulm Pharmacol Ther. 2018;51:10–17.
- Cars T, Eriksson I, Granath A, et al. Antibiotic use and bacterial complications following upper respiratory tract infections: a populationbased study. BMJ Open. 2017;7:e016221.
- Moore M, Stuart B, Little P, et al. Predictors of pneumonia in lower respiratory tract infections: 3C prospective cough complication cohort study. Eur Respir J. 2017;50:5.
- Gillissen A, Wittig T, Ehmen M, et al. multi-centre, randomised, double-blind, placebo-controlled clinical trial on the efficacy and tolerability of GeloMyrtol® forte in acute bronchitis. Drug Res (Stuttg). 2013;63(1):19–27.
- Petursson P. GPs’ reasons for “non-pharmacological” prescribing of antibiotics A phenomenological study. Scand J Prim Health Care. 2005;23(2):120–125.