Introduction
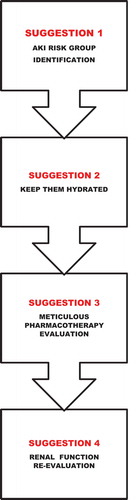
Acute kidney injury (AKI) is a heterogeneous group of conditions characterized by a sudden decrease in glomerular filtration rate (GFR), which usually induces the accumulation of nitrogenous-waste substances in the blood. It is expressed as an increase in serum creatinine levels (≥ 0.3 mg/dl within 48 hours or ≥1.5 times from baseline within the previous 7 days) or by a urine volume reduction of ˂0.5 ml/kg/h in 6 hours [Citation1]. AKI is a relevant condition since it is usually associated with 1–7% and 30–50% of hospital and intensive care unit (ICU) admissions, respectively; showing a significant morbidity-mortality rate, and progression to chronic kidney disease (CKD) [Citation1–7]. Even though many strategies have been proposed to achieve an early AKI diagnosis (e.g. novel biomarkers, informatics alarms), and an AKI effective treatment (e.g. renal protective drugs, biocompatible renal replacement therapies), both objectives remain unachieved; therefore, AKI prevention is currently the best ‘therapeutic’ strategy for this condition [Citation1–4]. As mentioned above, AKI prevention is currently the best medical approach to this syndrome. In this sense, Meersch et al. have demonstrated that the implementation of the KDIGO guidelines reduced the frequency and severity of AKI after cardiac surgery in high-risk patients [Citation8]. In addition, Malhotra. Koyner, Menon et al. have highlighted the potentially beneficial role of novel biomarkers and readily available electronic health record data to provide a timely and certain AKI diagnosis in hospitalized patients [Citation6,Citation7,Citation9]. As far as we know, there is practically no information regarding ambulatory AKI characteristics, nor a systematic approach that proposes how to achieve AKI primary prevention in ambulatory patients. Moreover, even though Samuel et al. described two ambulatory care programs for AKI patients after their hospital discharge, these programs constitute an AKI secondary prevention approach but not a primary one [Citation10]. Finally, the above mentioned AKI diagnosis means (novel biomarkers, health electronic bases, etc.) are not universally available and are even rarer in the ambulatory consult. Therefore, this article originally reviews how simple maneuvers could contribute to AKI primary prevention in the primary care field, where probably most of the undiagnosed and avoidable AKI occurs [Citation5]. It is worth pointing out that even though the series of AKI primary prevention maneuvers here proposed are not evidence based, they are strongly based on the currently known AKI pathophysiology ():
Suggestion 1: identification of AKI susceptible patient
Ambulatory patients susceptible to developing AKI should be identified in order to try to preserve their renal function. AKI susceptible patients are those who have renal structural and functional alterations which predispose them to developing AKI (fragile kidney), or those who have a clinical condition that can damage their kidneys (renal adverse condition). Nonetheless, the numerous clinical scores, computerized algorithms, and renal functional studies (e.g. furosemide test) which have been proposed to determine patient´s AKI risk are usually based on expensive biomarkers, laboratory parameters or physiological tests not frequently available in the ambulatory consult [Citation6–9,Citation11]. Due to this reason, the main patient´s characteristics and conditions which suggest AKI susceptibility, and can be easily detected at the ambulatory consult are listed below [Citation1,Citation5,Citation12]:
a) Fragile kidney ● age ≥ 65 years old ● chronic kidney disease – proteinuria ● diabetes mellitus ● long-term hypertension
b) Renal adverse conditions ● advanced chronic cardiac, hepatic or respiratory insufficiency (renal hypoperfusion) ● significant anemia: hemoglobin < 11 g/L (renal hypoxia) ● septic status (renal hypoperfusion) ● rhabdomyolysis (tubular damage) ● oncologic patient on chemotherapy (tubular damage)
Suggestion 2: encourage patients to keep themselves adequately hydrated
Dehydration is one of the most prevalent AKI inducing mechanisms, particularly in older individuals. Therefore, it is crucial to encourage them and their caregivers (if they are assisted by one) to keep themselves and the patient, respectively, adequately hydrated. This is particularly relevant for those who are frail, live in warm climates, or have reduced access to water (immobility syndrome). Physical examination suggestive of hypovolaemia, along with a history of recent vomiting or diarrhea, use of diuretics, or hypernatremia should prompt the diagnosis of dehydration. However, it is important to be aware that in many cases the traditional signs of volume depletion may be difficult to detect in the older individuals. Moreover, dry mouth and skin, orthostatic hypotension and skinfold are all signs usually found in healthy older adults, not necessarily meaning a state of dehydration. It is worth mentioning that axillary dryness is the most reliable clinical sign of dehydration in this group [Citation13]. Since daily body water requirement is around 35 cc/kg, the objective of keeping ambulatory patients adequately hydrated can be achieved by promoting a programmed daily fluid intake of around 1500–2000 cc. Of course, this recommendation should be adjusted to each patient´s clinical situation, since some patients could require higher water supply (fever, diarrhea, diabetes insipidus, etc.) while others could require lower water supply (heart failure or cirrhosis with hyponatremia, renal insufficiency, etc.) [Citation13]. It is worth pointing out that older individuals are especially predisposed to developing dehydration. This can be explained by, at least, two physiological changes attributed to aging: increased thirst threshold, and reduced water reabsorption capability in the collecting tubules due to medulla hypotonicity [Citation13]. When dehydration and/or hypovolemia is detected, these conditions must be corrected quickly and effectively in order to avoid its deleterious effect. Adequate rehydration (oral or intravenous) will depend on the degree of dehydration [Citation1]. In addition, it is important to point out that a salt and water overload status should also be avoided in this population. This is particularly relevant in older individuals since they usually have aging induced cardiac diastolic dysfunction, and can develop heart failure, and consequently AKI [Citation1,Citation13].
Suggestion 3: meticulous pharmacotherapy evaluation
A meticulous pharmacotherapy evaluation should be regularly performed in every patient especially when prescribed potentially nephrotoxic drugs () [Citation5–8]. Regarding drug prescription, the smallest possible amount of drugs should be prescribed and whenever possible, nephrotoxic drugs should not be associated. Before prescribing any drug, dosage should be evaluated according to its pharmacodynamic and pharmacokinetic characteristics (age, liver function, glomerular filtration rate, etc.) in order to avoid drug toxicity. This recommendation becomes even more crucial when nephrotoxic drugs are prescribed in the aforementioned AKI susceptible subgroups. When a nephrotoxic drug is absolutely needed, its renal damaging effect should be mitigated by minimizing its duration and dose, monitoring therapeutic levels (if possible and useful) and evaluating concomitant drugs administration to detect nephrotoxic interactions [Citation1,Citation2,Citation8–17]. In addition, drugs number and dose adjustment to avoid polypharmacy (≥4 prescribed drugs) and prevent nephrotoxicity are critically important. For this purpose, discontinuation of unnecessary prescriptions (deprescription) should be performed at each consult [Citation1,Citation7]. Additionally, it should be taken into account that some drugs, such as quinolones, potent diuretics (loop diuretics, thiazides), and proton pump inhibitors, can induce AKI not due to toxicity, but to acute interstitial nephritis [Citation8]. It is worth mentioning that when diagnostic studies based on iodinated radiocontrast media are required (contrasted imaging, angiography, etc.), iso-osmolar or low-osmolar contrast media with intravenous volume expansion (isotonic sodium chloride or sodium bicarbonate solution) should be prescribed. Besides, a careful drug evaluation that may increase the risk of renal damage should take place a-priori. In this case, drugs such as non-steroidal anti-inflammatory drugs (NSAIDs) may be replaced (or discontinued if they are non-essential) by non-nephrotoxic alternative drugs (e.g. opioids) until the procedure has been completed. This strategy is crucial in every patient, but becomes mandatory in the AKI susceptible subgroups [Citation1,Citation5–7]. Finally, laxatives should not contain sodium phosphate, due to the risk of inducing AKI.
Table 1. Main nephrotoxic drugs in ambulatory patients
Suggestion 4: renal function revaluation
Aside from advanced renal insufficiency, renal damage is characteristically asymptomatic. Therefore, renal function should be monitored by measuring serum creatinine level in those individuals taking nephrotoxic drugs, especially if they are susceptible to AKI. The frequency of this renal monitoring in the ambulatory patient should be individualized, since it depends on the renal toxicity of the drug and the degree of renal functional deterioration; varying between monthly to yearly. Regarding the radiocontrast-based studies (imaging or angiography), serum creatinine measurement should be performed 48 hours after the procedure, and in the case of an angiography, it should also be performed a week after the procedure [Citation1,Citation2,Citation9,Citation11]. This recommendation is based on the following facts: contrast-induced renal damage can be usually detected 48 hours after its infusion, while post-angiography atheroembolic renal damage can be detected a week after it. This is the lapse in which the atheroembolism induced immunologic renal damage can reduce renal function [Citation18,Citation19]
Conclusion
Simple maneuvers such as keeping patients well hydrated and performing meticulous medication review could help to primary prevent many cases of acute kidney injury in ambulatory patients.
Declaration of interest
The contents of the paper and the opinions expressed within are those of the authors, and it was the decision of the authors to submit the manuscript for publication.
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
References
- KDIGO Clinical Practice. Guideline for Acute Kidney Injury. Kidney Int Suppl. 2012;2(Supplement 1):124–138.
- Blanco VE, Hernandorena CV, Scibona P, et al. Acute kidney injury pharmacokinetic changes and its impact on drug prescription. Healthcare (Basel). 2019 Jan 14;7(1):E10.
- Musso CG, Terrasa S, Ciocchini M, et al. Looking for a better definition and diagnostic strategy for acute kidney injury: a new proposal. Arch Argent Pediatr. 2019 Feb 1;117(1):4–5.
- Musso C, Aguilera J, Otero C, et al. Informatic nephrology. Int Urol Nephrol. 2013 Aug;45(4):1033–1038.
- Negi S, Koreeda D, Kobayashi S, et al. Acute kidney injury: epidemiology, outcomes, complications, and therapeutic strategies. Semin Dial. 2018 Sep;31(5):519–527.
- Malhotra R, Siew E. Biomarkers for the early detection and prognosis of acute kidney injury. Clin J Am Soc Nephrol. 2017 Jan 6;12(1):149–173.
- Koyner J, Adhikari R, Edelson D, et al. Development of a multicenter ward–based AKI prediction model. Clin J Am Soc Nephrol. 2016 Nov 7;11(11):1935–1943. Published online 2016 Sep 15.
- Meersch M, Schmidt C, Hoffmeier A, et al. Prevention of cardiac surgery-associated AKI by implementing the KDIGO guidelines in high risk patients identified by biomarkers: the PrevAKI randomized controlled trial. Intensive Care Med. 2017;43(11):1551–1561. Published online 2017 Jan 21
- Koyner J, Davison D, Brasha-Mitchell E, et al. Furosemide stress test and biomarkers for the prediction of AKI severity. J Am Soc Nephrol. 2015 Aug;26(8):2023–2031. Published online 2015 Feb 5
- Silver SA, Goldstein SL, Harel Z, et al. Ambulatory care after acute kidney injury: an opportunity to improve patient outcomes. Can J Kidney Health Dis. 2015;(2):36. Published online 2015 Oct 6.
- Menon S, Goldstein S, Mottes T, et al. Urinary biomarker incorporation into the renal angina index early in intensive care unit admission optimizes acute kidney injury prediction in critically ill children: a prospective cohort study. Nephrol Dial Transplant. 2016 Apr;31(4):586–594. Published online 2016 Feb 2
- Chao C-T, Tsai H-B, Chiang C-K, et al., COGENT study group. Acute kidney injury as a risk factor for diagnostic discrepancy among geriatric patients: a pilot study. Sci Rep. 2016;6:38549. Published online 2016 Dec 16.
- Musso CG, Vilas M. Water, electrolyte, and acid-base disorders in the elderly. In: Musso CG, Jauregui JR, Macías-Núñez JF, et al., editors. Clinical nephrogeriatrics. An evidence-based guide. Cham: Springer; 2019. p. 43–62.
- Musso CG, Vilas M. Nephroprevention in very old patients. Rev Colomb Nefrol. 2015;2(2):131–136.
- De Broe ME, Porter GA, Bennett WM, et al. Clinical nephrotoxins. Renal injury from drugs and chemicals. New York: Springer; 2008.
- Levey AS, James MT. Acute Kidney Injury. Ann Intern Med. 2018 Jun 5;168(11):837.
- Chawla LS, Bellomo R, Bihorac A, et al. Acute disease quality initiative workgroup 16. Acute kidney disease and renal recovery: consensus report of the acute disease quality initiative (ADQI) 16 workgroup. Nat Rev Nephrol. 2017 Apr;13(4):241–257.
- Rennke H, Denker B. Renal pathophysiology. Phiadelphia: Lippincott Williams & Wilkins; 2007.
- Market Juri A. Prevention of kidney disease: is it a reachable chimera? Rev Colomb Nefrol. 2016;3(1):1–3.