ABSTRACT
In real practice, there is a paradox in the management of patients with ‘long-term Covid-19.’ Indeed, Family physicians (FPs) are on the front line in the management process of these patients. For ‘long-term Covid-19’ patients, and according to the World Health Organization guideline, the cardiopulmonary rehabilitation (CPR) should be provided not only at tertiary- or secondary care but mainly at primary care with a real implication of FPs. However, specific guidelines/recommendations were addressed for FPs. Therefore, an alternative including the CPR minimal advice that an FP should provide to ‘long-term Covid-19’ patients, seems to be necessary to respond to the needs of FPs to face their involvement with ‘long-term Covid-19’ patients. Thus, this paper aimed to report the CPR ‘minimal advice’ that should be provided by FPs managing ‘long-term Covid-19’ patients with incapacity (i.e.; alteration of the cardiorespiratory and muscular chain). According to the authors, FPs should be more cautious in the prescription of exercise and nutrition program and informed about the minimal advices related to nutritional and physical exercise rehabilitation guidelines when taking care of ‘long-term Covid-19’ patients, and how these guidelines can relieve the mental and physical problems, improve immunity, and accelerate the recovery process of the patients. With the occurrence of new variants of the severe acute respiratory syndrome coronavirus 2, the nutritional and exercise rehabilitation guidelines implemented by FPs become indispensable to promote the recovery of Covid-19 patients and support a return to normal life.
Background
The coronavirus disease 19 (Covid-19) is a systemic disease, which induces several symptoms () [Citation1]. A Chinese study revealed that the disease can be mild (i.e.; no viral pneumonia or hypoxia signs) or moderate (i.e.; clinical signs of pneumonia) in 81% of cases, was severe (i.e.; need of oxygen therapy) in 14% of cases, and critical (e.g.; respiratory failure, multiple organ failure) in 5% of cases [Citation2]. Although vaccination and implementing of preventive healthcare measures (e.g.; quarantine, confinement, isolation, social distancing, lockdown) imposed by health authorities aim to prevent the decline of immunocompetence and mitigate the Covid-19 virus outbreak [Citation3], the aftermath of the Covid-19 pandemic may not only induce psychological problems [Citation4,Citation5] but also decrease physical activity behavior [Citation5,Citation6], increase sedentary time [Citation3], and alter the nutritional status in both the general population and patients [Citation7,Citation8]. On the one hand, a significant reduction in body cell mass and phase angle during the active infection with slow regression toward hospital discharge was reported [Citation8]. On the other hand, the mean unintended weight loss during hospitalization of patients with Covid-19 was 7.6%, and at discharge, 8.4% of patients were malnourished [Citation7].
Figure 1. Symptoms and signs of coronavirus disease 19 (Covid-19) and some acute/chronic complications linked with Covid-19 in the cardiorespiratory and neuro-muscular chain.
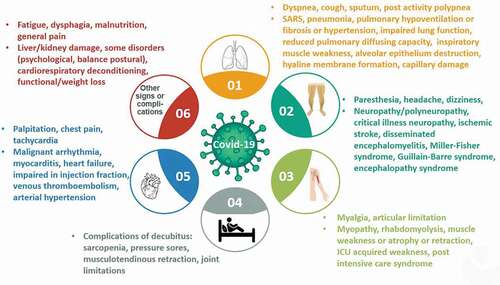
During the acute phase of Covid-19, different organs implicated during the adaptation to exercise can be affected (). First, the lung is the most affected organ by the coronavirus leading to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [Citation9]. Second, Covid-19 contributes to cardiovascular complications, including acute myocardial injury, and neuromuscular manifestations including myalgia [Citation9–11] (). Third, muscle alteration is an important predictive factor for the severity of Covid-19 [Citation12] that is majored by the consequences of a long period of rest prescribed by physicians for Covid-19 patients [Citation13] (). After a hospitalization period of 2–3 months, the physical performance of patients with moderate and severe Covid-19 was reduced (e.g.; grip strength decreased by 32%, 6-min walk distance decreased by 13%) [Citation14]. The issue with the Covid-19 is that even if patients are cured, 40% to 90% of them continue to experience numerous manifestations for weeks and months, and the disease is therefore named ‘long-term Covid-19’ [Citation15].
The ‘long-term Covid-19’ has several clinical manifestations: (i) the alteration of the cardiorespiratory and neuromuscular chain [Citation15], such as fatigue (58%), dyspnea (24%), post-activity polypnea (21%), cough (19%), chest pain/discomfort (16%), resting tachycardia (11%), palpitations (11%), general pain (11%), reduced pulmonary diffusing capacity (10%), pulmonary fibrosis (5%), sputum (3%), stroke (3%), arterial hypertension (1%), myocarditis (1%), and arrhythmia (0.4%), and (ii) the alteration of the nutritional status [Citation15] such as weight loss (12%). Hence, nutritional and exercise rehabilitation managements following the discharge of Covid-19 patients require attention and are necessary to overcome the pandemic situation [Citation16–21]. Nowadays, there are several guidelines related to the management of ‘long-term Covid-19’ patients [Citation16–21]. In these guidelines, nutritional rehabilitation and physical training rehabilitation are the cornerstones of the cardiopulmonary rehabilitation (CPR) program. In ‘long-term Covid-19’ patients, recent researches reported the effectiveness of a full program of CPR on lung function, psychological distress, cognitive impairment, exercise performance, and quality of life [Citation22–24]. According to the world health organization guideline, CPR should be provided for ‘long-term Covid-19’ patients mainly at primary‐care [Citation25]. In other words, a real implication of family physicians (FPs) is needed [Citation26]. The FPs need to be prepared to take care for patients presenting chronic manifestations of this complex disease [Citation26]. However, in real life, little documents related to the practice of CPR during the management of ‘long-term Covid-19’ patients were addressed for FPs [Citation16,Citation26,Citation27]. This is a conflicting and embarrassing situation for FPs. Consequently, the main aim of this letter to the Editor was to highlight the minimal advices related to the nutritional and physical exercise rehabilitation, which FPs should provide for their ‘long-term Covid-19’ patients. Combining nutrition rehabilitation with physical exercise rehabilitation for ‘long-term Covid-19’ patients is indispensable to resume the normal life and promote the physical and mental health recovery [Citation16–20].
Recommendations
Nutritional rehabilitation recommendations
In order to boost the immune system, discharged Covid-19 patients should restore muscle strength and provide the body with the necessary nutrients [Citation28]. Physician and rehabilitation experts from ‘Hospital for Special Surgery’ published a guideline freely available online [Citation28]. A summary of the 10 nutrition steps that should be communicated to ‘long-term Covid-19’ patients are detailed in Box 1. In brief, ‘long-term Covid-19’ patients should create and follow a routine and schedule for meals/snacks [Citation28]. This method will ensure they obtain the needed calories and nutrients, especially in case of anorexia. In order to keep appetite somewhat engaging, patients with ageusia can select foods with different textures (e.g.; crunchy, creamy). Patients with anosmia are encouraged to choose foods that can be eaten cold (e.g.; sandwiches, cold pasta salads or other grains, cottage cheese/Greek yogurt with fruit) [Citation28]. Then, patients need to obtain calories and pay specific consideration to take adequate protein throughout the day (Box 1). They should eat several nutrients that support immune function. Some guidance on science-based recommendations for nutrients (e.g.; Vitamin C, Vitamin D, Zinc, Calcium, Omega-3s, gut health, probiotics, and prebiotics) and the amounts to help ‘long-term Covid-19’ patients maintain a healthy immune system, are detailed in Box 1. In summary, ‘long-term Covid-19’ patients are stimulated to choose calcium-rich dairy or dairy alternatives, nutritious fats like olive oil, avocado, fish, and nuts, sufficiently of fruits and vegetables rich in Vitamin C and other nutrients [Citation28]. They should get enough Vitamin D to keep their levels in the appropriate range [Citation28]. Some other health issues need further attention from the FPs [Citation28]. First, FPs need to help ‘long-term Covid-19’ with diabetes mellitus to control their glycemia [Citation28]. Second, ‘long-term Covid-19’ patients with some chronic conditions (e.g.; heart disease, arterial hypertension, chronic respiratory diseases) may need individualized counseling [Citation28]. Third, in addition to the supplements outlined in Box 1, and especially in patients ≥ 65 years, three nutritional supplements can be considered (β-hydroxy-β-methyl butyrate, creatine, and tart cherry juice) [Citation28]. Fourth, it is useful that each ‘long-term Covid-19’ patient gets a weekly food diary. This would help in excluding allergies and/or food intolerances and will provide a better estimate of the total caloric content. Fifth, due to the long-term inflammatory environment to which ‘long-term Covid-19’ patients are exposed [Citation29], it is necessary to increase foods rich of anti-oxidants substances [e.g.; vegetables (pumpkin, eggplant, spinach), fruits (peaches, apple, grapes), non-vegetarian sources (egg, fish), whole grains (oats, brown rice), nuts (almonds, walnuts), herbs and species (ginger, garlic), and other sources (tea, coffee)] [Citation30]. For instance, in ‘long-term Covid-19’ patients with identified endothelial dysfunction, l-Arginine supplementation (6–8 g/day) improved endothelial function [Citation31]. Sixth, due to the metabolic alterations provoked by the SARS-CoV-2 infection [Citation32], it is necessary to increase foods rich in carnitine (e.g.; animal products like meat, fish, and poultry) or to include L-carnitine among dietary supplements (e.g.; standard dose: 0.5–2 g/day) for its effect on aerobic metabolism [Citation33].
Table 1. Recommendations for nutritional rehabilitation: eating well to regain the strength after COVID-19
Physical exercise rehabilitation recommendations
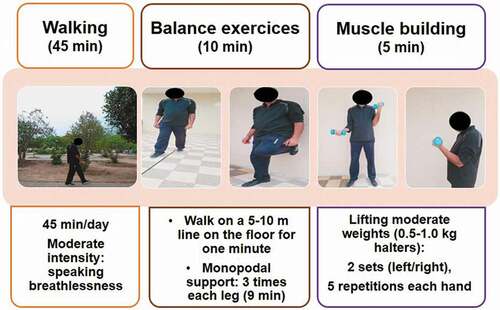
Exercise is highly recommended for Covid-19 patients after discharge to help in the process of recovery, prevent the occurrence of the disease, and avoid the risk of sequel [Citation16–20]. According to the authors’ opinion, the physical exercise rehabilitation should include at least 12 sessions (i.e.; three sessions/ week for four weeks, or two sessions/week for six weeks). Each session lasts one hour. resumes a typical session of a physical exercise rehabilitation that FPs should recommend to the ‘long-term Covid-19’ patients. The authors suggest that the physical exercise rehabilitation includes three items related to walking, balance posture exercises, and muscle building.
The first item consists on aerobic reconditioning via walking for 45 minutes. The walking intensity can be appraised by the patient’s ability of speaking during walk without being out of breath. At first, the patient walks at a slow pace for five minutes, and then he/she reaches gradually the breathlessness speaking and maintains this rhythm for 10 min. It is recommended that patients repeat two additional cycles of walking (the rule of 3 × 5 min, 3 × 10 min) ().
The second item consists of balance posture exercises, which includes at least two types of exercises. The first is walking on a straight line of 5–10 m for 1 min (). The second exercise is the monopodal support where the patient should stand up feet slightly apart, keep upper body straight, raise the knee until placing thigh in a horizontal position for 5–10 seconds, and then lower the knee toward the initial position. This exercise, which should be repeated three times on each leg, lasts around 10 min [Citation34] ().
The third item consists on a muscle-building exercise for the upper limbs () [Citation34]. For this exercise, lightweight halters are needed (i.e.; 0.5 to 1.0 kg). The patient should hold one halter in each hand. Starting with arms alongside the body; the patient should simultaneously raise arms to the side-up to shoulder height without bending elbows. Then, the patient should go back down slowly. The aforementioned movements can be done whether in the frontal or sagittal plans [Citation34] (). The patient should perform two sets of five repetitions each during 5 min.
Finally, there are potential associations between physical activity and a risk of SARS-CoV-2 infection, severe illness from Covid-19 and Covid-19 related death [Citation35]. For example, Lee et al. [Citation35] have established that adults who engaged in both aerobic (e.g.; 150–300 min a week of moderate intensity of physical activity) and muscle strengthening activities according to the 2018 physical activity guidelines [Citation36], were associated with a decreased likelihood of a SARS-CoV-2 infection, severe Covid-19 illness, and Covid-19 related death. Their results suggest that engaging in physical exercise proves potential benefits to fight Covid-19 [Citation35].
Future directions
We appeal to promote the CPR for ‘long-term Covid-19’ patients in family medicine. We invite other investigators to contact our team to reasonably set an international multicentre protocol. It is interesting to evaluate the effects of our proposed protocol in real life by evaluating some interesting parameters such as dyspnea and quality of life data.
To conclude, since FPs are in the frontline of the management of ‘long-term Covid-19’ patients, they should be more cautious in the prescription of exercise and nutrition program and informed about the minimal advices related to nutritional and physical exercise rehabilitation guidelines when taking care of ‘long-term Covid-19’ patients, and how these guidelines can relieve the mental and physical problems, improve immunity, and accelerate the recovery process of the patients. With the occurrence of new variants of the SARS-CoV-2, the nutritional and exercise rehabilitation guidelines implemented by FPs become indispensable to promote the recovery of Covid-19 patients and support a return to normal life.
Disclosure of financial/other competing interests
The authors have no relevant conflicts of interest to disclose. Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Ketfi A, Chabati O, Chemali S, et al. Preliminary data on the clinical, biological and radiological characteristics of algerian patients hospitalized for Covid-19. Pan Afr Med J. 2020;35(Suppl 2):77.
- Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama. 2020;323(13):1239–1242.
- Ghram A, Briki W, Mansoor H, et al. Home-based exercise can be beneficial for counteracting sedentary behavior and physical inactivity during the COVID-19 pandemic in older adults. Postgrad Med. 2021;133(5):469–480.
- Msheik El Khoury F, Talih F, Khatib MFE, et al. Factors associated with mental health outcomes: results from a tertiary referral hospital in Lebanon during the COVID-19 pandemic. Libyan J Med. 2021;16(1):1901438.
- Akbari H, Pourabbas, M, Yoosefi, M, et al. How physical activity behavior affected well-being, anxiety and sleep quality during COVID-19 restrictions in Iran. Eur Rev Med Pharmacol Sci. 2021;25(24):7847–7857.
- Smirmaul BPC, Arena R. The urgent need to sit less and move more during the COVID-19 pandemic. J Cardiopulm Rehabil Prev. 2020;40(5):287–289.
- Fiorindi C, Campani F, Rasero L, et al. Prevalence of nutritional risk and malnutrition during and after hospitalization for COVID-19 infection: preliminary results of a single-centre experience. Clin Nutr ESPEN. 2021;45:351–355.
- Kellnar A, Hoppe JM, Brunner S, et al. Hospitalization for COVID-19 is associated with significant changes in body composition. Clin Nutr ESPEN. 2021;45:499–502.
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062.
- Tajbakhsh A, Gheibi Hayat SM, Taghizadeh H, et al. COVID-19 and cardiac injury: clinical manifestations, biomarkers, mechanisms, diagnosis, treatment, and follow up. Expert Rev Anti Infect Ther. 2021;19(3):345–357.
- Guidon AC, Amato AA. COVID-19 and neuromuscular disorders. Neurology. 2020;94(22):959–969.
- Fang D. SARS: facts and considerations for the orthopaedic community. J Orthop Surg (Hong Kong). 2003;11(1):3–5.
- Zhang P, Li J, Liu H, et al. Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: a 15-year follow-up from a prospective cohort study. Bone Res. 2020;8(1):8.
- Lau HM, Lee EW-C, Wong CN-C, et al. The impact of severe acute respiratory syndrome on the physical profile and quality of life. Arch Phys Med Rehabil. 2005;86(6):1134–1140.
- Lopez-Leon S, Wegman-Ostrosky T, Perelman C, et al. More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci Rep. 2021;11(1):16144.
- Greenhalgh T, Knight M, A’Court C, et al. Management of post-acute covid-19 in primary care. Bmj. 2020;370:m3026.
- Andrejak C, Blanc F-X, Costes F, et al. Guide for follow-up of patients with SARS-CoV-2 pneumonia. Management proposals developed by the French-language respiratory medicine society. Version of 10 May 2020. Rev Mal Respir. 2020;37(6):505–510.
- Stein J, Visco CJ, Barbuto S. Rehabilitation medicine response to the covid-19 pandemic. Am J Phys Med Rehabil. 2020;99(7):573–579.
- Agostini F, Mangone M, Ruiu P, et al. Rehabilitation setting during and after Covid-19: an overview on recommendations. J Rehabil Med. 2021;53(1):jrm00141.
- Bessis S. The COVID-19 pandemic. Med Mal Infect. 2020;50(8):8S20.
- World health organization. Support for rehabilitation self-management after COVID-19-relatedillness. (last access: December 26th 2021). Available from this URL: https://cdn.who.int/media/docs/default-source/ageing/support-for-rehabilitation-self-management-after-covid-19-related-illness-engf5cec00b-350b-4eb0-bc24-0704df509ae1.pdf?sfvrsn=203566f0_1&download=true
- Gloeckl R, Leitl D, Jarosch I, et al. Benefits of pulmonary rehabilitation in COVID-19: a prospective observational cohort study. ERJ Open Res. 2021;7(2):2.
- Daynes E, Gerlis C, Chaplin E, et al. Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition - A cohort study. Chron Respir Dis. 2021;18:14799731211015691.
- Reina-Gutierrez S, Torres-Costoso A, Martínez-Vizcaíno V, et al. Effectiveness of pulmonary rehabilitation in interstitial lung disease, including coronavirus diseases: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2021;102(10):1989–1997. e3.
- Negrini S, Mills J-A, Arienti C, et al. “Rehabilitation research framework for patients with COVID-19” defined by cochrane rehabilitation and the world health organization rehabilitation programme. Arch Phys Med Rehabil. 2021;102(7):1424–1430.
- Greenhalgh T, Knight M. Long COVID: a primer for family physicians. Am Fam Physician. 2020;102(12):716–717.
- Benzarti W, Toulgui E, Prefaut C, et al. General practitioners should provide the cardiorespiratory rehabilitation’ ‘minimum advice’ for long COVID-19 patients. Libyan J Med. 2022;17(1):2009101.
- Hospital for special surgery (HSS). Eating well to regain your strength after COVID-19 . (Last visit: December 26th, 2021). (Last visit: December 26th, 2021): https://www.hss.edu/conditions_eating-well-regain-your-strength-after-covid-19.asp
- Petrushevska M, Zendelovska, D, Atanasovska, E, et al. Presentation of cytokine profile in relation to oxidative stress parameters in patients with severe COVID-19: a case-control pilot study. F1000Res. 2021;10:719.
- Adebayo A, Varzideh F, Wilson S, et al. l-Arginine and COVID-19: an update. Nutrients. 2021;13(11):3951.
- Strohle A, von Bibra H, Hahn A. L-Arginine and vascular health. Med Monatsschr Pharm. 2016;39(12):515–520.
- D’Ardes D, Rossi, I, Bucciarelli, B, et al. Metabolic changes in SARS-CoV-2 infection: clinical data and molecular hypothesis to explain alterations of lipid profile and thyroid function observed in COVID-19 patients. Life (Basel). 2021;11:8.
- Bremer J. Carnitine–metabolism and functions. Physiol Rev. 1983;63(4):1420–1480.
- Daily exercise training. A practical session. ( Last visit: December 26th, 2021). Available from this URL: http://www.respir-sud.com/english/rehabilitation/12/105/2/D%C3%A9monstration.html
- Lee SW, Lee J, Moon SY, et al. Physical activity and the risk of SARS-CoV-2 infection, severe COVID-19 illness and COVID-19 related mortality in South Korea: a nationwide cohort study. Br J Sports Med. 2021. DOI:https://doi.org/10.1136/bjsports-2021-104203.
- Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–2028.