?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
This study examines the effects of ethnic minority populations and income inequalities on COVID-19 excess mortality within English local councils. We demonstrate empirically that councils with large ethnic minority populations and high-income inequalities exhibit higher excess mortality during the first wave of the pandemic. We further show that the association between a large ethnic minority population and high excess mortality is manifested significantly more in councils with larger income inequalities. Our findings call for immediate actions and long-term policies to address social and income inequalities as these inequalities affect population health conditions.
1. INTRODUCTION
Inequalities within a region represent a serious problem with important health implications for the population (Brown & Rees, Citation2006). Such inequalities are found to exacerbate during a crisis period (Mussida & Parisi, Citation2020) and (to some extent) are driven by the ethnic background (Venturini & Villosio, Citation2018) and the economic condition (Braveman et al., Citation2011; Liao & De Maio, Citation2021) of the population living in a region. The recent COVID-19 pandemic has been blamed for having widened pre-existing inequalities, especially those stemming from individuals’ ethnic backgrounds (Collinson, Citation2020). Considering that the recent health crisis is regional and local (Bailey et al., Citation2020; Kuhlmann & Franzke, Citation2022) our study examines the association between COVID-19-related excess mortality, ethnic minority population and income inequality within English local councils during the first wave of the pandemic. As Bailey et al. (Citation2020) point out ‘A regional analysis is essential to fully understand and manage the unequal impacts of the current pandemic, not least because Covid-19 is unlikely to be the last of its kind’ (p. 1163).
The discrimination faced by ethnic minorities is widespread in both developing and developed countries, with national and local governments being criticized for not doing enough to address it (Khan, Citation2015). A review by the UK Equality and Human Rights Commission (EHRC) outlined that ethnic minorities in the UK face entrenched race inequality in many areas, including health (EHRC, Citation2016). Differences in health conditions across ethnic groups have been repeatedly documented by previous studies conducted before the COVID-19 pandemic (e.g., Bouchard et al., Citation2015; Fiscella & Sanders, Citation2016; Nazroo, Citation2003; Williams & Mohammed, Citation2009). These differences have been explained by several factors that characterize ethnic minorities when compared with white ethnic groups, including their economic, cultural and lifestyle conditions, and pathophysiological differences in responding to viruses (Fiscella & Sanders, Citation2016; Khunti et al., Citation2020). Additionally, previous studies have pointed out that ethnic minorities may experience poorer health conditions due to discrimination, which may cause stress and reduce the immune system’s ability to combat and contrast viruses (Williams et al., Citation2003).
Social and economic determinants of health inequalities have increasingly drawn attention in the areas of policymaking and academic research (Hosseinpoor et al., Citation2018; World Health Organization (WHO), Citation2018). Several studies have been conducted in the relevant academic literature to investigate the role income inequalities play in health inequalities. Marmot (Citation2005) has highlighted that poverty is the main cause of inequalities in health across the world and that necessary policies aiming to promote relief of poverty should take into consideration more equal development of health systems. In a similar vein, Graham (Citation2009) points out that the economic and social policies adopted in high-income societies have resulted in greater national wealth and population health. Nevertheless, Collison et al. (Citation2007, Citation2010) show that in Anglo-American systems higher levels of mortality in infants are associated with higher income inequalities and consider this association as the result of poor social outcomes of Anglo-American capitalism and the failure of neo-liberalism policies. Their results support those of Coburn (Citation2004) who shows that neo-liberalism is associated with greater poverty, income and health inequalities, while less neo-liberal countries are found to have healthier populations than neo-liberal ones. Braveman et al. (Citation2011), in their review of the social determinants of health and health inequality, point out that although income increases usually have positive effects on health, the high average income within a geographical area may be detrimental to health equality among ethnic groups when ethnic minorities coexist with wealthy white ethnic groups as high income might expose ethnic minorities to more discrimination.
The COVID-19 outbreak has been blamed for playing a key role in exacerbating the existing ethnic and income inequalities by impacting mostly individuals that belong to groups in a disadvantageous position in terms of their ethnicity and wealth. Preliminary studies have indeed found higher mortality rates for ethnic minority groups. For example, Gross et al. (Citation2020) find that, in the United States, the COVID-19 mortality rate for Afro-Americans is more than three times the rate for whites, and the rate for Latinos is almost double the rate for non-Latinos whites. Aldridge et al. (Citation2020) use data from patients with a positive COVID-19 test who died in hospitals in England in March and April 2020 and find a lower risk of death for white Irish and British ethnic groups and an increased risk of death for black, Asian and minority ethnic (BAME) groups. In their conclusions, the authors urgently call for actions to be taken to reduce the risk of death for minority groups, such as better income protection, occupational risk reduction and removal of barriers to access healthcare. They further stress the important role that national and local governments should play in reducing ethnic inequalities in health.
During the first wave of the pandemic, ethnic minorities experienced a higher level of mortality risk of COVID-19 than the white population in the UK (Ayoubkhani et al., Citation2021; White & Nafilyan, Citation2020). In addition, although the mortality risk of minority ethnic groups was reduced after the introduction of lockdown, males from minority groups kept experiencing higher levels of mortality (Ayoubkhani et al., Citation2021). Nafilyan et al. (Citation2021) present similar results during the first wave of the pandemic. During the second wave, they show that differences between the white population and ethnic minority groups were not as strong as in the first wave, although still differences existed with some subgroups (e.g., Pakistani and Bangladeshi). Interestingly, both studies show that the higher mortality risk within the ethnic-minorities population is, to some extent, explained by geographical variation in the determinants of inequality. In particular, local authority districts are found to drive the difference (Ayoubkhani et al., Citation2021). Nevertheless, these studies do not examine specific local characteristics that drive these differences.
Although COVID-19 is a global pandemic, it takes ‘the form of intense local epidemics’ (Amdaoud et al., Citation2021, p. 639). One important dimension that appears to play an important role in the diffusion of COVID-19 is the economic development of a local area. Ascani et al. (Citation2021) examine the association between province-level COVID-19 cases and province-level characteristics of economic activities in Italy. They show that provinces with geographically concentrated economic activities are found to exhibit a much higher number of cases. They attribute their findings to more interactions among people in these provinces. In addition, Bloise and Tancioni (Citation2021) find that the level of COVID-19 cases in Italian provinces is positively associated with their productivity, level of international business relationships and employment rate. In a study of 125 regions from 12 European countries, Amdaoud et al. (Citation2021) show that a region’s COVID-19 mortality rate is positively associated with its population age and negatively associated with its level of adherence to European Union (EU) objectives. Contrary to Bloise and Tancioni (Citation2021), their study shows that regions’ level of economic development (as measured by gross domestic product (GDP) per capita) is negatively associated with COVID-19-related mortality whereas regions’ level of unemployment is positively associated with mortality due to COVID-19. Finally, focusing on US states and counties, respectively, Oronce et al. (Citation2020) and Liao and De Maio (Citation2021) show that income inequalities within a region are strong determinants of both COVID-19 cases and related mortality.
This study aims to contribute to these streams of literature by investigating the relationship between ethnic minorities and the levels of COVID-19-related excess mortality during the first wave of the current COVID-19 pandemic across English local councils. In addition, this study explores the direct effect of the economic condition of the population across the English councils on COVID-19 excess mortality as well as its moderating role in the relationship between COVID-19 excess mortality and ethnic minorities. Such a study can have important policymaking implications as ‘racial and ethnic inequality, discrimination and racism remain entrenched features of “the social life of the nation” across all areas – from education to employment, housing to health, … – and across all minority groups’ (Byrne et al., Citation2020, p. 10). Although some recent studies have explored the exposure of ethnic minorities to the pandemic in England (Aldridge et al., Citation2020; Ayoubkhani et al., Citation2021; Khunti et al., Citation2020; Nafilyan et al., Citation2021; White & Nafilyan, Citation2020), the socio-economic factors affecting this association are still underexplored (Liao & De Maio, Citation2021).
Previous studies have found that ethnic minorities face higher health disparities when compared with other ethnic groups as they are more likely to be at risk of poor health (e.g., Bouchard et al., Citation2015; Fiscella & Sanders, Citation2016; Nazroo, Citation2003). This has been explained because several disadvantageous socio-economic factors characterize ethnic minorities. For instance, ethnic minorities are more likely to have low income, live in poor and overcrowded accommodation, and are employed in less secure and lower paid essential jobs than white ethnic groups (Aldridge et al., Citation2020; Fiscella & Sanders, Citation2016; Khunti et al., Citation2020). All these factors are particularly relevant to the exposure of ethnic minorities to the COVID-19 pandemic. People living in crowded households, being employed in essential and less secure jobs and/or with lower income might find social distancing, one of the main measures used to prevent exposure to the pandemic, more difficult to practice, which, in turn, might result in a wider spread of the virus in their local community. Ethnic minorities are also likely to have poorer access to healthcare services and be subject to greater discrimination than white ethnic groups. Medical studies have indeed found that discrimination can adversely affect the health of the subject discriminated because of an increase in stress and anxiety (Williams et al., Citation2003), potentially leading to worse COVID-19 outcomes. Hence, the first research question of our study is formulated as follows:
RQ1: Is the level of population with ethnic minority backgrounds in English local councils associated with COVID-19-related excess mortality?
RQ2: Is the level of income inequality within English local councils associated with COVID-19-related excess mortality?
RQ3: Does the level of income inequality within English local councils moderate the relationship between the level of population with ethnic minority backgrounds and COVID-19-related excess mortality?
2. DATA AND METHOD
To investigate our research questions, we collect data on COVID-19 cases and excess mortality recorded during the period March–July 2020 for the full population of 314 single and lower tier local councils in England which include 56 unitary authorities, 36 metropolitan boroughs, 32 London boroughs, 188 district councils and two sui generis authorities. We then collect data on local councils’ population ethnicity, income inequality and other demographic characteristics as described in Appendix A in the supplemental data online. From the set of 314 local councils, four local councilsFootnote1 for which data for all the necessary variables were not available were excluded. Hence, our analysis includes 310 local councils.Footnote2 We focus our analysis on the ‘first wave’ of the pandemic as it can be seen as an exogenous, unexpected shock to individuals’ lives and public authorities. At later stages of the pandemic, it can be expected that individuals have adjusted their activities, and public authorities their policies and regulations to mitigate their exposure to COVID-19. Hence our tests would not capture any effects on the ‘ordinary times’.
To examine our research questions on the association of COVID-19 excess mortality with ethnic minorities and income inequality within English local councils as well as the role that income inequality plays in the association between COVID-19 excess mortality and ethnic minorities, we adopt a path analysis approach based on SEM. Following previous studies (Goswami et al., Citation2021; Hamidi et al., Citation2020), this model was considered the most appropriate for the multivariate analysis as the main variables of interest (ethnic minorities and income inequality) could affect simultaneously the excess mortality and COVID-19 infection rate, with the latter being a precursor of the excess mortality recorded in the period analysed. Path analysis allows us to investigate the relationship between ethnic minorities population, income inequality and COVID-19 to excess mortality, both directly and indirectly, via COVID-19 infection rate as the mediator. We use different model specifications to test our results, with the following set of equations being used in our main analysis.
(1)
(1)
(2)
(2)
In Equationequation (1)(1)
(1) , the dependent variable EXCESS_MORT is measured, following the Office for National Statistics’ (ONS) procedure, as the ratio between the deaths recorded in the period March–July 2020 to the average number of deaths recorded in the same period in 2015–19 in a local council i. The main focus is on the two main variables of interest: %BAME as a proxy of ethnic minorities, which is measured as the projected proportion of the population living in 2019 in the local council i that has black, Asian, mixed or other ethnicities,Footnote3 and INC_INEQ, as proxied by the Gini coefficient at local council level (Hortas-Rico & Rios, Citation2019; Royuela et al., Citation2019). Following previous studies, we include several control variables to account for major determinants of the excess mortality recorded during the pandemic outbreak, related to the characteristics of the population living in the local councils analysed and of the health services and infrastructures operating in these local councils. As for population characteristics, we control for the proportion of the population living in the most and least income deprived areas, the proportion of the population with an age equal to or above 65 years and the life expectancy of the population at the age of 65. COVID-19-related deaths are more (less) common in the most (least) income-deprived areas (Bach-Mortensen & Degli Esposti, Citation2021; Caul, Citation2020) among elderly people and people with health issues or disabilities (Mueller et al., Citation2020). The quality and readiness of the healthcare system represented an important determinant of COVID-19-related deaths during the first wave of the pandemic (Bauer et al., Citation2020). Therefore, we control for the percentage of adult critical care beds occupied, the Summary Hospital-level Mortality Indicator (SHMI) and the average number of urgent operations cancelled in the healthcare facilities accessible by the population of a local council i and expected them to be positively associated to COVID-19 excess mortality, as higher values for these variables indicate lower quality and lower readiness of the health system.
In Equationequation (2)(2)
(2) , the dependent variable COVID19_RATE is measured as the percentage of the population that contracted COVID-19 in a local council i as of 31 July 2020. The association of the dependent variable with the two main variables of interest (%BAME and INC_INEQ) is then examined. We also control for the proportion of the population living in the most and least income-deprived areas, as COVID-19 incidents have been found to be higher (lower) in the most (least) income-deprived areas (Baena-Díez et al., Citation2020). Moreover, since COVID-19 is highly contagious, we control for population density and for the proportion of the population that contracted COVID-19 in other local councils within the same region, as the transmission of the disease can be facilitated in dense areas and in proximity to areas with higher COVID-19 incidence. Appendix A in the supplemental data online reports detailed definitions and sources for all variables.
To examine our research questions, we used an incremental model approach in developing Equationequation (1)(1)
(1) which consists of four models: model (1) includes all control variables and considers only the effect of the variable %BAME; model (2) includes all control variables and considers only the effect of the variable INC_INEQ; model (3) includes all control variables and both variables of interest: %BAME and INC_INEQ; and model (4) includes all variables and the interaction between %BAME and INC_INEQ.
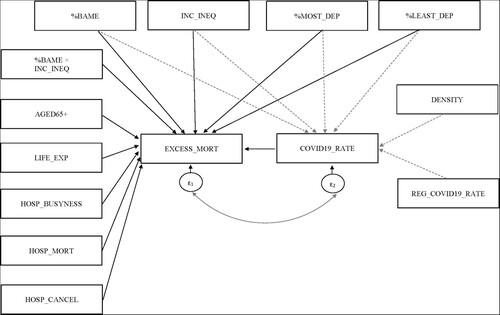
shows the path structure used for estimating the different path coefficients in our full model (model 4). The one-way arrow represents the expected direction of causality. Solid black arrows indicate direct effects on EXCESS_MORT. Dashed grey arrows indicate indirect effects on EXCESS_MORT, mediated through effects on COVID-19_RATE. The variables %BAME, INC_INEQ, %MOST_DEP and %LEAST_DEP are expected to impact the variable EXCESS_MORT both directly and indirectly (through the variable COVID19_RATE). The variables AGED65+, LIFE_EXP, HOSP_BUSYNESS, HOSP_MORT and HOSP_CANCEL are expected to impact EXCESS_MORT only directly. Finally, the variables DENSITY and REG_COVID19_RATE are expected to affect EXCESS_MORT indirectly, only, through the variable COVID19_RATE. We also allow a covariance structure between the errors of EXCESS_MORT and COVID19_RATE represented by the curved arrow.
Figure 1. Causal path diagram for excess mortality in terms of ethnic minorities, income inequality and other variables.
To examine our first research question (i.e., the relation between excess mortality and ethnic minorities), we focus on the coefficient β1 of the %BAME variable in Equationequation (1)(1)
(1) . A positive and statistically significant coefficient β1 indicates that councils with larger groups of ethnic minorities present a significantly larger excess mortality due to the COVID-19 pandemic. For examining the second research question (i.e., the relation between COVID-19 excess mortality and income inequalities) our attention is on the coefficients β2 of the INC_INEQ variable in Equationequation (1)
(1)
(1) . A positive and statistically significant coefficient β2 indicates that councils with higher income inequalities present a significantly larger excess mortality due to the COVID-19 pandemic. Whilst for our final research question (i.e., income inequality as a moderating factor of the relationship between COVID-19 excess mortality and ethnic minorities), the focus is on the coefficient β3 of the interaction term between the variables %BAME and INC_INEQ in Equationequation (1)
(1)
(1) , which is expected to be positive and statistically significant.
3. RESULTS
3.1. Data description and univariate analysis
presents descriptive statistics for the 310 local councils analysed and for councils characterized by low- and high-income inequality separately.Footnote4 Interestingly, it is shown that councils with high-income inequalities are characterized by a significantly higher excess mortality, a larger ethnic minority population, a higher proportion of the population living in the least deprived neighbourhood, and a lower proportion of the population living in the most deprived neighbourhood when compared with councils with low-income inequalities in terms of both mean and median values. Taking these preliminary findings together, descriptive statistics indicate that the COVID-19 pandemic has been more detrimental in councils where there are higher income inequalities. In addition, councils with high-income inequalities exhibit higher life expectancy, a lower COVID-19 infection rate in the councils and in the other councils within the same region, a less aged population and lower hospitality mortality than councils with lower income inequalities.
Table 1. Descriptive statistics for the 310 local councils analysed and for subgroups of high- and low-income unequal council.
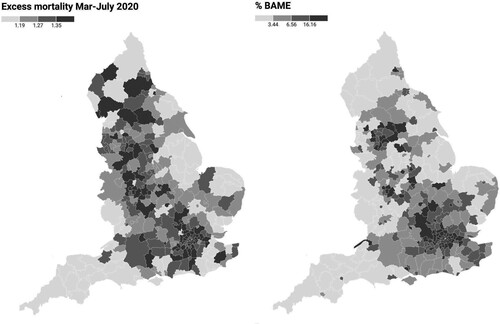
In order to provide a more comprehensive picture of our two main variables of interest, we also report two maps which portray the excess mortality (EXCESS_MORT) by councils (left-hand side of ) and the percentage of ethnic minorities population (%BAME) by councils (right-hand side of ). Councils are grouped in quartiles with darker colours indicating higher excess mortality and higher ethnic minorities populations, respectively. Regarding excess mortality, the map shows that various councils around large cities (such as Birmingham and the Greater London area) have been severely hit by the pandemic. Interestingly, and to some extent unexpectedly, we also witness high values of excess mortality in less populated areas (e.g., in the north of the country in councils such as Carlisle, South Lakeland and Craven, to name but a few). Turning to the second map, councils with a large proportion of ethnic minorities are primarily found within the Greater London area and in councils around other large cities such as Bristol, Birmingham and Manchester. The two maps exhibit some notable similarities as high values of the EXCESS_MORT variable overlap with high values of the %BAME variable in various councils, particularly around large cities. In a similar vein, we also see that low values of the two variables are also found in the same councils, especially in the South-West and in the East of the country. Although the purpose of these maps is to describe more clearly the two main variables of our study, it also provides some preliminary descriptive evidence of a potential association between EXCESS_MORT and %BAME variables.
reports Pearson correlation coefficients among all variables, which gives a first indication of the associations among the variables. As it is expected, %BAME and INC_INEQ are found to be positively and significantly correlated to EXCESS_MORT. The above provides preliminary evidence, at a univariate level, that councils with larger ethnic minorities and higher income inequality experience significantly larger mortality attributed to COVID-19. Also, COVID19_RATE, HOSP_BUSYNESS and LIFE_EXP are found to be positively and significantly correlated with EXCESS_MORT. On the contrary, AGED65+ and HOSP_MORT are found to be negatively and significantly correlated to EXCESS_MORT. Lastly, reviewing the correlation coefficients among all independent variables, we can conclude that there are no serious problems of multicollinearity as the coefficients are within the conventional levels (Gujarati, Citation1995).
Table 2. Pearson’s correlation coefficients.
3.2. Path analysis (structural equation models)
Regarding the results of the path analysis, reports the coefficients of our main models. In relation to our first research question, the coefficient of our main independent variable %BAME is 0.003 (statistically significant at the 1% level), which indicates that the proportion of the ethnic minorities population is positively associated with COVID-19 excess mortality within a local council. This indicates that a 1% increase in the value of the variable %BAME leads to an increase in the excess mortality recorded in a council by 0.003 (see model 3 in ). Turning next to our second research question, our results show a positive and statistically significant association (at 1% level) between excess mortality and income inequality (coefficient 0.118). This indicates that a 1% increase in the value of the variable INC_INEQ (equivalent to an increase of 0.0014 of the Gini index) leads to an increase of the excess mortality recorded in the council by 0.00118 (see model 3 in ). To the extent that councils with a higher proportion of ethnic minorities exhibit higher income inequality, it can be argued that there is a moderating effect of INC_INEQ on the association between %BAME and EXCESS MORT as our third research question suggests. Model 4 examines this potential channel. The results indicate that the level of income inequality of a council plays a significant moderating role in the association between COVID-19 excess mortality and ethnicity. As shown in , model 4, the interaction term between %BAME and INC_INEQ (coefficient 0.007) is positive and statistically significant at a 1% level, indicating that the positive association between ethnic minorities and COVID-19 excess mortality intensifies as income inequality increases. Precisely, a simultaneous 1% increase in the values of the variables %BAME and INC_INEQ leads to an additional increase of the excess mortality recorded in the council by 0.00007 (see model 4 in ).
Table 3. Main results.
As per the rest of the direct effects, all models show that excess mortality is positively associated with the COVID-19 infection rate recorded in the council which is an expected finding as more COVID-19 cases should lead to more COVID-19 deaths. Furthermore, shows that excess mortality is higher in those councils with a higher life expectancy and in those served by hospitals with a higher level of busyness recorded before the pandemic started. Finally, also shows that a local council’s excess mortality (EXCESS_MORT) is negatively associated with the pre-pandemic ratio of hospital mortality (HOSP_MORT). At first glance, this result might seem to be counterintuitive as hospitals that had lower mortality pre-pandemic would have been expected to be more prepared to handle the pandemic and record lower excess mortality. However, it should be noted that previous studies have shown that hospital mortality is positively associated with the number of cases that are emergency admissions in a hospital and negatively associated with the number of specialist doctors working in a hospital (Jarman et al., Citation1999). Taking into account that during the first wave of the pandemic, most hospital admissions were emergency admissions and that a very large number of critically ill COVID-19 patients were transferred between hospitals for comparable or more specialist treatment (Discombe, Citation2021), we conclude that this negative association may capture the transfer of critically ill COVID-19 patients from least specialized hospitals (i.e., those with higher mortality rates before the pandemic) to most specialized hospitals (i.e., those with lower mortality rates before the pandemic).
In relation to the indirect effects, our models show that the COVID-19 infection rate is positively associated with ethnicity, while negatively associated with income inequality. Our results also show that the COVID-19 infection rate is positively associated with the COVID-19 infection rate recorded in the other councils of the same region, confirming that geography affects the spread of diseases. Further, the COVID-19 infection rate is positively associated with the proportion of people living in the most deprived areas of the council, confirming that people living in more disadvantageous conditions were more likely to contract the virus. Finally, councils’ density is found to be negatively associated with the COVID-19 infection rate.Footnote5 Although this finding seems counterintuitive, recent findings suggest the opposite. For instance, Hamidi et al. (Citation2020) find a strong negative association between US counties’ density and COVID-19 death rates. Interestingly, CitationHamidi et al. find this negative association after controlling for factors similar to those used in our models (i.e., socio-economics and healthcare infrastructure). Hence, following their rationale, we conclude that our findings may be driven by better healthcare units which are usually found in dense areas and a plethora of services available in such areas that enable effective social distancing interventions.
3.3. Additional analyses
Besides our main analysis, we perform some additional analyses to examine the sensitivity of our results in different model specifications.
We first test if the relationship between ethnic minorities and COVID-19 excess mortality is affected by the percentage of the population living in the most and least deprived neighbourhoods within a local council. To investigate the role of deprivation within a council, we included in Equationequation (1)(1)
(1) the interaction term of the variables %BAME and %MOST_DEP and the interaction term of the variables %BAME and %LEAST_DEP. reports the results of this analysis, showing that ethnic minorities are significantly and positively associated with COVID-19 excess mortality and that this association become significantly weaker in local councils with a higher percentage of population living in the least deprived neighbourhood, while the percentage of the population living in the most deprived neighbourhood has no significant effect on the above association.
Table 4. Additional analysis. Income deprivation and the relationship between COVID-19 excess mortality and ethnic minorities.
This result indicates that when ethnic minorities live in areas characterized by higher levels of population with high income the excess mortality caused by COVID-19 is lower, suggesting that ethnic minorities suffer less when they live in areas where a higher percentage of the population is high-income earners. On the contrary, ethnic minorities are found to suffer the most when high-income earners represent a small fraction of the total population of the council. Overall, these results support our previous analysis that the economic conditions of the councils play a key role in the association between ethnicity and COVID-19 excess mortality.
Second, we employ an alternative proxy of income inequality based on the absolute difference between the proportion of a council’s population that works in high-paid jobs and the proportion of a council’s population that works in low-paid jobs.Footnote6 shows the results, which indicate that the association between ethnic minority populations and excess mortality is significantly stronger in local councils characterized by higher job income inequality.
Table 5. Additional analysis: job inequality and the relationship between COVID-19 excess mortality and ethnic minorities.
Third, we use the proportion of the population living in the local council i that has a White-British ethnicity as an alternative proxy for ethnicity. We run our main models again using this alternative proxy. Our results, reported in , show that White-British ethnicity population is negatively associated with COVID-19 excess mortality and that this association become significantly lower when the level of income inequality increases.
Table 6. Additional analysis: ethnic minorities are estimated as the proportion of the population that has White British ethnicity.
4. CONCLUSIONS
This study investigates how populations with ethnic minorities and income inequality are associated with COVID-19 excess mortality within English local councils over the first wave of the COVID-19 pandemic (i.e., March–July 2020). Our findings demonstrate that ethnic minorities contributed more to the death toll of the COVID-19 pandemic within local councils. This finding confirms voices which argue that ethnic minorities are more vulnerable to health crises (Collinson, Citation2020) and highlights the need for tailored policies which will protect these populations. It is indicative that the Mayor of London decided to support BAME staff across the Greater London Authority (Mayor of London, Citation2020) for that reason. Further, we show that this association is particularly strong in councils that exhibit high-income inequalities. To that end, we show that it is how income is distributed within a community that determines individuals’ health (Braveman et al., Citation2011). For instance, as our local analysis shows, the level of excess mortality in the London area, a region with a high average income (ONS, Citation2021), is strongly affected by the interaction between ethnic minorities and income inequality.
Our findings provide important contributions to the extant literature with practical implications for local councils. It contributes to regional studies literature by providing empirical evidence on important differences among local councils. Although reducing health inequalities is one of the main objectives local councils are expected to pursue (Ezzamel et al., Citation2007), our study shows that English local councils, particularly those with high-income inequality, have a long distance to walk to eliminate health inequalities. Further, it contributes to the literature on social inequalities in health confirming the results of previous studies that ethnic minority groups are more likely to suffer health inequalities than white ethnic groups (Aldridge et al., Citation2020; Bouchard et al., Citation2015; Fiscella & Sanders, Citation2016; Gross et al., Citation2020; Khunti et al., Citation2020; Nazroo, Citation2003; Price-Haywood et al., Citation2020; Williams & Mohammed, Citation2009).
Such differences indicate that local councils may need to adopt diverse policies to address the problems of their local communities. Especially councils exhibiting high levels of income inequality need to take action should they want to alleviate health inequalities that appear to stem from individuals belonging to ethnic minorities. Although lessening income inequality is a long-term policy goal which cannot have an immediate effect on the current health crisis, the burst out of a new pandemic in the future is almost certain (WHO, Citationn.d.). Hence, our study suggests that, to alleviate the observed adverse effects of ethnic and income inequalities on ethnic minorities’ health, local governments and other public authorities need to adopt immediate policies and strategies during a health crisis.
During health crises, central governments can provide local governments with additional financial support for establishing temporary grants directed to vulnerable groups such as ethnic minorities. Considering that our findings indicate that ethnic minorities suffered more in councils with high-income inequalities, it becomes apparent that economic aid to the poorer of a local community is necessary to reduce their financial burden and uncertainty. Further, as income inequalities are found to have a negative psychological impact on poor individuals (Braveman et al., Citation2011), our study urges local governments to explore more immediate policy interventions which will address the psychological impact of income inequalities on the least advantaged parts of their population. To that end, local services aiming at supporting psychologically vulnerable groups are necessary. In a similar vein, our findings show that secondary healthcare services needed to be supported during the first wave of the pandemic as hospital busyness is found to affect excess mortality. It should be stressed, however, that all the above are heavily dependent on how central governments distribute their available resources and funding. For instance, policy in England is dominated by the national, rather than local, government since the latter receives a large fraction of its funding from the former. For doing so the national government uses formulae to allocate that funding to local councils by service. Hence, our results indicate that all local policies are dependent on the national government’s formulae applied for their funding.
Moreover, local councils need to ensure that all members of their community are well-informed about the risks they are facing and about the measures that individuals can take to protect themselves. This is particularly important in light of our, rather counterintuitive, findings that a council’s population density is negatively associated with councils’ excess mortality. During the first wave of the pandemic, there was a widespread belief that more dense areas (particularly large cities) were hit harder by the pandemic. That may have put people residing in less populated areas at risk as they may have falsely believed that they were safe. Finally, our analysis reveals that excess mortality within a council is indirectly affected by the percentage of the population that contracted COVID-19 in other local councils within the same region. Such finding urges close cooperation among local governments.
In addition, our local analysis provides useful insights into the current pandemic which can be of use to local authorities in their efforts to confront the successive waves of COVID-19. Our analysis identifies where the hotspots of COVID-19 excess mortality are, indicating what regions are in higher need of relevant resources, infrastructure and other means of support to the more vulnerable parts of the population. To that end, regions such as the London area, West Midlands, North West, North East, West Yorkshire and South Yorkshire are found to be in greater need of intervention policies.
Despite these important contributions, we acknowledge that this study is subject to limitations, which open avenues for future research. First, our analysis could have benefitted from more detailed data referring to smaller areas about the ethnic and demographic characteristics of the recorded COVID-19 deaths (and in turn excess mortality) in English local councils, which were unfortunately not available at the moment the analysis was performed. Future research can incorporate this data when becomes available. Second, the focus of our study is the immediate effect of ethnic minorities population and income inequalities on COVID-19 excess mortality in English local councils during the first wave of the pandemic. This study does not examine the medium- and long- term effects of councils’ characteristics on their population health. Future studies can investigate relevant research questions. Last, we analyse our research questions in a single institutional setting. Although our findings can be generalized to other developed countries, we acknowledge that a more comprehensive picture would emerge by studying additional countries.
Despite these limitations, our study provides important insights into the association between COVID-19 excess mortality, ethnic minorities population and income inequalities within English local councils and questions the effectiveness of the strategies adopted by these councils in confronting such inequalities. Finally, it calls for actions to be taken at the local and national levels to overcome the effects of ethnic and income inequalities on population health.
Supplemental Material
Download PDF (248.2 KB)ACKNOWLEDGEMENTS
We thank the three anonymous reviewers and editor Ben Derudder for the excellent comments we received during the review process. Earlier versions of this paper benefited from the valuable comments made by Foteini Netsika MD and the participants of the seminars at Audencia Business School and the University of Essex. Any remaining errors are our sole responsibility.
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the authors.
Notes
1. These councils are Buckinghamshire, City of London, Isles of Scilly and West Devon.
2. See in Appendix A in the supplemental data online for the list of the local councils analysed and relevant data.
3. The ethnical group ‘other ethnicities’ excludes the minority population ‘White Other’.
4. We ranked English local councils based on their Gini coefficient from the most unequal (rank 1) to the least unequal (rank 310). Those ranked from positions 1 to 155 were included in the subgroup of the most unequal local councils, while those ranked from positions 156 to 310 were included in the subgroup of the least unequal local councils.
5. Although the variable of density, measured as the ratio between the total population of the council and area size, controls sufficiently the effect of council density on the excess of mortality within the council, we acknowledge that household density (i.e., persons per household or persons per room in a housing unit) can also play an important role in the overall mortality.
6. For doing so, we use the 2019 ‘Annual Population Survey’ of the ONS. The survey identifies nine scales of jobs based on their average income. To estimate the difference, we use the upper two as those with the higher pay (Category 1: managers, directors and senior officials; Category 2: professional occupations) and the lower two as those with the lower pay (Category 8: process, plant and machine operatives; Category 9: elementary occupations).
REFERENCES
- Aldridge, R. W., Lewer, D., Katikireddi, S. V., Mathur, R., Pathak, N., Burns, R., Fragaszy, E., Johnson, A. M., Devakumar, D., Abubakar, I., & Hayward, A. (2020). Black, Asian and minority ethnic groups in England are at increased risk of death from COVID-19: Indirect standardisation of NHS mortality data. Wellcome Open Research, 5(88), 1–20. 10.12688/wellcomeopenres.15922.2
- Amdaoud, M., Arcuri, G., & Levratto, N. (2021). Are regions equal in adversity? A spatial analysis of spread and dynamics of COVID-19 in Europe. The European Journal of Health Economics, 22(4), 629–642. https://doi.org/10.1007/s10198-021-01280-6
- Ascani, A., Faggian, A., & Montresor, S. (2021). The geography of COVID-19 and the structure of local economies: The case of Italy. Journal of Regional Science, 61(2), 407–441. https://doi.org/10.1111/jors.12510
- Ayoubkhani, D., Nafilyan, V., White, C., Goldblatt, P., Gaughan, C., Blackwell, L., Rogers, N., Banerjee, A., Khunti, K., Glickman, M., Humberstone, B., & Diamond, I. (2021). Ethnic-minority groups in England and Wales – Factors associated with the size and timing of elevated COVID-19 mortality: A retrospective cohort study linking census and death records. International Journal of Epidemiology, 49(6), 1951–1962. https://doi.org/10.1093/ije/dyaa208
- Bach-Mortensen, A. M., & Degli Esposti, M. (2021). Is area deprivation associated with greater impacts of COVID-19 in care homes across England? A preliminary analysis of COVID-19 outbreaks and deaths. Journal of Epidemiology and Community Health, 75(7), 624–627. https://doi.org/10.1136/jech-2020-215039
- Baena-Díez, J. M., Barroso, M., Cordeiro-Coelho, S. I., Díaz, J. L., & Grau, M. (2020). Impact of COVID-19 outbreak by income: Hitting hardest the most deprived. Journal of Public Health, 42(4), 698–703. https://doi.org/10.1093/pubmed/fdaa136
- Bailey, D., Clark, J., Colombelli, A., Corradini, C., De Propris, L., Derudder, B., Fratesi, U., Fritsch, M., Harrison, J., Hatfield, M., Kemeny, T., Kogler, D. F., Lagendijk, A., Lawton, P., Ortega-Argilés, R., Otero, C. I., & Usai, S. (2020). Regions in a time of pandemic. Regional Studies, 54(9), 1163–1174. https://doi.org/10.1080/00343404.2020.1798611
- Bauer, J., Brüggmann, D., Klingelhöfer, D., Maier, W., Schwettmann, L., Weiss, D. J., & Groneberg, D. A. (2020). Access to intensive care in 14 European countries: A spatial analysis of intensive care need and capacity in the light of COVID-19. Intensive Care Medicine, 46(11), 2026–2034. https://doi.org/10.1007/s00134-020-06229-6
- Bloise, F., & Tancioni, M. (2021). Predicting the spread of COVID-19 in Italy using machine learning: Do socio-economic factors matter? Structural Change and Economic Dynamics, 56, 310–329. https://doi.org/10.1016/j.strueco.2021.01.001
- Bouchard, L., Albertini, M., Batista, R., & De Montigny, J. (2015). Research on health inequalities: A bibliometric analysis (1966–2014). Social Science and Medicine, 141, 100–108. https://doi.org/10.1016/j.socscimed.2015.07.022
- Braveman, P., Egerter, S., & Williams, D. R. (2011). The social determinants of health: Coming of age. Annual Review of Public Health, 32(1), 381–398. https://doi.org/10.1146/annurev-publhealth-031210-101218
- Brown, D., & Rees, P. (2006). Trends in local and small area mortality and morbidity in Yorkshire and the Humber: Monitoring health inequalities. Regional Studies, 40(5), 437–458. https://doi.org/10.1080/00343400600757395
- Byrne, B., Alexander, C., Khan, O., Nazroo, J., & Shankley, W. (2020). Ethnicity, race and inequality in the UK: State of the nation. Policy Press.
- Caul, S. (2020). Deaths involving COVID-19 by local area and socioeconomic deprivation: Deaths occurring between 1 March and 31 July 2020. Office for National Statistics (ONS). https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsinvolvingcovid19bylocalareasanddeprivation/deathsoccurringbetween1marchand31july2020
- Coburn, D. (2004). Beyond the income inequality hypothesis: Class, neo-liberalism, and health inequalities. Social Science & Medicine, 58(1), 41–56.
- Collinson, A. (2020). Coronavirus: Ethnic minorities ‘over-exposed’ to Covid-19. BBC. https://www.bbc.com/news/health-53651954
- Collison, D., Dey, C., Hannah, G., & Stevenson, L. (2007). Income inequality and child mortality in wealthy nations. Journal of Public Health, 29(2), 114–117. https://doi.org/10.1093/pubmed/fdm009
- Collison, D., Dey, C., Hannah, G., & Stevenson, L. (2010). Anglo-American capitalism: The role and potential role of social accounting. Accounting, Auditing and Accountability Journal, 23(8), 956–998. https://doi.org/10.1108/09513571011092510
- Discombe, M. (2021). Critically ill covid patients moved between hospitals in record numbers. Health Service Journal. https://www.hsj.co.uk/coronavirus/exclusive-critically-ill-covid-patients-moved-between-hospitals-in-record-numbers/7029357.article
- Equality and Human Rights Commission (EHRC). (2016). Race report: Healing a divided Britain: The need for a comprehensive race equality strategy. https://www.equalityhumanrights.com/en/race-report-healing-divided-britain
- Ezzamel, M., Hyndman, N., Johnsen, Å, Lapsley, I., & Pallot, J. (2007). Experiencing institutionalization: The development of new budgets in the UK devolved bodies. Accounting, Auditing and Accountability Journal, 20(1), 11–40. https://doi.org/10.1108/09513570710731191
- Fiscella, K., & Sanders, M. R. (2016). Racial and ethnic disparities in the quality of health care. Annual Review of Public Health, 37(1), 375–394. https://doi.org/10.1146/annurev-publhealth-032315-021439
- Goswami, G. G., Ali, A. M., & Islam, S. (2021). A panel path analysis approach to the determinants of coronavirus disease 2019 transmission: Does testing matter for confirmed cases?’. Journal of Economic Studies, 48(8), 1624–1648. https://doi.org/10.1108/JES-07-2020-0326
- Graham, H. (2009). Health inequalities, social determinants and public health policy. Policy and Politics, 37(4), 463–479. https://doi.org/10.1332/030557309X445618
- Gross, C. P., Essien, U. R., Pasha, S., Gross, J. R., Wang, S. Y., & Nunez-Smith, M. (2020). Racial and ethnic disparities in population level COVID-19 mortality. Journal of General Internal Medicine, 35(10), 3097–3099. https://doi.org/10.1007/s11606-020-06081-w
- Gujarati, D. (1995). Basic econometrics (3rd ed.). McGraw-Hill.
- Hamidi, S., Sabouri, S., & Ewing, R. (2020). Does density aggravate the COVID-19 pandemic? Early findings and lessons for planners. Journal of the American Planning Association, 86(4), 495–509. https://doi.org/10.1080/01944363.2020.1777891
- Hortas-Rico, M., & Rios, V. (2019). The drivers of local income inequality: A spatial Bayesian model-averaging approach. Regional Studies, 53(8), 1207–1220. https://doi.org/10.1080/00343404.2019.1566698
- Hosseinpoor, A. R., Bergen, N., Schlotheuber, A., & Grove, J. (2018). Measuring health inequalities in the context of sustainable development goals. Bulletin of the World Health Organization, 96(9), 654–659. https://doi.org/10.2471/BLT.18.210401
- Jarman, B., Gault, S., Alves, B., Hider, A., Dolan, S., Cook, A., Hurwitz, B., & Iezzoni, L. I. (1999). Explaining differences in English hospital death rates using routinely collected data. Bmj, 318(7197), 1515–1520.
- Khan, O. (2015). Ethnic inequality is widespread and a drag on the global economy, The Guardian, 20 January. https://www.theguardian.com/public-leaders-network/2015/jan/20/ethnic-inequality-widespread-global-economy
- Khunti, K., Singh, A. K., Pareek, M., & Hanif, W. (2020). Is ethnicity linked to incidence or outcomes of COVID-19? BMJ, 369, m1548. https://doi.org/10.1136/bmj.m1548
- Kuhlmann, S., & Franzke, J. (2022). Multi-level responses to COVID-19: Crisis coordination in Germany from an intergovernmental perspective. Local Government Studies, 48(2), 312–334. https://doi.org/10.1080/03003930.2021.1904398
- Liao, T. F., & De Maio, F. (2021). Association of social and economic inequality with coronavirus disease 2019 incidence and mortality across US counties. JAMA Network Open, 4(1), 1–10. 10.1001/jamanetworkopen.2020.34578
- Marmot, M. (2005). Social determinants of health inequalities. The Lancet, 365(9464), 1099–1104. https://doi.org/10.1016/S0140-6736(05)71146-6
- Mayor of London. (2020). Mayor introduces risk assessments for BAME staff. Press Release, 1 June. https://www.london.gov.uk/press-releases/mayoral/mayor-introduces-risk-assessments-for-bame-staff
- Mueller, A. L., McNamara, M. S., & Sinclair, D. A. (2020). Why does COVID-19 disproportionately affect older people? Aging, 12(10), 9959–9981. https://doi.org/10.18632/aging.103344
- Mussida, C., & Parisi, M. L. (2020). Features of personal income inequality before and during the crisis: An analysis of Italian regions. Regional Studies, 54(4), 472–482. https://doi.org/10.1080/00343404.2019.1624711
- Nafilyan, V., Islam, N., Mathur, R., Ayoubkhani, D., Banerjee, A., Glickman, M., Humberstone, B., Diamond, I., & Khunti, K. (2021). Ethnic differences in COVID-19 mortality during the first two waves of the coronavirus pandemic: A nationwide cohort study of 29 million adults in England. European Journal of Epidemiology, 36(6), 605–617. https://doi.org/10.1007/s10654-021-00765-1
- Nazroo, J. Y. (2003). The structuring of ethnic inequalities in health: Economic position, racial discrimination, and racism. American Journal of Public Health, 93(2), 277–284. https://doi.org/10.2105/AJPH.93.2.277
- Office for National Statistics (ONS). (2021). Regional gross disposable household income, UK: 1997 to 2019. https://www.ons.gov.uk/economy/regionalaccounts/grossdisposablehouseholdincome/bulletins/regionalgrossdisposablehouseholdincomegdhi/1997to2019
- Oronce, C. I. A., Scannell, C. A., Kawachi, I., & Tsugawa, Y. (2020). Association between state-level income inequality and COVID-19 cases and mortality in the USA. Journal of General Internal Medicine, 35(9), 2791–2793. https://doi.org/10.1007/s11606-020-05971-3
- Price-Haywood, E. G., Burton, J., Fort, D., & Seoane, L. (2020). Hospitalization and mortality among black patients and white patients with COVID-19. New England Journal of Medicine, 382(26), 2534–2543. https://doi.org/10.1056/NEJMsa2011686
- Royuela, V., Veneri, P., & Ramos, R. (2019). The short-run relationship between inequality and growth: Evidence from OECD regions during the great recession. Regional Studies, 53(4), 574–586. https://doi.org/10.1080/00343404.2018.1476752
- Venturini, A., & Villosio, C. (2018). Are migrants an asset in recession? Insights from Italy. Journal of Ethnic and Migration Studies, 44(14), 2340–2357. https://doi.org/10.1080/1369183X.2017.1345992
- White, C., & Nafilyan, V. (2020). Coronavirus (COVID-19) related deaths by ethnic group, England and Wales: 2 March 2020 to 15 May 2020. Office for National Statistics (ONS). https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/coronaviruscovid19relateddeathsbyethnicgroupenglandandwales/2march2020to15may2020
- Williams, D. R., & Mohammed, S. A. (2009). Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine, 32(1), 20–47. https://doi.org/10.1007/s10865-008-9185-0
- Williams, D. R., Neighbors, H. W., & Jackson, J. S. (2003). Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health, 93(2), 200–208. https://doi.org/10.2105/AJPH.93.2.200
- World Health Organization (WHO). (2018). Global health observatory data: Health equity monitor. https://www.who.int/data/gho/health-equity
- World Health Organization (WHO). (n.d.). The next flu pandemic: A matter of ‘when’, not ‘if’. http://www.emro.who.int/pandemic-epidemic-diseases/news/the-next-flu-pandemic-a-matter-of-when-not-if.html