?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
The COVID-19 pandemic sparked a surge in the number and scope of governmental interventions in both centralised and decentralised states. While decentralisation theories and recent empirical studies suggest that highly decentralised systems are more resilient to shocks and cope better with adversity, other research presents inconclusive or even contradictory findings. Yet, little is still known about how decentralised governments coped with the COVID-19 health emergency. Using an original dataset of 445 regions across 26 Organisation for Economic Co-operation and Development (OECD) countries for 2020 and 2021, this article finds that excess mortality rates during the COVID-19 pandemic are not connected to the degree of fiscal and political decentralisation, but rather tied to the mismatch between the two dimensions, also known as unfunded mandates. Large unfunded mandates are positively associated with higher excess mortality rates during COVID-19. Fiscal and political decentralisation, by contrast, become statistically insignificant when unfunded mandates are considered. Hence, better – not more – decentralisation is needed as unfunded mandates represented a threat to the capacity of subnational authorities to address the COVID-19 emergency. In emergency situations, the dysfunctionality caused by unfunded mandates undermines the effectiveness of the response of the relevant public authorities to pressing challenges.
1. INTRODUCTION
In 2020, healthcare systems worldwide were stretched to the limit by the COVID-19 pandemic. To contain the disease and avoid the collapse of health centres, over half of the world’s population was forced into lockdown and other strict containment measures were adopted (Organisation for Economic Co-operation and Development (OECD), Citation2020). Despite these measures, during 2020 alone, more than 1.8 million excess deaths were reported across 36 OECD countries relative to the five previous years (OECD, Citation2021a, Citation2021b). Not all countries and regions in the OECD, however, were homogenously affected.
Defined as the transfer of power and resources from central to subnational tiers of government (OECD, Citation2017), differences in decentralisation may have contributed to the uneven regional impact of COVID-19. The institutional structure of a country affects its performance in different areas (Lv et al., Citation2022). Yet, studies published so far have shed little light on the extent to which fiscal and/or political decentralisation are linked to better health outcomes. Considering the capacity of health systems crucial in comprehending excess mortality within the OECD (Díaz-Ramírez et al., Citation2022), two perspectives have emerged. On one hand, it has been argued that decentralised systems, equipped with a heightened capacity to adapt, inherently promote policy flexibility, ultimately enhancing healthcare provision (Asfaw et al., Citation2007; Collins & Green, Citation1994). Such adaptable structures are posited to curtail excess mortality during a pandemic. Conversely, contrasting voices contend that decentralising health services fragments resources, yielding diseconomies of scale that trigger efficiency losses and compromising quality (Jiménez-Rubio & Smith, Citation2005; Naudé, Citation2020).
The variety of empirical results may derive from the omission of a relevant explanatory variable. Existing studies on decentralisation and health outcomes have something in common: they all test the effects of fiscal and political decentralisation on healthcare as two independent variables, unrelated to each other. In so doing, researchers make the crucial assumption that ‘finance follows function’, that is, that devolved responsibilities to subnational governments always come accompanied by the necessary resources to fulfil them (Bahl & Martínez-Vázquez, Citation2013). This is a far-fetched assumption, as subnational authorities often complain about mismatches between their powers and the resources available to fulfil their mandates. These ‘unfunded mandates’ are the norm rather than the exception. Failing to factor in the presence and the width of unfunded mandates may therefore bias the empirical results obtained in studies so far.
This study sets out to fill this gap in existing knowledge by adding unfunded mandates – that is, the mismatch between the powers devolved and resources available to subnational governments – to models testing the link between decentralisation and COVID-19 excess mortality rates. Using an original cross-sectional dataset of 445 regions in 26 OECD countries, we analyse the extent to which unfunded mandates (as well as fiscal and political decentralisation separately) raise COVID-19 excess mortality rates. We seek to determine whether it is the extent of fiscal or political decentralisation of healthcare what affects excess mortality, or whether it is rather the magnitude of the unfunded mandate (i.e., alignment between both dimensions of decentralisation) what drives variation in the regional rates of excess mortality.
This study is structured as follows. Section 2 overviews the literature on the link between decentralisation, efficiency and healthcare, and delves into the concept of unfunded mandates. Section 3 outlines the research question and hypotheses, the methodology, and the data used for our econometric estimations. Section 4 includes the empirical results and analysis. Section 5 summarises the conclusions, policy implications and ideas for future research.
2. DECENTRALISATION AND HEALTHCARE UNDER UNFUNDED MANDATES
2.1. Decentralisation, efficiency and healthcare
The interest in understanding the complexity of decentralisation has been a constant for over five decades. Theorists of decentralisation have traditionally been divided into two camps. The first one argues that decentralising powers delivers gains in efficiency (Oates, Citation1972). The second strand posits that, as appealing as decentralisation may sound, it may fall short of delivering on its promises of efficiency gains and hamper economic development.
This longstanding division also applies to analyses of the healthcare sector. Following Klugman (Citation1994), subnational authorities are more likely to understand regional healthcare needs and preferences, focusing, for instance, on elderly care solutions in regions where older people abound or directing more resources to preventive care in places with a younger population. Decentralised systems are also perceived as more flexible and less resistant to change (Collins & Green, Citation1994). Moreover, decentralised countries have governance coordination systems between the different tiers of government in place (Aubrecht et al., Citation2022; Naudé, Citation2020). All these factors are perceived to make decentralised health systems more ‘prepared by design’ (Carinci, Citation2020) to face times of adversity, such as the advent of a pandemic.
Yet, decentralising healthcare powers to lower tiers of government could also lead to a more unequal and dysfunctional healthcare system. Indeed, decentralised subnational entities may enjoy different analytical, operational and institutional capacities (Capano & Lippi, Citation2021): if the redistributive effect of centralisation is removed or is deficient, poorer regions will be less able to afford the health services their population demands, prompting both patients and healthcare professionals to vote with their feet. The fragmentation of subnational healthcare and the resulting regional disparities in health provision could be exacerbated in a system where the centre is weak and lacks an effective equalisation mechanism. Without a strong national lead, limited economies of scale may restrict adequate healthcare production (Jiménez-Rubio & Smith, Citation2005). In the event of an emergency, weak central governments may lack the capacity to coordinate emergency responses (Kuhn & Morlino, Citation2022) and become unable to control political ‘blame games’ (Schneider, Citation2008). This may explain why in the early stages of the COVID-19 pandemic there was a tendency to recentralise the health response in several countries of the OECD (de Biase & Dougherty, Citation2021).
Empirical findings regarding the correlation between decentralisation and healthcare system outcomes present a similarly varied and sometimes conflicting landscape. While the capacity of health systems is pivotal for effectively addressing health emergencies (Díaz-Ramírez et al., Citation2022), the question remains: which decentralisation framework is best suited to mitigate excess mortality? Robalino et al. (Citation2001) show that greater fiscal decentralisation is associated with lower mortality rates, particularly in lower income countries. Similar results have been reported, using different measures for health outcomes, for developed: Spain (Cantarero & Pascual, Citation2008), Germany (Kuhn & Morlino, Citation2022) – and developing countries: India (Asfaw et al., Citation2007), Honduras (Zarychta, Citation2020). By contrast, negative and significant relationships between decentralisation and health outcomes are also frequently reported. For example, Navarro et al. (Citation2020) showed how the decentralisation of the Philippines’s healthcare system complicated the task of providing services in poorer regions, due to the legal and budgetary weakness of the central government. In Pakistan (Zaidi et al., Citation2019) and Indonesia (Kristiansen & Santoso, Citation2006), two countries with a weak central government stewardship capacity of healthcare, inequities in child immunisation rates or the number of health professionals for birth assistance at the district level are rife. China’s decentralised health system has also contributed to a highly territorially uneven health provision (Hao et al., Citation2021). Decentralised healthcare also resulted in very unequal responses to the first wave of the COVID-19 pandemic among neighbouring Italian regions, such as Lombardy, Emilia-Romagna and Veneto (Capano & Lippi, Citation2021). There is also research that concludes that the relationship between decentralisation and healthcare outcomes is more complex. It may be positive but non-linear (Cavalieri & Ferrante, Citation2020); depend on the level of development of the region (Di Novi et al., Citation2019); or hump-shaped, pointing to an optimal level of decentralisation for healthcare outcomes (Dougherty et al., Citation2022).
The huge variety of empirical results points to two potential weaknesses in previous research. First, most previous studies linking decentralisation with differences in the availability and quality of healthcare provision measure one dimension of decentralisation only (fiscal, political, or administrative), using national-level data. Second, they tend to rely on small samples – frequently, single-country analyses – which are hardly generalisable.
2.2. The threat of unfunded mandates
These mixed results reported above suggest that decentralisation is not a panacea to address the dysfunctionalities of healthcare systems. Indeed, decentralisation may aggravate them. Hence, it seems essential that, in order to address health emergency situations more effectively, ‘better’ (not more) decentralisation of health systems may be needed. How can a ‘better’ decentralisation be achieved?
‘Better’ (or optimal) decentralisation is a situation where subnational authorities receive the necessary resources for each of the responsibilities that are devolved to them. Nevertheless, this is rarely the case. During a process of decentralisation, devolved responsibilities are often not adequately financed. In other words, sometimes finance does not follow function (Bahl, Citation1999). This phenomenon, which has received limited scholarly attention, is usually referred to as ‘unfunded mandates’ (e.g., Adler, Citation1997; Posner, Citation1998). The materialisation of unfunded mandates in decentralised countries reflects the competing interests of central and subnational governments. For the central government, decentralisation can be perceived as a politically desirable tool to shirk policy responsibilities without facing their costs (Bennett, Citation2014; Hart & Welham, Citation2016). However, subnational governments may reject such opportunistic behaviour, as it directly threatens their financial sustainability and their effective capacity to cater for the needs of their citizens.
The width and frequency at which unfunded mandates emerge depends on the degree of legitimacy enjoyed by both central and subnational entities during the decentralisation process (Rodríguez-Pose & Gill, Citation2003). When legitimacy falls with central governments, they will feel freer to devolve more powers than resources. Unfunded mandates will proliferate as a result. By contrast, when regions hold the upper hand, subnational governments have a wider margin of manoeuvre to negotiate and obtain more resources for the devolved responsibilities they must fulfil. This power hierarchy, which determines the presence and dimension of unfunded mandates, can vary over time as decentralisation is intensified or as the cost for the provision of services at the local level increases. If legitimacy tilts towards the central government, resources may not adapt and match subnational needs, thereby widening unfunded mandates. Similarly, if political differences emerge between central and regional governments, the allocation of funding may respond to political interests rather than efficiency, again enlarging misalignments between devolved responsibilities and resources.
Despite the limited attention that they have received, unfunded mandates are present in countries across the world irrespective of their federal or unitary nature and regardless of their level of development. Examples range from Dutch municipalities, whose portfolio of responsibilities has increased while the financial resources to fulfil them have remained stable (de Groot, Citation2019), through South Africa, where many subnational authorities complain about their lack of funding to attract the human capacities required to implement essential local economic development policies (Khambule, Citation2020), to the UK, where indirectly elected regional development agencies have been expected to fulfil many responsibilities without the appropriate budget (Lee, Citation2017; Morgan, Citation2002).
Unfunded mandates are essential to understand the effects of decentralisation processes on variables such as economic growth or mortality rates. Large mismatches between responsibilities and funding can be expected to undermine the capacity of subnational governments to spend time and resources to gather information, adapt policies to their constituents’ needs, and implement them with the necessary expertise (Klugman, Citation1994; Prud’homme, Citation1995). The resulting ineffectiveness may undermine policy innovation, competition, and public trust. Efficiency gains may suffer as a consequence (Donahue, Citation1997; Rodrik et al., Citation2004).
Specifically in the health sector, unfunded mandates may translate into fewer primordial services being offered, especially in poorer areas. If subnational authorities lack sufficient funding (or the powers to raise it), healthcare provision may become inefficient and ineffective. Unfunded mandates may jeopardise the response to shocks like the COVID-19 pandemic, leading to collapses in the healthcare system and worse health outcomes. For instance, the US’s ‘New Federalism’ doctrine, which during the Trump presidency required state and local governments to comply with balanced budget requirements, squeezed lower government tier budgets. This particularly affected subnational governments in the poorest areas of the US, often leading to pay cuts and layoffs. As the pandemic surfaced, some state and local governments quickly became overburdened (Im, Citation2021). Other pre-COVID-19 studies in Indonesia or the Philippines also show that insufficient equalisation transfers as well as insufficient powers to levy taxes locally force subnational authorities to reorient their priorities and often resort to privatisation strategies that further fuel interpersonal and interterritorial inequalities in access to healthcare (Liwanag & Wyss, Citation2018; Rakmawati et al., Citation2019).
Therefore, devolving healthcare without the appropriate resources may result in worse healthcare performance and outcomes. To our knowledge, no study on decentralisation and healthcare to date has duly incorporated unfunded mandates as a variable in its own right to assess the effects of decentralisation on healthcare in a cross-regional analysis. Instead, most research has devoted efforts to determine the impact of the degree of fiscal and political decentralisation on various indicators related to healthcare, critically assuming that finance follows function. Unfunded mandates are mentioned in different studies, but these take the form of case studies that offer limited generalisability (e.g., Bahl & Martínez-Vázquez, Citation2013; Boex & Martínez-Vázquez, Citation2006). There is thus an important gap about how unfunded mandates affect the impact of decentralisation on health outcomes.
3. METHODOLOGY
3.1. Research question and hypotheses
This paper assesses the connection between the existence of unfunded mandates and the levels of excess mortality observed in OECD regions during the COVID-19 pandemic. We define unfunded mandates as the mismatch between the powers and resources decentralised to subnational tiers of government (Rodríguez-Pose & Vidal-Bover, Citation2022). We also control for fiscal and political decentralisation, in line with most previous research on the topic. Building upon the discussion above, we posit that the occurrence and scale of unfunded mandates at the regional level are linked to excess mortality rates during COVID-19.
We also expect that large unfunded mandates may affect the link between fiscal and political decentralisation, on the one hand, and the health implications of COVID-19, on the other, meaning that, everything else being equal, considering unfunded mandates (as a proxy for the quality of the decentralisation framework) will reduce the significance of fiscal and political decentralisation levels by themselves for the quality of responses to COVID-19. This hypothesis is anchored on the perception that it is not the extent to which fiscal and political decentralisation is pursued, but rather the mismatch between the two, that mattered for health outcomes during the pandemic.
Additionally, we anticipate that substantial unfunded mandates may affect the relationship between fiscal and political decentralisation on one side and excess mortality on the other. In other words, while holding other factors constant, considering unfunded mandates (as an indicator of decentralisation framework quality) could diminish the standalone impact of fiscal and political decentralisation levels on the effectiveness of COVID-19 responses. This hypothesis is based on the premise that it is not merely the degree of fiscal and political decentralisation pursued, but rather the mismatch between the two, that had implications for health outcomes during the pandemic.
3.2. Data
Decentralisation studies at country-level generally suffer from inadequate data. This problem is aggravated when conducting research at subnational level (Martínez-Vázquez et al., Citation2017). And the shortage not only applies to our variables of interest (i.e., fiscal and political decentralisation, unfunded mandates, and COVID-19 excess mortality rates), but also to the relevant control variables. We therefore have built a large cross-regional dataset on decentralisation and unfunded mandates for 445 regions in 26 OECD countries. These data have been manually extracted primarily from international, national, and regional statistical offices (see Tables A1 and A2 in Appendix A in the supplemental data online).
The unit of analysis is OECD regions. ‘Regions’ are mostly defined at the OECD Territorial Level 2 (TL2), which encompasses the first administrative tier of subnational government. This is also the regional level at which more information is available for both the variables of interest and the controls. However, for those countries where TL2 constitutes merely a statistical region (e.g., the Czech Republic), TL3 is used provided data are available (see Table A3 in Appendix A in the supplemental data online for the regions comprised in our regressions).
One of the widely acknowledged realities in decentralisation research is the absence of a singular measure for decentralisation (Martínez-Vázquez & McNab, Citation2003). Decentralisation is a multidimensional process that induces changes in a region’s fiscal, political, and administrative indicators (Jiménez-Rubio & Smith, Citation2005). For fiscal decentralisation, the share of total public expenditure spent by subnational entities is the most commonly used proxy. However, this metric is only available at the national level. As a result, we have devised an alternative indicator measuring the expenditure capacity per capita for each of the 445 regions considered. The data were collected manually from the individual budgets of each region. All currencies were converted into constant 2015 US dollars, adjusted by purchasing power parity (see Table A1 in Appendix A in the supplemental data online).
When it comes to political decentralisation, we recognise the challenge of accurately evaluating this extensive phenomenon through a single indicator (Ezcurra & Rodríguez-Pose, Citation2013). Different scholars have provided different indices, where values for relevant aspects related to political decentralisation are weighted and added up to form composite indicators. Among these indicators, we select the most complete and widely used regional authority index (RAI), proposed by Hooghe et al. (Citation2016, Citation2021). To our knowledge, this is the only index that provides within-country variation (Filippetti & Sacchi, Citation2016; Lessmann, Citation2012). The RAI overall score results from the addition of the values in eight subcategories organised around two main pillars: self-rule and shared rule. The former calculates the degree of authority by the region over its own territory. The latter estimates a region’s degree of authority (or influence) over the central government decisions. Two of these subcategories measure fiscal elements too (i.e., fiscal autonomy and fiscal control). Since this could generate collinearity issues in our estimations, we remove the values for these two categories and recalculate the RAI overall score, used as our proxy for political decentralisation.
Measuring unfunded mandates is even more intricate, as this indicator has rarely been used as a quantitative variable in its own right. To address this, we have constructed an unfunded mandates index by amalgamating indicators of political and fiscal decentralisation. Following Rodríguez-Pose and Vidal-Bover (Citation2022), we first make fiscal and political decentralisation comparable by standardising them around the mean (mean = 0, standard deviation = 1). We then deduct the standardised fiscal decentralisation values from those of political decentralisation, yielding a relative index that gauges unfunded mandates. A positive value in the unfunded mandates index indicates that a region’s degree of unfunded mandates surpasses the OECD average. Conversely, a negative value suggests that unfunded mandates in that region are less pronounced than in the average OECD region. This novel index provides an estimated degree of unfunded mandates for each region relative to the gap between fiscal and political decentralisation in all the remaining regions of our sample.
The dependent variable measures health outcomes during the COVID-19 pandemic through excess mortality rates. We use data on weekly deaths per region from international, national, and regional statistical offices (depending on availability) to calculate excess mortality rates from the deviation from expected deaths in a specific region over the 24 months covered in the analysis (2020 and 2021). More precisely, excess mortality is estimated by calculating the ratio between the number of deaths per week during the period of interest and the average deaths for the same weeks in the period 2015–19. The weekly data covering the period from January 2020 to December 2021 has been grouped into four categories, corresponding to the four semesters within this time frame. For each semester, the average weekly values for each region are computed. Subsequently, a comparative analysis is conducted between these averaged values and corresponding data from the equivalent semesters spanning 2015–19. Certainly, this proxy is not without its problems. Not all excess deaths during this period were due to COVID-19. Factors such as the fear or inability to reach a hospital during the pandemic may have affected excess mortality. However, even this type of excess mortality is an indirect consequence of COVID-19. Excess mortality is also a more reliable indicator of the health incidence of COVID-19 than other alternatives. Previous research has underlined that using the number of COVID-19 cases or the official toll of COVID-19 deaths is likely to suffer from the deficiencies and inaccuracies of COVID-19 case reporting and from variations and modifications in the definition of what is considered a ‘COVID-19 death’ (Rodríguez-Pose & Burlina, Citation2021). COVID-19 reporting, especially early in the pandemic, also became a political football, which may have influenced reported statistics (Dombey & Burn-Murdoch, Citation2020). Mortality, by contrast, is measured in a far more reliable and consistent way. Hence, sticking to excess mortality circumvents the limitations and vagaries of other types of COVID-19 reporting, as it is generally considered the most accurate indicator of the overall incidence of COVID-19 (Vanella et al., Citation2021).
The analysis also includes several control variables that have previously been deemed relevant in the study of decentralisation and health (Canavire-Bacarreza et al., Citation2017). Seven control variables are used in the analysis. First is the level of development, measured by regional gross domestic product (GDP) per capita as the impact of decentralisation is contingent on the wealth of a territory (Lessmann, Citation2012). We also include demographic indicators, such as population and population density, since COVID-19, as a contagious disease, thrives in the denser environment of larger cities. Similarly, regional accessibility has been identified as a driver of the spread of the disease (Rodríguez-Pose & Burlina, Citation2021). We thus include a measure of interregional mobility as a control. Education is also taken into account, as more educated individuals have shown greater rates of awareness of and adherence to protective behaviours, such as social distancing or mask wearing (Bish & Michie, Citation2010; Kleitman et al., Citation2021). The quality of the air and the environment have also been linked to excess death rates, with recent studies in Poland, Sweden, and Latin America suggesting that worse air quality results in higher COVID-19 mortality rates (Bonilla et al., Citation2023; Semczuk-Kaczmarek et al., Citation2022; Yu et al., Citation2022). We use regional estimates of air pollution as a control. In addition, studies suggest that, even in highly decentralised countries, strong leadership is required to ensure coordination and government effectiveness (Robalino et al., Citation2001). We use the World Bank’s government effectiveness indicator to control for the central government’s ability to coordinate and lead in times of adversity. Finally, we also include a continental dummy variable for the five mega-regions of the OECD: Latin America, North America, Western Europe, Eastern Europe, and Asia and the Pacific. Table A1 in Appendix A in the supplemental data online offers a detailed description of all variables used in this analysis as well as their sources.
3.3. Model specification
To test the two hypotheses, an original dataset containing data for 445 regions in 26 OECD countries has been built. Our dependent variable (COVID-19-related excess mortality) offers reliable data for 24 months, covering the entire 2020 and 2021. Considering the diverse policy strategies implemented across the studied regions during this period, we conduct our estimations for the entire duration as well as in six-month intervals. This approach enables us to identify potential statistical shifts over time. Given the exceptional circumstances of the pandemic, we run a series of ordinary least square (OLS) regressions. The regressions always include all control variables, but the three independent variables of interest are not regressed simultaneously to avoid incurring in multicollinearity. Given that the sign and statistical significance of unfunded mandates are the primary focus of this article, our estimations encompass three regression models for all the examined time periods. These models include one with only unfunded mandates, another with both unfunded mandates and fiscal decentralisation, and a third with unfunded mandates and political decentralisation. Thus, our comprehensive model takes on the following structure:
where
represents excess mortality in region i for period t (pandemic period);
stands for unfunded mandates and denotes the difference between political decentralisation and fiscal decentralisation;
captures the level of fiscal decentralisation;
captures that of political decentralisation; and
encapsulates the seven relevant control variables considered (regional GDP per capita, population, population density, share of population aged 20–64 years old with tertiary education, air pollution, interregional mobility, and government effectiveness).
represents the continental dummy variables, acting as a fixed-effects term; while
denotes the error term. All standard errors are clustered at the regional level to capture potential serial correlation in the residual error term.
4. RESULTS
4.1. Descriptive statistics
Even though OECD regions share many similar characteristics, individual indicators show substantial variation. This is even more the case regarding the degree of decentralisation, where each country has its own historical context and institutional structure. provides a summary of descriptive statistics regarding our main variables of interest.Footnote1 As evident from the minimum and maximum columns, certain regions experience a fiscal and political decentralisation mismatch that is approximately four times greater than that of the region with the smallest discrepancy (consider, for instance, the Silesian voivodeship in Poland and the Irish Mid-West region). Additionally, notable variation exists in the levels of both fiscal and political decentralisation. The data underscore the widely recognised contrast in fiscal and political autonomy between Spain’s autonomous communities and the French regions.
Table 1. Unfunded mandates, decentralisation and COVID-19 excess mortality.
As regards excess mortality, lists the four main periods considered in the analysis. Although this remains descriptive, the mean scores for the six-month periods follow a logical pattern: as the pandemic started in most OECD countries between late February and late March 2020, the period for the first half of the year shows a relatively low mean score (although a significantly high maximum value), if compared to the second half of 2020, which displays a substantial increase probably due to the low immunisation rates of the population at that moment. Later, in the first half of 2021, the population at risk underwent mass vaccination programmes and policy measures to avoid the spread of the virus (such as antigen testing in some countries) may have already been more fine-tuned. Most of these measures remained well into the second half of 2021. Overall, there are significant variations in the sample during the two-year period.
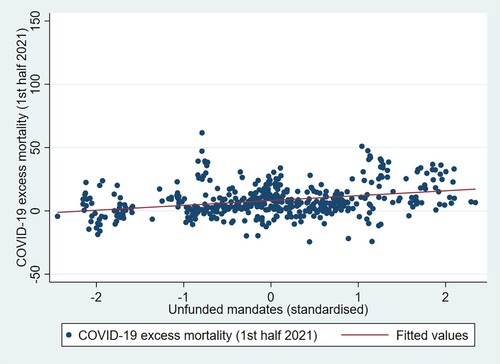
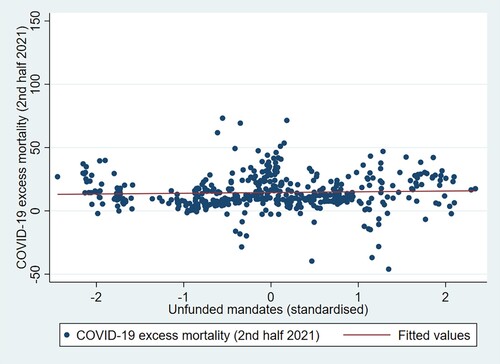
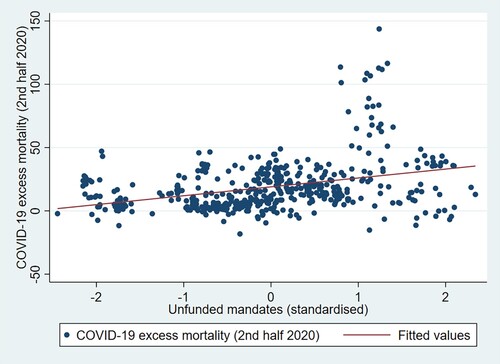
Simple correlation analyses point to a potential, but relatively marginal, link between the presence of unfunded mandates and excess mortality linked to COVID-19.Footnote2 show that, irrespective of the level of unfunded mandates, there is considerable variation in excess mortality rates. Nevertheless, as the regression line shows in all figures – with the exception of – there is a marginally positive correlation between unfunded mandates and excess mortality. Observations showing higher values of excess mortality generally happen when the values of unfunded mandates are above the mean of 0. Although some of these cases could be considered outliers, there is a distinct group of regions with higher values of excess mortality that are also clearly above the average OECD region in terms of unfunded mandates. These include some Mexican states, US states and Polish voivodeships, among others. Conversely, regions with higher than average values of excess mortality coupled with low or average levels of unfunded mandates are far less common. This correlation is most clear in on data for the second half of 2020, when mortality was highest. These correlation graphs point us to the need to apply inferential techniques to assess whether this relationship between variables, which may be driven by some outliers, holds when controlling for a set of relevant factors that may have also influence excess mortality in COVID-19 times.
Figure 1. Unfunded mandates and excess mortality (24 months).
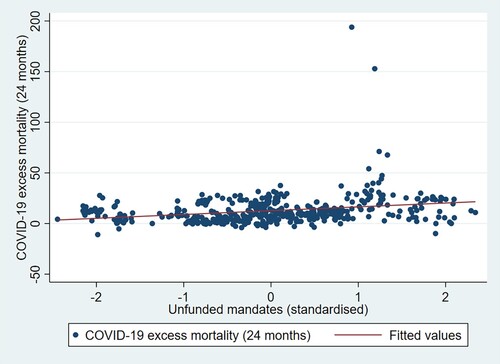
Figure 2. Unfunded mandates and excess mortality (first half 2020).
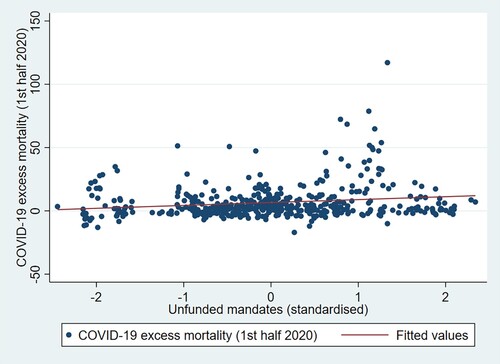
Figure 3. Unfunded mandates and excess mortality (second half 2020).
4.2. Regression results
4.2.1. Regressions for the whole period
We conduct different ordinary least squares estimations using the excess mortality rate during the pandemic as the dependent variable for different periods. Given the cross-sectional structure of our dataset, this method allows for closer examination of time variations. reports the results of conducting five different regressions on the dependent variable for the 24 months for which we have reliable data. First, we examine the behaviour of the two decentralisation variables separately. As can be seen, fiscal and political decentralisation are negatively associated with excess mortality (, regressions 1 and 2). Regional autonomy is thus connected with lower excess mortality, perhaps due to the increased capacity to tailor a region’s response to a crisis depending on its characteristics and resources, as a substantial part of the literature suggests (e.g., Collins & Green, Citation1994; Heitmueller & Roemheld, Citation2020). This is in line with studies that have found, both before or during COVID-19 times, that higher fiscal and political decentralisation is associated with better health outcomes (McCann et al., Citation2022; Robalino et al., Citation2001; Rodríguez-Pose & Burlina, Citation2021).
Table 2. Regressions for excess mortality over 24 months (entire available period).
But what happens when the mismatch between the two main dimensions of decentralisation is considered? What happens when unfunded mandates are included in the analysis? Regression 3 removes the two variables previously analysed separately and adds unfunded mandates. As can be seen, unfunded mandates are extremely relevant when it comes to explaining excess mortality rates. As we had hypothesised, the magnitude, sign, and statistical significance of the estimated coefficient point to the existence of a strong and positive association between unfunded mandates and excess mortality. This is further corroborated in regressions 4 and 5 on . To avoid multicollinearity issues, each of these regressions adds one of the two dimensions of decentralisation. When unfunded mandates are considered in the model together with another decentralisation variable, both variables for fiscal and political decentralisation become insignificant, whilst that of unfunded mandates remains positive and statistically significant at over the 5% level of significance. Hence, while decentralisation may have helped reduce excess mortality during the pandemic, it is in fact not the degree of decentralisation that mattered the most for better health outcomes, but rather the width of the gap between the two dimensions of decentralisation. This represents a clear policy implication for decision-makers when decentralising, as better – not necessarily more – decentralisation is required for the healthcare system to operate more efficiently under a massive health shock like the COVID-19 pandemic.
As for the control variables, we do not observe significant anomalies and all of them are strongly consistent throughout the five regression models. There is no significant relationship between demographic indicators and excess mortality.Footnote3 Similarly, regional GDP per capita does not seem to affect mortality rates. On the other hand, higher education attainment rates are connected to a reduction in excess mortality rates. This gives credence to arguments whereby more educated individuals were more likely to be aware of and comply with health norms as well as adopt greater health precautions (Bish & Michie, Citation2010). Air pollution is significant and positively associated with mortality rates, as indicated by the literature (Cohen et al., Citation2017; Semczuk-Kaczmarek et al., Citation2022; Yu et al., Citation2022). In addition, whereas demographic factors did not seem to exert an impact on mortality rates, interregional mobility appears to push mortality rates upwards.Footnote4 Mobility exposed people to greater risks of contagion, increasing the likelihood of dying from COVID-19 (Bardey et al., Citation2021; Vega-Villalobos et al., Citation2022). Finally, even the most decentralised regions require better institutions (Rodríguez-Pose & Burlina, Citation2021; Rodríguez-Pose and Muštra, Citation2022) and effective leadership and guidance from the central government, especially during an emergency (Capano & Lippi, Citation2021). Accordingly, government effectiveness at the central level is negatively linked with excess mortality and strongly significant at the 1%. All estimations include continental fixed effects, which (although not displayed) show that Latin American regions in OECD member countries had higher mortality rates during the period of analysis than regions in other continental or supranational groupings, once other factors are controlled for.
4.2.2. Regressions for each of the four semesters
In order to explore the temporal variations of a cross-sectional dataset, we split the excess mortality data into four six-monthly periods in . These three periods provide an overview of how the factors that drove the incidence of the pandemic from its very start changed over time.
Table 3. Regressions for excess mortality per semester.
The models for the first semester of 2020 reveal that our main variables of interest (unfunded mandates and fiscal and political decentralisation) are statistically irrelevant to explaining patterns of excess mortality. OECD regions, faced with a phenomenon most of them were ill-equipped for, reacted slowly. They were unprepared and had to improvise and learn how to fight COVID-19 in a process of trial and error. Factors such as the degree of decentralisation or the level of unfunded mandates made virtually no difference as a means to control excess mortality rates (, regressions 1–3). Instead, government effectiveness at the national level was key, as indicated by the high magnitude of the coefficients.
Yet, the process of learning paid off already in the second half of 2020, particularly in regions with a better match between their health responsibilities and the resources at their disposal. During this period, regions with less unfunded mandates became better at fighting the pandemic – the coefficient becomes positive and strongly significant (, regressions 4–6). Regions with higher unfunded mandates, in contrast, were less capable of reacting adequately and far from ready to combat COVID-19. Consequently, excess mortality was significantly higher in these regions. Again, as in , neither fiscal nor political decentralisation alone are relevant to explain these regional disparities in terms of health outcomes. Government effectiveness at the national level remains a pivotal factor (albeit the magnitude of its coefficients is lower than in the previous regressions), and air pollution gains importance and significance, as its coefficients show. With education, population, and regional GDP per capita being statistically significant, this model captures a significant percentage of the existing variation, as shown by the R2 value. These statistical trends were maintained in the first and second semesters of 2021, when larger unfunded mandates were positively associated with excess mortality rates.
Control variables show broadly consistent results, in line with previous research (Rodríguez-Pose & Burlina, Citation2021). The share of educated people is connected to lower regional excess mortality rates, as does central government effectiveness. Conversely, air pollution and, this time, population size are linked to higher mortality rates. Finally, interregional mobility shows significant temporal variation, moving from slightly statistically significant at first, insignificant during the second period, and highly significant in the last two periods. Strict lockdown measures put in place in most countries at the beginning of the pandemic contributed to limit the expansion of the virus (Waitzberg et al., Citation2021). Yet, as lockdowns started to be lifted and interregional mobility re-emerged, mobility became, once again, a factor behind the spread of COVID-19, contributing to greater excess mortality, especially in those OECD regions where immunisation rates were lower.
5. CONCLUSIONS
Since decentralisation processes became a global phenomenon, research has focused most of its efforts in determining what level of decentralisation – fiscal, political or administrative – increases efficiency and enhances the performance in key indicators related to economic development. While some authors have argued that decentralisation spurs economic development (Iimi, Citation2005); others have warned that the economic impact of decentralisation is far less positive (Rodríguez-Pose & Ezcurra, Citation2011) or that there may be an optimal level of decentralisation above which decentralisation’s benefits derail and turn into hindrances (Thießen, Citation2003). This empirical ambiguity is reproduced in studies on the link between decentralisation and health outcomes, with some research perceiving decentralisation as linked to lower mortality rates (e.g., Robalino et al., Citation2001) and others seeing it as related to the opposite (e.g., Navarro et al., Citation2020).
We hypothesise that this heterogeneity of results may stem from the omission of a relevant explanatory variable. To our knowledge, all empirical studies have assessed the effect of the degree of both fiscal and political decentralisation on health outcomes separately. In so doing, these studies assume that ‘finance follows function’, that is, that devolved responsibilities to elected lower tiers of government come with the necessary resources to fulfil them. This is, however, rarely the case as mismatches between powers and resources, also known as unfunded mandates, are more common than the lack thereof (Bahl & Martínez-Vázquez, Citation2013). Hence, the mixed results in existing research leave policymakers blind in the context of decentralisation processes and even becomes dangerous when an emergency situation such as a pandemic emerges. For all we know, decentralisation (or lack of it) may have contributed to increasing or reducing the number of COVID-19 deaths.
Using a novel dataset for 445 regions in 26 OECD countries, our analysis provides regional estimates for unfunded mandates and finds sufficient support to conclude that unfunded mandates matter more than fiscal and political decentralisation by themselves. In other words, it is not so much the degree of fiscal and political decentralisation that is relevant for lower excess mortality during COVID-19, but rather the size of the gap between the two dimensions.
We also find that, at the beginning of the pandemic, OECD regions were, on average, unprepared and rose slowly to the challenge. This may explain why, irrespective of a country’s institutional structure, neither decentralisation variables nor unfunded mandates are significant in the first half of 2020. Once the situation stabilised in the second half of 2020 and governments learned how to fight COVID-19, unfunded mandates became a serious obstacle preventing regions from reacting to the virus and curtailing their capacity to redress excess mortality rates in comparison to those regions with a better match between levels of autonomy and the resources at their disposal. This pattern continued into 2021. Levels of fiscal and political decentralisation, by contrast, become irrelevant for explaining excess mortality rates, when accounting for the mismatch between the two. Hence, it is not the degree of fiscal or political decentralisation that has mattered for health outcomes during the pandemic. Instead, it is the gap between fiscal and political decentralisation that matters for lower excess mortality during COVID-19. Therefore, our models suggest that better rather than more decentralisation should be pursued for OECD healthcare systems to react effectively and in a coordinated manner in the event of a critical emergency, thus being able to save more lives. Our study further highlights that the effectiveness of the national government has a notably strong negative correlation that is statistically significant. This finding lends support to the notion that, regardless of a country’s extent of decentralisation, the central government played a decisive role in issuing national directives, as well as in spearheading and harmonising efforts in combatting COVID-19.
What policy implications can be extracted from this analysis? Policymakers have sometimes perceived and pursued decentralisation as a magic bullet to solve a wide-ranging of economic, societal, and political challenges. Nevertheless, more decentralisation – whether fiscal or political – is unlikely to yield any of the purported benefits if ‘finance does not follow function’. When unfunded mandates are rife, the capacity of autonomous regional governments to deliver on their goals is strongly curtailed. Particularly in the health sector, decentralised entities must be allocated human and financial capacities to make public healthcare accessible to their constituents while the central government may still need to intervene to avoid diseconomies of scale. Otherwise, a scarcity of resources may unleash dysfunctionalities that can contribute to the collapse of healthcare systems and, thus, have a considerable cost in human lives. Therefore, if ‘finance follows function’, the recent COVID-19 experience teaches us that a narrower gap in terms of powers and resources can reduce excess mortality rates in case of health emergencies.
The findings concerning the relationship between unfunded mandates and health outcomes – as well as the broader impact of unfunded mandates on economic development (Rodríguez-Pose & Vidal-Bover, Citation2022) – underline the significance of crafting decentralisation frameworks that empower governing bodies and institutions to efficiently provide public goods and services. This imperative extends beyond healthcare and encompasses sectors such as education, transportation, mobility, waste management, and more. In situations where unfunded mandates persist, the need to potentially reform the decentralisation framework rises. This can involve addressing funding gaps through increased resource allocation or adopting alternative governance mechanisms like inter-municipal or inter-regional cooperation, along with territorial reforms such as municipal or regional mergers or partitions (OECD-UCLG, Citation2022).
As any study in the field of decentralisation, this article is subject to some limitations. Granular data at the regional level for many observations is novel and informative, but it also reduces the data options available. For example, the proxy for political decentralisation (RAI) does provide some regional variation for several countries, but it is rather limited. This complicates the task of investigating within-country differences. In addition, our research cannot be generalised to developing and emerging economies, as the OECD members are selected primarily based on levels of development. It would thus be interesting to consider expanding the analysis to other economies globally to check whether the connection between unfunded mandates and excess mortality holds. Moreover, given the wide variety of decentralisation forms, it would be enlightening to examine data not only on COVID-19 outcomes, but also on the COVID-19 response. Econometric estimations could test the effect of specific policy choices at the regional level on health outcomes, such as adopting stricter or milder types of lockdowns, social distancing measures, antigen testing, or business closures. The effect of these policies would probably be mediated by the level of political decentralisation and, by extension, that of unfunded mandates.
In spite of these limitations and the research possibilities that lie ahead, this article makes a significant contribution to the field of decentralisation by shedding light on the relationship between unfunded mandates and excess mortality rates during COVID-19. By estimating and testing the concept of unfunded mandates – which has so far received limited scholarly attention – we are able to convey the message that pushing for higher levels of decentralisation will not solve issues related to healthcare and may even prove counterproductive. Instead, the focus should be redirected to addressing the mismatches that usually exist between fiscal and political decentralisation. Neglecting this important factor has consequences that go beyond academic discussions of institutional design. Regions with wide unfunded mandates will likely suffer from worse health outcomes and higher excess mortality rates, prompting social discontent about geographical disparities in service provision (Iammarino et al., Citation2019). Therefore, policymakers should ensure that ‘finance follows function’ by building and continuously working towards the improvement of an effective decentralised system that eliminates unfunded mandates and thus removes any potential for healthcare system dysfunctionalities that may end up costing precious lives.
Supplemental Material
Download PDF (261.7 KB)ACKNOWLEDGEMENTS
We thank the special issue editors, the associate editor overseeing the submission, and the three reviewers for their insightful comments and suggestions throughout the refereeing process. We are also grateful to the participants at the 5th DERNET International Conference titled ‘Decentralization and the Governance of Extreme Events’ (organised by the network DERNET and managed by the GEN research group and the Universitat Pompeu Fabra), as well as to those involved in our sessions at the 61st ERSA Congress in Pécs and at an AQR workshop in Barcelona and another one in London. Their collective constructive feedback has considerably enriched the contents of this article. The content of the paper reflects the views of the authors and does not necessarily represent the official views of the OECD.
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the authors.
Notes
1. See Table A4 in Appendix A in the supplemental data online for an extended summary of descriptive statistics for all variables used in the estimations.
2. See Table A5 in Appendix A in the supplemental data online for all possible pairwise correlations with the variables used in this study.
3. Tables A6 and A7 in Appendix A in the supplemental data online incorporate additional demographic indicators, namely weighted population density and the proportion of the young population (aged 15–29) relative to the total regional population, respectively. These supplemental tables show minimal alterations in the regression outcomes, particularly with regard to the variables of primary interest.
4. Table A8 in Appendix A in the supplemental data online reveals that the inclusion of international mobility (referring to the proportion of newcomers from foreign countries to a specific region) holds no statistical significance and has virtually no influence on the outcomes of the regressions presented in .
REFERENCES
- Adler, R. W. (1997). Unfunded mandates and fiscal federalism: A critique. Vanderbilt Law Review, 50, 1137–1256. https://scholarship.law.vanderbilt.edu/vlr/vol50/iss5/2/
- Asfaw, A., Frohberg, K., James, K. S., & Jütting, J. (2007). Fiscal decentralization and infant mortality: Empirical evidence from rural India. Journal of Developing Areas, 41(1), 17–35. https://doi.org/10.1353/jda.2008.0026
- Aubrecht, P., Essink, J., Kovac, M., & Vandenberghe, A.-S. (2022). Centralised and decentralised responses to COVID-19: The EU and the USA compared. Utrecht Law Review, 18(1), 93–107. https://doi.org/10.36633/ulr.738
- Bahl, R. (1999). Fiscal decentralization as development policy. Public Budgeting & Finance, 19(2), 59–75. https://doi.org/10.1046/j.0275-1100.1999.01163.x
- Bahl, R., & Martínez-Vázquez, J. (2013). Sequencing fiscal decentralization. Annals of Economics and Finance, 14(2), 623–670.
- Bardey, D., Fernández, M., & Gravel, A. (2021). Coronavirus and social distancing: Do non-pharmaceutical interventions work (at least) in the short run? Toulouse School of Economics Working Papers, 21(1189), 1–19. https://www.tse-fr.eu/fr/publications/coronavirus-and-social-distancing-do-non-pharmaceutical-interventions-work-least-short-run
- Bennett, J. T. (2014). Mandate madness: How congress forces states and localities to do its bidding and pay for the privilege. Routledge.
- Bish, A., & Michie, S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British Journal of Health Psychology, 15(4), 797–824. https://doi.org/10.1348/135910710X485826
- Boex, J., & Martínez-Vázquez, J. (2006). Local government financial reform in developing countries: The case of Tanzania. Palgrave Macmillan.
- Bonilla, J., López-Feldman, A., Pereda, P. C., Lopez-Feldman, A., Rivera, N. M., & Ruiz-Tagle, J. C. (2023). Association between long-term air pollution exposure and COVID-19 mortality in Latin America. PLoS One, 18(1), 1–21. https://doi.org/10.1371/journal.pone.0280355
- Canavire-Bacarreza, G., Martínez-Vázquez, J., & Yedgenov, B. (2017). Reexamining the determinants of fiscal decentralization: What is the role of geography? Journal of Economic Geography, 17(6), 1209–1249. https://doi.org/10.1093/jeg/lbw032
- Cantarero, D., & Pascual, M. (2008). Analysing the impact of fiscal decentralization health outcomes: Empirical evidence from Spain. Applied Economics Letters, 15(2), 109–111. https://doi.org/10.1080/13504850600770913
- Capano, G., & Lippi, A. (2021). Decentralization, policy capacities, and varieties of first health response to the COVID-19 outbreak: Evidence from three regions in Italy. Journal of European Public Policy, 28(8), 1197–1218. https://doi.org/10.1080/13501763.2021.1942156
- Carinci, F. (2020). COVID-19: Preparedness, decentralization, and the hunt for patient zero. BMJ, 368. https://doi.org/10.1136/bmj.m799
- Cavalieri, M., & Ferrante, L. (2020). Convergence, decentralization and spatial effects: An analysis of Italian regional health outcomes. Health Policy, 124(2), 164–173. https://doi.org/10.1016/j.healthpol.2019.12.001
- Cohen, A. J., Brauer, M., Burnett, R., Anderson, H. R., Frostad, J., Estep, K., Balakrishnan, K., Brunekreef, B., Dandona, L., Dandona, R., Feigin, V., Freedman, G., Hubbell, B., Jobling, A., Kan, H., Knibbs, L., Liu, Y., Martin, R., Morawska, L., … Forouzanfar, M. H. (2017). Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: An analysis of data from the global burden of diseases study 2015. The Lancet, 389(10082), 1907–1918. https://doi.org/10.1016/S0140-6736(17)30505-6
- Collins, C., & Green, A. (1994). Decentralization and primary health care: Some negative implications in developing countries. International Journal of Health Sciences, 24(3), 459–475. https://doi.org/10.2190/G1XJ-PX06-1LVD-2FXQ
- de Biase, P., & Dougherty, S. (2021). Federalism and public health decentralization in the time of COVID-19. OECD Working Papers on Fiscal Federalism, 33, 1–44. https://www.oecd-ilibrary.org/governance/federalism-and-public-health-decentralisation-in-the-time-of-covid-19_b78ec8bb-en
- de Groot, H. (2019). Growth and shrinkage: Challenges for governance and solidarity. In B. Bock et al. (Eds.), Towards a cohesive country: Population decline and regional equality of opportunity (pp. 30–49). Platform31.
- Díaz-Ramírez, M., Veneri, P., & Lembcke, A. C. (2022). Where did it hit harder? Understanding the geography of excess mortality during the COVID-19 pandemic. Journal of Regional Science, 62(3), 889–908. https://doi.org/10.1111/jors.12595
- Di Novi, C., Piacenza, M., Robone, S., & Turati, G. (2019). Does fiscal decentralization affect regional disparities in health? Quasi-experimental evidence from Italy. Regional Science and Urban Economics, 78, 1–14. https://doi.org/10.1016/j.regsciurbeco.2019.103465
- Dombey, D., & Burn-Murdoch, J. (2020). Flawed data casts cloud over Spain’s lockdown strategy. Financial Times, 4, 2020. https://www.ft.com/content/77eb7a13-cd26-41dd-9642-616708b43673
- Donahue, J. D. (1997). Disunited states. HarperCollins.
- Dougherty, S., Lorenzoni, L., Marino, A., & Murtin, F. (2022). The impact of decentralisation on the performance of health care systems: A non-linear relationship. The European Journal of Health Economics, 23, 705–715. https://doi.org/10.1007/s10198-021-01390-1
- Ezcurra, R., & Rodríguez-Pose, A. (2013). Political decentralization, economic growth and regional disparities in the OECD. Regional Studies, 47(3), 388–401. https://doi.org/10.1080/00343404.2012.731046
- Filippetti, A., & Sacchi, A. (2016). Decentralization and economic growth reconsidered: The role of regional authority. Environment and Planning C: Government and Policy, 34(8), 1793–1824. https://doi.org/10.1177/0263774X16642230
- Hao, Y., Liu, J., Lu, Z., Shi, R., & Wu, H. (2021). Impact of income inequality and fiscal decentralization on public health: Evidence from China. Economic Modelling, 94, 934–944. https://doi.org/10.1016/j.econmod.2020.02.034
- Hart, T., & Welham, B. (2016). Fiscal decentralisation: A public financial management introductory guide. Overseas Development Institute. https://cdn.odi.org/media/documents/11063.pdf
- Heitmueller, A., & Roemheld, L. (2020). COVID-19 and the false dichotomy between centralised and decentralised healthcare systems. The BMJ Opinion. https://blogs.bmj.com/bmj/2020/08/05/covid-19-and-the-false-dichotomy-between-centralised-and-decentralised-healthcare-systems/
- Hooghe, L., et al. (2021). Regional authority index (RAI). EUI Research Data. Robert Schuman Centre for Advanced Studies. https://hdl.handle.net/1814/70298
- Hooghe, L., Marks, G., Schakel, A. H., Osterkatz, S. C., Niedzwiecki, S., & Shair-Rosenfield, S. (2016). Measuring regional authority: A postfunctionalist theory of governance, Vol. I. Oxford University Press.
- Iammarino, S., Rodríguez-Pose, A., & Storper, M. (2019). Regional inequality in Europe: Evidence, theory and policy implications. Journal of Economic Geography, 19(2), 273–298. https://doi.org/10.1093/jeg/lby021
- Iimi, A. (2005). Decentralization and economic growth revisited: An empirical note. Journal of Urban Economics, 57(3), 449–461. https://doi.org/10.1016/j.jue.2004.12.007
- Im, H. B. (2021). The US, South Korea, and COVID-19. In J. N. Pieterse, H. Lim, & H. Khondker (Eds.), COVID-19 and governance: Crisis reveals (pp. 179–191). Routledge.
- Jiménez-Rubio, D., & Smith, P. C. (2005). Decentralisation of health care and its impact on health outcomes. Discussion Papers, Department of Economics, University of York. https://www.york.ac.uk/media/economics/documents/discussionpapers/2005/0510a.pdf
- Khambule, I. (2020). A question of capacity and funding: The role of local economic development agencies in South Africa’s development landscape. Urban Forum, 31(1), 95–113. https://doi.org/10.1007/s12132-019-09380-6
- Kleitman, S., Fullerton, D. J., Zhang, L. M., Blanchard, M. D., Lee, J., Stankov, L., & Thompson, V. (2021). To comply or not comply? A latent profile analysis of behaviours and attitudes during the COVID-19 pandemic. PLoS One, 16(7), 1–22. https://doi.org/10.1371/journal.pone.0255268
- Klugman, J. (1994). Decentralisation: A survey of literature from a human development perspective. UNDP Human Development Report Office 1994 Occasional Papers. https://doi.org/10.2139/ssrn.2294658
- Kristiansen, S., & Santoso, P. (2006). Surviving decentralisation? Impacts of regional autonomy on health service provision in Indonesia. Health Policy, 77(3), 247–259. https://doi.org/10.1016/j.healthpol.2005.07.013
- Kuhn, K., & Morlino, I. (2022). Decentralisation in times of crisis: Asset or liability? The case of Germany and Italy during COVID-19. Swiss Political Science Review, 28(1), 105–115. https://doi.org/10.111/spsr.12482
- Lee, N. (2017). Powerhouse of cards? Understanding the ‘Northern powerhouse’. Regional Studies, 51(3), 478–489. https://doi.org/10.1080/00343404.2016.1196289
- Lessmann, C. (2012). Regional inequality and decentralization: An empirical analysis. Environment and Planning A, 44(6), 1363–1388. https://doi.org/10.1068/a44267
- Liwanag, H. J., & Wyss, K. (2018). What conditions enable decentralization to improve the health system? Qualitative analysis of perspectives on decision space after 25 years of devolution in the Philippines. PLoS One, 13(11), 1–20. https://doi.org/10.1371/journal.pone.0206809
- Lv, A., Luo, T., & Duckett, J. (2022). Centralization vs. decentralization in COVID-19 responses: Lessons from China. Journal of Health Politics, Policy and Law, 47(3), 411–427. https://doi.org/10.1215/03616878-9626908
- Martínez-Vázquez, J., Lago-Peñas, S., & Sacchi, A. (2017). The impact of fiscal decentralization: A survey. Journal of Economic Surveys, 31(4), 1095–1129. https://doi.org/10.1111/joes.12182
- Martínez-Vázquez, J., & McNab, R. M. (2003). Fiscal decentralization and economic growth. World Development, 31(9), 1597–1616. https://doi.org/10.1016/S0305-750X(03)00109-8
- McCann, P., Ortega-Argilés, R., & Yuan, P. Y. (2022). The COVID-19 shock in European regions. Regional Studies, 56(7), 1142–1160. https://doi.org/10.1080/00343404.2021.1983164
- Morgan, K. (2002). The English question: Regional perspectives on a fractured nation. Regional Studies, 36(7), 797–810. https://doi.org/10.1080/0034340022000006114
- Naudé, W. (2020). Entrepreneurial recovery from COVID-19: Decentralization, democratization, demand, distribution, and demography. Discussion Paper Series, Institute of Labor Economics, IZA DP No. 13436. https://www.iza.org/publications/dp/13436/entrepreneurial-recovery-from-covid-19-decentralization-democratization-demand-distribution-and-demography
- Navarro, S., Yusingco, M. H., & Sison, S. V. (2020). Interrogating the centralization-decentralization tension in the Philippines in the midst of the COVID-19 pandemic. ASOG Working Paper, 20((010|10)), 1–25. https://doi.org/10.2139/ssrn.3721883
- Oates, W. E. (1972). Fiscal federalism. Harcourt Brace Jovanovich.
- Organisation for Economic Co-operation and Development (OECD). (2017). Multi-level governance reforms: Overview of OECD country experiences. OECD Multi-Level Governance Studies, OECD Publ. https://doi.org/10.1787/9789264272866-en
- Organisation for Economic Co-operation and Development (OECD). (2020). The territorial impact of COVID-19: Managing the crisis across levels of government. OECD Policy Responses to Coronavirus (COVID-19). https://doi.org/10.1787/a2c6abaf-en
- Organisation for Economic Co-operation and Development (OECD). (2021a). Health at a glance 2021: OECD indicators – Excess mortality. https://www.oecd-ilibrary.org/sites/ec2de914-en/index.html?itemId=/content/component/ec2de914-en
- Organisation for Economic Co-operation and Development (OECD). (2021b). Regional statistics. https://stats.oecd.org/Index.aspx?DataSetCode=REGION_DEMOGR
- OECD-UCLG. (2022). 2022 synthesis report world observatory on subnational government finance and investment. OECD Publ. https://doi.org/10.1787/b80a8cdb-en
- Posner, P. L. (1998). The politics of unfunded mandates: Whither federalism? Georgetown University Press.
- Prud’homme, R. (1995). The dangers of decentralization. The World Bank Research Observer, 10(2), 201–220. https://doi.org/10.1093/wbro/10.2.201
- Rakmawati, T., Hinchcliff, R., & Pardosi, J. F. (2019). District-level impacts of health system decentralization in Indonesia: A systematic review. The International Journal of Health Planning and Management, 34(2), e1026–e1053. https://doi.org/10.1002/hpm.2768
- Robalino, D. A., Picazo, O. F., & Voetberg, A. (2001). Does fiscal decentralization improve health outcomes? Evidence from a cross-country analysis. Policy Research Working Papers, 2565, 1–20. https://openknowledge.worldbank.org/handle/10986/19698
- Rodrik, D., Subramanian, A., & Trebbi, F. (2004). Institutions rule: The primacy of institutions over geography and integration in economic development. Journal of Economic Growth, 9(2), 131–165. https://doi.org/10.1023/B:JOEG.0000031425.72248.85
- Rodríguez-Pose, A., & Burlina, C. (2021). Institutions and the uneven geography of the first wave of the COVID-19 pandemic. Journal of Regional Science, 61(4), 728–752. https://doi.org/10.1111/jors.12541
- Rodríguez-Pose, A., & Ezcurra, R. (2011). Is fiscal decentralization harmful for economic growth? Evidence from the OECD countries. Journal of Economic Geography, 11(4), 619–643. https://doi.org/10.1093/jeg/lbq025
- Rodríguez-Pose, A., & Gill, N. (2003). The global trend towards devolution and its implications. Environment and Planning C: Government and Policy, 21(3), 333–351. https://doi.org/10.1068/c0235
- Rodríguez-Pose, A., & Muštra, V. (2022). The economic returns of decentralisation: Government quality and the role of space. Environment and Planning A: Economy and Space, 54(8), 1604–1622. https://doi.org/10.1177/0308518X221118913
- Rodríguez-Pose, A., & Vidal-Bover, M. (2022). Unfunded mandates and the economic impact of decentralisation. When finance does not follow function. Political Studies. https://doi.org/10.1177/00323217221136666
- Schneider, S. (2008). Who’s to blame? (Mis)perceptions of the intergovernmental response to disasters. Publius: The Journal of Federalism, 38(4), 715–738. https://doi.org/10.1093/publius/pjn019
- Semczuk-Kaczmarek, K., Rys-Czaporowska, A., Sierdzinski, J., Szymanski, F. M., & Platek, A. E. (2022). Association between air pollution and COVID-19 mortality and morbidity. Internal and Emergency Medicine, 17(2), 467–473. https://doi.org/10.1007/s11739-021-02834-5
- Thießen, U. (2003). Fiscal decentralisation and economic growth in high-income OECD countries. Fiscal Studies, 24(3), 237–274. https://doi.org/10.1111/j.1475-5890.2003.tb00084.x
- Vanella, P., Basellini, U., & Lange, B. (2021). Assessing excess mortality in times of pandemics based on principal component analysis of weekly mortality data – The case of COVID-19. Genus, 77(1), 1–16. https://doi.org/10.1186/s41118-021-00123-9
- Vega-Villalobos, A., Almanza-Ortega, N. N., Torres-Poveda, K., Pérez-Ortega, J., & Barahona, I. (2022). Correlation between mobility in mass transport and mortality due to COVID-19: A comparison of Mexico city, New York and Madrid from a data science perspective. PLoS One, 17(3), 1–14. https://doi.org/10.1371/journal.pone.0264713
- Waitzberg, R., Hernández-Quevedo, C., Bernal-Delgado, E., Estupiñán-Romero, F., Angulo-Pueyo, E., Theodorou, M., Kantaris, M., Charalambous, C., Gabriel, E., Economou, C., Kaitelidou, D., Konstantakopoulou, O., Vildiridi, L. V., Meshulam, A., de Belvis, A. G., Morsella, A., Bezzina, A., Vincenti, K., Augusto, G. F., … Maresso, A. (2021). Early health system responses to the COVID-19 pandemic in Mediterranean countries: A tale of successes and challenges. Health Policy, SI, 1–11. https://doi.org/10.1016/j.healthpol.2021.10.007
- Yu, Z., Bellander, T., Bergström, A., Dillner, J., Eneroth, K., Engardt, M., Georgelis, A., Kull, I., Ljungman, P., Pershagen, G., & Stafoggia, M. (2022). Association of short-term air pollution exposure with SARS-CoV-2 infection among young adults in Sweden. JAMA Network Open, 5(4), 1–12. https://doi.org/10.1001/jamanetworkopen.2022.8109
- Zaidi, S. A., Bigdeli, M., Langlois, E. V., Riaz, A., Orr, D. W., Idrees, N., & Bump, J. B. (2019). Health system changes after decentralization: Progress, challenges and dynamics in Pakistan. BMJ Global Health, 4(1), 1–8. https://doi.org/10.1136/bmjgh-2018-001013
- Zarychta, A. (2020). Making social services work better for the poor: Evidence from a natural experiment with health sector decentralization in Honduras. World Development, 133, 1–16. https://doi.org/10.1016/j.worlddev.2020.104996