ABSTRACT
Despite common lessons learned during the SARS pandemic in 2003, country responses to the COVID-19 pandemic in Southeast Asia have been very diverse, with many lacking coordination among government bodies. I consider how government structure and political decentralisation shape emergency response to extreme events, focusing on two of Southeast Asia’s largest decentralised countries, Indonesia and the Philippines. I explore variation in provincial-level responses and outcomes, showing that intergovernmental coordination can augment the beneficial aspects of decentralisation in world regions where human and economic costs associated with extreme events are high.
1. INTRODUCTION
The COVID-19 pandemic highlighted an extreme circumstance of crisis response pressures facing governance regimes around the world, with evident regional variation in the severity of the pandemic’s effects (Bourdin & Levratto, Citationforthcoming; Guaitioli & Pancrazi, Citation2021; Pandey & Saxena, Citation2022). Federal systems in India and the United States saw wide-ranging policies adopted by state governments, including restrictive measures – e.g., lockdowns, school closures and mask and vaccine mandates – and forms of assistance – e.g., mobile telemedicine units, income support and emergency investment in healthcare systems. Although some state-level policies were applauded for their originality and effectiveness, their non-uniform application tended to exacerbate inequalities in COVID-19 outcomes (c.f., Wong & Balzer, Citation2022).
In Southeast Asia, countries with highly diverse and increasingly urbanised populations faced a number of distinct challenges in their responses to COVID-19. The vast share of their populations live in low- and middle-income countries (LMICs) where healthcare systems are underdeveloped and state capacity is generally weak. Air pollution is a problem in nearly every country in the region, contributing to already poor respiratory health before the pandemic. The presence of megacities in nearly every country posed a severe risk of the rapid and unmanageable spread of COVID-19 and overwhelmed hospital systems, while most of Southeast Asia’s rural populations live so far from modern infrastructure and healthcare that non-urban spread of COVID-19 posed a distinct risk to loss of life among already economically-disadvantaged populations.
In the early months of the pandemic, some Southeast Asian countries were better able to prevent wide-scale outbreaks. Yet, data from the larger countries showed clear regional variation in infection and fatality rates during transmission waves. Decentralisation appears to exert a complex influence in how effective crisis management systems work in the region. After controlling for level of economic development and urbanisation, decentralised countries with higher degrees of intergovernmental coordination appeared more capable of developing consistent policies, communicating to their populations with clearer messaging and facilitating testing and vaccination programmes. Conversely, decentralised countries with limited channels for coordination often fought to stay ahead of the pandemic in the early months and subsequently struggled with vaccine rollouts later on, notably exhibiting greater within-country regional variation.
In the following sections, I offer a critical perspective on the potential for decentralisation to improve emergency response in LMIC contexts. While the extant literature focuses heavily on the importance of coordination between national-level agencies (An & Tang, Citation2020) and between international and domestic partners (Zhang et al., Citation2023), I argue that crisis management systems produce worse outcomes when they fail to coordinate among different levels of government within a decentralised country, e.g., between national and regional governments.Footnote1 I evaluate my argument using a comparative subnational analysis of health outcomes from the COVID-19 pandemic, alongside analysis of casualty and affected population outcomes that result from other natural extreme events and disasters from 1990 to 2022, in Indonesia and the Philippines. The analysis shows the importance of national-regional coordination in shaping emergency health outcomes across regions in unitary but decentralised countries. It also provides a distinctly LMIC perspective to wider debates about how coordination shapes outcomes in response to crisis (Bourdin & Levratto, Citationforthcoming; McCann et al., Citation2022; Palomino et al., Citation2023) and improves responsiveness and resilience (Arias-Yurisch et al., Citationforthcoming; Bailey et al., Citation2021; Berta et al., Citation2022).
2. HOW DECENTRALISATION SHAPES GOVERNANCE DURING CRISIS MANAGEMENT
Scholars and development specialists have highlighted the merits of decentralised forms of governance as a means to improving government representation, accountability and responsiveness (Blair, Citation2000; Faguet, Citation2014). Bringing government decision-making ‘closer to home’ theoretically leads to more effective governance because regional decision-makers are more likely to know the needs of their local population better and to be more aware of the infrastructural and demographic challenges facing policy adoption and implementation (Dias-Cayeros et al., Citation2014; Faguet, Citation2004). Regional decision-makers are also more likely to be susceptible to community-based pressures, claims of shared identity with, or electoral competition within the local population that result in greater responsiveness and attentiveness to local demands (Fiszbein, Citation1997; Gonçalvez, Citation2014). In theory, localised decision-making results in more responsive elites and better governance, and should empower and engage local populations with positive consequences for democratic governance and accountability.
Yet, healthcare provision is an area where greater regional authority often leads to conditional and inconsistent outcomes. Empowering local decision-makers can reduce healthcare inequities in lower socio-economic groups by improving community-based care provision and successfully targeting those groups with specialised messaging (Regmi et al., Citation2010). However, assessment of access and utilisation of different types of healthcare initiatives reveals stark differences in how decentralisation affects the demand and supply of services because the ability to claim credit for healthcare’s social benefits conditions how much regional authorities are willing to invest in access and service improvements (Bardhan & Mookherjee, Citation1998; Besley & Coate, Citation2003; Birn et al., Citation2000).
Conversely, certain aspects of nationalised models improve healthcare service provision. Incentives to improve provision may be absent at subnational levels due to a lack of clear responsibility attribution (Hicken et al., Citation2016), and uniform subnational capacity to deliver healthcare tends to exist only in middle- and high-income countries, leading to worse outcomes in LMICs (Khaleghian, Citation2004). Capacity gaps in healthcare provision and local governance exacerbate inequity in care quality across a country (Maharani & Tampubolon, Citation2015). Capacity is an especially acute issue for healthcare provision that requires routine clinician retraining (Namazzi et al. Citation2017) or coordination of information regarding standards in patient care, local trends in outcomes and processes to collect, track and share individual patient data (La Vincente et al., Citation2013; Lakshminarayanan, Citation2003).
In the context of crisis management, the relationship between decentralised systems and policy outcomes becomes even more complex and amplified: decentralisation is linked to extremes of both shockingly poor and highly effective governmental response at the subnational level (Lele, Citation2023; Shringare & Fernandes, Citation2020). When a crisis demands a rapid and comprehensive response, regional governments may be strategically well-positioned to provide immediate and targeted support, yet they may lack the necessary financial resources or full information to execute that supporting role (Schlegelmilch et al., Citation2015). Consider management of the response to a typhoon-induced mudslide or a highly-contagious mosquito-borne pandemic – those situations require local know-how and supportive central governments to mobilise an effective response.
While response to COVID-19 represented a unique situation, with limited precedent in modern medical history, three lessons from the broader literature on crisis management are of particular importance here. First, local capacity is an immense hurdle facing the most effective and efficient deployment of crisis response. It is critical to develop and maintain local capacity, and also key to sustain that capacity by regularly updating and communicating national and international standards in best practices (Asmorowati et al., Citation2022; Putra & Matsuyuki, Citation2019). Second, communication mechanisms are often insufficiently developed or poorly executed, especially with respect to channelling regulations among levels and agencies of government and transmission of data to enable more adaptive responses (Comfort et al., Citation2004; Gillespie et al., Citation2016). Finally, coordination among partners at different levels or from different jurisdictions is a widely referenced challenge in mounting an effective response to crises, especially those that span internal and external borders, diffuse rapidly and affect multiple different aspects of the physical and economic health of a nation (Arias-Yurisch et al., Citationforthcoming; Comfort et al., Citation2020).
3. WHY DECENTRALISATION WITHOUT COORDINATION HAMPERS RESPONSE TO CRISIS
Even with adequate resource input, the transfer, management and use of those resources may still fail to ensure crisis response and effective service provision due to an absence of coordination between the central government and ministries who typically provide or manage the distribution of resources and the local governments utilising them (Schlegelmilch et al., Citation2015). Where local governments and civil servants are empowered to make decisions about the best way to implement policies and respond to emergency situations, they may still rely upon or benefit from national officials and high-ranking bureaucrats providing up-to-date information, coordination among local government units and dissemination of best practices and innovative approaches in public administration. In short, even if local governments and civil servants know the local lay of the land, they are still likely to find assistance and value in the resources provided and coordinated at the national level.
Comfort (Citation2007) highlights coordination – aligning resources, tasks and time to achieve a shared goal – as one of four critical aspects of emergency management. In this context, coordination facilitates crisis response by providing a framework through which distinct actors share a common goal and pool their respective resources and perspectives to help achieve that goal. Such coordination mimics non-traditional leadership approaches to governance, which prioritise communal or transformational decision-making: the collectively-decided sum of diverse and varied viewpoints and assessments leads to more innovative and responsive policy-making, especially in challenging political environments (c.f., Shair-Rosenfield & Wood, Citation2017). Yet, the literature that emphasises the importance of coordinreeeation in crisis response and management typically addresses its role in facilitating governance between actors and agencies at the national level (An & Tang, Citation2020) or among supranational actors and national governments (Zhang et al., Citation2023).
Where attention to coordination between national and regional governments exist, the focus tends to be on federal or highly decentralised OECD countries, such as the US and Italy. These find that an absence of coordination can hamper governance and response mechanisms where regions are especially empowered (c.f., Guaitioli & Pancrazi, Citation2021; Haffajee & Mello, Citation2020). But many LMICs with decentralised political, administrative or fiscal authority arrange these systems under much ‘weaker’ versions of devolution compared to the structure and authority granted to the US or Italian regions (c.f., Shair-Rosenfield et al., Citation2021). Because central authorities still retain substantial control over policymaking and resourcing disbursement, the role of coordination in unitary and decentralised systems in LMICs is presumed extraneous and thus remains underexplored. Consider healthcare, where there is often a national health ministry whose structure is replicated in regional and local agencies, which are then tasked to organise and provide aspects of healthcare to their populations. In a weakly decentralised health system, data sharing may be uniformly structured through a common data portal, but this relies on local capacity for input and requires central monitoring to ensure uniform use and standardised outputs. This example suggests that such systems may rely on generally-accepted benchmarking and target standards, yet outputs and metrics may not be consistently applied. Finally, weakly decentralised systems may follow relatively uniform processes for staffing recruitment and compensation, but need local resources in order to actually fulfil these obligations.
Due to their lack of coordination between central, regional, and local entities, such decentralised systems in LMICs often fail in their ability to facilitate service delivery and responsiveness, especially during periods of crisis.Footnote2 Key to explaining the quality of governance during an emergency is the degree to which channels for coordination – to disseminate clear and consistent information, to funnel resources up and down the vertical chain of command, and to clarify distribution of responsibilities – exist among decentralised actors. Particularly where there are region-specific inequalities, such as weak local capacity or limited financial resources common in LMICs, coordination becomes even more important. In such contexts, vertical coordination between the national ministry and regions or horizonal coordination among regions may reduce the effect of those inequalities. For example, where regional capacity in healthcare provision is weak, strong coordination can help direct crucial information about basic standards and best practices, enable regular training by national experts with local practitioners or reduce capacity gaps by coordinating staffing processes and service delivery through routine consultations among partners.
4. CHALLENGES TO EMERGENCY MANAGEMENT AND CRISIS RESPONSE IN SOUTHEAST ASIA
From the perspective of crisis management, Southeast Asian countries face numerous challenges related to weak and/or non-uniform capacity across regions. The countries comprise approximately 8.5% of the world’s population and are home to some of the world’s fastest urbanisation in the past half century. Many of the region’s countries have large and/or highly diverse landscapes that sit on the Ring of Fire in the path of frequent natural disasters due to extreme weather and seismic activity. Since 2000, five of the world’s 15 deadliest earthquakes (many provoking large and destructive tsunamis) occurred there, incurring tens of thousands of lives lost and immense damage to property and infrastructure. Typhoons and other cyclones with the potential for tremendous devastation due to high winds and subsequent high rainfall are common events in the region.
The scale of populations, geographic diversity and climactic challenges faced in the region has resulted in a great deal of attention placed on building government capacity in risk management and preparedness to face natural disasters. Yet, many Southeast Asian countries have weak state capacity and infrastructure. Since block transfers and grants comprise a substantial portion of the resources available to regions to finance policy implementation, local governments rarely fully control their ability to meet key service delivery goals. When combined with generally high levels of corruption, poor oversight and limited accountability mechanisms (c.f., Atkinson et al., Citation2015; Hutchcroft, Citation2012), most government responses to crises have been inadequate and reliant on improvements from infusions of resources from international partners. Partners including the Association of Southeast Asian Nations, United Nations Development Programme and the US and Australian Agencies for International Development have created platforms for sharing information to improve risk assessment, risk management and disaster preparedness.Footnote3 However, many of these efforts have emerged only as ‘Build Back Better’ initiatives expanded in recent years (Fernandez & Ahmed, Citation2019).
4.1. Lessons from comparing intergovernmental coordination in Indonesia and the Philippines
To evaluate the relationship between decentralisation and intergovernmental coordination on COVID-19 outcomes in Southeast Asia, I use a paired comparison of two cases: Indonesia and the Philippines. The two cases are often considered to follow a ‘Most Similar Systems Design’, with geographic, political and socioeconomic similarities that are important to control for in social scientific analysis (c.f., Eaton & Shair-Rosenfield, Citationforthcoming). Both are archipelagos facing environmental and infrastructural challenges that are often exacerbated by their generally weak states and endemic corruption. They have similar modest levels of economic development, populations in urban areas and over 65 years of age and incidence of cardiovascular disease and diabetes in their populations. Both countries now have national health insurance schemes administered by the central government, though the Philippines began its roll out 20 years earlier than Indonesia.
Decentralisation occurred shortly following each country’s transition to democracy, and both were praised by international nongovernmental organisations for their speed of decentralisation. They have comparable (and comparatively average) levels of decentralisation at the first tier of subnational government in cross-national datasets: the standard Indonesian provinces, Philippines provinces and Philippines highly-urbanised and independent component cities (HUCs and ICCs) all score ‘11’ on self-rule in the Regional Authority Index (Shair-Rosenfield et al., Citation2014), a commonly-used decentralisation measure. In Indonesia, decentralisation in a range of policy areas empowers both the first (provincial) and second (municipal) tiers of regional government. However, fears of regionalism and secessionist pressures prompted the strategy of empowering both levels, resulting in a dilution of capacity building for coordinated service delivery at the provincial level. While the Philippines has long eschewed full-scale federalism, it has decentralised substantial authority and financial resources to the provinces and independent cities that comprise its primary regional layer of government. Fiscal transfers follow a relatively automated formula and disbursement process, so that subnational units are well aware of what resources will be available, from provincial all the way down to barangay (village) level.Footnote4
4.2. Comparing COVID-19 responses and outcomes
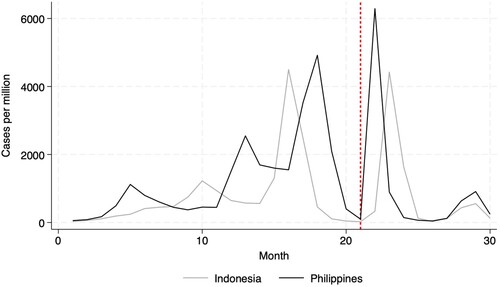
The two countries demonstrated some similarities in their response and ability to mitigate some of the worst outcomes from COVID-19. shows patterns in new monthly COVID-19 cases from April 2020 to September 2022, with Indonesia the grey line, the Philippines the black line and the dashed reference bar showing when the Omicron variant emerged in December 2021. The Philippines shows an especially high peak following the emergence of the Omicron variant due to high socialisation levels over the Christmas holiday in the Catholic country. While both countries enforced travel restrictions for most of 2020-21, the Philippines reintroduced constraints at the outset of the Delta variant’s spread that remained until the spring of 2022.
Figure 1. New monthly cases per 1 million population.
Source: Our World in Data (Ritchie et al., Citation2020).
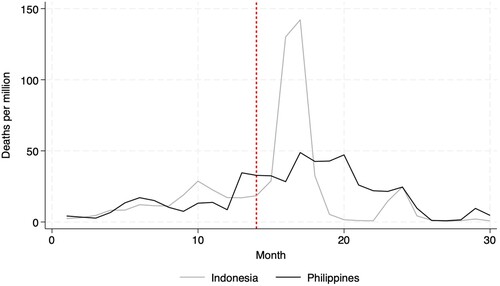
In contrast, there was greater divergence in new death trends following the Delta variant’s spread in 2021. shows the new monthly death counts, scaled to 1 million population, with the dashed reference bar indicating when Delta became the dominant variant globally. The high peak in deaths in the Indonesian case corresponds to the spread of Delta, but then from 2022 the two countries follow similar patterns in new low monthly death counts. Much of the decline and continued low rate is due to their vaccination programmes, where similar and fast increasing rates of full vaccination occurred from December 2021.
Figure 2. New monthly deaths per 1 million population.
Source: Our World in Data (Ritchie et al., Citation2020).
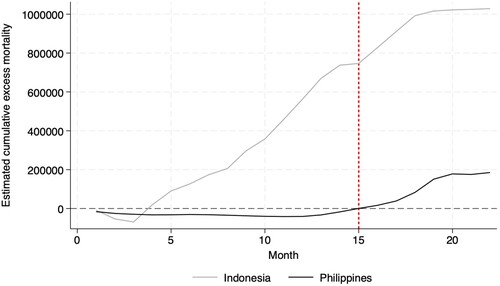
Importantly, the estimated excess cumulative mortality figures suggest a clearer point of divergence between the less coordinated Indonesian case and the more coordinated Philippines case. shows the estimated cumulative excess mortality counts from the WHO. While the Philippines remains net negative in terms of excess mortality through May 2021,Footnote5 Indonesia’s excess mortality becomes positive quite early in the pandemic and continues to climb to the highest rate in Southeast Asia. Yet, given their similarities in most other respects, what explains this divergence?
Figure 3. Estimate cumulative excess mortality.
Source: World Health Organization.
4.3. Contrasting within-case variation in response to extreme events at the provincial level
Closer examination of region-level differences within the two cases points to the role of more limited attention to and investment in coordination shaping this divergence between the Indonesian and Philippines cases. Situated within the broader context of crisis management, preparation for and responses to extreme events, it is unclear why such a divergence would emerge. Both countries face high annual levels of extreme events which are not uniformly distributed across the country. Similar extreme events plague both, including earthquakes, floods and landslides, tidal waves/tsunamis, cyclones/typhoons and forest and land fires, with state-level emergency management agencies facing routine criticism for failures to prepare and respond. Both countries receive funding and capacity building support from international agencies to help develop coordinated resilience projects and pilot interventions and trial programming have targeted specific local governments that are deemed to be at enhanced risk for human and economic costs of extreme events and climate crises.
Additionally, both cases are comparably decentralised in terms of governance, although the Philippines has a much larger number of first-tier subnational units (121–34 in Indonesia) due to the distinction in HUCs and ICCs that operate outside of provincial control. This means that there are potentially greater coordination issues, both among first-tier units in general and between HUCs and ICCs that are physically located within a province that does not directly govern them. Despite this complicating factor, the response to COVID in the Philippines has actually been better, at least as measured by the excess mortality rate.
Part of the reason for Indonesia’s much higher cumulative excess mortality rate results from evident failures in data sharing and coordination across levels of government: in the summer of 2021 when the Delta variant drove a huge surge in cases and deaths, discrepancies detected by an independent domestic data initiative in IndonesiaFootnote6 showed that regional governments were reporting different case and death rates. The lack of consistent data sharing during the surge led to difficulties in mounting an effective government response, especially given the government’s transfer of authority over testing sites to the military instead of health authorities (Indonesian Presidential Decree Nos. 7 and 9 Year 2020). In contrast, particularly during the Delta wave and into the vaccination rollout, no similar reporting of data coordination failures emerged from the Philippines where health authorities at national and local levels remained the source of testing and vaccinations.
In Indonesia, variations in response to COVID-19 centred on weak capacity as the explanation for failure to reduce positivity and excess mortality rates. Decentralisation hampered efforts to remain on top of transmission and fatality rates, in large part because the relatively free-flow of people across subnational borders was not coupled by a similar free-flow of data sharing by local authorities or consistent coordination between local, provincial, and national authorities. The Ministry of Health’s organisational structure follows a uniform decentralised arrangement: the general structure and major personnel of the national ministry is reflected in a companion group in the subnational ministry at each province, city and municipality at the first and second tiers of government. Yet, much of the limited data sharing and coordination was further stymied by the fact that the military (Tentara Nasional Indonesia or TNI), rather than the Ministry of Health, was tasked with much of the COVID-19 response effort. This ensured that various aspects of data sharing and coordination were further complicated by the addition of another agency to the governing process.
In recent years, an effort to improve health inequalities between urban and rural populations and between the ‘Inner’ (e.g., on Java) and ‘Outer’ (e.g., farmost Eastern and Western) provinces has led to greater emphasis on building more public health clinics (pusat kesehatan masyarakat), known by the shorthand ‘puskesmas’, in underserved localities. This particular expansion in access to basic healthcare services reflects an attempt to reduce disparities between populations that have a multitude of options – urban settings with both public hospitals and private clinics – and those whose geographic location reduces the chance that they reside within a 4-hour trip from the nearest health facility. The six provinces on Java underscore the reality that while puskesmas growth on Java has remained stagnant compared to elsewhere in the country, private healthcare options in urban and peri-urban areas have proliferated since the early 2000s and now account for a substantial part of healthcare service utilisation in these settings, especially in the western half of the island (the provinces of Banten and West Java, plus the Jakarta metropolitan region).
Outside of urban centres on Java, local populations should be better able to access routine health services where access to puskesmas is most comprehensive. These are also settings where the local population should be most likely to know how and where to access health services within their local community, and thus not need to travel to seek care elsewhere. As a result, where there are higher puskesmas-to-population ratios, there should generally be healthier populations who know there is healthcare access within the local community. However, the advancement of puskesmas access in rural communities and ‘off-Java’ communities does not come with commensurate investment in coordination between puskesmas providers and local, provincial and national health services more generally. And the proliferation of private health options in areas where there has not been improvement in puskesmas access further magnify these discrepancies: private providers do not tend to engage in any forms of coordination with government-financed healthcare providers, they serve to complement (or displace) public care provision (Chee et al., Citation2009).
In the Philippines, there is a similar parallel structure between national, provincial and city health officials as exists in Indonesia. However, during COVID-19 there were more central restrictions imposed on the population than in Indonesia, and for a longer duration. While decentralisation hampered efforts to reduce transmission rates, especially around major religious holidays when there was increased travel, there was a generally stronger effort and success in sharing and tracking data across subnational units. This was especially true within the context of the HUCs and ICCs within provincial geographic boundaries, where a lot of within-geographic province travel occurred but was easier to contain and measure in terms of spread and transmission than cross-provincial travel.
In the Philippines, barangay health clinics and rural health units are rooted in a community-based approach to service provision initially inherited from the Spanish colonial system that predates both authoritarian recentralisation and more recent efforts at decentralisation. Nestled in communities at the most local level within the current decentralised system of governance, these clinics and health units are coordinated through the national Department of Health (DoH) and the national insurance system, PhilHealth, with intermediary support at the city level (HUCs/ICCs alongside the small component cities). There are elements of coordination and data sharing between local providers and national health officials for health services such as childhood nutrition and maternal healthcare, with efforts to track progress and target underperforming barangay. While capacity and resource issues plague the barangay clinics, and patients typically must be referred for more complex treatments, these clinics are well embedded in local communities while simultaneously incorporated into provincial and national, networks that transmit challenges upward.
Two specific mechanisms in the Philippines further underscore the ways in which coordination and collaboration across levels of government occur. First, greater collaboration between the DoH and local units has been formalised in the 1997 Comprehensive Healthcare Agreement and implemented via the DoH’s Local Government Assistance and Monitoring Service, both of which acknowledge and provide systemic response to capacity differences and variation across localities (Perez, Citation1998). Second, the Local Government Code of 1991 provided for local health boards, among other such sectoral bodies, each of whose membership includes a local government unit representative, a DoH representative, and a representative of the private or local NGO health sector (Bossert & Beauvais, Citation2002, p. 25). The local health boards are responsible for, among other roles, proposing the local annual health budget and advising local health agencies on community matters (Bossert & Beauvais, Citation2002). Other advances, including multiple pieces of legislation expanding and embedding the national insurance scheme and standardisation of healthcare worker payscales, enhanced the universality of care standards and required coordination between different healthcare levels in the Philippines. As a result, the response to public health crises tends to be much more coordinated, beyond basic data sharing to encompass best practices and universal standards of care provision. No comparable coordination or standardisation mechanisms exist in Indonesia.
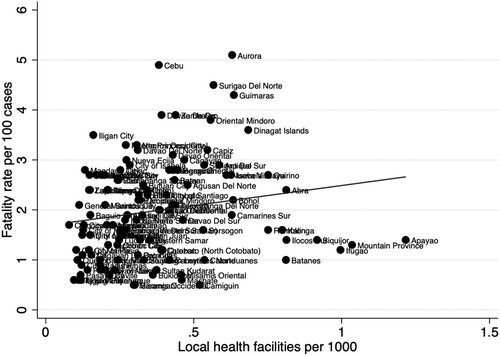
One way to consider the role of coordination in response to COVID-19 is to evaluate the relationship between rates of local health providers such as the barangay health clinics and puskesmas and fatality rates. Where clinics are built specifically to address access gaps between under- and better-served communities, more clinics should translate into better health outcomes across different localities. Weak coordination makes this simple relationship evident – the presence of more (fewer) health facilities should simply translate into better (worse) local health outcomes – whereas a better coordinated system may be able to otherwise compensate for access disparities. In the case of weak coordination, we should expect that higher clinic coverage rates will be associated with lower COVID fatality rates. Alternatively, where widespread access to these types of clinics is long-standing or even focused on preventive care, rather than newly created to reduce access gaps between localities, additional clinics should have limited impact on health outcomes. Here, stronger coordination makes this especially true because health outcomes should already be more uniform (and better), and thus less susceptible to differences in per capita health facility rates. Thus, each additional facility has limited impact on access and health outcomes for the local population and the observed correlation should be weak or non-existent.
To evaluate these propositions in the Indonesian and Philippines cases, I aggregate the presence of clinics (puskesmas in Indonesia and barangay health clinics and rural health units in the Philippines) to the total number located within the subnational unit then scaled to the subnational unit’s population (in 1000s). This results in a comparable first-tier regional unit measure. The COVID-19 fatality rate is also calculated at the provincial or HUC/ICC level, with the total deaths as the numerator and the total case rate as the denominator (both reported by the national statistical agency’s official health measures accounting for COVID positivity and associated death). The Indonesian data come from the Indonesian Central Statistics Bureau and the Ministry of Health’s COVID tracker, and the Philippines data come from the National Health Facility RegistryFootnote7 and the Department of Health’s COVID tracker.Footnote8 shows the scatterplot and fit line for Indonesia and shows the scatterplot and fit line for the Philippines, with each dot representing a first-tier subnational unit labelled by name or official acronym. The time period is from March 2020 until September 2022.
Figure 4. Indonesian puskesmas and COVID fatality rates by province.
Sources: Indonesian Central Statistics Body; Indonesian Ministry of Health.
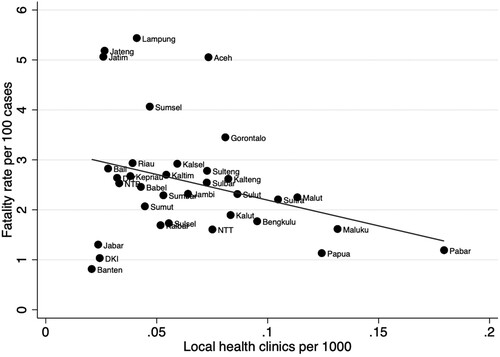
Figure 5. Philippines health clinics and COVID fatality rates by province/HUC/ICC.
Sources: Philippines National Health Facility Registry; Philippines Department of Health.
As indicates, there is a negative correlation between the puskesmas rate and fatality rate at the provincial level in Indonesia. The vast majority of Indonesia’s 34 provinces fall relatively close to the fit line, with some outliers at the lower end of the x-axis: provinces on the island of Java have very low rates of puskesmas but are split between very low and very high COVID-19 fatality rates. Much of this difference stems from an important on-Java distinction. Jakarta (DKI), West Java (Jabar) and Banten (Banten) are all clustered in close proximity to each other on the western side of the island, with the lowest COVID-19 fatality rates in the country and some of the country’s highest private healthcare utilisation rates. For example, a 2009 USAID report estimated that West Java had 22 public hospitals compared with 120 private hospitals (Chee et al., Citation2009, p. 17). In contrast, Central Java (Jateng) and East Java (Jatim) are often plagued by capacity issues present elsewhere in the country but have not seen a commensurate increase in puskesmas as provinces off Java despite a pressing need for such increases. In contrast to their predominantly urbanised western Java provincial counterparts, private health facilities in these two provinces are less common and predominantly concentrated in cities, despite their geography covering large rural areas.
In contrast, tells a very different story in the Philippines, with less evidence of a relationship between community health facility and COVID-19 fatality rates. If anything, the correlation is weak and slightly positive, with much higher values on the x-axis. It is also worth noting that when comparing the two cases, the Philippines has a much larger number of provinces, HUCs and ICCs with fatality rates below two, and a much higher rate of local clinics and health units to provide care at the barangay level. One way to interpret the Philippines data is that the much larger proportion of provinces with fatality rates below one indicates better overall responsiveness and less variance within the system more generally. More specifically, a slightly positive slope also shows one of the costs of coordination: the need and desire to coordinate among a much larger number of care units may inevitably be challenged by the difficulty in carrying out coordination as the number of facilities increases. Given the complex geography of the country, the Philippines is a place where even the best-intended plans for coordination may stumble or fall a bit short in efforts to reduce the impact of crisis across so many healthcare clinics. Taken together, these two figures present a very clear divergence in health system access and preparedness to tackle COVID-19.
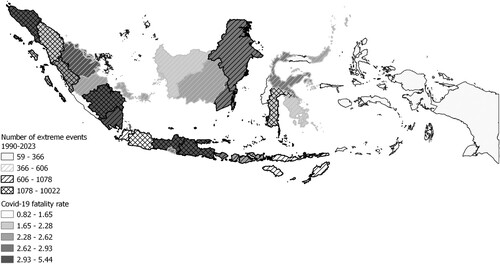
highlights a few key outliers in the Indonesian case that bear additional attention on the role of coordination. Provinces that have much higher fatality rates than their puskesmas rates would predict include Aceh, Lampung and Central and East Java. Three of these provinces share another similarity: they are three of the top four provinces ranked by the number of extreme climate and weather events tracked by Indonesia’s National Disaster Management Agency (BNPB) since 1990. In the map in , darker shading indicates higher COVID-19 fatality rates while darker single hashed lines and cross hashed lines indicate higher numbers of extreme events in the prior 30 years in the different Indonesian provinces. As the figure shows, the highest COVID-19 fatality rates are often found in provinces with the highest levels of extreme events. This suggests that the ability of such provinces to prepare for and respond to the pandemic was more limited, perhaps as a result of routinely being the location of extreme events that incur high human and economic costs, such as large numbers of fatalities, scores of displaced individuals and infrastructural damages. These are also places where efforts to build regional resilience are highly unique and specialised in response to particular event responses, which may reduce incentives to participate in or be prepared to engage in coordination with the rest of the provinces.
Figure 6. Provincial COVID fatality rate and extreme events from 1990–2023.
Sources: Indonesian National Disaster Management Agency; Indonesian Ministry of Health.
5. WIDER REGIONAL POLICY IMPLICATIONS
Lessons for other regions are possible given that provinces in Indonesia and the Philippines represent paradigmatic cases of regions, especially in LMIC contexts: these regions hold relatively average levels of authority in international comparative measures and for the types and scope of policies they control, and they exist within unitary systems that have devolved important aspects of governing to the regions (Shair-Rosenfield et al., Citation2021). This analysis of relatively ‘typical’ regions shows the need to consider coordination efforts within such decentralised systems. One particular implication for other regions, particularly in the context of public health policy in LMICs, is that the building of additional health clinics in underserved communities may serve an important role in care access. Even if it is not a panacea for resolving unequal health outcomes among regions, and capacity and resource gaps may constrain staffing and effectiveness of care provision at the regional level, adding clinic locations in the regions where they are most needed should minimise disparities between regional health outcomes.
A second implication emerges from the map in showing where extreme event activity overlaps with higher COVID fatality rates. Regions that frequently experience extreme weather events – torrential rain and ensuing mudslides, earthquakes, hurricanes or flooding – often receive extra resources from national governments and international aid programmes to build and reinforce institutions that can facilitate local resilience.Footnote9 These resources are essential to helping regional populations prepare for and recover from disasters, but may be simultaneously insufficient to empower response and resilience to other forms of crisis. When (re)designing institutions of crisis response and resilience, one lesson for regions (and the national governments and international assistance programmes that support them) is to prioritise and consider how to integrate coordination mechanisms that more generally facilitate working with other regional and national bodies.
6. CONCLUSION
The COVID-19 pandemic posed serious challenges for governments around the world, and even where the demographic consequences of COVID-19 have been limited, it has taken immense governmental response and restrictions to accomplish the feat.Footnote10 This analysis shows a part of the story leading to within-country divergence in how well governments responded to the pandemic. Both Indonesia and the Philippines, fairly decentralised and modestly coordinated, demonstrate similar overall responses to the pandemic. Yet, their ability to avoid peaks in case and death counts has varied over time and in response to different challenges. In particular, the Philippines weathered the Delta storm with greater resilience and its peak in case count did not manifest in the same peak in the death count as occurred in neighbouring Indonesia. Some of this resulted from failures in Indonesia at a time when a fast and coordinated response to Delta – a more deadly variant that caused greater risk of serious complications – was needed.
Although scholars have called for greater attention to the importance of coordination to better prepare countries to deal with emergency situations (c.f., Comfort et al., Citation2020), many countries still have limited channels through which such coordination can take place among regions or between national and regional governments. While this analysis shows that coordination can play a role in mitigating the impact of extreme events, there are limitations to what can be claimed using a single paired country-level comparison. In particular, this comparative analysis does not address how factors such as regional capacity, ongoing training and accreditation programmes, or region-specific disaster resilience efforts affect how receptive different regions are to coordination efforts during crises and disasters. For example, are regions with high capacity in emergency response more or less receptive to coordination efforts than low-capacity counterparts? The Indonesian case, notably on Java, notionally suggests that high-capacity regions may not be especially receptive to coordination efforts where they are expected to bolster low-capacity outcomes. Alternatively, resistance to coordination may be lower when routine healthcare training and accreditation activities are available, but there is regional variation in the degree to which local providers undertake such opportunities. Finally, do unique efforts to increase regional resilience in response to localised crises undermine broader acceptance of or engagement with general coordination efforts? Future research could adopt a similar paired comparative approach, comparing pairs or groups of regions within countries, to examine how variation in regional capacity, training and accreditation activities, and regionally-tailored emergency response programmes shape responses to and support for broader coordination efforts.
Finally, the focus here has been on how coordination can mitigate the potential negative effects of decentralisation in emergency management situations in LMICs. Yet, greater efforts to coordinate may be endogenous to decentralisation, especially if policymakers recognise the relative importance of coordination in responding to crises. Previous work has shown that decentralisation can improve cooperation among health policy stakeholders by encouraging the development of relationships and strengthening networks through which trust-building and a sense of shared purpose and goals among relevant elites and service providers can occur (Molina-Garzón et al., Citation2022; Zarychta, Citation2020). However, the ability to convince stakeholders of the value of coordination may differ during crisis situations because policymakers have less time to seriously consider the value in coordinated efforts or collaboratively build trust. While this analysis focuses on a short-term crisis response when decentralised institutional authority in Indonesia and the Philippines was static, future research should focus on whether aspects of the relationship between decentralisation and coordination in these cases develops specifically in response to challenges raised by COVID-19. In particular, scholars should continue to examine the relationship between post-pandemic evolutions in region-level public health infrastructure, institutions and capacity building in Indonesian and Philippines provinces and changes in regional crisis and health coordination and outcomes.
ACKNOWLEDGEMENTS
I would like to thank the special issue editors, the associate editor and three reviewers for their insightful comments and suggestions, as well as very helpful feedback from the organisers and participants at the 5th DERNET International Conference titled ‘Decentralization and the Governance of Extreme Events', all of which greatly contributed to improvements to the manuscript. All remaining errors are my own.
DISCLOSURE STATEMENT
No potential conflict of interest was reported by the author.
Notes
1. The exception tends to be the US, where state sovereignty is identified as a distinct barrier to emergency response (c.f., Haffajee & Mello, Citation2020).
2. Alternatively, failures at monitoring, credibility and consultation can degrade the ability of actors to successfully complete tasks at various stages of the policy making and execution process (c.f., Ricks & Donner, Citation2021).
3. Some Southeast Asia examples include: https://www.undp.org/indonesia/blog/infographic-petra; https://www.fao.org/faolex/results/details/en/c/LEX-FAOC168037/; https://unhabitat.org.ph/shield/; https://asean.org/our-communities/asean-socio-cultural-community/disaster-management-humanitarian-assistance/.
4. Political factors have often complicated disbursement of these resources, but without affecting the specific amounts of the IRA transfers (Eaton, Citation2001; Shair-Rosenfield, Citation2016).
5. Some of this figure may be attributed to the fact that then-President Duterte’s war on drugs, which has been accused of tens of thousands of extrajudicial deaths in recent years, likely declined as the pandemic curbed daily social interactions and movement of people.
8. Both of these subnational health facility data sources are high quality and comprehensive, and are regularly used by health economists, public policy scholars and political scientists both within and outside each country.
9. See note 3 for Southeast Asian examples.
10. Taiwan and New Zealand, with their impressively low case and death rates, achieved their successes by implementing some of the world’s most severe isolation and quarantine policies.
REFERENCES
- An, B. Y., & Tang, S.-Y. (2020). Lessons from COVID-19 responses in east Asia: Institutional infrastructure and enduring policy instruments. The American Review of Public Administration, 50(6-7), 790–800. https://doi.org/10.1177/0275074020943707
- Arias-Yurisch, K., Retamal-Soto, K., & Ramos-Fuenzalida, C. (Forthcoming). The prevalence of a bonding strategy in COVID-19 response networks: Explaining intermunicipal partnering in the Santiago metropolitan region, Chile. Regional Studies, https://doi.org/10.1080/00343404.2022.2141465
- Asmorowati, S., Schubert, V., & Ningrum, A. P. (2022). Policy capacity, local autonomy, and human agency: Tensions in the intergovernmental coordination in Indonesia’s social welfare response amid the COVID-19 pandemic. Journal of Asian Public Policy, 15(2), 213–227. https://doi.org/10.1080/17516234.2020.1869142
- Atkinson, J., Hicken, A., & Ravanilla, N. (2015). Pork & typhoons: The influence of political connections on disaster response. In R. Mendoza, & E. Beja Jr (Eds.), Building inclusive democracies in ASEAN (pp. 74–96). Anvil.
- Bailey, D., Crescenzi, R., Roller, E., Anguelovski, I., Datta, A., & Harrison, J. (2021). Regions in COVID-19 recovery. Regional Studies, 55(12), 1955–1965. https://doi.org/10.1080/00343404.2021.2003768
- Bardhan, P., & Mookherjee, D. (1998). Expenditure decentralization and the delivery of public services in developing countries. In Working paper C98-104. Center for International Development Economics Research.
- Berta, P., Vinciotti, V., & Moscone, F. (2022). The association between hospital cooperation and the quality of healthcare. Regional Studies, 56(11), 1858–1873. https://doi.org/10.1080/00343404.2021.2009792
- Besley, T., & Coate, S. (2003). Centralized versus decentralized provision of local public goods: A political economy approach. Journal of Public Economics, 87(12), 2611–2637. https://doi.org/10.1016/S0047-2727(02)00141-X
- Birn, A.-E., Zimmerman, S., & Garfield, R. (2000). To decentralize or not to decentralize, is that the question? Nicaraguan health policy under structural adjustment in the 1990s. International Journal of Health Services, 30(1), 111–128. https://doi.org/10.2190/C6TB-B16Y-60HV-M3QW
- Blair, H. (2000). Participation and accountability at the periphery: Democratic local government in six countries. World Development, 28(1), 21–39. https://doi.org/10.1016/S0305-750X(99)00109-6
- Bossert, T. J., & Beauvais, J. C. (2002). Decentralization of health systems in Ghana, Zambia, Uganda, and the Philippines: A comparative analysis of decision space. Health Policy and Planning, 17(1), 14–31. https://doi.org/10.1093/heapol/17.1.14
- Bourdin, S., & Levratto, N. (Forthcoming). The spatial footprint of COVID-19 and local policy answers. Regional Studies, https://doi.org/10.1080/00343404.2023.2242411
- Chee, G., Borowitz, M., & Barraclough, A. (2009). Private sector healthcare in Indonesia. In Report prepared for the US agency for international development. Health Systems 20/20 Project, Abt Associates Inc.
- Comfort, L. K. (2007). Crisis management in hindsight: Cognition, communication, coordination, and control. Public Administration Review, 67(s1), 189–197. https://doi.org/10.1111/j.1540-6210.2007.00827.x
- Comfort, L. K., Kapucu, N., Ko, K., Menoni, S., & Siciliano, M. (2020). Crisis decision-making on a global scale: Transition from cognition to collective action under threat of COVID-19. Public Administration Review, 80(4), 616–622. https://doi.org/10.1111/puar.13252
- Comfort, L. K., Ko, K., & Zagorecki, A. (2004). Coordination in rapidly evolving disaster response systems: The role of information. American Behavioral Scientist, 48(3), 295–313. https://doi.org/10.1177/0002764204268987
- Dias-Cayeros, A., Magaloni, B., & Ruiz-Euler, A. (2014). Traditional governance, citizen engagement, and local public goods: Evidence from Mexico. World Development, 53, 80–93. https://doi.org/10.1016/j.worlddev.2013.01.008
- Eaton, K. (2001). Political obstacles to decentralization: Evidence from Argentina and the Philippines. Development and Change, 32(1), 101–127. https://doi.org/10.1111/1467-7660.00198
- Eaton, K., & Shair-Rosenfield, S. (Forthcoming). Peace at what cost? Territorial autonomy as a response to internal armed conflict in Indonesia and the Philippines. Peacebuilding, https://doi.org/10.1080/21647259.2023.2251284
- Faguet, J.-P. (2004). Does decentralization increase responsiveness to local needs? Evidence from Bolivia. Journal of Public Economics, 88(3-4), 867–893. https://doi.org/10.1016/S0047-2727(02)00185-8
- Faguet, J.-P. (2014). Decentralization and governance. World Development, 53, 2–13. https://doi.org/10.1016/j.worlddev.2013.01.002
- Fernandez, G., & Ahmed, I. (2019). ‘Build back better’ approach to disaster recovery: Research trends since 2006. Progress in Disaster Science, 1, 100003. https://doi.org/10.1016/j.pdisas.2019.100003
- Fiszbein, A. (1997). The emergence of local capacity: Lessons from Colombia. World Development, 25(7), 1029–1043. https://doi.org/10.1016/S0305-750X(97)00020-X
- Gillespie, A. M., Obregon, R., El Asawi, R., Richey, C., Manoncourt, E., Joshi, K., Naqvi, S., Pouye, A., Safi, N., Chitnis, K., & Quereshi, S. (2016). Social mobilization and community engagement central to the Ebola response in West Africa: Lessons for future public health emergencies. Global Health: Science and Practice, 4(4), 626–646. https://doi.org/10.9745/GHSP-D-16-00226
- Gonçalvez, S. (2014). The effects of participatory budgeting on municipal expenditures and infant mortality in Brazil. World Development, 53, 94–110. https://doi.org/10.1016/j.worlddev.2013.01.009
- Guaitioli, G., & Pancrazi, R. (2021). COVID-19: Regional policies and local infection risk: Evidence from Italy with a modelling study. The Lancet Regional Health-Europe, 8. https://doi.org/10.1016/j.lanepe.2021.100169
- Haffajee, R. L., & Mello, M. M. (2020). Thinking globally, acting locally: The U.S. response to COVID-19. The New England Journal of Medicine, 382(22), e75. https://doi.org/10.1056/NEJMp2006740
- Hicken, A., Kollman, K., & Simmons, J. W. (2016). Party system nationalization and the provision of public health services. Political Science Research and Methods, 4(3), 573–594. https://doi.org/10.1017/psrm.2015.41
- Hutchcroft, P. (2012). Re-slicing the pie of patronage: The politics of the internal revenue allotment in the Philippines, 1991-2010. The Philippine Review of Economics, 49(1), 109–148.
- Khaleghian, P. (2004). Decentralization and public services: The case of immunization. Social Science & Medicine, 59(1), 163–183. https://doi.org/10.1016/j.socscimed.2003.10.013
- La Vincente, S., Aldaba, B., Firth, S., Kraft, A., Jimenez-Soto, E., & Clark, A. (2013). Supporting local planning and budgeting for maternal, neonatal and child health in the Philippines. Health Research Policy and Systems, 11(1), 3. https://doi.org/10.1186/1478-4505-11-3
- Lakshminarayanan, R. (2003). Decentralisation and its implications for reproductive health: The Philippines experience. Reproductive Health Matters, 11(21), 96–107. https://doi.org/10.1016/S0968-8080(03)02168-2
- Lele, G. (2023). Concurrency as crisis decision-making governance: Lessons from Indonesia's response to the COVID-19 pandemic. Regional & Federal Studies, 307–332. https://doi.org/10.1080/13597566.2021.1960513
- Maharani, A., & Tampubolon, G. (2015). Has decentralisation affected child immunisation status in Indonesia? Global Health Action, 7(1), 24913. https://doi.org/10.3402/gha.v7.24913
- McCann, P., Ortega-Arguilés, R., & Yuan, P.-Y. (2022). The COVID-19 shock in European regions. Regional Studies, 56(7), 1142–1160. https://doi.org/10.1080/00343404.2021.1983164
- Molina-Garzón, A., Grillos, T., Zarychta, A., & Andersson, K. P. (2020). Decentralization can increase cooperation among public officials. American Journal of Political Science, 66(3), 554–569. https://doi.org/10.1111/ajps.12606
- Namazzi, G., Okuga, M., Tetui, M., Muhumuza Kananura, R., Kakaire, A., Namutamba, S., Mutebi, A., Namusoke Kiwanuka, S., Eirapa-Kiracho, E., & Waiswa, P. (2017). Working with community health workers to improve maternal and newborn health outcomes: implementation and scale-up lessons from eastern Uganda. Global Health Action, 10(sup4), 1345495. https://doi.org/10.1080/16549716.2017.1345495
- Palomino, J. C., Rodriguez, J. G., & Sebastian, R. (2023). The COVID-19 shock on the labour market: Poverty and inequality effects across Spanish regions. Regional Studies, 57(5), 814–828. https://doi.org/10.1080/00343404.2022.2110227
- Pandey, A., & Saxena, N. K. (2022). Effectiveness of government policies in controlling COVID-19 in India. International Journal of Health Services, 52(1), 30–37. https://doi.org/10.1177/0020731420983749
- Perez, J. A. (1998). Health worker benefits in a period of broad civil service reform: the Philippine experience. Unpublished manuscript available at: https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=6c7932cdd8912699290e4224bbcc77040c1f0585.
- Putra, D. I., & Matsuyuki, M. (2019). Disaster management following decentralization in Indonesia: Regulation, institutional establishment, planning, and budgeting. Journal of Disaster Research, 14(1), 173–187. https://doi.org/10.20965/jdr.2019.p0173
- Regmi, K., Naidoo, J., Pilkington, P. A., & Greer, A. (2010). Decentralization and district health services in Nepal: Understanding the views of service users and service providers. Journal of Public Health, 32(3), 406–417. https://doi.org/10.1093/pubmed/fdp116
- Ricks, J. I., & Doner, R. F. (2021). Getting institutions right: Matching institutional capacities to development tasks. World Development, 139, 105334. https://doi.org/10.1016/j.worlddev.2020.105334
- Ritchie, H., Mathieu, E., Rodés-Guirao, L., Appel, C., Giattino, C., Ortiz-Ospina, E., Hasell, J., Macdonald, B., Beltekian, D., & Roser, M. (2020). Coronavirus Pandemic (COVID-19). Published online at OurWorldInData.org. https://ourworldindata.org/coronavirus.
- Schlegelmilch, J., Petkova, E., & Redlener, I. (2015). Disaster prepared: How federal funding in the USA supports health system and public health readiness. Journal of Business Continuity and Emergency Planning, 9, 112–118.
- Shair-Rosenfield, S. (2016). The causes and effects of the local government code in the Philippines: Locked in a status quo of weakly decentralized authority? Journal of Southeast Asian Economics, 33(2), 157–171. https://doi.org/10.1355/ae33-2c
- Shair-Rosenfield, S., Marks, G., & Hooghe, L. (2014). A comparative measure of decentralization for Southeast Asia. Journal of East Asian Studies, 14(1), 85–107. https://doi.org/10.1017/S1598240800009590
- Shair-Rosenfield, S., Schakel, A. H., Niedzwiecki, S., Marks, G., Hooghe, L., & Chapman-Osterkatz, S. (2021). Language difference and regional authority. Regional & Federal Studies, 31(1), 73–97. https://doi.org/10.1080/13597566.2020.1831476
- Shair-Rosenfield, S., & Wood, R. M. (2017). Governing well after war: How improving female representation prolongs post-conflict peace. The Journal of Politics, 79(3), 995–1009. https://doi.org/10.1086/691056
- Shringare, A., & Fernandes, S. (2020). COVID-19 pandemic in India points to need for a decentralized response. State and Local Government Review, 52(3), 195–199. https://doi.org/10.1177/0160323X20984524
- Wong, A. K., & Balzer, L. B. (2022). State-level masking mandates and COVID-19 outcomes in the United States: A demonstration of the causal roadmap. Epidemiology, 33(2), 228–236. https://doi.org/10.1097/EDE.0000000000001453
- Zarychta, A. (2020). Making social services work better for the poor: Evidence from a natural experiment with health sector decentralization in Honduras. World Development, 133, 104996. https://doi.org/10.1016/j.worlddev.2020.104996
- Zhang, X.-X., Jin, Y.-Z., Lu, Y.-H., Huang, L.-L., Wu, C.-X., Lv, S., Chen, Z., Xiang, H., & Zhuo, X.-N. (2023). Infectious disease control: From health security strengthening to health systems improvement at global level. Global Health Research and Policy, 8(1), 38. https://doi.org/10.1186/s41256-023-00319-w
