Abstract
Hip fractures in elderly carry a high mortality. Our objective was to test the hypothesis that plasma lactate concentration at hospital admission can be used to identify patients with a high risk for poor outcome. Hip fracture patients admitted to a university hospital in Sweden from January 2011 to August 2014 in whom a venous lactate was obtained at admission were included in this prospective observational study. Primary outcome measure was 30-d mortality and secondary outcome measure was a composite outcome of 30-d mortality and postoperative complications. Lactate concentration was evaluated as a continuous predictor using logistic regression, crude and adjusted for age, gender and American Society of Anesthesiology Physical Status (ASA PS) score. Discrimination was evaluated using receiver operating characteristics (ROC) analysis. Totally, 690 patients were included. Median age was 84 years (interquartile range [IQR] 77–90). At 30-d follow-up, mortality was 7.2%, and 45% of the patients had suffered the composite outcome. Median lactate level was 1.3 mmol/L (IQR 1.0–1.8 mmol/L). The odds ratio (OR) by each 1.0 mmol/L increase in the lactate concentration for 30-d mortality was 1.13 (95% CI 0.77–1.68) while for the composite outcome it was 1.06 (95% CI 0.85–1.3). Similar results were obtained after adjustment for age, sex and ASA PS classification for both outcomes. Area under the ROC curve for lactate as a predictor of 30-d mortality was 0.51 (95% CI 0.45–0.57). In our cohort, plasma lactate at admission does not appear to be a useful biomarker to identify high-risk patients after hip fracture.
| Abbreviations | ||
| ASAPS | = | American Society of Anesthesiologists Physical Status Classification |
| BP | = | Blood pressure |
| BPM | = | Beats per minute |
| CI | = | Confidence interval |
| COPD | = | Chronic Obstructive Pulmonary Disease |
| IQR | = | Interquartile Range |
| ISS | = | Injury Severity Score |
| LR | = | Likelihood Ratio |
| N | = | Number |
| OR | = | Odds Ratio |
| ROC | = | Receiver Operating Characteristics |
Background
Hip fracture in the elderly is a serious acute condition with 30-d mortality of 7–10% in Western Europe and in North America [Citation1–3]. Patients commonly suffer from multiple comorbidities resulting in a limited physiologic reserve, which is likely to contribute to the high mortality and morbidity in spite of the low severity of the trauma [Citation4,Citation5]. Early recognition of high-risk patients has the potential to improve outcome and several clinical scoring systems based on comorbidities and demographics have been described for this purpose [Citation6–9]. Surprisingly, while plasma concentrations of several biomarkers such as creatinine and haemoglobin have been shown to be associated with poor outcome and improve accuracy of scoring systems, less is known about lactate as a biomarker in this setting [Citation6,Citation10–13].
In trauma, plasma lactate concentration most commonly increases when oxygen delivery to tissues is less than demand, and although lactate may increase through other mechanisms an increase in lactate is frequently regarded as a biomarker of inadequate organ perfusion [Citation14]. Given that inadequate tissue oxygenation is suggested to be a major cause of poor outcome and complications in acute illness, it is not surprising that many studies have suggested early elevation of lactate concentrations in plasma to predict poor outcome in different settings including trauma, surgery and sepsis [Citation15–22]. Treatment strategies with the objective to normalize an increased lactate have also been suggested to improve outcome in both trauma and sepsis [Citation23,Citation24]. Based on the hypothesis that lactate may identify patients with limited cardiovascular reserve amenable to therapeutic interventions, venous lactate could be a potential biomarker also in hip fracture patients. Some support for this hypothesis was found in recent observational studies on cohort of hip fracture patients from the UK suggesting that elevated lactate concentrations are associated with increased mortality [Citation22,Citation25]. However, to our knowledge, the external validity of these findings have not been investigated. Moreover, no data are available concerning the accuracy of lactate to predict complications in hip fracture patients.
Based on these considerations, this study was designed to evaluate if venous lactate concentrations at arrival to hospital can predict mortality and morbidity in a cohort of hip fracture patients. Data from a prospective observational single centre study were used and 30-d mortality was the primary outcome measure and a composite of 30-d mortality and complications was the secondary outcome measure.
Methods
Study design
This was a prospective observational cohort study for hip fracture patients admitted to Skåne University Hospital, Lund, Sweden. The recruitment started 31 January 2011 and ended on 30 August 2014. Patients were followed for 1 year after inclusion. The overall objective of the study was to assess accuracy of several biomarkers to predict outcome. The manuscript was prepared according to the STROBE guidelines for reporting of observational studies [Citation26]. Registered at Clinicaltrials.gov with identification number NCT01280253 on 18 January 2011.
Inclusion and exclusion criteria
Ambulance and emergency department staff performed patient screening. Inclusion criteria were out of hospital cervical, trochanteric or subtrochanteric fracture of the neck of the femur and blood sampling within 3 h from first contact with health care providers. Exclusion criteria were not informed consent, non-operative management, pathological fracture, multi-trauma, patients who were already admitted when suffering their hip fracture and if follow-up was not possible within the Swedish National Quality Register for hip fracture patients. Eligible patients in which plasma lactate was not measured were considered as screening failures.
Lactate analysis
A venous blood gas sample was drawn either at the emergency department or at the orthopaedic ward within 3 h of arrival to the hospital. Lactate was analysed within 15 min after sampling using an amperometric method on a blood gas analyser (Radiometers ABL800 Flex, Copenhagen, Denmark). Calibration of the analyser was performed according to the manufacturer’s instructions and the coefficient of variation for the analysis is 1.3–2.1% according to internal quality control at the laboratory.
Outcome measures
Primary outcome measure was 30-d mortality and secondary outcome measure was a composite outcome of 30-d mortality and postoperative complications (cardiovascular, respiratory, wound related or renal complications, infections and bleeding). Complications were defined as previously described for the POSSUM score for hip fracture patients, which is an audit system for quality control of surgical outcome [Citation27]. Complications during the first 30-d of admission were identified by investigators through examination of the patients’ medical records. For definition of complications please see Supplementary material S1. Data from the ambulance and the hospital medical records regarding vital parameters, comorbidities, prescribed medications, administered fluids, blood transfusions and perioperative data were also collected. The accuracy of the data in the database was checked against source data by the external monitors in a sample of 31 patients and the fraction of wrong entries was found to be <0.1%. Outcome data for eligible patients not included at Lund University hospital during the study period and on a national level was extracted from the Swedish National Quality Register for Patients with Hip Fractures and compared to the patient cohort.
Statistics
The number of patients in which lactate was sampled as described above determined the sample size. The predictive ability of the lactate level with respect to 30-d mortality or a composite end-point including 30-d mortality and complications was evaluated using a logistic regression model. Both a crude model and a model adjusted for age, sex and American Society of Anesthesiology (ASA) status was used to estimate the odds ratio (OR) with 95% confidence intervals (95% CI). The area under the receiver operating characteristics (ROC) curve, sensitivity, specificity and likelihood ratios (LRs) (positive and negative) were also calculated to assess discrimination and accuracy. Lactate was primarily evaluated using the previously suggested cut-off of 2.0 mmol/L [Citation28] and secondarily by using a new cut-off based on maximizing the Youden index for the present cohort. The discriminating ability of lactate for 30-d mortality was evaluated with equal weight given to sensitivity and specificity [Citation29]. The performance of the new cut-off was assessed using bootstrapping. In each replication, a sample was drawn with replacement from the whole study sample and used to derive the cut-off. Further, the performance of the cut-off was assessed using the subjects not included in this replication sample. The procedure was repeated 1000 times and bootstrap bias-corrected 95% CIs were calculated. The final cut-off was calculated based on all the included subjects [Citation30]. A Kaplan–Meier plot was used to visualize the survival during the first 30 d after admission in patients with a lactate level below or above the 2.0 mmol/L threshold and survival was analysed using a Log Rank test. Stata™ (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP) and The R Project (R Core Team. 2013. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria) were used for analyses.
Results
Demographics
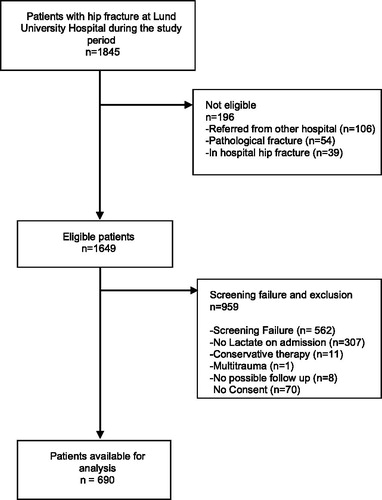
A total of 1845 patients were admitted with a hip fracture diagnosis at Lund University Hospital during the study period and 1649 were eligible for inclusion (). Of those, 690 patients (42.1%) had lactate measured at arrival and were included in the study. Patient demographics, vital signs and laboratory data at arrival are shown in . Median age was 84.3 years (interquartile range [IQR] 77.3–90.2). About 94% of the patients were operated within 36 h of arrival to the hospital. Spinal analgesia was the main anaesthetic in 65% of the patients. The 30-d mortality was 7.2% (n = 50) and 45% (n = 311) of the patients had suffered complications at 30 d (). In an attempt to assess if our sample was a representative sample of eligible patients presenting at Lund University Hospital and on a national level, demographic data were extracted from the Swedish National Quality Register for Hip Fracture Patients during the study period. The demographic data for eligible patients admitted to Lund University Hospital that were not included in our cohort as well as demographic data for patients fulfilling inclusion criteria on a national level were found to be very similar to those in the included cohort ().
Table 1. Demographics, co-morbidities, laboratory values and vital parameters on admission, choice of anaesthesia, fluid administration and time to operation.
Table 2. Outcomes presented by baseline lactate level.
Table 3. Demographics of the study cohort compared to study site and nationally during the study period.
Lactate as a predictor of outcome
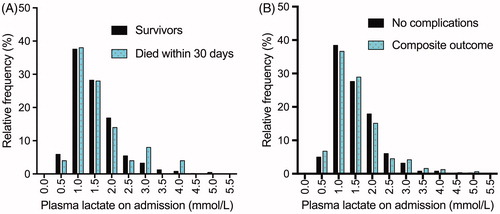
Median lactate level was 1.3 mmol/L (range 0.4–5.1 mmol/L, IQR 1.0–1.8 mmol/L) and distribution of lactate concentrations in 30-d survivors and non-survivors, respectively, are shown in . The OR by each 1.0 mmol/L increase in the lactate concentration for 30-d mortality was 1.13 (95% CI 0.77–1.68) while for the composite outcome it was 1.06 (95% CI 0.85–1.3). Similar results were obtained after adjustment for age, sex and ASA physical status (PS) classification for both outcomes.
Figure 2. Histogram showing distribution of lactate concentrations for 30-d mortality (A) and the composite of 30-d mortality and complications secondary outcomes (B).
The calculated area under the ROC curve for lactate as a linear predictor 30-d mortality was 0.51 (95% CI 0.45–0.57) and for the composite outcome 0.49 (95% CI 0.47–0.53), (). A Kaplan–Meier plot of mortality the first 30 d after admission for patients with lactate <2.0 mmol/L or ≥2.0 mmol/L is presented in . No difference in mortality between the two groups was detected. Time to operation, fluid administration during the first 24 h after admission and mode of anaesthesia were similar in patients with lactate <2.0 mmol/L and ≥2.0 mmol/L, respectively (). Accuracy of lactate as predictor of poor outcome using 2.0 mmol/L as a cut-off, was poor with positive and negative LRs close to one for both 30-d mortality and the composite outcome ().
Figure 3. Kaplan–Meier survival curve of patients with lactate concentration< 2.0 mmol/L and ≥2.0 mmol/L. Log rank (Mantel-Cox) significance 0.73. Note that the Y-axis is shortened for clarification.
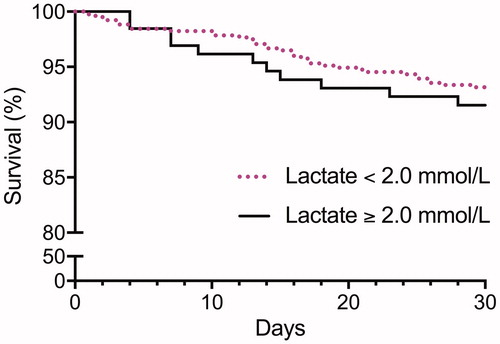
Table 4. Accuracy and predictive qualities for lactate as a predictor of 30-d mortality or a composite outcome (30-d mortality and complications).
The lactate cut-off that maximizes the Youden index for 30-d mortality in our cohort was found to be 2.2 mmol/L. Accuracy of the new cut-off was also found to be poor with positive and negative LRs close to one for both 30-d mortality and the composite outcome (). Based on previous studies, we analysed higher lactate cut-offs and a lactate cut-off of 4.0 mmol/L (n = 7 patients) had a LR + of 2.0 for mortality and 1.0 for complications [Citation31].
Discussion
No association between increased plasma lactate concentration at arrival to hospital and 30-d mortality or morbidity could be detected in this cohort of hip fracture patients.
Our results are in contrast to recent studies in which plasma lactate was reported to predict 30-d mortality in patients suffering from hip fractures [Citation22,Citation25]. The studies are of similar size and mortality, age and gender distribution in the two cohorts are almost identical to our study. However, about 15% of the patients in those studies had lactate concentrations above 3.0 mmol/L compared to 5% of our cohort. This observation could be explained by differences in prehospital and perioperative care as well as timing of blood sampling in relation to the trauma, which in turn may have influenced the predictive value of lactate.
To our knowledge this is the first study investigating the association between lactate at admission and morbidity in hip fracture patients. Complications were carefully monitored and occurred in a large portion of the patients giving the composite outcome more power to detect an association between lactate and poor outcome. The finding that plasma lactate concentration was not associated with complication rate supports the limited predictive value of early lactate increases in our cohort.
Only a small number of the studies investigating lactate as a predictor of poor outcome have focused specifically on the geriatric population. In one recent retrospective study, it was reported that a venous lactate concentration >2.5 mmol/L in trauma patients ≥65 years old was associated with a higher mortality also after correction for age, Glasgow coma scale and injury severity score (ISS) [Citation32]. Similarly, another retrospective study reported an increased mortality in normotensive trauma patients ≥55 years old with a lactate >2.5 mmol/L [Citation33]. Unfortunately accuracy was not reported in any of these studies. Several characteristics of the above-mentioned studies differ from the present one, which may explain the different results. The average age in these studies was at least 5 years lower than in the present study and a higher number of patients had elevated lactate levels.
It was recently suggested that lactate is not an independent predictor of outcome in a large cohorts of sepsis patients [Citation28,Citation34], while the combination of hypotension requiring vasopressor therapy to maintain mean blood pressure 65 mmHg or greater and having a serum lactate level greater than 2.0 mmol/L after adequate fluid resuscitation was a predictor of poor outcome. Hypotension was rare in our cohort (n = 2) and the predictive value of the combination of hypotension and lactate was not meaningful to analyse.
Taken together our results suggest that lactate is not universally useful as a screening tool to identify high-risk patients and that the predictive ability is dependent on the clinical context in which it is applied. Interestingly, a recent study suggested that a venous lactate >4.0 mmol/L at admission to the emergency ward was not associated with an increased mortality if the increase was deemed to be secondary to reasons other than tissue hypoxia [Citation31]. If applicable to our cohort, those results suggest that high lactate values may be secondary to factors other than trauma-induced hypoperfusion and consequently that factors other than tissue hypoxia are of more importance for outcome in elderly frail patients suffering from hip fractures. Such factors include age, gender, residence, ASA grade, cognitive function and mobility [Citation8].
Strengths and limitations
Strengths of our study include the prospective design and the careful characterization of the patients. Moreover, external monitoring showed that data entered in the data base reliably reflected source data.
Limitations of the study include that lactate was only available in 42% of all patients fulfilling inclusion criteria. Based on this it could be argued that our cohort represents a selected subset of patients. However, patient demographics and the outcome in our cohort is similar to that in the national registry indicating that our cohort is a representative sample both on a hospital and national level. Another limitation is that the treating clinicians were not blinded to the results of the lactate analysis and we cannot exclude that the patients with increased lactate may have received additional care with the objective to optimize oxygen delivery. If so, this could have decreased the prognostic value of lactate. However, analysing lactate is not a routine analysis for these patients in our institution and it is unlikely that it was systematically considered in the workup of these patients. This statement is supported by the finding that volumes of administered fluids did not differ between groups above or below threshold lactate level ().
Conclusions
We conclude that, in contrast to previous studies in hip fracture patients, the plasma concentration of lactate at admission in this large cohort of well-characterised elderly patients with an isolated hip fracture did not predict 30-d mortality or morbidity. Thus, plasma lactate does not appear to be universally useful as a biomarker to identify high-risk patients in this patient category.
Ethics approval and consent to participate
The study was approved by the Regional Ethical Review Board in Lund (EPN application numbers 2010/218 and 2011/506). A written consent was obtained for every participant within 72 h of admission. If consent was not obtained patients were excluded from the study.
Supplemental Material
Download PDF (77.2 KB)Acknowledgments
The following persons contributed greatly with data collection, registration and handling of blood samples: Susann Schrey, Lena Jönsson, Anne Adolfsson, Carina Lilja. We are also deeply grateful to ambulance staff of Region Skåne, emergency ward staff and the staff at the orthopaedic wards at Skåne University hospital (Lund) for recruiting patients to this study.
Disclosure statement
No potential conflict of interests was reported by the author(s).
Additional information
Funding
References
- Roberts SE, Goldacre MJ. Time trends and demography of mortality after fractured neck of femur in an English population, 1968-98: database study. BMJ. 2003;327:771–775.
- Medin E, Goude F, Melberg HO, et al. European regional differences in all-cause mortality and length of stay for patients with hip fracture. Health Econ. 2015;24:53–64.
- Physicians RCo. National hip fracture database annual report 2017. London: RCP; 2017.
- Foss NB, Kehlet H. Mortality analysis in hip fracture patients: implications for design of future outcome trials. Br J Anaesth. 2005;94:24–29.
- Bergeron E, Lavoie A, Belcaid A, et al. Should patients with isolated hip fractures be included in trauma registries? J Trauma. 2005;58:793–797.
- Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101:511–517.
- Soderqvist A, Ekstrom W, Ponzer S, et al. Prediction of mortality in elderly patients with hip fractures: a two-year prospective study of 1,944 patients. Gerontology. 2009;55:496–504.
- Smith T, Pelpola K, Ball M, et al. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014;43:464–471.
- Jonsson MH, Bentzer P, Turkiewicz A, et al. Accuracy of the physiological and operative severity score for the enumeration of mortality and morbidity score and the Nottingham risk score in hip fracture patients in Sweden - a prospective observational study. Acta Anaesthesiologica Scandinavica. 2018;62:1057–1063.
- Fisher A, Fisher L, Srikusalanukul W, et al. Usefulness of simple biomarkers at admission as independent indicators and predictors of in-hospital mortality in older hip fracture patients. Injury. 2018;49:829–840.
- Katsanos S, Mavrogenis AF, Kafkas N, et al. Cardiac biomarkers predict 1-year mortality in elderly patients undergoing hip fracture surgery. Orthopedics. 2017;40:e417–e424.
- Bjorkelund KB, Hommel A, Thorngren KG, et al. Factors at admission associated with 4 months outcome in elderly patients with hip fracture. Aana J. 2009;77:49–58.
- Gruson KI, Aharonoff GB, Egol KA, et al. The relationship between admission hemoglobin level and outcome after hip fracture. J Orthop Trauma. 2002;16:39–44.
- Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014;371:2309–2319.
- Guyette F, Suffoletto B, Castillo JL, et al. Prehospital serum lactate as a predictor of outcomes in trauma patients: a retrospective observational study. J Trauma: Injury, Infect Crit Care. 2011;70:782–786.
- Parsikia A, Bones K, Kaplan M, et al. The predictive value of initial serum lactate in trauma patients. Shock. 2014;42:199–204.
- Husain FA, Martin MJ, Mullenix PS, et al. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003;185:485–491.
- Trzeciak S, Dellinger RP, Chansky ME, et al. Serum lactate as a predictor of mortality in patients with infection. Intens Care Med. 2007;33:970–977.
- Nichol AD, Egi M, Pettila V, et al. Relative hyperlactatemia and hospital mortality in critically ill patients: a retrospective multi-centre study. Crit Care. 2010;14:R25.
- Rishu AH, Khan R, Al-Dorzi HM, et al. Even mild hyperlactatemia is associated with increased mortality in critically ill patients. Crit Care. 2013;17:R197
- Varis E, Pettila V, Poukkanen M, et al. Evolution of blood lactate and 90-day mortality in septic shock. A post hoc analysis of the FINNAKI study. Shock. 2017;47:574–581.
- Venkatesan M, Smith RP, Balasubramanian S, et al. Serum lactate as a marker of mortality in patients with hip fracture: a prospective study. Injury. 2015;46:2201–2205.
- Jansen TC, van Bommel J, Schoonderbeek FJ, et al. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182:752–761.
- Blow O, Magliore L, Claridge JA, et al. The golden hour and the silver day: detection and correction of occult hypoperfusion within 24 hours improves outcome from major trauma. J Trauma. 1999;47:964–969.
- Uzoigwe CE, Venkatesan M, Smith R, et al. Serum lactate is a prognostic indicator in patients with hip fracture. Hip Int. 2012;22:580–584.
- Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Int J Surg. 2014;12:1500–1524.
- Wright DM, Blanckley S, Stewart GJ, et al. The use of orthopaedic POSSUM as an audit tool for fractured neck of femur. Injury. 2008;39:430–435.
- Singer M, Deutschman CS, Seymour CW, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA. 2016;315:801–810.
- Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35.
- Max Kuhn KJ. Applied predictive modeling. New York (NY): Springer; 2013. p. 600.
- van den Nouland DP, Brouwers MC, Stassen PM. Prognostic value of plasma lactate levels in a retrospective cohort presenting at a university hospital emergency department. BMJ Open. 2017;7:e011450.
- Salottolo KM, Mains CW, Offner PJ, et al. A retrospective analysis of geriatric trauma patients: venous lactate is a better predictor of mortality than traditional vital signs. Scand J Trauma Resusc Emerg Med. 2013;21:7.
- Neville AL, Nemtsev D, Manasrah R, et al. Mortality risk stratification in elderly trauma patients based on initial arterial lactate and base deficit levels. Am Surg. 2011;77:1337–1341.
- Shankar-Hari M, Phillips GS, Levy ML, et al. Developing a new definition and assessing new clinical criteria for septic shock: for the third international consensus definitions for sepsis and septic shock. (Sepsis-3). JAMA. 2016;315:775–787.