Abstract
This study aimed to evaluate the value of cystatin C (Cys C) in predicting the perioperative and long-term prognosis of renal transplantation (RT). The clinical data of 198 RT recipients were collected. Blood samples were obtained daily until 7 d after transplantation and then discharge day to determine the serum levels of Cys C. The receiver-operating characteristic (ROC) analysis and the area under the curve (AUC) were used to determine the diagnostic accuracy of Cys C for delayed graft function (DGF). The presence of shrunken pore syndrome (SPS) with a cystatin C-based estimate of glomerular filtration rate less than 70% of a creatinine-based estimate, was also evaluated as a prognostic factor for the development of DGF. The serum Cys C levels of patients with DGF were higher than those of the non-DGF group. Cys C showed a higher AUC (0.928) in the ROC analysis than did sCr (0.862). Compared to the non-SPS group, there were more patients diagnosed with SPS in the DGF group (p < .05). The follow-up data showed that patients diagnosed with SPS had higher levels of sCr and Cys C compared to other patients, suggesting a poor long-term prognosis. Our findings suggest that Cys C is a sensitive indicator of renal function during the perioperative period. Cys C at a concentration of 4.9 mg/L had the highest sum of sensitivity and specificity for prediction of DGF, with a sensitivity of 0.889 and a specificity of 0.8. SPS is associated with the development of DGF and the poor long-term prognosis of RT.
Introduction
Kidney allotransplantation is the optimal treatment strategy for end-stage renal disease. With the expansion of Donation after Circulatory Death (DCD), the number of renal transplantation (RT) recipients in China has been increasing continuously in recent years [Citation1]. Perioperative management is the key to successful transplantation. Delayed graft function (DGF) is a common complication after allograft RT, usually caused by ischemic reperfusion injury and acute rejection of the transplanted kidney [Citation2]. Patients with DGF require hemodialysis within one week after the operation. The occurrence of DGF has been shown to reduce the survival of the allograft, increase the incidence of acute rejection, and affect the postoperative survival of the recipient [Citation3]. Therefore, early diagnosis and timely intervention of DGF are important for a better prognosis of RT. However, no indicator is currently available for precise evaluation of renal status during the perioperative period. The use of serum creatinine (sCr) levels to indicate renal function has some limitations because sCr is affected not only by renal function but also by age and other individual differences [Citation4]. The levels of sCr increase only when the glomerular filtration rate (GFR) decreases by more than 50% [Citation5].
Cystatin C (Cys C) is superior to sCr as a marker of GFR [Citation6]. The kidney is the only organ where Cys C is degraded, which effectively reduces the effects of other factors on serum Cys C levels [Citation7]. Cys C is more reliable than sCr in the assessment of renal function and can be used as a sensitive marker for the early diagnosis of renal injury [Citation8]. Shrunken pore syndrome (SPS) refers to impaired glomerular filtration of proteins between 12 and 29 kDa [Citation9]. Patients diagnosed with SPS showed increased 3- and 5-year mortality rates [Citation10]. However, the prognosis of patients with SPS following RT has not been reported.
Our study aimed to investigate whether serum Cys C levels could be used to assess DGF during the perioperative period and to predict the long-term prognosis of RT recipients.
Methods
This retrospective study was approved by the medical ethics committee of the Third Affiliated Hospital of Soochow University, Suzhou, China. The Helsinki Declaration was strictly followed. The clinical data of patients were collected from January 2019 to December 2020. All patients were diagnosed with end-stage renal disease (ESRD) and received RT for the first time. The inclusion criteria were as follows: (1) the donor and the recipient had the same ABO blood type; (2) patients were routinely treated with Tacrolimus (FK506)/mycophenolate mofetil (MMF)/glucocorticoid; (3) patients were aged between 18 and 60 years. Finally, 198 patients were included in the analysis, with a mean age of 42 years.
Laboratory examinations
Blood samples were collected from all patients the morning before surgery, within 3–6 h after surgery, daily during the 1st week after surgery, and then discharge day. The serum Cys C levels were measured by a laboratory technician blinded to patients’ information. The latex-enhanced immunoturbidimetric method and the Cystatin C Kit (Meikang Biotech, China) were used. The serum levels of creatinine were measured by enzymatic creatinine-2 reagents (Siemens Healthcare Diagnostics Inc., Germany) using the enzyme method.
Definitions of DGF and SPS
DGF is defined as the need for dialysis within the first week after RT due to poor graft recovery [Citation11]. Patients with hypervolemia and hyperkalemia were excluded. Patients who required no dialysis within the first week after RT were categorized into the non-DGF group [Citation2,Citation3]. Patients were discharged when their renal function and the doses of antirejection drugs were stable. Infection, such as pneumonia or urinary tract infection, was not observed. The wound healed well and the internal stent was removed.
The estimated GFR (eGFR) was calculated from sCr and Cys C using the CKD-EPI (2009 [Citation12] and 2012 [Citation13]) formula ().
Table 1. The CKD-EPI formula for calculating eGFR.
SPS is a condition in which the ratio of Cys C-based eGFR and sCr-based eGFR is less than 0.7 (SPS = eGFRCys C/eGFRsCr ≤ 0.7) [Citation9].
Statistical analysis
Data were analyzed using SPSS 26.0 and the diagrams were plotted using Graphpad 8.0. Kolmogorov-Smirnov test was used to examine the normality of the variables. Normally distributed data were summarized as mean and standard deviation. Continuous variables were compared by Mann–Whitney test or t-test. Categorical variables were shown as percentages and compared by the Chi-square test. The receiver-operating characteristic (ROC) curves and the area under the curve (AUC) were used to determine the efficiency of sCr and Cys C in predicting DGF. The cut-off point with the maximum sum of sensitivity and specificity was selected. All analyses were two-tailed with a significance level of 0.05.
Results
Patients’ characteristics
The clinical characteristics of 198 RT recipients at baseline are shown in . Among these patients, 39 suffered DGF. All variables listed in were normally distributed. No significant difference in baseline clinical features was observed between the two groups (p > .05).
Table 2. Baseline clinical features of patients with or without DGF.
The levels of cys C and sCr in the DGF and non-DGF groups
The concentrations of Cys C and sCr in the two groups are shown in . The results of sCr and Cys C levels were normally distributed. The DGF group showed markedly higher levels of sCr and Cys C at all time points compared to the non-DGF group (p < .05).
Table 3. The levels of Cys C and sCr in patients with or without DGF.
The longitudinal changes at the first week after RT in Cys C and sCr levels in DGF and non-DGF patients are shown in . The sCr concentrations in both groups declined rapidly after surgery and then further decreased slowly in the following days. The Cys C and sCr levels of DGF patients were higher than those of the non-DGF group at all time points. However, the decrease in Cys C levels in the DGF group was slower than that in patients without DGF.
Figure 1. The longitudinal changes of cystatin C (Cys C) (left panel) and serum creatinine (sCr) (right panel) in delayed graft function (DGF) and prompt graft function (non-DGF) patients. The Cys C and sCr levels of DGF patients were higher than those of the non-DGF group at all time points. The sCr concentrations in both groups declined rapidly after surgery, the decrease in Cys C levels in the DGF group was slower than that in patients without DGF.

ROC analysis of sCr and cys C for predicting DGF
The predictive value of sCr and Cys C was evaluated by the ROC curves. The AUC and P-values for these markers on postoperative days 1, 2, 3 and 7 are shown in and . Both Cys C and sCr accurately predicted DGF. Cys C showed the largest AUC (0.928). The cut-off points for Cys C and sCr were then selected according to the maximum sum of sensitivity and specificity. Cys C at a concentration of 4.9 mg/L had the highest sum of sensitivity and specificity, with a sensitivity of 0.889 and a specificity of 0.8.
Figure 2. ROC analysis of sCr (A) and Cys C (B) for predicting DGF. Both Cys C and sCr predicted DGF, Cys C showed the largest area under curve.
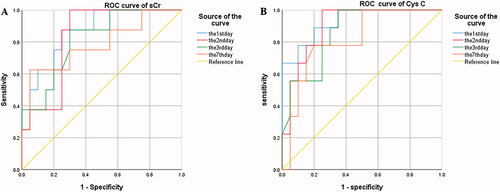
Table 4. The predictive value of Cys C and sCr by the ROC curves.
SPS in RT recipients
To determine whether there was a pathophysiological association between SPS and RT outcomes, the concentrations of Cys C and sCr in patients with or without SPS at discharge day were compared. There were 32 patients in the DGF group and 51 in the non-DGF group diagnosed with SPS. The proportion of cases with SPS in the DGF group was higher than that in patients without DGF (p < .05) in . The Cys C levels of patients with SPS were higher than those of the non-SPS group (p < .05), shown in .
Table 5. SPS in RT recipients with or without DGF.
Table 6. The levels of Cys C and sCr in RT recipients with or without SPS.
Follow-up of patients with or without SPS
Patients were followed in the outpatient department for one year after surgery. The follow-up data showed that patients with SPS had significantly higher levels of sCr and Cys C compared to other patients (p < .05), shown in .
Table 7. Follow-up of RT recipients with or without SPS.
Discussion
DGF is a common complication after RT that affects both recipient and graft survival. The diagnosis of DGF depends on the need for hemodialysis, changes in sCr levels, and other factors [Citation14]. Some predictive models have been developed for the diagnosis of DGF, but they were not effective and accurate due to complex influences [Citation15]. Neither sCr nor sCr-based eGFR is a reliable diagnostic indicator for DGF. The sCr levels increase only when GFR decreases by more than 50%. Also, sCr levels are affected by various factors, such as gender, age, and dietary habits, which may lead to an inaccurate diagnosis of the disease [Citation16]. Clinically, new markers are expected to evaluate renal status after RT. Cys C is a cysteine protease inhibitor and its levels are not affected by age, gender, inflammatory response, protein intake, etc. The kidney is the only organ where Cys C is degraded. It is filtered by the glomerulus, and neither secreted nor excreted by the renal tubules [Citation17]. Therefore, Cys C has been considered a better indicator of renal function and GFR than sCr and has been routinely measured in critically ill patients and patients after cardiac surgery [Citation18].
Our study found that the Cys C levels of patients with DGF were significantly higher than those in the non-DGF group. The analysis of the longitudinal changes in Cys C showed that the decrease in Cys C levels was not evident. The ROC curves showed that Cys C had the largest AUC and the highest sensitivity, and the highest diagnostic efficiency was observed on postoperative day 1. Also, patients may receive dialysis on subsequent days. Therefore, the Cys C levels should be measured on the first day after the operation, because Cys C is a more reliable diagnostic marker for DGF than sCr. It is also considered a sensitive marker for early acute kidney injury [Citation19]. The Cys C levels can be used to predict both DGF and renal function at discharge with better efficiency than sCr [Citation20]. Taken together, Cys C is more sensitive than sCr in indicating GFR damage for a short period of time and in predicting the recovery of graft renal function.
The long-term prognosis of RT is complicated because the renal function can be affected by many factors. The effect of DGF on long-term renal function following RT is manifested by the decrease of GFR [Citation21]. Cys C is a more accurate and sensitive indicator for GFR than sCr. In this study, we followed RT recipients for one year and introduced the term ‘SPS’ for the first time. SPS is a newly defined kidney disorder in which the ratio of Cys C-based eGFR over sCr-based eGFR is less than 0.7 (SPS = eGFRCys C/eGFRsCr ≤ 0.7) [Citation22]. SPS indicates renal function impairment and is associated with elevated levels of atherosclerosis-promoting proteins [Citation23]. During long-term follow-up, patients with SPS showed a higher mortality rate compared to other patients [Citation9,Citation10]. SPS is also associated with an increased risk of cardiac surgery and is an independent predictor of long-term mortality in patients undergoing coronary artery bypass grafting [Citation24,Citation25]. Our study showed a higher proportion of patients with SPS in the DGF group compared to the non-DGF population. At one- year post-operation, recipients who were diagnosed with SPS showed highly expressed sCr and Cys C, which was consistent with the findings that DGF led to a decrease in eGFR expression during long-term follow-up [Citation21]. A decrease in eGFR may increase mortality in patients [Citation26]. We speculated that recipients who were diagnosed with SPS based on the Cys C levels might have a poor prognosis. The diagnosis of SPS may enable early intervention, reduce the progression of chronic rejection, and therefore improve the follow-up of patients with potentially poor prognoses.
Our study has some limitations. First, it was a single-center study with a short follow-up time and a small sample size. Multicenter studies with long-term follow-up and a larger sample size are needed. Secondly, it was a retrospective study. Although inclusion criteria were established, selection bias might occur. Further investigations with a prospective design are needed.
Conclusions
Cys C is a reliable indicator of renal function after RT. Cys C at a concentration of 4.9 mg/L had the highest sum of sensitivity and specificity for prediction of DGF, with a sensitivity of 0.889 and a specificity of 0.8. SPS is associated with the development of DGF and the poor long-term prognosis of RT. Therefore, Cys C may be used to predict the perioperative and long-term prognosis of RT recipients.
Author contributions
All authors participated in this study including data interpretation and manuscript preparation. Cuixing Zhou performed the data management and statistical analyses. All authors took full responsivities for the manuscript.
Consent to participate
Written informed consent for the study was obtained from each patient involved in the study after oral notification.
Consent for publication
Written consent for publication was obtained from all the patients involved in our study. No identifiable individual patient or health person was involved in this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Zhang L, Zeng L, Gao X, et al. Transformation of organ donation in China. Transpl Int. 2015;28(4):410–415.
- Mannon RB. Delayed graft function: the AKI of kidney transplantation. Nephron. 2018;140(2):94–98.
- Bahl D, Haddad Z, Datoo A, et al. Delayed graft function in kidney transplantation. Curr Opin Organ Transplant. 2019;24(1):82–86.
- Hsu RK, Hsu CY, McCulloch CE, et al. Research-based versus clinical serum creatinine measurements and the association of acute kidney injury with subsequent kidney function: findings from the chronic renal insufficiency cohort study. Clin Kidney J. 2020;13(1):55–62.
- Pozzoli S, Simonini M, Manunta P. Predicting acute kidney injury: current status and future challenges. J Nephrol. 2018;31(2):209–223.
- Grubb A. Cystatin C is indispensable for evaluation of kidney disease EJIFCC. EJIFCC. 2017;28(4):268–276.
- Kar S, Paglialunga S, Islam R. Cystatin C is a more reliable biomarker for determining eGFR to support drug development studies. J Clin Pharmacol. 2018;58(10):1239–1247.
- Ferguson TW, Komenda P, Tangri N. Cystatin C as a biomarker for estimating glomerular filtration rate. Curr Opin Nephrol Hypertens. 2015;24(3):295–300.
- Grubb A. Shrunken pore syndrome – a common kidney disorder with high mortality. Diagnosis, prevalence, pathophysiology and treatment options. Clin Biochem. 2020;83:12–20.
- Åkesson A, Lindström V, Nyman U, et al. Shrunken pore syndrome and mortality: a cohort study of patients with measured GFR and known comorbidities. Scand J Clin Lab Invest. 2020;80(5):412–422.
- Siedlecki A, Irish W, Brennan DC. Delayed graft function in the kidney transplant. Am J Transplant. 2011;11(11):2279–2296.
- Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612.
- Inker LA, Schmid CH, Tighiouart H, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med. 2012;367(1):20–29.
- Chen R, Wang H, Song L, et al. Predictors and one-year outcomes of patients with delayed graft function after deceased donor kidney transplantation. BMC Nephrol. 2020;21(1):526.
- De Geus HR, Betjes MG, Bakker J. Biomarkers for the prediction of acute kidney injury: a narrative review on current status and future challenges. Clin Kidney J. 2012;5(2):102–108.
- Porrini E, Ruggenenti P, Luis-Lima S, et al. Estimated GFR: time for a critical appraisal. Nat Rev Nephrol. 2019;15(3):177–190.
- Inker LA, Okparavero A. Cystatin C as a marker of glomerular filtration rate: prospects and limitations. Curr Opin Nephrol Hypertens. 2011;20(6):631–639.
- Lee SH, Youn YN, Choo HC, et al. Cystatin C as a predictive marker of renal dysfunction and mid-term outcomes following off-pump coronary artery bypass grafting. Heart. 2015;101(19):1562–1568.
- Beker BM, Corleto MG, Fieiras C, et al. Novel acute kidney injury biomarkers: their characteristics, utility and concerns. Int Urol Nephrol. 2018;50(4):705–713.
- Li F, Hu L, Zhao X, et al. The value of cystatin C and urinary and serum neutrophil gelatinase-associated lipocalin during the perioperative period of renal transplantation. Transl Androl Urol. 2019;8(5):432–441.
- Lee J, Song SH, Lee JY, et al. The recovery status from delayed graft function can predict long-term outcome after deceased donor kidney transplantation. Sci Rep. 2017;7(1):13725.
- Grubb A, Lindström V, Jonsson M, et al. Reduction in glomerular pore size is not restricted to pregnant women. Evidence for a new syndrome: ‘Shrunken pore syndrome’. Scand J Clin Lab Invest. 2015;75(4):333–340.
- Almén MS, Björk J, Nyman U, et al. Shrunken pore syndrome is associated with increased levels of atherosclerosis-promoting proteins. Kidney Int Rep. 2019;4(1):67–79.
- Herou E, Dardashti A, Nozohoor S, et al. The mortality increase in cardiac surgery patients associated with shrunken pore syndrome correlates with the eGFRcystatin C/eGFRcreatinine-ratio. Scand J Clin Lab Invest. 2019;79(3):167–173.
- Ljungberg J, Johansson B, Bergdahl IA, et al. Mild impairment of renal function (shrunken pore syndrome) is associated with increased risk for future surgery for aortic stenosis. Scand J Clin Lab Invest. 2019;79(7):524–530.
- Mooney JF, Croal BL, Cassidy S, et al. Relative value of cystatin C and creatinine-based estimates of glomerular filtration rate in predicting long-term mortality after cardiac surgery: a cohort study. BMJ Open. 2019;9(9):e029379.
