Abstract
IgE sensitization profiles to single birch allergens in birch-sensitized patients differ among European countries. The aim of this study was to determine the distribution of specific IgE antibodies to major and minor birch pollen allergens in a population of allergic Norwegian individuals by using a birch allergic blood donor population as a surrogate sample. Sixty blood donors were recruited and sampled based on birch allergy symptoms such as rhinitis, rhinoconjunctivitis and/or mild asthma in previous seasons. All sera were collected before start of the pollen season and tested using a line blot assay (Euroimmun AG, Lübeck, Germany) for IgE to birch and timothy pollen. Both extracts, single allergens, and cross-reacting carbohydrate determinants (CCD) were analysed. Only donors with specific IgE to birch and/or timothy grass were further evaluated. Specific IgE to birch pollen extract was found in 52 sera, and sensitization to timothy grass in 40 sera. Specific IgE to Bet v 1 was predominant in contrast to Bet v 4 which was absent. However, sensitization to the minor allergens Bet v 2 and 6 was always found together with high levels of IgE to Bet v 1. Subjects sensitized to the profilin Bet v 2 from birch were also sensitized to Phl p 12 from timothy grass. In conclusion, there was predominantly Bet v 1 sensitization in this cohort and low sensitization to minor allergens and cross-reactive allergens (Bet v 2, Bet v 4, Phl p 7 and Phl p 12).
Background
Immunoglobulin E (IgE) mediated pollen allergy is a substantial health issue in developed countries. Methods used to assess IgE sensitization patterns are skin prick test and plasma/serum analysis of allergen specific IgE to commercially available pollen extracts. Diagnostic pollen extracts serve as screening for sensitization to one or more particular allergenic molecules (allergens), contained in the extract. Each pollen-sensitized individual has a unique sensitization profile showing not only what allergens the patient is sensitized to, but also how high the concentration is of specific IgE to a particular allergen.
Knowing a patient’s individual sensitization profile is useful when prescribing therapeutic pollen vaccine for patients selected for allergen-specific immunotherapy (ASIT). The allergenic profile of the pollen vaccine product used for a particular patient should match the patient`s sensitization profile. Mapping of sensitization profiles in a larger population helps to understand exposure to various allergens and allergy development in a given geographic region.
It is estimated that 20% or more of the Norwegian population has some kind of pollen allergy [Citation1]. The pollen season in Norway is long, starting with alder late in winter followed by hazel, birch, Salix, and ending with timothy grass in summer and weed in autumn. Distribution of the tree types in the long-stretched country varies among regions, but as tree pollen tends to spread more than grass pollen, facilitated by the distance from the ground and the winds, tree pollen is widely spread in all parts of Norway even if the distribution of the trees is different from south to north. Other factors facilitating this spread of pollen are dry sunny weather, high temperatures, high radiation (minimal clouds), wind and low air humidity. Thus, the weather condition is an indicator of pollen seasons in the different parts of Norway [Citation2].
The major birch pollen allergen shares a sequence homology of approximately 80% with major allergens in alder and hazel [Citation3]. Proteins in the birch extract show a huge cross reactivity with similar proteins from other plants and foods. Sensitization patterns to birch and its components in a blood donor population (healthy adults aged 18–70) provide valuable data to determine the birch sensitization profiles in a general Norwegian adult population with allergy. Similar studies, using patient material however, were earlier carried out in Sweden [Citation4], and many other countries [Citation5].
Birch extract consists of both major and minor allergen molecules with varying clinical impact. Of these Bet v 1 is the major allergen molecule belonging to the pathogenesis related protein group 10 (PR-10), with a sensitization rate of about >90% among birch sensitized individuals. It is the most clinically important allergen among the birch-sensitized individuals [Citation6–8]. Bet v 2 is a profilin, which is a plant panallergen. In a study from Austria, 10–20% of all persons with sensitization to birch are also sensitized to Bet v 2 [Citation9]. Bet v 3 and Bet v 4 are polcalcins (calcium binding proteins). They are also panallergens and can cross-react with unrelated species as well [Citation10]. Less than 10% of birch allergic individuals are sensitized to polcalcins. Bet v 6 is a minor allergen of birch with almost 32% sensitization among birch allergic individuals in a German study. It belongs to the isoflavone reductases, and was formerly named Bet v 5 [Citation11]. In addition, Bet v 7, a cyclophilin, and Bet v 8 from the pectin methyl-esterase protein family, are minor birch allergens [Citation12]. Sensitization to CCD (cross-reacting carbohydrate determinants) can also be the cause of positive IgE tests to natural birch extract. This sensitization does not have any clinical relevance, as the CCD molecules give false positive reactions to birch extract [Citation13].
Pathogen related protein (PR-10) is common in plants from the Fagales order and shows significant cross reactivity throughout the species. This leads to allergic symptoms upon ingestion of various foods that contain Bet v 1 homologous proteins [Citation14]. Other minor allergen molecules can give symptoms on atypical times, for their appearance, due to cross reactivity beyond the same species. Knowledge about the common molecular profiles for allergens is therefore of great importance for public health.
There are several published studies on molecular sensitization profiles to pollen allergens in patients both from Scandinavia and from Central Europe [Citation6,Citation7] showing different sensitization profiles and patterns in different regions. Although Panzners study [Citation7] uses multiplex method for IgE detection, both studies lack testing for IgE to Bet v 6, a relatively common minor birch allergen [Citation15].
The aim of our study was to assess IgE sensitization profiles in a cohort of birch pollen allergic individuals. Because obtaining serum samples from pollen allergic patients was resource-intensive, we used blood donors from Oslo and surrounding regions in South-East Norway as a surrogate population sample, in order to reveal the distribution of sensitization to specific pollen allergen molecules in the adult Norwegian population with pollen allergy. We also aimed to apply a cost effective way of mapping a large number of persons for many allergen molecules rapidly.
Methods
Study design
The study has a cross sectional design.
Participants
We recruited sixty blood donors with self-reported symptoms of birch allergy from the blood bank of Oslo University Hospital. A blood sample from all the participants was tested for IgE antibodies as described below. The participants were part of a larger randomized clinical trial approved by the regional ethical committee [Citation16]. All blood samples were collected at the time of inclusion (early February to mid-April, before start of the pollen season) and kept frozen at −40 °C until analysis.
We assume that the distribution of molecular sensitization in the pollen allergic general population is similar to that of the blood donors with pollen allergy. However, the severity of symptoms is lower in the blood donor population due to selection guidelines for donors, which exclude individuals with severe allergies [Citation17].
IgE oligoplex assay
We used an oligoplex line blot enzyme-immunoassay (EIA) to detect IgE against birch (t3), timothy grass (g6), their components as listed below, and CCD. The test was purchased from Euroimmun AG, Lubeck, Germany, and employed according to the manufacturer’s instructions. This assay can analyse numerous allergens in a short time period, in a large number of individuals. The test results were obtained quantitative in kUA/L, and reported in a semi-quantitative way in EAST classes (), which corresponds well to clinical symptoms [Citation18].
Table 1. EAST classes with Assumed clinical correlation the classes are defined according to the following concentrations*.
Allergens used in the oligoplex assay
Birch pollens:
Birch t3
rBet v 1 PR-10, Birch Betula verrucosa t215
r Bet v 2 Profilin, Birch Betula verrucosa t216
rBet v 4 Birch Betula verrucosa t220
r Bet v 6 Birch Betula verrucosa t225
rBet v 2, rBet v 4 Birch Betula verrucosa t221
Grass pollens:
Timothy g6
rPhl p 1 Timothy Phleum pratense g205
rPhl p 2 Timothy Phleum pratense g206
nPhl p 4 Timothy Phleum pratense g208
rPhl p 5b Timothy Phleum pratense g215
rPhl p 6 Timothy Phleum pratense g209
rPhl p 7 Timothy Phleum pratense g210
rPhl p 11 Timothy Phleum pratense g211
r Phl p 12 Profilin, Timothy Phleum pratense g212
CCD: MUXF3 cross reacting carbohydrate determinant, Bromelain o214
Statistics
For statistical analyses of Pearson correlations, the statistical and graphics package GraphPad Prism 9.2.0 was employed. P values <.05 were considered statistically significant.
Results
Out of 60 sera tested, 52 (86,7%) reacted with birch extract. The distribution of sensitization to major and minor birch pollen allergens were as follows: Bet v 1 (94.2%), Bet v 2 (1.9%) and Bet v 6 (11.5%) and CCD (9.6%) (). Specific IgE to Bet v 1 was predominant in this population. In contrast, no reactivity to Bet v 4 was detected. Further, when sensitization to minor allergens (Bet v 2 and 6) was found, it was always in patients with Bet v 1 sensitization who present high (classes 4 and 5) levels of IgE to Bet v 1. We also tested for IgE to timothy grass and its components and found sensitization in 40 of the recruited donors (67%). 73% of persons sensitized to birch were also sensitized to grass (). One person sensitized to the profilin Bet v 2 from birch was also sensitized to Phl p 12 (profilin from timothy grass).
Figure 1. Heat map showing the sensitization to birch and timothy grass extracts and molecular sensitization profiles to single birch and timothy grass allergens. Results for each subject given in EAST classes (0: green, 1: light yellow, 2: yellow, 3: orange, 4: light red, 5: bright red).
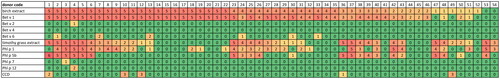
When associations between sensitization to birch and timothy grass allergens were examined, there was as expected high positive correlations between t3 and Bet v 1 (r = 0.926), and between timothy grass extract (g6) and its most important allergen Phl p 1 (r = 0.704). There were no significant correlations between birch and timothy grass extracts (t3 versus g6) or allergens (Bet v 1 versus Phl p 1). Correlations between Bet v 2 and other allergens were not performed, since only one person was sensitized to Bet v 2. The same was the case for the minor timothy grass allergens Phl p 7 and 12.
Discussion
Here, we assess IgE sensitization profiles to birch and timothy grass pollen allergens in birch pollen allergic blood donors by use of an oligoplex specific Ig-E assay. The study therefore does not describe sensitization patterns to pollen in the general Norwegian population. The present population tested was recruited for participation in a previous intervention study in birch pollen allergic blood donors [Citation16]. However, it is undisputable that the major allergy in the normal Norwegian population is sensitization to birch pollen (Bet v 1), as shown by previous reports [Citation6,Citation7]. In addition, a majority (73%) of the subjects were also sensitized to timothy grass pollen. Sensitization patterns described in our study are for birch pollen allergens comparable with those for Scandinavian countries [Citation6] but lower than those from Central Europe [Citation7].
Assessing molecular profiles of birch allergy in a group representing the Norwegian adult population is of great importance, because the duration of the allergy season is long, and cross-reactivity and genuine allergy give various symptoms. Symptoms also tend to last longer when cross-reactivity is involved [Citation5]. It may be important to know which main allergen the individual is reacting to when planning for allergen immunotherapy. When Bet v 1 is the major allergen, immunotherapy to birch has good effect on symptoms from related species as well [Citation19]. However, immunotherapy with timothy grass pollen extract does not help against symptoms from birch allergy [Citation20]. Since only one person was double positive for the minor allergens Bet v 2 and Phl p 12 (), our practice to use Bet v 2 sensitization as a surrogate marker for all profilins could not be evaluated.
Use of oligoplex assays with numerous allergens to assess molecular allergy patterns has both advantages and limitations. One advantage is that sensitization towards a broad array of allergens can be tested, enabling opportunity to detect sensitization to many allergen molecules both specific and potentially cross-reactive. Oligoplex assays are particularly of advantage for individuals with multi-sensitization and complex sensitization patterns. Such assays have improved much lately. The cost is reduced due to need of fewer reagents and use of less sample volume compared to singleplex methods [Citation18]. In our study, we tested for IgE to both birch and timothy grass allergens.
Interpretation of extract-based test results of specific IgE to pollen should consider the fact that pollen extracts contain CCD which is an allergen without clinical relevance [Citation21,Citation22]. However, without molecular diagnostics, one cannot differentiate between clinically relevant allergy and reaction due to cross-reactive proteins with varying severity of symptoms.
There are however some limitations to such assays. The feasibility of testing large groups of individuals with so many allergens can be debated. Also, cost benefit when testing individuals with simple sensitization patterns is not effective. Compared to singleplex assays, the oligoplex approach becomes costly in these individuals.
The prevalence of sensitization to timothy grass pollen allergens in our study may not be representative for the overall timothy grass pollen allergic population as our study participants were recruited solely based on symptoms of birch pollen allergy.
To avoid obvious confounding factors such as variable allergen exposure, the blood samples were collected before the start of the pollen season. In this period most of the participants did not need anti-allergic medication, thus any potential pharmacological influence on the results was avoided.
Conclusions
Blood donors with birch pollen allergy were used as a surrogate population sample for pollen allergic patients, in order to study distribution of sensitization to pollen on molecular level in adult Norwegians with pollen allergy. The line blot method employed is a user-friendly and cost-effective way of rapidly mapping a large sample number for reactivity to many allergen molecules. The distribution of molecular sensitization patterns in our population sample is similar to previously published data for Nordic countries.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Facts about pollen allergy. Norwegian Association for Asthma and Allergy | NAAF [cited 2023 Jun 12]. Available from: https://www.naaf.no/allergi/pollenallergi/fakta-om-pollenallergi.
- When does the season start?. Norwegian Association for Asthma and Allergy | NAAF [cited 2023 Jun 12] Avialable from: https://www.naaf.no/allergi/pollenallergi/nar-starter-pollensesongen.
- Heath MD, Collis J, Batten T, et al. Molecular, proteomic and immunological parameters of allergens provide inclusion criteria for new candidates within established grass and tree homologous groups. World Allergy Organ J. 2015;8:1–11.
- Stern A, van Hage-Hamsten M, Sondell K, et al. Is allergy screening of blood donors necessary? A comparison between questionnaire answers and the presence of circulating IgE antibodies. Vox Sang. 1995;69(2):114–119. doi: 10.1111/j.1423-0410.1995.tb01680.x.
- Biedermann T, Winther L, Till SJ, et al. Birch pollen allergy in Europe. Allergy. 2019;74(7):1237–1248. doi: 10.1111/all.13758.
- Moverare R, Westritschnig K, Svensson M, et al. Different IgE reactivity profiles in birch pollen-sensitive patients from six European populations revealed by recombinant allergens: an imprint of local sensitization. Int Arch Allergy Immunol. 2002;128(4):325–335. doi: 10.1159/000063855.
- Panzner P, Vachova M, Vitovcova P, et al. A comprehensive analysis of Middle-European molecular sensitization profiles to pollen allergens. Int Arch Allergy Immunol. 2014;164(1):74–82. doi: 10.1159/000362760.
- Matricardi PM, Kleine-Tebbe J, Hoffmann HJ, et al. EAACI molecular allergology user’s guide (MAUG). Pediatric Allergy Immunology. 2016;27(S23):1–250. doi: 10.1111/pai.12563.
- Valenta R, Duchêne M, Vrtala S, et al. Profilin, a novel plant pan-allergen. Int Arch Allergy Immunol. 1992;99(2-4):271–273. doi: 10.1159/000236263.
- Asero R, Jimeno L, Barber D. Preliminary results of a skin prick test-based study of the prevalence and clinical impact of hypersensitivity to pollen panallergens (polcalcin and profilin). J Investig Allergol Clin Immunol. 2010;20:35–38.
- Karamloo F, Schmitz N, Scheurer S, et al. Molecular cloning and characterization of a birch pollen minor allergen, bet v 5, belonging to a family of isoflavone reductase-related proteins. J Allergy Clin Immunol. 1999;104(5):991–999. doi: 10.1016/s0091-6749(99)70080-1.
- Mahler V, Fischer S, Heiss S, et al. cDna cloning and characterization of a cross-reactive birch pollen allergen: identification as a pectin esterase. Int Arch Allergy Immunol. 2001;124(1-3):64–66. doi: 10.1159/000053670.
- Ebo DG, Hagendorens MM, Bridts CH, et al. Sensitization to crossreactive carbohydrate determinants and the ubiquitous protein profilin: mimickers of allergy. Clin Exp Allergy. 2004;34(1):137–144. doi: 10.1111/j.1365-2222.2004.01837.x.
- Hauser M, Asam C, Himly M, et al. Bet v 1-like pollen allergens of multiple fagales species can sensitize atopic individuals. Clin Exp Allergy. 2011;41(12):1804–1814. doi: 10.1111/j.1365-2222.2011.03866.x.
- Wellhausen A, Schoning B, Petersen A, et al. IgE binding to a new cross-reactive structure: a 35 kDa protein in birch pollen, exotic fruit and other plant foods. Z Ernahrungswiss. 1996;35(4):348–355. doi: 10.1007/BF01610553.
- Mahmood F, Hetland G, Nentwich I, et al. Agaricus blazei-based mushroom extract supplementation to birch allergic blood donors: a randomized clinical trial. Nutrients. 2019;11(10):2339. doi: 10.3390/nu11102339.
- Nissen-Meyer LSH, Seghatchian J. Donor health assessment – when is blood donation safe? Transfus Apher Sci. 2019;58(1):113–116. doi: 10.1016/j.transci.2018.12.016.
- Popescu F-D, Mariana V. Precision medicine allergy immunoassay methods for assessing immunoglobulin E sensitization to aeroallergen molecules. World J Methodol. 2018;8(3):17–36. doi: 10.5662/wjm.v8.i3.17.
- Kleine-Tebbe J, Zuberbier T, Werfel T, et al. Is allergy immunotherapy with birch sufficient to treat patients allergic to pollen of tree species of the birch homologous group? Allergy. 2020;75(6):1327–1336. doi: 10.1111/all.14130.
- Ellis AK, Tenn MW, Steacy LM, et al. Lack of effect of timothy grass pollen sublingual immunotherapy tablet on birch pollen-induced allergic rhinoconjunctivitis in an environmental exposure unit. Ann Allergy Asthma Immunol. 2018;120(5):495–503.e2. doi: 10.1016/j.anai.2018.02.003.
- van Ree R. Carbohydrate epitopes and their relevance for the diagnosis and treatment of allergic diseases. Int Arch Allergy Immunol. 2002;129(3):189–197. doi: 10.1159/000066770.
- Kochuyt AM, Van Hoeyveld EM, Stevens EA. Prevalence and clinical relevance of specific immunoglobulin E to pollen caused by sting- induced specific immunoglobulin E to crossreacting carbohydrate determinants in Hymenoptera venoms. Clin Exp Allergy. 2005;35(4):441–447. doi: 10.1111/j.1365-2222.2005.02217.x.
