Abstract
Objective: Distal esophageal spasm (DES) is a rare motility disorder characterized by premature and rapidly propagated contractions of the distal esophagus. Treatment options are limited and often poorly effective. Peroral endoscopic myotomy (POEM) seems an effective and attractive new treatment option for DES. In this case report we describe some of the difficulties that could arise.
Materials and methods: A 84-year old man with therapy-refractory DES and complaints of severe dysphagia and chest pain underwent a POEM procedure under general anesthesia. A longer myotomy was performed to cleave the circular muscle layer from start till end of the spastic contractions.
Results: The length of the myotomy was 16 cm. Hyperactive spastic contractions during the procedure complicated the creation of the submucosal tunnel, extended the duration (134 vs. 60–90 min for achalasia), increased postoperative pain and prolonged hospital admission. Intravenously nitroglycerin peroperative diminished spastic contractions. Postoperative a remnant of spastic contractions was present, proximal to the myotomy, causing persistent symptoms.
Conclusion: Performing POEM for DES is challenging due to reactive hyperactive spastic contractions during the procedure causing technical difficulties and an extended procedure. A long myotomy, several centimeters above the proximal border of the spastic region, is essential to prevent remnants of spasticity.
Introduction
Distal esophageal spasm (DES) is a rare motility disorder associated with dysphagia and chest pain [Citation1,Citation2]. It is characterized by premature and rapidly propagated contractions of the smooth muscle in the distal esophagus. High-resolution manometry (HRM) is the gold standard to diagnose DES reflected by a reduced distal latency (premature contraction) and spastic contractions [Citation3]. Treatment of DES remains challenging because the treatment options are limited, poorly effective or have a transient effect. Here we describe a case of an 84-year old man with DES refractory to conventional therapy who was treated with peroral endoscopic myotomy (POEM). POEM is a promising, effective and permanent treatment for DES, however in this case we highlight some of the difficulties that could arise.
Case and procedure
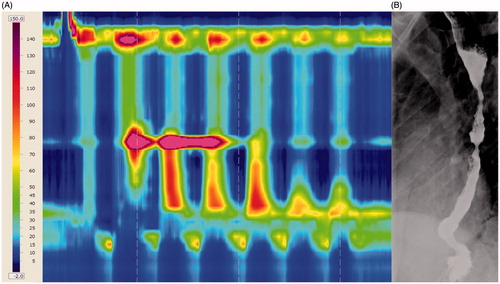
An 84-year old man was referred for dysphagia for solids and liquids, occasional regurgitation and episodic chest pain for many years. There was no weight loss. He had a history of pure sensory stroke without permanent damage, hypercholesterolemia, adrenocorticotropic hormone (ACTH) deficiency resulting in hyponatremia and hypoglycemia treated with hydrocortisone. Furthermore he was taking acetylsalicylic acid, simvastatin, dipyridamole, pantoprazole and vitamin D. Seven months before referral an upper endoscopy showed no abnormalities of the esophagus and biopsies were negative for eosinophilic esophagitis. Conventional manometry revealed simultaneous high-amplitude contractions and normal relaxation of the lower esophageal sphincter (LES) [Citation4]. DES was diagnosed. After failure of treatment with nifedipine, sublingual nitroglycerin, proton pump inhibitors and endoscopic botulinum toxin injections the patient was referred to our center. The Eckardt score (symptom score assessing dysphagia, regurgitation, chest pain and weight loss in achalasia) was five [Citation5]. HRM revealed simultaneous, hypertensive and distally repetitive contractions with a normal LES relaxation (integrated relaxation pressure (IRP) of 8.3 mmHg) and distal latency of three seconds, compatible with DES (). A barium esophagogram showed delayed passage of barium contrast along the entire esophagus with tertiary spastic contractions, resembling a corkscrew (). POEM was purposed and the patient gave informed consent for this procedure. The procedure and follow-up was performed according to the Declaration of Helsinki.
Figure 1. High-resolution manometry (A) and barium esophagogram (B) before treatment. The high-resolution manometry (HRM) shows simultaneous, hypertensive and distally repetitive contractions after a swallow with a normal LES relaxation (integrated relaxation pressure (IRP) of 8.3 mmHg) and distal latency of three seconds typical for DES. On the barium esophagogram tertiary, spastic contractions are seen, resembling a corkscrew and passage of barium contrast is delayed.
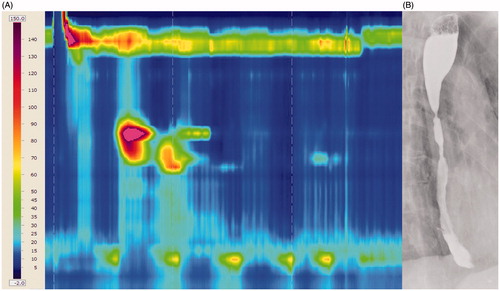
POEM, as described by Inoue et al. was performed under general anesthesia [Citation6]. It was decided to perform a longer myotomy of the circular muscle layer than usual and the mucosal entry was made more proximal, 19 cm above the esophagogastric junction. The myotomy was started 3 cm below the mucosal entry with a total length of 16 cm, 14 cm in the esophagus and 2 cm in the stomach. Hyperactive spastic contractions during the procedure complicated the creation of the submucosal tunnel and made the duration of the procedure longer (134 vs. 60–90 min for achalasia). Therefore, 0.9 mg nitroglycerin (in total) was given intravenously which diminished the spastic contractions. A pneumoperitoneum was effectively desufflated. Post-operatively the patient experienced retrosternal pain which was treated by paracetamol, metamizol and morphine. The water-soluble contrast radiograph of the esophagus the next morning showed a stenosis proximal of the incision with a prestenotic dilation which was attributed to edema and spasm (). This was associated with severe dysphagia. The dysphagia improved two days after the procedure and the patient was discharged. At three months follow-up the symptoms of the patient had improved further, resulting in an Eckardt score of two. However, the patient still experienced dysphagia and occasional episodes of non-passage. HRM demonstrated that proximal to the myotomy a small segment with hypertensive and spastic contractions was still present (). The barium esophagogram showed a proximal prestenotic dilation (). No further treatment was performed because the symptoms were acceptable for the patient.
Figure 2. Radiograph with water-soluble contrast one day after POEM procedure. It demonstrates a stenosis proximal of the incision with a prestenotic dilation which is attributed to edema and spasm and caused severe dysphagia for the patient.

Figure 3. High-resolution manometry (A) and barium esophagogram (B) three months after POEM procedure. Proximal to the myotomy a small segment with hypertensive and spastic contractions is still present on the high-resolution manometry. The barium esophagogram confirms this by showing a proximal prestenotic dilation. These findings explain the cause of high dysphagia the patient still experienced after treatment.
Discussion
The premature and rapidly propagated contractions in DES are caused by the impairment of esophageal inhibitory neural function. Treatment is challenging and in many patients medical treatment is insufficient. POEM has been introduced for achalasia treatment as a less invasive alternative to Heller myotomy [Citation6,Citation7]. For DES, POEM has the advantage over laparoscopic Heller myotomy that the myotomy can be more extended, also cleaving the circular muscles in the mid and proximal esophagus [Citation8–10]. However, this case shows that POEM for DES can be challenging and we have learned two lessons. First, reactive spastic contractions during and after the procedure may complicate execution of the technique and lengthen the procedure, increase post-operative pain and prolong hospital admission. Nitroglycerin during the procedure can be helpful. Second, the myotomy should start more proximally than usual, at least several centimeters above the proximal border of the spastic region. Otherwise a remnant of spastic contractions proximal to the myotomy will remain, causing persistent symptoms. HRM can be helpful for guidance. A recent systematic review and meta-analysis on POEM for spastic esophageal disorders which included achalasia type III, distal esophageal spasm and hypercontractile (Jackhammer) esophagus, revealed that POEM is a safe and highly effective treatment for this type of disorders [Citation11]. The tailored procedure with an extended myotomy is a major advantage over other therapeutic options for DES. Based on the literature and our experience we conclude that POEM is a promising treatment for patients with therapy-refractory DES, however the above described caveats should be taken into account.
Disclosure statement
F.A. Ponds: No conflicts of interest.
A.J.P.M. Smout: Bayer (personal fee), Almirall (personal fee)and Will-Pharma (personal fee).
P. Fockens: Olympus (grant, personal fee), Fuijfilm (grant)and Cook (grant, personal fee), Boston (grant).
A.J. Bredenoord: Endostim (grant), Medical Measurement Systems (grant, personal fee), Danone (grant), GivenImaging (grant), Astellas (personal fee), AstraZeneca (personal fee) and Almirall (personal fee).
References
- Richter JE, Castell DO. Diffuse esophageal spasm: a reappraisal. Ann Intern Med. 1984;100:242–245.
- Roman S, Kahrilas PJ. Distal esophageal spasm. Dysphagia. 2012;27:115–123.
- Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–174.
- Spechler SJ, Castell DO. Classification of oesophageal motility abnormalities. Gut. 2001;49:145–151.
- Eckardt VF. Clinical presentations and complications of achalasia. Gastrointest Endosc Clin N Am. 2001;11:281–292.
- Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271.
- von Renteln D, Fuchs KH, Fockens P, et al. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309–311.
- Kandulski A, Fuchs KH, Weigt J, Malfertheiner P. Jackhammer esophagus: high-resolution manometry and therapeutic approach using peroral endoscopic myotomy (POEM). Dis Esophagus 2016;29:695-696.
- Louis H, Covas A, Coppens E, et al. Distal esophageal spasm treated by peroral endoscopic myotomy. Am J Gastroenterol. 2012;107:1926–1927.
- Shiwaku H, Inoue H, Beppu R, et al. Successful treatment of diffuse esophageal spasm by peroral endoscopic myotomy. Gastrointest Endosc. 2013;77:149–150.
- Khan MA, Kumbhari V, Ngamruengphong S, et al. Is POEM the answer for management of spastic esophageal disorders? A systematic review and meta-analysis. Dig Dis Sci. 2017;62:35–44.
