Abstract
Objectives: The clinical relevance of small to moderate sliding hiatal hernias is controversial. The aims of the present study were to (1) investigate which symptoms are associated with sliding hiatal hernias and (2) define the length of a sliding hiatal hernia at which gastrointestinal symptoms occur.
Methods: A study population representative of the general Swedish population answered a questionnaire regarding gastrointestinal symptoms and was investigated with an upper endoscopy. The length of any sliding hiatal hernia was measured.
Results: Only reflux-related symptoms were associated with length of the hiatal hernia (acid regurgitation OR 1.46, CI 1.19–1.79, heartburn OR 1.27, CI 1.05–1.54), and the association did not become significant until an axial hiatal hernia length of 2 cm.
Conclusions: Only reflux symptoms could be attributed to sliding hiatal hernias. Hiatal hernias less than 2 cm should be considered clinically insignificant.
Introduction
A hiatal hernia (HH) is diagnosed when elements of the abdominal cavity herniate through the esophageal hiatus into the mediastinum. HH can be assessed with radiographic, manometric and endoscopic investigations. Most commonly it is the stomach that herniates through the hiatus, and four different types of HH have been described. The most common type of HH is type 1, sliding HH, which constitutes 85–95% of all cases [Citation1–3].
Sliding HH is a common finding at endoscopy, with a prevalence of up to 25% in the general population [Citation4]. A sliding HH is considered present when the gastroesophageal junction (GEJ) is dislocated orally into the thoracic cavity, resulting in a discrepancy between the level of the GEJ and the diaphragmatic hiatus. The GEJ and hiatus are, however, not static, but move several centimeters with breathing and swallowing, which leads to a physiological herniation [Citation1,Citation5]. There is no consensus as to when a physiological herniation becomes a pathological hiatal hernia, but a commonly used cutoff point is 2 cm [Citation1,Citation6]. This is however less than the physiological movement, why this diagnostic definition is controversial. Some authors continue to argue that a short segment hiatal hernia (SSHH) defined as less than 2 cm in length is of clinical significance [Citation7].
The clinical significance of HH has been controversial for decades. It is accepted that HH probably leads to increased gastroesophageal reflux (GER) [Citation1,Citation6,Citation8,Citation9]. There remains however some controversy whether hiatal hernias may also lead to other symptoms, and some argue that HH can give rise to dyspeptic symptoms or dysphagia [Citation2,Citation10].
It has been shown that the interobserver agreement regarding the endoscopic length measurement is poor even under ideal conditions [Citation11]. As a result, the concept of measuring HH endoscopically suffers from this inherent weakness. Another way to assess the GEJ is by grading the gastroesophageal flap valve by using the Hill classification, an approach that has been shown to be reproducible [Citation12].
The aims of the present study were to (1) investigate which gastrointestinal symptoms are associated with sliding hiatal hernias and (2) define the length of a sliding HH at which gastrointestinal symptoms occur.
Materials and methods
A comprehensive description of the setting, population, esophagogastroduodenoscopy (EGD) procedure and symptom evaluation has been given elsewhere [Citation13].
Study population
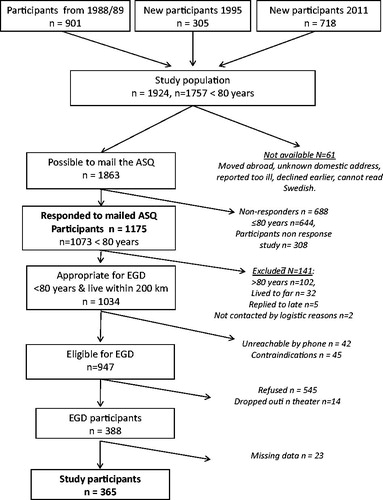
A population cohort in Östhammar, Uppsala county, Sweden, has been studied for over two decades regarding gastrointestinal symptoms [Citation14]. The study population is representative of the general Swedish population in terms of gender, age, income and other potential selection factors. In 2012 this population was invited to participate in the present study. To be invited to the EGD, the subjects had to have participated in the 2011 study. illustrates the study population and dropouts. Exclusion criteria for EGD were angina pectoris, myocardial infarction (last 6 months), congestive heart failure, severe lung disease, severe liver disease, esophageal varices, treatment with anticoagulants, need for anesthesia for the endoscopy, earlier surgery of the stomach, and those 80 years old or above.
Of the 388 individuals who completed the EGD, 23 were excluded because of missing data, leaving 365 individuals in the present study.
Symptoms were evaluated using the validated Abdominal Symptom Questionnaire (ASQ) including 13 upper gastrointestinal symptoms [Citation15]. The participants reported if they had been troubled by any of the symptoms during the last three months.
Endoscopy
The upper endoscopy followed a strict and structured endoscopic protocol, investigating the esophagus, stomach and upper duodenum. The distance between the incisors and GEJ, and between the incisors and hiatus was measured. The length of any sliding hiatal hernia was defined as the discrepancy between these two measurements. The GEJ was defined as the proximal margin of the gastric mucosal folds [Citation16]. The hiatus was defined as the level of the diaphragmatic pitch. The endoscopies were performed by five experienced endoscopists (Among them the authors BW, PH, AF, and LA), who were blinded to the presence of any symptoms. Two of the endoscopists were gastroenterologists, two were surgeons, and one was general practitioner.
Statistics
For identifying upper gastrointestinal symptoms independently associated with the length of HH, multivariable logistic regression analyses were performed. Length of HH was independently associated with a symptom if a HH statistically significantly contributed to the prediction of the symptom compared to a reduced model containing age, gender, body mass index (BMI), Helicobacter pylori infection, and the use of proton pump inhibitors (PPI). The comparison between the model with HH included and the reduced model was based on a likelihood-ratio test. In a first step, multivariable logistic regressions was conducted to identify symptoms independently associated with herniation, the HH as a continuous variable. For symptoms associated with HH, and in order to assess at which length of a sliding HH gastrointestinal symptoms occur, separate multivariable logistic models were performed with each unique combination of symptom as the dependent variable and binary HH cutoff of different length of a sliding HH as independent variable.
Data were analyzed with the statistical software packages Stata (version 13.1; StataCorp LP, College Station, TX). p values (two-sided) <.05 were interpreted as statistically significant.
Ethics
Approval was obtained from the Ethics Committee of Uppsala University (Dnr. 2010/443), and all participants gave their informed consent.
Results
A total of 365 patients were included in the final analysis, 189 women and 176 men. The participants were between 20 and 79 years of age (median 55 years). A total of 107 participants reported acid regurgitations and/or heartburn. Two hundred and forty-nine participants had sliding HH, and fifty-eight participants had esophagitis. Of these 58 participants 36 had grade-A esophagitis according to the LA classification, 19 had grade B, and 3 had grade C ( and ).
Table 1. Demographics of the study population.
Table 2. The length of any sliding hiatal hernia (distance between the gastroesophageal junction and the diaphragmatic pinch) in the investigated population.
The only symptoms that were associated with length of the HH were reflux-related (). Increasing length of sliding HH was significantly associated with a higher odds of acid regurgitation (OR 1.46, CI 1.19–1.79), and heartburn (OR 1.27 CI 1.05–1.54).
Table 3. Associations between increasing length of hiatal hernia and different upper GI-symptoms in ASQ.
When evaluating the association between reflux symptoms and length of HH in a binary fashion, the association became significant at a length of 2 cm ().
Table 4. In order to investigate at which length the HH becomes clinically significant, the association between gastroesophageal reflux and increasing length of HH were evaluated.
Excluding those on current PPI-medication did not alter the results.
Discussion
Sliding HH is a common finding at endoscopy, but there is no clear endoscopic definition of a clinically relevant HH. There are furthermore controversies regarding which symptoms that can be attributed to HH. In an endoscopic population-based study where validated symptom assessments and a standardized endoscopy were both carefully applied, we found that hernias smaller than 2 cm endoscopically were not related to symptoms, and sliding hernias 2 cm or larger were only associated with reflux symptoms but not with any other upper GI symptoms.
HH of different lengths are common findings at endoscopy and are considered present when there is an oral displacement of the GEJ and the proximal part of the stomach into the thoracic cavity. However, the GEJ is a complex anatomical area that moves several centimeters with breathing and swallowing, giving rise to ‘physiological herniation’ of the GEJ. There has been no consensus as to when this ‘physiological herniation’ becomes pathological but our present data suggest that small hernias are asymptomatic and of no clinical relevance.
In the present study, we have investigated a random sample of the normal population, and not a group of patients seeking medical care. In this way, we avoid any referral bias and minimizing selection bias based on high response rates. Since both HH and functional GI symptoms are common in the population, results can be difficult to interpret when analyzing the prevalence of HH in a symptomatic group of patients.
Weaknesses of this study include the lack of an objective measurement of GER, that is, 24-h pH monitoring. There are also known weaknesses in the endoscopic length measurement in esophagus, where the interobserver agreement is a potential limitation for precision [Citation11]. One way to avoid this limitation when assessing the antireflux barrier of the GEJ, is to use the Hill classification, which has been used for grading of the GEJ flap valve mechanism [Citation12]. The Hill classification however is less commonly used in clinical practice but it has been proven to have at least as strong association with GERD as HH [Citation17].
In summary, the present study demonstrates that the only symptoms attributable to HH are symptoms of heartburn and acid regurgitation. Furthermore, our study suggests that hernias less than 2 cm should not be considered as clinically significant. Since there is a known limitation in endoscopic measurement of length, it may be of greater value to assess the GEJ using the Hill classification than to measure the length of small sliding HH, especially in the context of GERD with or without esophagitis [Citation17].
Acknowledgements
The present study was supported by Olympus Solna Sverige AB, who supplied equipment for the realization of the study. The authors have no other affiliation with this company.
Disclosure statement
The authors declare that they have no conflicts of interest concerning this article.
References
- Kahrilas PJ, Kim HC, Pandolfino JE. Approaches to the diagnosis and grading of hiatal hernia. Best Pract Res Clin Gastroenterol. 2008;22:601–616.
- Mittal RK. Hiatal hernia: myth or reality? Am J Med. 1997;103:33S–39S.
- Gordon C, Kang JY, Neild PJ, et al. The role of the hiatus hernia in gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2004;20:719–732.
- Ronkainen J, Aro P, Storskrubb T, et al. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand J Gastroenterol. 2005;40:275–285.
- Lee YY, Whiting JGH, Robertson EV, et al. Measuring movement and location of the gastroesophageal junction: research and clinical implications. Scand J Gastroenterol. 2013;48:401–411.
- Hyun JJ, Bak Y-T. Clinical significance of hiatal hernia. Gut Liver. 2011;5:267–277.
- Hyun JJ, Kim JH, Yeon JE, et al. Short segment hiatal hernia: is it a clinically significant entity? J Neurogastroenterol Motil. 2010;16:35–39.
- Petersen H, Johannessen T, Sandvik AK. Relationship between endoscopic hiatus hernia and gastroesophageal reflux symptoms. Scand J Gastroenterol. 1991;26:921–926.
- Sgouros SN, Mpakos D, Rodias M, et al. Prevalence and axial length of hiatus hernia in patients, with nonerosive reflux disease: a prospective study. J Clin Gastroenterol. 2007;41:814–818.
- Tibbling L, Johansson M, Mjönes AB, et al. Globus jugularis and dysphagia in patients with hiatus hernia. Eur Arch Otorhinolaryngol. 2009;267:251–254.
- Guda N, Partington S, Vakil NB. Inter- and intra-observer variability in the measurement of length at endoscopy: implications for the measurement of Barrett’s esophagus. Gastrointestinal Endoscopy. 2004;59:655–658.
- Hill LD, Kozarek RA, Kraemer SJM, et al. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointestinal Endoscopy. 1996;44:541–547.
- Agreus L, Hellström PM, Talley NJ, et al. Towards a healthy stomach? Helicobacter pylori prevalence has dramatically decreased over 23 years in adults in a Swedish community. UEGJ. 3rd Ed. 2016;4:686–696.
- Agréus L, Svärdsudd K, Nyren O. The epidemiology of abdominal symptoms: prevalence and demographic characteristics in a Swedish adult population: a report from the Abdominal Symptom Study. Scand J Gastroenterol. 1994;13:383–388.
- Agréus L, Svärdsudd K, Nyren O, et al. Reproducibility and validity of a postal questionnaire. The abdominal symptom study. Scand J Prim Health Care. 1993;11:252–262.
- Wallner B. Endoscopically defined gastroesophageal junction coincides with the anatomical gastroesophageal junction. Surg Endosc. 2009;23:2155–2158.
- Hansdotter I, Björ O, Andreasson A, et al. Hill classification is superior to the axial length of a hiatal hernia for assessment of the mechanical anti-reflux barrier at the gastroesophageal junction. Endosc Int Open. 2016;4:(3):E311–7.