Abstract
Objectives: Faecal Calprotectin (FC) is a sensitive marker for gut inflammation. However, slightly elevated FC levels are also common in subjects without inflammation. We investigated the association between FC and clinical factors including concomitant use of medical therapy in patients with a normal colonoscopy.
Material and methods: Out-patients (n = 1263) referred for colonoscopy, performed FC test (CALPRO) the day before the start of bowel preparation. All subjects answered questionnaires that included questions on the present and past health history, concomitant medical treatment and gastrointestinal symptoms (GSRS). A medical record chart review was performed to check for concomitant disease, cause of referral and the result of the colonoscopy including biopsies. Inclusion criteria were a normal colonoscopy. Exclusion criteria were inflammatory bowel disease, colon cancer and high-grade dysplasia.
Results: Five hundred ninety subjects fulfilled the inclusion criteria and completed the study. Thirty-six per cent of the subjects had a FC >50 µg/g. In a logistic regression analysis, age (adjusted OR: 1.051; CI: 1.032–1.071), and the use of proton pump inhibitors (adjusted OR: 3.843; CI: 2.338–6.316), non-steroid anti-inflammatory drugs (adjusted OR: 2.411; CI: 1.162–5.002) and acetylsalicylic acid (adjusted OR: 2.934; CI: 1.085–3.448) were significantly associated with an elevated FC (>50 µg/g).
Conclusions: More than one-third of the patients with a normal colonoscopy performed in clinical routine had a slightly elevated FC level. Our results emphasise the need for attention to age, the use of proton pump inhibitors, non-steroid anti-inflammatory drugs and acetylsalicylic acid in the interpretation of FC tests in clinical practice.
Introduction
Calprotectin is a protein with antibacterial properties that are mainly found in the cytoplasm of neutrophil granulocytes and it has been used as a diagnostic tool to detect inflammation since the early 2000s [Citation1]. Faecal calprotectin (FC) is a sensitive marker of gut inflammation, especially colonic inflammation, and is mainly used in discriminating inflammatory bowel disease (IBD) from functional bowel disorders [Citation1–3]. In patients with IBD, FC levels correlate well with the degree of inflammatory activity; therefore FC has partly replaced endoscopy in the evaluation of inflammatory activity in patients with IBD [Citation4–7]. However, a moderate elevation of FC is also commonly seen in subjects without IBD, which thereby hampers the test specificity [Citation8]. Factors that trigger neutrophils elevate calprotectin. For example, infectious enteritis, diverticulitis, microscopic colitis and rheumatologic disease have been associated with increased FC levels [Citation9–13]. In addition, increased FC levels were shown in patients with colorectal cancer, adenomas and juvenile polyps [Citation14–17]. FC levels are also dependent on age and are seen in both the neonatal period and the elderly [Citation8,Citation18]. For example, more than 25% of subjects 50–70 years old have FC levels above 50 μg/g without any known disease [Citation8]. Many older subjects, as well as subjects with gut symptoms, are on drugs that may directly or indirectly have an effect on gut integrity. It is well known that the use of nonsteroidal anti-inflammatory drugs (NSAID) is associated with a moderate rise in FC levels [Citation19–22]. Also, in some studies, acetylsalicylic acid was shown to be associated with elevated FC levels, whereas this is not the case in some other studies [Citation23–25]. Despite a large number of studies on FC in the last decade, there is still uncertainty as to how to interpret an increased FC level in non-IBD patients. It is not known if drugs other than NSAID, or other factors are associated with FC.
The present study focussed on subjects referred for colonoscopy and with a normal outcome of the examination. We aimed to study the association between factors that include concomitant use of medical therapy and FC levels in patients with a normal colonoscopy.
Methods
Study population
This study is based on the Faecal and Endoscopic Colorectal Study in Umeå (FECSU) entailing a cohort of 1263 patients who underwent colonoscopy at the University Hospital in Umeå, Sweden between May 2007 and February 2013 [Citation26]. All outpatients, independent of cause of referral and who had undergone planned colonoscopy at the endoscopy unit at Norrlands University hospital (Umeå Sweden) were invited to participate in the study. Umeå University hospital has a primary catchment area of 150,000 citizens. Approximately 2500 outpatients were scheduled for colonoscopy during the time period that the study was performed. Exclusion criteria in the FECSU study were if the colonoscopy was planned to be scheduled in less than one week from the decision to investigate the colon, or if the patient had concomitant mental disease, dementia or low-performance status that could restrict the patient from filling in questionnaires or to leaving stool sample. In addition, during some periods (i.e., summer and periods of reorganization) there was a temporary stop in the recruitment of subjects for the study thus resulting in ∼2100 patients were invited. Of these, 1263 patients accepted to participate in the study. All study participants filled in written consent, questionnaires and answered questions about their concomitant medication use (‘What drugs are you currently taking?’), and their present and past health history before they started their bowel preparation for the colonoscopy.
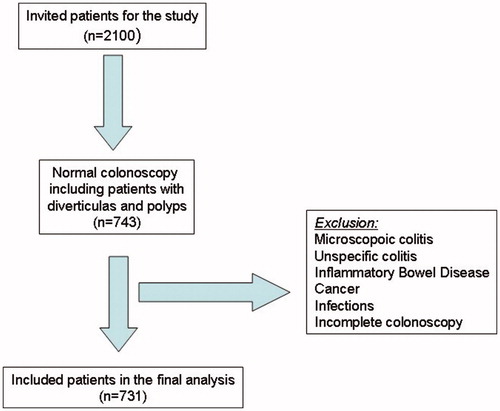
In addition, a medical record chart review was performed to check concomitant diseases, the cause of referral for colonoscopy and the result of the colonoscopy including data on biopsy specimens if available. Only the patients who had a complete colonoscopy to caecum and with a normal endoscopic finding were included in the analysis. Patients with known IBD, microscopic colitis, unspecific colitis or colon malignancies including high-grade dysplasia were not included. Due to the high prevalence in the study population of haemorrhoids, diverticulosis and benign polyps, we included patients with these findings. We used dichotomised variables for haemorrhoids (yes or no), diverticula (yes or no) and hyperplastic polyps/adenoma (yes or no). Seven hundred thirty-one patients fulfilled the inclusion criteria and were included in the analysis.
Faecal calprotectin (FC)
Patients were informed to collect the stool sample the day before the patients started the bowel preparation for the colonoscopy. The stool sample was sent the same day as the colonoscopy was performed to the accredited Department of Laboratory Medicine, Clinical Chemistry, Umeå University Hospital. The samples were analysed using the CALPRO® calprotectin ELISA test according to the manufacturer (Calpro AS Norway). FC was analysed in a single stool sample before colonoscopy preparation. The lowest limit of detection was 20 µg/g faeces, and the upper limit of the analytical range was 10000 µg/g. We used FC level >50 µg/g to define a positive FC test [Citation17].
Faecal immunological test for haemoglobin (FIT)
In a subset of patients (n = 147) a faecal immunological test for haemoglobin (FIT) was analysed from the same stool sample as the FC. FIT was analysed using immunological Analyze F.O.B Test (ANL products AB, Sweden), according to the manufacturer's instruction. A positive test indicates that the sample contains >40 ng/ml of human haemoglobin. Due to the study design, only one single sample per patient was analysed.
Colonoscopy
The colonoscopy was performed in clinical routine by 33 different colonoscopists. Mucosa samples were taken only if the physician judged the need of samples necessary for the clinical assessment. All biopsy specimens were judged by experienced pathologists. Both the physician that performed the colonoscopy and the pathologist were blinded to the outcome of the questionnaires and the result of the FC test.
Gastrointestinal symptoms
For evaluation of the presence of any gastrointestinal symptoms in the last week we used 18 questions from the Gastrointestinal Symptom Rating Scale (GSRS) and GSRS for irritable bowel syndrome (GSRS-IBS) [Citation27,Citation28]. The GSRS and GSRS-IBS are validated questionnaires using a Likert scale (0–6 points) spanning from no symptoms to very severe symptoms. The items are grouped into symptoms clusters for abdominal pain (two items), bloating (three items), diarrhoea (four items) constipation (two items), gastroesophageal reflux (two items) and dyspepsia (three items).
Statistically methods
SPSS version 23 was used for data analysis. Mann–Whitney tests were used for comparison of FC levels. Chi-square tests were used to determine differences in proportions of patients for all dichotomy data. We only analysed factors that were found/reported in at least 10 subjects. Concomitant medications were recorded on the basis of subgroups (i.e., beta blockers, proton-pump inhibitors). A Spearman test was used to analyse correlations between FC levels and gastrointestinal symptoms scores.
A logistic regression analysis with dependent variable FC >50 µg/g was used to control for possible confounding factors. Age, gender and all factors that in the chi-square analysis that showed a p-value below .10 were included as independent variables in the logistic regression analysis. Age was included as a continuous variable and all other variables as dichotomised variables.
Ethics
The study protocol was approved by the Regional Ethical Review Board in Umeå, Sweden (Dnr 08–184 M; Dnr 07–045 M). All individuals in this study signed a written consent form.
Results
Basal characteristics
Seven hundred and thirty-one subjects fulfilled the inclusion criteria (). There were missing data for 141 patients (missed stool samples or incomplete questionnaires) leaving 590 subjects (80.7%) in the final analysis. The basal characteristics of these patients are presented in . There was an equal gender distribution and the most common cause of referral was bleeding (obscure or occult). More than one-third of the patients had a FC level above the cut-off of 50 µg/g.
Table 1. Basal characteristics, cause of referral for colonoscopy and faecal calprotectin outcome in patients (n = 590) referred for colonoscopy with a normal colonoscopy outcome. Note that a single patient may have more than one cause of referral.
Concomitant medical therapy and FC levels
There were several drugs associated with increased FC levels (Supplementary Table 1). We performed a logistic regression analysis with FC >50 µg/g as dependent variable and age, gender and all variables with a p < 0.10 on the Chi-square test as independent variables. Three drugs showed a significant association with increased FC levels in the logistic regression analysis (). Proton pump inhibitor (PPI) use showed the strongest association followed by the use of non-steroid anti-inflammatory drugs (NSAID) and the use of acetylsalicylic acid. Also, age was significantly associated with increased FC levels. The findings of diverticulosis, haemorrhoids or benign polyps on colonoscopy were not associated with increased FC levels.
Table 2. Patients referred for colonoscopy and with a normal colonoscopy finding (n = 590). Logistic regression with dependent variable FC >50 µg/g and independent variables age, male gender, diverticulosis and drugs.
FIT and FC levels
In a subgroup of the patients, FC and FIT were simultaneously analysed from the same stool sample. Significantly more subjects showed a FC > 50 µg/g than a positive FIT test (32% vs 10%; p < .05) (). A FC > 50 µg/g was also significantly more common than a positive FIT test in patients on PPI (64%% vs 19%; p < .001) and in patients on acetylsalicylic acid (63% vs 16%; p < .001).
Table 3. The outcome of faecal calprotectin (FC) test and a faecal immunological test (FIT) in patients referred for colonoscopy and with a normal colonoscopy finding (n = 277). A FC above 50 µg/g is regarded as a positive FC test. The proportion of positive tests is shown for all patients and for patients using acetylsalicylic acid, non-steroidal anti-inflammatory drugs and proton pump inhibitors.
Gastrointestinal symptoms and FC levels
There was a significant but only modest correlation between FC levels and total GSRS-IBS score. Also in the sub-scores for dyspepsia, satiety and diarrhoea, there were modest correlations with FC levels (). Using the median as cut-off only total GSRS IBS score showed a significant association with FC levels (>50 µg/g). When adding total GSRS-IBS score in the logistic regression model, it had no significant influence on the effect of NSAID, acetylsalicylic acid and PPI on FC levels.
Table 4. The correlation between reported gastrointestinal symptoms and faecal calprotectin in patients referred for colonoscopy and with a normal colonoscopy outcome.
Discussion
FC has been proven to be a sensitive marker of gut inflammation and is commonly used in clinical practice to discriminate IBD from functional GI disorders [Citation1–3]. However, the test is hampered with a low specificity and there is still uncertainty of how to interpret slightly elevated FC levels. The present study focussed at investigating possible factors associated with an elevated FC in patients with a normal outcome on colonoscopy. More than one-third of the patients had elevated FC levels, and elevated levels were associated with age and to the use of PPIs, NSAIDs and acetylsalicylic acid in the multivariate analysis. Interestingly, the use of PPIs showed the strongest association to increased FC levels. Increasing age and the use of NSAIDs were shown to be associated with a rise in FC in previous studies [Citation8,Citation19–22]. In patients using acetylsalicylic acid, the data from previous studies are contradicting [Citation23–25]. For example, one small study showed no increase in faecal calprotectin in patients on prophylactic low doses of acetylsalicylic acid [Citation25]. NSAIDs and acetylsalicylic acid are both known to induce enteropathy that includes small erosions or ulcers and these may correspond with inflammation or bleeding from the mucosa. A reduction of mucus, prostaglandins and altering cytokines has been seen in patients treated with NSAIDs [Citation29]. This could lead to intestinal erosions, ulcers, inflammation, stricture, bleeding, protein loss and loss of villi. All of these findings are commonly seen when investigating the small bowel in patients treated with NSAID [Citation29]. Usually, healthy subjects lose 1–2 mL blood in the gastrointestinal tract every day. Previous studies have shown that the use of acetylsalicylic acid and NSAIDs increases the mean faecal blood loss by two to four times; this means that more patients should be positive for FIT [Citation30]. However, in our subgroup analysis, relatively few of these subjects had a positive FIT test.
Also, in a British study, PPIs were to be associated with FC levels [Citation31]. The present study confirms in a larger cohort, and after adjustment for the use of other drugs, that PPIs are associated with increased FC levels in the stool. The reason that PPI use is associated with increased FC levels is uncertain and raises some questions. One possibility could be a positive association between PPIs and inflammation. The lack of data on direct pro-inflammatory effects of PPIs argues against this. Instead, in vitro and in vivo studies have shown that PPIs have anti-oxidative properties [Citation32,Citation33]. It is also known that PPIs, by blocking v-type H+K+ATPases in neutrophil granulocytes, can change their inflammatory abilities to release an oxidative burst and also inhibit their ability to express adhesion molecules [Citation34–36]. The anti-inflammatory effect is separated from its lowering effect of gastric acid in rats and has been shown to protect from ischaemia and reperfusion injuries as well as from NSAID (indometacin) effects of the gut [Citation37,Citation38]. To conclude, PPIs shows more characteristic of having anti-inflammatory actions than pro-inflammatory actions, and other sources are probably more appropriate to cause increased FC levels in stool.
An alternative theory is that PPI treatment induces a bacterial overgrowth with a secondary response of the immune system in the gut. PPIs have been shown to promote bacterial growth due to the inhibition of acid production in the stomach, which may result in a response of neutrophils to bacteria in the gut [Citation39–41]. Naturally occurring bacteria and fungi contain H+K+ATPase. PPIs may affect these microorganisms by direct interaction with the H+K+ATPase and thereby altering the pH-level [Citation39]. There are several studies indicating that PPIs can change the gut microbiota [Citation39–41]. In patients with systemic sclerosis there was an association between dysbiosis and increased FC levels [Citation42]. Also, there is an increased risk of gastroenteritis in PPI users [Citation43]. For example, pathogenic bacteria such as Vibrio cholera and Campylobacter do not survive in a low pH, but when the pH rises these bacteria can evolve and cause gastroenteritis [Citation43]. However, PPIs have also shown to suppress growth and eliminate microbiota through a direct effect on H+ATPase [Citation36].
There could also be factors that influence the stability of calprotectin protein that have impact on the outcome of a FC test. For example, human calprotectin has shown a marked increased thermal stability when pH increases from 7.0 to 8.0 [Citation44], and therefore an increased pH alone could explain the higher FC levels in patients using PPIs.
In our study, we did not investigate the upper gastrointestinal tract, and perhaps the PPI use mirrors a not yet discovered upper GI disease. However, in a study from Italy, there was no association between chronic active gastritis, chronic non-active gastritis or infection with Helicobacter pylori and an increase in FC levels in the stool [Citation45]. In line with this, no association was found with dyspepsia and PPI use and FC levels in a British study [Citation31]. The present study only showed a modest correlation between symptoms of dyspepsia and FC levels, and no association between symptoms of gastroesophageal reflux and FC levels were observed. Adding these GI symptoms in the logistic regression model did not change the association between PPI use and FC levels. Therefore, disease in the upper GI tract probably does not explain the association between PPI use and increased FC levels.
Finally, could increased FC levels reflect an occult gastrointestinal bleeding? A majority of the patients in our study was referred due to suspected gastrointestinal bleeding. Therefore in a subset of patients, we compared a FIT analysis with FC from the same stool sample. The method for FIT was identical to the one used in clinical routine. A ‘positive’ FC test was three times as common as a positive FIT for all patients as well as for the patients who used PPIs and acetylsalicylic acid. Therefore, factors other than GI bleeding are involved in the increase of FC levels in the subjects in our study.
There are some limitations to our study. Firstly, this is a cross-sectional study and, therefore, we are unable to draw conclusions of the cause-effect relationship between PPI use and FC levels. Secondly, we have not consequently investigated the upper GI tract or the small bowel in the study subjects. Therefore, in some patients, there might be undetected pathology in the upper GI tract or small bowel that can cause increases in FC levels. Thirdly, the subjects in the present study belong to a selected group (subjects referred to colonoscopy), and therefore our data may not be fully applicable to a general population. Lastly, there may be other confounders that we did not have data for that might have effect on FC levels.
The strength in our study is that we tested a stool sample just before the preparation of the colonoscopy, and we only included subjects with a normal outcome of the colon investigation. The number of subjects allowed us to make conclusions and to perform a logistic regression analysis, at least for drugs that are commonly used (e.g., PPIs).
To conclude, we found that increased age, the use of NSAIDs, acetylsalicylic acid and PPIs were associated with an increase in FC levels in patients with a normal colonoscopy. Therefore, the use of these drugs should be considered in the interpretation of FC tests in clinical practice.
Supplemental Material
Download MS Word (66.5 KB)Acknowledgement
The authors would like to thanks the staff of the Endoscopic unit at Umeå University Hospital, Umeå, Sweden.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- D'Angelo F, Felley C, Frossard JL. Calprotectin in daily practice: where do we stand in 2017? Digestion. 2017;95:293–301.
- Caviglia GP, Pantaleoni S, Touscoz GA, et al. Fecal calprotectin is an effective diagnostic tool that differentiates inflammatory from functional intestinal disorders. Scand J Gastroenterol. 2014;49:1419–1424.
- Kalantari H, Taheri A, Yaran M. Fecal calprotectin is a useful marker to diagnose ulcerative colitis from irritable bowel syndrome. Adv Biomed Res. 2015;4:85.
- Kawashima K, Ishihara S, Yuki T. Fecal calprotectin predicts relapse and histological mucosal healing in ulcerative colitis. BMC Gastroenterol. 2016;16:47.
- Theede K, Holck S, Ibsen P, et al. Fecal calprotectin predicts relapse and histological mucosal healing in ulcerative colitis. Inflamm Bowel Dis. 2016;22:1042–1048.
- Walsham NE, Sherwood RA. Fecal calprotectin in inflammatory bowel disease. Clin Exp Gastroenterol. 2016;9:21–29.
- Yamaguchi S, Takeuchi Y, Arai K, et al. Fecal calprotectin is a clinically relevant biomarker of mucosal healing in patients with quiescent ulcerative colitis. J Gastroenterol Hepatol. 2016;31:93–98.
- Poullis A, Foster R, Shetty A, et al. Bowel inflammation as measured by fecal calprotectin: a link between lifestyle factors and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev. 2004;13:279–284.
- Nielsen HL, Engberg J, Ejlertsen T, et al. Evaluation of fecal calprotectin in Campylobacter concisus and Campylobacter jejuni/coli gastroenteritis. Scand J Gastroenterol. 2013;48:633–635.
- Kim J, Kim H, Oh HJ, et al. Fecal calprotectin level reflects the severity of Clostridium difficile infection. Ann Lab Med. 2017;37:53–57.
- Tursi A. Biomarkers in diverticular diseases of the colon. Dig Dis. 2012;30:12–18.
- Wildt S, Nordgaard-Lassen I, Bendtsen F, et al. Metabolic and inflammatory faecal markers in collagenous colitis. Eur J Gastroenterol Hepatol. 2007;19:567–574.
- Matzkies FG, Targan SR, Berel D, et al. Markers of intestinal inflammation in patients with ankylosing spondylitis: a pilot study. Scand J Gastroenterol. 2012;47:435–444.
- Olafsdottir I, Nemeth A, Lörinc E, et al. Value of fecal calprotectin as a biomarker for juvenile polyps in children investigated with colonoscopy. J Pediatr Gastroenterol Nutr. 2016;62:43–46.
- Lehmann FS, Trapani F, Fueglistaler I, et al. Clinical and histopathological correlations of fecal calprotectin release in colorectal carcinoma. Wjg. 2014;200:4994–4999.
- Pezzilli R, Barassi A, Morselli Labate AM, et al. Fecal calprotectin levels in patients with colonic polyposis. Dig Dis Sci. 2008;53:47–51.
- Tibble J, Sigthorsson G, Foster R, et al. Faecal calprotectin and faecal occult blood tests in the diagnosis of colorectal carcinoma and adenoma. Gut. 2001;49:402–408.
- Li F, Ma J, Geng S, et al. Fecal calprotectin concentrations in healthy children aged 1-18 months. PLoS One. 2015;10:e0119574.
- Tibble JA, Sigthorsson G, Foster R, et al. High prevalence of NSAID enteropathy as shown by a simple faecal test. Gut. 1999;45:362–366.
- Meling TR, Aabakken L, Røseth A, et al. Faecal calprotectin shedding after short-term treatment with non-steroidal anti-inflammatory drugs. Scand J Gastroenterol. 1996;31:339–344.
- Maiden L, Thjodleifsson B, Theodors A, et al. A quantitative analysis of NSAID-induced small bowel pathology by capsule enteroscopy. Gastroenterology. 2005;128:1172–1178.
- Rendek Z, Falk M, Grodzinsky E, et al. Effect of oral diclofenac intake on faecal calprotectin. Scand J Gastroenterol. 2016; 51:28–32.
- Smecuol E, Pinto Sanchez MI, Suarez A, et al. Low-dose aspirin affects the small bowel mucosa: results of a pilot study with a multidimensional assessment. Clin Gastroenterol Hepatol. 2009;7:524–529.
- Shiotani A, Kamada T, Haruma K. Low-dose aspirin-induced gastrointestinal diseases: past, present, and future. J Gastroenterol. 2008;43:581–588.
- Montalto M, Curigliano V, Santoro L, et al. Prophylactic aspirin therapy does not increase faecal calprotectin concentrations. Eur J Gastroenterol Hepatol. 2006;18:965–967.
- Eklöf V, Löfgren-Burström A, Zingmark C, et al. Cancer-associated fecal microbial markers in colorectal cancer detection. Int J Cancer. 2017;15:141.
- Dimenäs E, Glise H, Hallerbäck B, et al. Quality of life in patients with upper gastrointestinal symptoms. An improved evaluation of treatment regimens? Scand J Gastroenterol. 1993;28:681–687.
- Wiklund IK, Fullerton S, Hawkey CJ, et al. An irritable bowel syndrome-specific symptom questionnaire: development and validation. Scand J Gastroenterol. 2003;38:947–954.
- Shin SJ, Noh CK, Lim SG, et al. Non-steroidal anti-inflammatory drug-induced enteropathy. Intest Res. 2017;15:446–455.
- Moore RA, Derry S, McQuay HJ. Faecal blood loss with aspirin, nonsteroidal anti-inflammatory drugs and cyclo-oxygenase-2 selective inhibitors: systematic review of randomized trials using autologous chromium-labelled erythrocytes. Arthritis Res Ther. 2008;10:R7.
- Poullis A, Foster R, Mendall MA, et al. Proton pump inhibitors are associated with elevation of faecal calprotectin and may affect specificity. Eur J Gastroenterol Hepatol. 2003;15:573–574.
- Lapenna D, de Gioia S, Ciofani G, et al. Antioxidant properties of omeprazole. FEBS Lett. 1996;382:189–192.
- Biswas K, Bandyopadhyay U, Chattopadhyay I, et al. A novel antioxidant and antiapoptotic role of omeprazole to block gastric ulcer through scavenging of hydroxyl radical. J Biol Chem. 2003;278:10993–11001.
- Suzuki M, Nakamura M, Mori M, et al. Lansoprazole inhibits oxygen-derived free radical production from neutrophils activated by Helicobacter pylori. J Clin Gastroenterol. 1995;20:Suppl 2:S93–S96.
- Handa O, Yoshida N, Fujita N, et al. Molecular mechanisms involved in anti-inflammatory effects of proton pump inhibitors. Inflamm Res. 2006;55:476–480.
- Kedika RR, Souza RF, Spechler SJ. Potential anti-inflammatory effects of proton pump inhibitors: a review and discussion of the clinical implications. Dig Dis Sci. 2009;54:2312–2317.
- Kuroda M, Yoshida N, Ichikawa H, et al. Lansoprazole, a proton pump inhibitor, reduces the severity of indomethacin-induced rat enteritis. Int J Mol Med. 2006;17:89–93.
- Ichikawa H, Yoshida N, Takagi T, et al. Lansoprazole ameliorates intestinal mucosal damage induced by ischemia-reperfusion in rats. Wjg. 2004;10:2814–2817.
- Vesper BJ, Jawdi A, Altman KW, et al. The effect of proton pump inhibitors on the human microbiota. Curr Drug Metab. 2009;10:84–89.
- Jackson MA, Goodrich JK, Maxan ME, et al. Proton pump inhibitors alter the composition of the gut microbiota. Gut. 2016;65:749–756.
- Castellani C, Singer G, Kashofer K, et al. The influence of proton pump inhibitors on the fecal microbiome of infants with gastroesophageal reflux-A prospective longitudinal interventional study. Front Cell Infect Microbiol. 2017;7:444.
- Andréasson K, Alrawi Z, Persson A, et al. Intestinal dysbiosis is common in systemic sclerosis and associated with gastrointestinal and extraintestinal features of disease. Arthritis Res Ther. 2016;18:278.
- Hassing RJ, Verbon A, de Visser H, et al. Proton pump inhibitors and gastroenteritis. Eur J Epidemiol. 2016;31:1057–1063.
- Yousefi R, Imani M, Ardestani SK, et al. Human calprotectin: effect of calcium and zinc on its secondary and tertiary structures, and role of pH in its thermal stability. Acta Biochim Biophys Sinica. 2007;39:795–802.
- Montalto M, Gallo A, Ianiro G, et al. Can chronic gastritis cause an increase in fecal calprotectin concentrations? World J Gastroenterol. 2010;16:3406–3410.