Abstract
Objectives
Assessing the experience of screening procedures is crucial for improving the quality and acceptance of colonoscopy in colorectal cancer screening. The aim of the study was to investigate the colonoscopy experience and associated factors among individuals who underwent a colonoscopy in the Screening of Swedish Colons (SCREESCO) study.
Methods
Participants in the Screening of Swedish Colons (SCREESCO; n = 7593) randomized clinical trial (colonoscopy vs. faecal immunochemical test (FIT)) were enrolled. The primary outcome was overall colonoscopy experience measured with a study-specific questionnaire. Secondary endpoints were measured using multiple regression analyses with factors that included sex, randomization group, geographical regions, university hospital, complications, sedation, clean bowel, time to cecum, and presence of polyps or cancer.
Results
A total of 6572 (87%) individuals responded to the questionnaire. The majority was satisfied with the information, care and treatment. Women reported more worry, discomfort and pain, but also better information, care and treatment compared with men. The FIT group was more worried and perceived more discomfort and pain than the colonoscopy group. Type of hospital (geographical region; university hospital vs. not university hospital) was also a significant predictor for the colonoscopy experience.
Conclusions
Although most participants were satisfied with the colonoscopy experience, the study has highlighted areas for improvement. Important factors for colonoscopy experience were gender, randomization group, and type of hospital and therefore crucial to bear in mind when designing screening programs.
Introduction
Colorectal cancer (CRC) screening programs are effective in reducing CRC incidence and CRC mortality [Citation1–4]. However, CRC screening programs are well known to face challenges due to low participation rates [Citation5]. The European Guidelines for Quality Assurance in Colorectal Cancer Screening recommends a participation rate of at least 65% [Citation6]. This rate differs around the world, ranging from 7% to 68%, but rate comparisons may be difficult due to organizational differences [Citation7]. A high quality of the colonoscopy procedure is therefore important. To improve quality of endoscopy services The European Society of Gastrointestinal Endoscopy (ESGE) recommends seven key performance measures for lower gastrointestinal endoscopy: (1) adequacy of bowel preparation; (2) cecal intubation rate; (3) adenoma detection rate; (4) appropriate polypectomy technique; (5) complication rate; (6) patient experience; (7) postpolypectomy surveillance [Citation8]. This paper deals with one of the seven key performance measures: patient experience. To measure patient experience, self-reported questionnaires captures the patient perspective and when acting upon the results, the acceptance of the colonoscopy procedure can improve. Although data, using the European colonoscopy quality investigation (ECQI) questionnaire, showed that only 23% of the 13 included endoscopy units in Sweden measured patient satisfaction outcome [Citation9].
Results from a systematic review found that the laxative bowel preparation, anticipation of pain, feelings of embarrassment and vulnerability, inadequate knowledge, fear of finding cancer, cost and the time required for the procedure, were all factors identified as obstacles to the uptake of CRC screening [Citation10]. In addition, results from a qualitative study by our research group showed that fear, worry about the colonoscopy and awareness of risks with the procedure were important factors, when invited individuals, decided not to attend CRC screening [Citation11]. These results correspond well with findings from the English [Citation12] and the Dutch [Citation13] Bowel Cancer Screening programs. Other factors for the colonoscopy experience are related to the endoscopist, such as the technical skills, manner, and gender, and the nursing staff, such as the explanation of the procedure and the post-procedure discussion [Citation14]. The role of the endoscopy assistant has also been indicated to have an impact on the endoscopy experience in terms of information and communication [Citation15], pain and conscious sedation during the colonoscopy [Citation16], Women, individuals with lower education, and those with intensity of religious practice have a greater wish for an endoscopist with the same gender [Citation17,Citation18]. However, choosing gender of the endoscopist was not considered important in a qualitative study by Nielsen et al. [Citation15], but still, individuals, especially men reported that they felt more embarrassed when the endoscopist was of the opposite gender. Gender is a further important factor for the colonoscopy experience, as women feel more vulnerable [Citation17] and more anxious and [Citation19] report more discomfort and pain [Citation12] compared to men. Women also report higher levels of anxiety related to their screening decision [Citation20], which may impact the colonoscopy experience. Another difference between men and women is the motivation for using conscious sedation during colonoscopy, where women’s motives for conscious sedation are to reduce fears, anxiety, and feelings of vulnerability, whereas men’s motive is to reduce pain [Citation17]. The aim of the present study was to investigate the colonoscopy experience and associated factors among individuals who underwent a colonoscopy in the Screening of Swedish Colons (SCREESCO) study.
Methods
Study design and setting
This was a descriptive and comparative study with a cross-sectional design and included both data from a self-reported questionnaire and clinical data from the ongoing SCREESCO study. The aim of the SCREESCO study was to investigate how CRC screening impact incidence and mortality in CRC. Furthermore, eighteen of the 21 counties of Sweden, including a total of 33 hospitals, participated in the study. The endoscopists in the study had to perform >100 colonoscopies per year and >1000 in total to be certified as experienced by the governor. Individuals from the Swedish Population Register aged 59 to 60-years-old (at time of randomization), were randomized to either colonoscopy (n = 30,000), high sensitive FIT (haemoglobin concentration 10 µg/g of faeces; n = 60,000), or control group. In total, 183,600 randomized individuals currently belong to the control group and had not been asked to participate in screening; however, these individuals are followed through the Swedish Cancer Register and the Causes of Death Register. Since the current study is part of the overall SCREESCO study all participants received information about the study, including benefits and harms related to FIT and colonoscopy method, developed according to guidelines provided by the regional Ethics Review Board. In addition, a leaflet with coloured pictures containing more brief information of the study was provided. Written informed consent for the current study was obtained when they took part in the SCREESCO study.
Participants and procedure
All individuals (n = 7719) randomized to screening who underwent a colonoscopy after randomization or after a positive FIT between 2014 and 2016 (5117 colonoscopies in the colonoscopy group and 2602 colonoscopies in the FIT group) were invited to respond to a study specific questionnaire that assessed their colonoscopy experience. The questionnaire, together with a pre-paid envelope to send it back to the endoscopy unit, was given to each participant directly after the colonoscopy examination, and they were requested to respond within 24 h.
Measures
Since the aim of the study was to measure subjective colonoscopy experience and no Swedish questionnaire was available, a study specific questionnaire was developed inspired by the development of patient reported experience measures (PREM) [Citation21]. The procedure was followed by 4 steps: (1) a literature search was performed to inventory questionnaires measuring colonoscopy experience in other European countries; (2) an item bank relevant to the Swedish context was gathered; (3) a qualitative study with focus group discussions and telephone interviews with the overall aim to investigate CRC screening experience were performed [Citation11], results from the question ‘How did you experience the screening method’ (not published) generated items and were added to the questionnaire; (4) the questionnaire was reviewed by professional expertise (three of the authors, KF, AF, RH, have extensive knowledge in endoscopy).The final questionnaire consisted of 10 questions (Q1–10, ). Nine questions had five response choices ranging from ‘bad’ to ‘very good’ or ‘not at all’ to ‘very much’ and one was a yes/no question. All clinical data were collected from the SCREESCO database.
Table 1. Study-specific questionnaire measuring colonoscopy experience.
Statistical analyses
Individuals who responded to at least one question in the questionnaire were included in the study. Clinical characteristics were presented in proportions by sex and randomization group, and potential differences were tested with the Chi-square test. The answers to the ten questions were included as outcome variables in ten separate multiple linear regression models. Missing data were low, 4% as a maximum. The coding of questions Q4, Q5, Q6 and Q7 were reversed, so that a poorer experience equated with a lower score, same as the other questions (1 = something bad or unpleasant and 5 = something good or not unpleasant).Factors considered to have a potential impact on colonoscopy experience, such as sex, randomization group (direct colonoscopy or FIT colonoscopy), hospital regions (five regions), type of hospital (university hospital, yes or no), complications (yes or no), sedation (deep, e.g., Propofol anaesthesia; mild, e.g., Alfentanil, Diazepam and/or Midazolam; none), clean bowel (yes or no), time to cecum (<10, 10–20, or >20 min), findings of polyps or cancer (yes or no), were entered into the regression models. The binary indicator of a ‘previous colonoscopy’ had 52% missing values; therefore, it was excluded from the regression analysis. The magnitude of the regression coefficients represented the strength of the association between each factor and the outcome variable, while the sign of the regression coefficient indicated whether the association was positive or negative. The size effect was not comparable between questions with five- and two-graded scales. The results from the regression analyses were presented with the regression coefficients, p-values, and 95% confidence intervals. For each model – one for each question – the goodness-of-fit was expressed by the R-square statistic. For all analyses, a p-value <.05 was considered statistically significant. The statistical analyses were performed with Stata version 15 (StataCorp, College Station, TX).
Ethical approval
Trial registration: Colonoscopy and FIT as Colorectal Cancer Screening Test in the Average Risk Population ID NCT02078804 Protocol ID 2012/2058-31/3. First received: 11 February 2014. The study was approved (Dnr 2012/2058-31/3; Dnr 2015/2058-31/3) by the regional Ethics Review Board at Karolinska Institutet, Stockholm, Sweden.
Results
A total of 6,572(85%) individuals responded to the questionnaire. Of those, 63% were in the colonoscopy group and 37% in the FIT group. Clinical characteristics, by sex and randomization group are shown in . Men and women showed the following significant differences: men were sedated to a lesser extent, had more findings of polyps or cancer, and shorter procedures (i.e., a shorter time to cecum).Primary outcomes showed that the majority was satisfied (ratings, good/very good) with the information about the procedure and about how they were cared and treated for during the procedure (97, 99, and 99%, respectively). 96% had taken at least half a day or more off work, 94% found the examination worth the effort, and 86% were willing to be re-examined in the future. shows the proportion of participants reporting ‘much’/‘very much’ to Q4–7 in the study specific questionnaire.
Figure 1. Proportions (%) of individuals, divided by gender and randomization group, who reported ‘much’/‘very much’ to questions 4–7 in the study specific questionnaire.
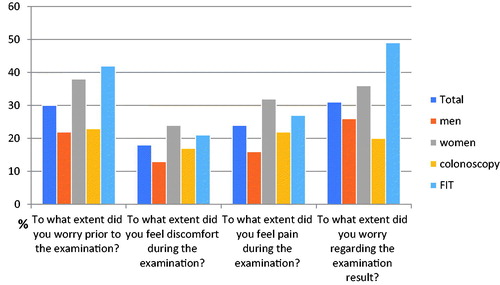
Table 2. Clinical characteristics presented by sex and randomization group.
All factors included in the multiple regression analyses are summarized in . Women felt significantly better informed about the colonoscopy procedure and perceived themselves as better treated and cared for during the colonoscopy compared with men. Conversely, women were more worried before the examination and about the result, and they perceived more discomfort and pain when compared with men. Men did take time off from work and were more willing to be re-examined in the future when compared with women.
Table 3. Regression models with the 10 questions in the study specific questionnaire measuring colonoscopy experience as dependent variables.
Table 4. Regression models with the 10 questions in the study specific questionnaire measuring colonoscopy experience as dependent variables.
Table 5. Regression models with the 10 questions in the study specific questionnaire measuring colonoscopy experience as dependent variables.
Participants in the FIT group were significantly more worried before the examination and about the result, and they perceived more discomfort and pain during the examination when compared with participants in the direct colonoscopy group.
Geographical region had an impact on how well informed the participants felt about the colonoscopy and if participants’ experienced discomfort and pain during the examination. Region was also a predictor of whether participants had to take time off work and whether they were willing to be re-examined in the future. Participants examined at hospitals other than university hospitals perceived themselves as significantly better informed, better cared, and better treated for during the colonoscopy. Participants examined at hospitals other than university hospitals were significantly less worried before the examination and for the result and perceived less discomfort and pain when compared with participants examined at university hospitals. In addition, participants examined at other hospitals than university hospitals found the examination more worth the effort and a larger proportion of participants could consider being re-examined.
Discussion
To our knowledge, this is the first study to investigate colonoscopy experience in individuals randomized to either FIT or colonoscopy in a CRC screening context. Important factors for colonoscopy experience were gender, randomization group, region and type of hospital. The majority of the participants were satisfied with the information given before the procedure and with how they were treated and cared for during the examination; this is in line with the results from the English Bowel Cancer Screening program [Citation13]. Even though a vast majority had to take at least half a day or more off work, the participants found it worth the effort to go through the colonoscopy and could imagine being re-examined in the future in order to reduce their risk for CRC.
Impact by gender
Women reported more colonoscopy-related worry, discomfort and pain when compared with men. This may be related to gender differences in attitudes, as previously reported by Ritvo et al. [Citation22], who described that women, independent of screening modality, expressed bodily intrusive thoughts and anxiety about the perforation related to CRC screening. By contrast, men expressed avoidant thoughts and viewed CRC screening as unnecessary health care. Interestingly though, in the current study, women reported they were better informed, and better treated and cared for compared with men. The reason for this could be related to factors not included in this study, such as differences in attitudes regarding how much information is needed [Citation23] or educational level and level of health literacy [Citation24]. The difference in how women and men perceived their care and treatment might also reflect how health care professionals treat individuals differently depending on group affiliation, such as ethnicity and gender [Citation25]. The treatment of women and men is known to differ depending on their gender, especially in pain management [Citation26]. In the current study, a higher proportion of women underwent the procedure under conscious sedation than men. Further studies are needed to determine if this is a result of a different motivation for conscious sedation between men and women [Citation17], if women are offered and encouraged more often to take conscious sedation by the endoscopist and endoscopy assistant, or if women request conscious sedation more often than men.
Impact of randomization group
An important factor noticed in the FIT group was higher scores for worry, both before the examination and for the result. Fear of finding cancer [Citation10] because of knowledge of having blood in the stool and having bowel symptoms [Citation26] may be a source of worry before the examination and needs to be addressed. Seeking the support of family and friends was one way of managing the waiting time for individuals with positive FIT in a Danish CRC screening program [Citation27]; however, only a few participants approached health care professionals for support in the current study. Confusing instructions have previously been reported as another factor that has an impact on anxiety about the result [Citation28] and points out the importance of how the result is delivered, especially since conscious sedation often is used during colonoscopy. In the current study the information of the colonoscopy procedure was given according to clinical practice at each hospital, therefore we do not now how participants were informed after the procedure. In addition, about 50% of the participants had conscious sedation, this together may impact on the result. Interventions, such as providing written information about the result of the colonoscopy, instructions about possible post-colonoscopy symptoms, and explanation of how the pathology result will be delivered, may decrease worry while the patient awaits the result. The ESGE recommendation to obtain informed consent prior to the colonoscopy procedure [Citation29] may be one way to secure that patients understand given information. In Swedish health care, thought, there is no such tradition as signing informed consent before receiving care. However, written and verbal information is given including benefits and risks.
Impact of geographical region and type of hospital
Other important factors that determined how well the participants felt about the procedure were the geographical regions and if the examination took place at a university hospital. Since this is a study, the written information was uniform for all hospitals; however, the verbal information delivered when the participant called to confirm the appointment was given according to standard practice at each hospital. The written information has been evaluated in a previous study, with positive results [Citation30], but the quality of the verbal information may differ between hospitals and can therefore impact the result. Furthermore, about 100 different endoscopists (of whom 10% are nurses) and 33 hospitals are participating in the SCREESCO study. As such, differences between the individual endoscopists may also reflect the results of the current study, where region and type of hospital had an impact on perceived discomfort and pain. This could reflect factors at an individual level, since the skills and manner of the endoscopist are reported to impact colonoscopy experience [Citation14,Citation16], or it could be related to the organization of the hospital or the working environment. The skills of the nursing staff and endoscopy assistants are also known to play a role in the colonoscopy experience [Citation14,Citation16], but these data are lacking for the SCREESCO study. According to ESGE recommendation [Citation29], the leadership roles and responsibilities are crucial for staffing to understand what is expected as well as introduction and training of staff. The results, in the current study, indicate the importance of measuring endoscopy services performance in a structured way, to achieve colonoscopy quality. To be able to do that, a Swedish national colonoscopy register, aiming at measuring colonoscopy quality including patient experience is currently under construction.
Strengths
This is one of the largest studies of its kind with a sample of participants who underwent a colonoscopy as a primary or secondary CRC screening method. In addition, the sample was drawn from the whole country encompassing both urban and rural areas. Another strength is the use of both self-reported and register data that enables extensive analyses. Finally, the high response rate that usually is a problem when using self-reported data strengthens the study.
Limitations
In this study we considered multiple outcomes, which entailed testing multiple hypotheses. Caution is therefore warranted when interpreting the significance of the tests, as the probability of an overall type I error might be increased. The explanatory value of the ten regression analyses is relatively low, although the regression analysis for ‘worry before the examination’ (Q4), ‘discomfort during colonoscopy’ (Q5), ‘pain during colonoscopy’ (Q6) and ‘worry about the result’ (Q7) may explain some of the variance of outcome variable better than the other regression analyses. This means that additional factors not captured in our questionnaire may be important for the colonoscopy experience, for example, the bowel preparation [Citation13,Citation31], patients’ expectations, the ability to choose appointment and/or examination methods, embarrassment [Citation15,Citation31], environmental factors at the endoscopy unit as well as factors related to the endoscopist [Citation13] and endoscopy assistant [Citation19]. The generalizability to other age groups may not be relevant since all participants were 60 years, although the age range is not that wide in CRC screening. In addition, about half of the participants had sedation during the procedure, which could affect patient recall of their experience.
Conclusions
This study adds to the understanding of how colonoscopy is experienced in a CRC screening sample containing participants randomized both to colonoscopy and to FIT. Most of the participants were satisfied with the information given before the procedure and with how they were treated and cared for during the examination. Important factors for colonoscopy experience were gender, randomization group, and type of hospital and therefore crucial to bear in mind when designing screening programs.
Acknowledgments
The authors thank all the survey participants and study coordinator Eva Berglund.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Mandel JS, Church TR, Bond JH, et al. The effect of fecal occult-blood screening on the incidence of colorectal cancer. N Engl J Med. 2000;343(22):1603–1607.
- Hewitson P, Glasziou P, Watson E, et al. Cochrane Systematic Review of colorectal cancer screening using the fecal occult blood test (hemoccult): an update. Am J Gastroenterol. 2008;103(6):1541–1549.
- Holme O, Loberg M, Kalager M, et al. Effect of flexible sigmoidoscopy screening on colorectal cancer incidence and mortality: a randomized clinical trial. JAMA. 2014;312(6):606–615.
- Atkin W, Wooldrage K, Parkin DM, et al. Long term effects of once-only flexible sigmoidoscopy screening after 17 years of follow-up: the UK flexible sigmoidoscopy screening randomised controlled trial. Lancet. 2017;389(10076):1299–1311.
- Ponti A, Anttila A, Ronco G, et al. Cancer screening in the European Union. Brussels (Belgium): European Commission; 2017. (Report on the implementation of the Council Recommendation on cancer screening, second report).
- Karsa L, Patnick J, Segnan N. European guidelines for quality assurance in colorectal cancer screening and diagnosis. first edition executive summary. Endoscopy. 2012;44(S03):SE1–SE8.
- Klabunde C, Blom J, Bulliard J-L, et al. Participation rates for organized colorectal cancer screening programmes: an international comparison. J Med Screen. 2015;22(3):119–126.
- Kaminski MF, Thomas-Gibson S, Bugajski M, et al. Performance measures for lower gastrointestinal endoscopy: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy. 2017;49(4):378–397.
- Toth E, Agrawal A, Amaro P, et al. Recording of European society of gastrointestinal endoscopy (ESGE) performance measures: observation from the European colonoscopy quality investigation (ECQI) questionnaire. Endoscopy. 2019;51(04):S134.
- McLachlan SA, Clements A, Austoker J. Patients’ experiences and reported barriers to colonoscopy in the screening context-a systematic review of the literature. Patient Educ Couns. 2012;86(2):137–146.
- Fritzell K, Stake Nilsson K, Jervaeus A, et al. The importance of people’s values and preferences for colorectal cancer screening participation. Eur J Public Health. 2017;27(6):1079–1084.
- Ghanouni A, Plumb A, Hewitson P, et al. Patients’ experience of colonoscopy in the English Bowel Cancer Screening Programme. Endoscopy. 2016;48(03):232–240.
- Denters MJ, Deutekom M, Bossuyt PM, et al. Patient burden of colonoscopy after positive fecal immunochemical testing for colorectal cancer screening. Endoscopy. 2013;45(5):342–349.
- McEntire J, Sahota J, Hydes T, et al. An evaluation of patient attitudes to colonoscopy and the importance of endoscopist interaction and the endoscopy environment to satisfaction and value. Scand J Gastroenterol. 2013;48(3):366–373.
- Neilson LJ, Patterson J, von Wagner C, et al. Patient experience of gastrointestinal endoscopy: informing the development of the Newcastle ENDOPREM™. Frontline Gastroenterol. 2020;11(3):209–217.
- Holme Ø, Pedersen IB, Medhus AW, et al. Endoscopy assistants influence the quality of colonoscopy. Endoscopy. 2018;50(9):871–877.
- Elphick DA, Donnelly MT, Smith KS, et al. Factors associated with abdominal discomfort during colonoscopy: a prospective analysis. Eur J Gastroenterol Hepatol. 2009;21(9):1076–1082.
- Lahat A, Assouline-Dayan Y, Katz HL, et al. The preference for an endoscopist specific sex: a link between ethnic origin, religious belief, socioeconomic status, and procedure type. Patient Prefer Adherence. 2013;7:897–903.
- Bensusan BI, Martín PH, Álvarez VA. Prospective study of anxiety in patients undergoing an outpatient colonoscopy. Rev Esp Enferm Dig. 2016;108(12):765–769.
- Wangmar J, von Vogelsang AC, Hultcrantz R, et al. Are anxiety levels associated with the decision to participate in a Swedish colorectal cancer screening program? A nationwide cross-sectional study. BMJ Open. 2018;8(12):e025109.
- Fernandes S, Fond G, Zendjidjian X, et al. The Patient-Reported Experience Measure for Improving qUality of Care in Mental Health (PREMIUM) Project in France: study protocol for the development and implementation strategy. Patient Prefer Adherence. 2019;13(13):165–177.
- Ritvo P, Myers RE, Paszat L, et al. Gender differences in attitudes impeding colorectal cancer screening. BMC Public Health. 2013;13:500.
- Friedemann-Sánchez G, Griffin JM, Partin MR. Gender differences in colorectal cancer screening barriers and information needs. Health Expect. 2007;10(2):148–170.
- van der Heide I, Uiters E, Jantine Schuit A, et al. Health literacy and informed decision making regarding colorectal cancer screening: a systematic review. Eur J Public Health. 2015;25(4):575–582.
- Wandner LD, Heft MW, Lok BC, et al. The impact of patients’ gender, race, and age on health care professionals’ pain management decisions: an online survey using virtual human technology. Int J Nurs Stud. 2014;51(5):726–733.
- Samulowitz A, Gremyr I, Eriksson E, et al. “Brave Men” and “Emotional Women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag. 2018;2018:1–14.
- Kirkegaard P, Edwards A, Bach Larsen M, et al. Waiting for diagnostic colonoscopy: a qualitative exploration of screening participants’ experiences in a FIT-based colorectal cancer screening program. Patient Prefer Adherence. 2018;12:845–852.
- Shafer LA, Walker JR, Waldman C, et al. Factors associated with anxiety about colonoscopy: the preparation, the procedure, and the anticipated findings. Dig Dis Sci. 2018;63(3):610–618.
- Valori R, Cortas G, de Lange T, et al. Performance measures for endoscopy services: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy. 2018;50(12):1186–1204.
- Wangmar J, Jervaeus A, Fritzell K, et al. Health literacy levels and views about being invited to a colorectal cancer screening program. Acta Oncol. 2018;57(6):743–749.
- Gareen IF, Siewert B, Vanness DJ, et al. Patient willingness for repeat screening and preference for cT colonography and optical colonoscopy in Acrin 6664: the national cT colonography trial. Patient Preference and Adherence. 2015;9:1043–1051.
