Abstract
Background and aims
Every fifth patient with ulcerative colitis (UC) experiences severe acute flare at some point in the course of the disease. Corticosteroids (Cs) remain the treatment of choice in acute flare. Data on the efficacy of first intravenous Cs in the long-term prognosis of UC are scarce and were investigated here.
Materials and methods
All episodes of patients with acute UC admitted to Tampere University Hospital and treated with intravenous Cs between January 2007 and January 2016 were identified from patient records and reviewed. The risks for colectomy and for continuous use of Cs were evaluated. Predictive factors were analysed.
Results
The study comprised 217 patients of whom 184 (85%) responded to intravenous Cs at index flare. Of the 33 non-responders, 31 (94%) were treated with intravenous cyclosporine A and 28 responded. Five (2.3%) patients needed emergency colectomy. Twenty-six (12%) patients underwent colectomy within 1 year of index flare. Overall colectomy rate was 56 (26%) during follow-up (median 7.5 years, range 0.1–10.5). Six months after index flare 66 (30%) patients were still on steroids. In this series 149 (69%) required further Cstherapy and 104 (48%) needed rehospitalization for new flare at some point during follow-up. Overall 155 patients were treated with thiopurines, of whom 72% within the first year after admission. A total of 36 patients had infliximab as a first-line biological treatment, nine needed second-line therapy with adalimumab or vedolizumab after infliximab failed.
Conclusion
Although intravenous Cs were efficient in inducing clinical response in patients with severe acute UC, only one fifth maintained remission in the long term. Two-thirds of patients required further Cs and the overall colectomy rate remained at 26%. High relapse rate indicates the need for closer monitoring of these patients. Enhancement of maintenance therapy should be considered at early stage after acute flare.
Introduction
Ulcerative colitis (UC) is a chronic inflammatory bowel disease, which often follows a remitting-relapsing course. Acute severe UC (ASUC) affects 15-25% of patients and in 30–40% of cases it appears at the onset of the disease [Citation1–3]. The condition may be life-threatening and require hospital admission. Corticosteroids (Cs) remain the treatment of choice in acute flare [Citation4].
Although the early outcomes of UC after first course of Cs are well known, data on long-term disease evolution in patients responding to this treatment are scarce. The aim of this study was to evaluate short- and long-term clinical outcomes after the first intravenous Cs treatment. Further, the outcomes after failed previous oral course of Cs or direct course of intravenous Cs were investigated and the outcomes in patients with disease onset at index flare and in those with UC diagnosed prior to the flare were evaluated.
Materials and methods
All patients aged 16 years or over and admitted for UC flare between January 2007 and January 2016 were identified from the electronic patient records. The inclusion criteria were first course of intravenous Cs on the hospital ward and follow-up for at least 6 months after hospitalization or until colectomy. Patients were followed-up from the date of index flare until colectomy, death, or the end of the observation period.
Data collected included epidemiological (gender, age at index flare, smoking status), clinical (UC duration, extent of the disease, prior Cs usage, disease severity, laboratory results at index flare) and treatment data (occurrence of new flares, need for further Cs therapy; Cyclosporine A (CyA), thiopurines, biologics or colectomy during follow-up).
The diagnosis of UC was made on basis of clinical history, symptoms, endoscopic and histological features. Disease extent was categorized by the Montreal classification and the severity of the flare was assessed by Mayo scoring system based on clinical and endoscopic characteristics. ASUC was characterized by more than six bloody stools/day along with any of the following: tachycardia, elevated temperature, anemia and/or ESR >30 mm/h (Truelove and Witt´s criteria) [Citation5].
Alleviation of UC was defined as clinical response to intravenous Cs with no need for colectomy or rescue therapy at the same hospitalization as the index flare. Relapse was defined as requiring further Cs treatment, rehospitalization, rescue-therapy, or colectomy later in follow-up.
Categorical variables were expressed as numbers and percentages. Quantitative data were expressed as medians and minimum and maximum values. Kaplan-Meier curves were used to display the time from index flare to colectomy. A p-value of <.05 was considered statistically significant. P-values were two-sided. Statistical analyses were performed using SPSS version 25.0. Due to the register-based nature of this study no ethical committee approval was required.
Results
A total of 217 patients were included, the median follow-up was 7.5 years (range 0.1–10.5 years). Baseline characteristics are shown in . Of the patients 130 (60%) had been diagnosed with UC 3 months prior to index flare, median time from diagnosis to index flare being 21 days (range 0–36 years).
Table 1. Demographic and clinical characteristics of 217 patients with ulcerative colitis treated with first course of intravenous corticosteroids.
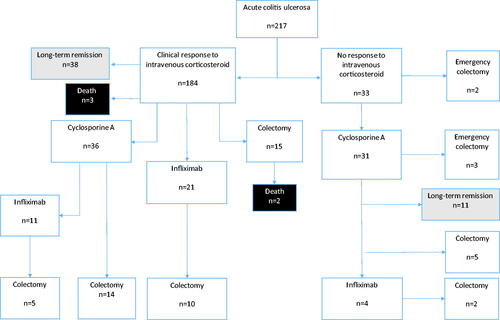
Altogether 184 (85%) of patients had clinical response to intravenous Cs () of whom 38 (21%) had long-term response with no need for further Cs, rehospitalization or colectomy. Non-responders were treated with CyA and 90%responded. A total of 36 patients initially responding to intravenous Cs needed CyA later due to a new flare of ASUC.
Figure 1. Outcome of the 217 patients with ulcerative colitis treated with their first course of intravenous corticosteroids. Data expressed as absolute frequencies.
Six months after index flare 66 (30%) patients were still on steroids. A total of 149 (69%) patients required another course of Cs at follow-up and 104 (48%) patients required rehospitalization due to a relapse. In this series 48 (22%) and 87 (40%) patients were re-admitted to hospital within 1 and 3 months of index flare, respectively. The median time for rehospitalization was 5 months (range 0.7–84 months).
Overall, 155 (71%) patients were treated with thiopurines, of whom 72% within the first year of admission. At some point during follow-up 36 (17%) patients were given infliximab as a first-line biological treatment and nine of these patients needed second-line therapy with adalimumab or vedolizumab after Infliximab failed.
Of the 33 nonresponders, five (2.3%) needed emergency colectomy, two immediately and three after rescue therapy with CyA had failed. Within one, three, and 12 months after index flare six (2.7%), 11 (5%) and 26 (12%) of patients were operated on. A total of 56 patients in our series underwent colectomy (). Five patients died during follow-up, none of the deaths were UC related.
Table 2. Clinical characteristics and outcomes of 217 patients during follow-up.
The comparison of patients responding to first intravenous Cs and patients failing to derive benefit from treatment is shown in . Sex, age, extent of UC or laboratory results at admission on index flare did not predict the clinical outcome. Endoscopic and clinical severity of the disease were significant predictors for the need for rescue therapy and colectomy. Prior failure of treatment with oral Cs had no significant effect on the clinical outcome.
Table 3. Predictors of response to first course of intravenous corticosteroid in 217 patients.
In this series 90% of patients with the onset of UC at index flare responded to intravenous Cs, a significant difference from the 81% of patients with the disease diagnosed prior to admission. Overall, 32% of the patients with UC diagnosed prior to index flare were operated on, a significant difference compared to the 18% colectomy rate of patients with no prior history of UC (p = .015). At follow-up, when evaluating the need for Cs, rehospitalization or biological treatments there was no significant difference between these groups.
Discussion
Despite the good primary response to intravenous Cs, a large proportion of patients relapsed during long-term follow-up. Almost 70% of patients needed a new course of Cs at some point during follow-up and 51% were taking thiopurines within 1 year of index flare. Overall colectomy rate was high, up to 26% in this series; the rate at index flare was 2.3% and 12% at 1-year follow-up.
A population-based study from the USA reported emergency colectomy rates of up to 16% after the first course of oral Cs for ASUC. However, no rescue therapies or immunosuppressive treatments were used in that series [Citation6]. Since that high colectomy rates have encouraged clinicians to search for rescue therapies. Cyclosporine A (CyA) and infliximab have emerged as effective colon rescue therapy and prior data suggest that they both are equally effective in steroid-refractory ASUC, at least in short-term use [Citation7,Citation8]. However, these patients have been shown to have a high risk of continuing symptoms and need for colectomy within a few months of index flare [Citation9,Citation10]. A systematic review by Turner et al. 2007 showed consistent colectomy rates of 27% in ASUC during the three decades from 1974 to 2004 despite the increased use of CyA [Citation11]. The short-term colectomy rates in our series were significantly lower than those reported in earlier studies. This difference may be due to patient selection and differences in treatment practices.
In our series 94% of the non-responders received CyA as a rescue therapy and 90% of these patients responded to treatment. Although the short-time outcome was good, half of the patients relapsed during follow-up and a quarter were operated on within 5 years of treatment. However, the long-term outcome of patients in our series initially responding to rescue therapy was significantly better than the respective 58% and 88% colectomy rates in 7-year follow-up reported in earlier studies by Campbell et al. 2005 and Moskovitz et al. 2006 [Citation12,Citation13].
A Swedish retrospective population-based study reported long-term colectomy rates of up to 64% in 10-year follow-up in patients with ASUC [Citation14]. That study was published prior to the systematic use of rescue therapies and the overall use of immunosuppressive treatments in this series was low. Dinesen et al. evaluated a large cohort with 750 patients and reported overall colectomy rate of 12% in 12.7-year follow-up. The colectomy among patients with no flares differed substantially from that among patients with several flares during follow-up (3-40%) [Citation2]. A recent multi-centre study of pediatric patients admitted with ASUC reported a colectomy rate of 36.4% at 5-year follow-up [Citation15]. The colectomy rate of 26% in our series was lower than that reported in those studies. The better outcome may be due to the use of biological agents as was shown in a recent study by Salameh et al. 2019 reporting a colectomy-free survival of 91% in ASUC within 5-year follow-up [Citation16].
Although the role of Cs is well established, earlier research shows that 30% of patients do not respond to treatment and that half of those responding to the first course of Cs will relapse in the following year [Citation6,Citation17]. Frequent use of Cs in the first year after diagnosis is a strong predictor of subsequent colectomy [Citation18]. In the present study we found a high response rate of 85% among UC patients with acute severe flare. However, only 21% of these patients stayed in long-term remission with no need for further Cs, rehospitalization or colectomy. Despite the overall good response to treatment at index flare, one-third of the patients were on steroids 6 months after treatment. Almost 70% of all patients needed further Cs therapy at follow-up and half of the patients were readmitted to hospital due to a new flare. Of all patients, 71% required immunosuppressive therapy with thiopurines and 72% of these treatments were initiated within 1 year of the index flare. High relapse rate and need for immunosuppressive treatment in the short term indicate the need for earlier enhancement of maintenance therapy after ASUC despite the good short-term response to Cs.
Severity of disease on admission was related to the outcome, as also shown in previous studies [Citation2]. Neither the gender or age of the patients nor the extent of UC affected the clinical outcome in this study. Six (2.8%) patients had Clostridium Difficile infection at index flare, but this did not predict response to Cs and the overall number of Cl. difficile infections was low in our series. Patients diagnosed at index flare had a significantly better outcome than patients with pre-existing disease. This helps to explain the difference in colectomy rates when comparing patients using thiopurine as maintenance therapy before and after index flare. Result is understandable considering varying duration and course of the disease prior to the index flare.
In the study by Llao et al. 2016, failure to respond to oral Cs predicted the need for rescue therapy and colectomy [Citation19]. In our series, 80% of the patients who failed to respond to oral Cs responded to intravenous Cs. This is in line with a study by Jeon et al. 2013 [Citation20]. Resistance to Cs is a known phenomenon and very variable sensitivity to Cs is observed in IBD patients [Citation21]. Our result implies that intravenous Cs can be administered after a preceding failure to respond to oral Cs.
This series is a single-centre study of the long-term clinical outcome of patients admitted for ASUC in the biological era. The number of patients and duration of the follow-up period are comparable to those reported in earlier studies. The limitations of this study are due to the register-based nature and reliance on computerized retrospective data.
In conclusion, although 85% of patients responded to the first intravenous Cs, the need for further Cs, rehospitalization and colectomy remains high in the long term. The high relapse rate indicates a need for closer monitoring of these patients and for earlier assessment of the adequacy of maintenance therapy after hospitalization for ASUC. However, despite emerging treatments surgery still plays a key role in the treatment of ASUC.
Disclosure statement
HE reports receiving congress and travel fees from Abbvie, Takeda, Pfizer, MSD. TI has received speaker fees from Tillotts Pharma and consulting fees from Janssen-Cilag, Pfizer and Takeda. AJ has received speaker fees and travel support from Abbvie, Ferring, Janssen-Cilag, MSD, Pfizer, Takeda, and Tillots Pharma. HH and PC have nothing to declare. PO reports receiving congress and travel fees from Gilead, Ferring, Janssen-Cilag, Pfizer and Tillots. The authors alone are responsible for the content and writing of the paper.
References
- Hindryckx P, Jairath V, D'Haens G. Acute severe ulcerative colitis: from pathophysiology to clinical management. Nat Rev Gastroenterol Hepatol. 2016;13(11):654–664.
- Dinesen LC, Walsh AJ, Protic MN, et al. The pattern and outcome of acute severe colitis. J Crohns Colitis. 2010;4(4):431–437.
- Fornaro R, Caratto M, Barbruni G, et al. Surgical and medical treatment in patients with acute severe ulcerative colitis. J Dig Dis. 2015;16(10):558–567.
- Harbord M, Eliakim R, Bettenworth D, European Crohn’s and Colitis Organisation [ECCO], et al. Third european evidence-based consensus on diagnosis and management of ulcerative colitis. part 2: Current management. J Crohns Colitis. 2017;11(7):769–784.
- Dignass A, Eliakim R, Magro F, et al. Second european evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: Definitions and diagnosis. J Crohns Colitis. 2012;6(10):965–990.
- Faubion WA, Jr, Loftus EV, Jr, Harmsen WS, et al. The natural history of corticosteroid therapy for inflammatory bowel disease: a population-based study. Gastroenterology. 2001;121(2):255–260.
- Duijvis NW, Ten Hove AS, Ponsioen CI, et al. Similar short- and long-term colectomy rates with ciclosporin and infliximab treatment in hospitalised ulcerative colitis patients. ECCOJC. 2016;10(7):821–827.
- Narula N, Marshall JK, Colombel JF, et al. Systematic review and meta-analysis: Infliximab or cyclosporine as rescue therapy in patients with severe ulcerative colitis refractory to steroids. Am J Gastroenterol. 2016;111(4):477–491.
- Yoon JY, Cheon JH, Park JJ, et al. Clinical outcomes and factors for response prediction after the first course of corticosteroid therapy in patients with active ulcerative colitis. J Gastroenterol Hepatol. 2011;26(7):1114–1122.
- Meyers S, Lerer PK, Feuer EJ, et al. Predicting the outcome of corticoid therapy for acute ulcerative colitis. results of a prospective, randomized, double-blind clinical trial. J Clin Gastroenterol. 1987;9(1):50–54.
- Turner D, Walsh CM, Steinhart AH, et al. Response to corticosteroids in severe ulcerative colitis: A systematic review of the literature and a meta-regression. Clin Gastroenterol Hepatol. 2007;5(1):103–110.
- Campbell S, Travis S, Jewell D. Ciclosporin use in acute ulcerative colitis: a long-term experience. Eur J Gastroenterol Hepatol. 2005;17(1):79–84.
- Moskovitz DN, Van Assche G, Maenhout B, et al. Incidence of colectomy during long-term follow-up after cyclosporine-induced remission of severe ulcerative colitis. Clin Gastroenterol Hepatol. 2006;4(6):760–765.
- Gustavsson A, Halfvarson J, Magnuson A, et al. Long-term colectomy rate after intensive intravenous corticosteroid therapy for ulcerative colitis prior to the immunosuppressive treatment era. Am J Gastroenterol. 2007;102(11):2513–2519.
- Krauthammer A, Tzivinikos C, Assa A, et al. Long-term outcomes of paediatric patients admitted with acute severe colitis- A multicentre study from the paediatric IBD porto group of ESPGHAN. J Crohns Colitis. 2019;13(12):1518–1526.
- Salameh R, Kirchgesner J, Allez M, et al. Long-term outcome of patients with acute severe ulcerative colitis responding to intravenous steroids. Aliment Pharmacol Ther. 2020;51(11):1096–1104.
- Garcia-Planella E, Mañosa M, Van Domselaar M, et al. Long-term outcome of ulcerative colitis in patients who achieve clinical remission with a first course of corticosteroids. Dig Liver Dis. 2012;44(3):206–210.
- Targownik LE, Nugent Z, Singh H, et al. Prevalence of and outcomes associated with corticosteroid prescription in inflammatory bowel disease. Inflamm Bowel Dis. 2014;20(4):622–630.
- Llao J, Naves JE, Ruiz-Cerulla A, et al. Improved outcome of acute severe ulcerative colitis while using early predictors of corticosteroid failure and rescue therapies. Dig Liver Dis. 2016;48(6):608–612.
- Jeon HH, Lee HJ, Jang HW, et al. Clinical outcomes and predictive factors in oral corticosteroid-refractory active ulcerative colitis. WJG. 2013;19(2):265–273.
- Sidoroff M, Kolho KL. Glucocorticoid sensitivity in inflammatory bowel disease. Ann Med. 2012;44(6):578–587.
