Abstract
Background and aims
Obesity with type-2 diabetes is a global challenge. Lifestyle interventions have limited effect for most patients. Bariatric surgery is highly effective, but resource-demanding, invasive and associated with serious complications. Recently, a new intragastric balloon was introduced, not requiring endoscopy for placement or removal (Elipse™, Allurion Inc., Natick, MA). The balloon is swallowed in a capsule and filled with water once in the stomach. The balloon self-deflates after 4 months and is naturally excreted. The present trial investigated balloon feasibility, safety and efficacy in patients with obesity and type-2 diabetes.
Patients and methods
We treated 19 patients, with type-2 diabetes and body mass index (BMI) of 30.0–39.9 kg/m2 at two Norwegian centers with the Elipse balloon. Patient follow-up during balloon treatment mimicked real-world clinical practice, including dietary plan and outpatient visits. The primary efficacy endpoints were total body weight loss (TBWL) and HbA1c at weeks 16 and 52.
Results
All patients underwent balloon insertion uneventfully as out-patients. Mean TBWL and HbA1c reduction after 16 and 52 weeks of balloon insertion was 3.9% (95%CI 2.1–5.7) and 0.8% (95%CI 1.9–3.5); and 7 (95%CI 4–10), and 1 (95%CI −6 to 9) mmol/mol, respectively. Adverse events occurred in two patients (10.5%): one developed gastric outlet obstruction, managed by endoscopic balloon removal; the other excessive vomiting and dehydration, managed conservatively.
Conclusions
This first Scandinavian real-world clinical trial with a new minimally invasive intragastric balloon system demonstrated good feasibility, but did not confirm expected efficacy for weight loss and diabetes control.
Introduction
Obesity and diabetes are rapidly increasing global challenges [Citation1–3]. Weight reduction and diabetes control by diet, physical activity, and behavior modification, show modest results at best [Citation4]. Bariatric surgery is currently the most effective method to reduce the burden of obesity and diabetes, but is resource-demanding and invasive, and carries significant adverse events and long-term health risks [Citation5–8]. Despite some advancement in drug therapy [Citation9], the large group of patients with obesity class 1 or 2 (body mass index (BMI) 30–39.9 kg/m2) and type 2 diabetes urgently needs therapies which are more effective than lifestyle intervention but less invasive than surgery [Citation10].
Intragastric balloon therapy has been proposed as a less invasive approach to weight loss in patients with obesity. Such therapy has been shown to result in significant weight loss [Citation11]. Balloon therapy increases satiety and reduces hunger by gastric space occupation, distension of the gastric walls and delayed gastric emptying. The application of intragastric balloons for weight loss, however, has been hampered by the need for gastroscopy for both insertion and removal of the balloon, which is resource-demanding, time-consuming, and burdensome for patients.
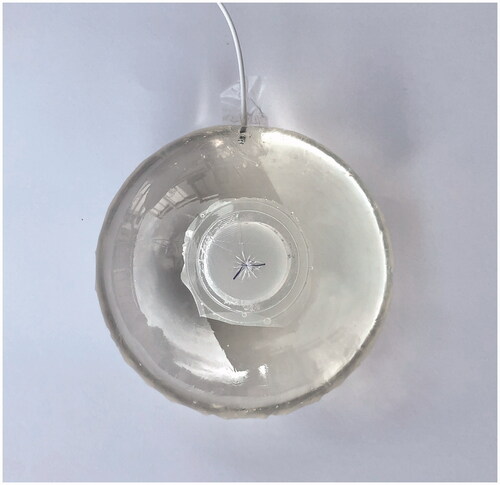
Recently, a novel intragastric balloon system which does not require endoscopy or anesthesia for placement or removal has been developed (Elipse™ intra gastric balloon (Allurion Inc, Natick, MA)). The balloon is contained in a capsule, which can be swallowed, and connected to a catheter (). Once in the stomach, the capsule dissolves, and the balloon is filled with 550 mL water through the catheter (). The catheter is dislodged from the balloon, after filling is completed, and withdrawn through the patient’s mouth. After 16 weeks, a degradable filament breaks down and opens a valve to release the fluid from the balloon. Subsequently, the empty balloon transits the gastrointestinal tract and is excreted naturally.
Figure 2. The balloon is filled through a catheter which can subsequently be dislodged. A self-opening valve will empty the balloon after 16 weeks.
Recent case series in selected patients at specialized centers have shown favorable safety and efficacy of the Elipse™ balloon for obesity treatment [Citation12–19], with mean total body weight loss (TBWL) of 12%, and few adverse events [Citation20]. There are limited data on the real-world performance of the new balloon system in patients with obesity and type 2 diabetes receiving standard follow-up based on current guidelines [Citation21,Citation22].
We performed a clinical pilot trial at two Norwegian centers treating obesity to assess real-life safety, feasibility and efficacy of the new balloon system for short-term (16 weeks) and long-term (52 weeks) weight loss. This pilot trial was conducted to inform a planned randomized trial comparing the new balloon system with bariatric surgery.
Patients and methods
Study design and aim
The study was a single-arm feasibility pilot study, intended to precede a randomized controlled trial comparing the Elipse™ balloon with laparoscopic bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass) in patients with type 2 diabetes and BMI of 30.0–39.9 kg/m2. The planned number of patients was twenty; ten at each of the two participating public centers treating obesity; Oslo University Hospital and Vestfold Hospital in Tønsberg, respectively.
The primary aims of the pilot study were to test feasibility of Elipse™ balloon treatment and study infrastructure, and assess safety and efficacy with the balloon, in addition to guide sample size calculations of the planned randomized trial. The primary efficacy endpoints were TBWL and HbA1c at 16 and 52 weeks after balloon insertion.
Patients
Men and women aged 18 years or older with BMI ≥30 and ≤40 kg/m2 and a diagnosis of type 2 diabetes, referred for obesity treatment to one of the participating centers during the study period without predefined exclusion criteria () were eligible for the trial. Women in childbearing age were required to document a negative pregnancy test.
Table 1. Exclusion criteria.
Balloon intervention
The Elipse™ balloon insertion procedure was performed as described by others [Citation19]. Briefly, all patients were administered ondansetron 8 mg t.i.d. for 5 days after balloon insertion, aprepitant 125 mg on day 1, then 80 mg daily for 2 days after insertion; and pantoprazol 20 mg b.i.d starting 3 days prior to treatment and lasting 16 weeks thereafter. On the day of balloon insertion, patients were advised to stop liquids and food 8 h prior to balloon insertion. The balloon capsule was placed at the back of the tongue by the physician and the patient was asked to swallow the capsule with some water. For patients who did not immediately succeed swallowing the capsule, a stylet was introduced into the catheter to direct the capsule toward the hypopharynx. After X-ray confirmed intragastric position of the balloon radiopaque marker, the balloon was filled with 550 mL of sterile water containing a preservative. The fully filled balloon contour within the stomach was verified by X-ray before the catheter was dislodged from the balloon. The balloon is designed to self-empty and be naturally excreted after 16 weeks.
Lifestyle intervention and follow-up
All patients started dietary intervention 2 weeks prior to balloon insertion. Patients at Oslo University Hospital were provided with diet recommendations by a nutritionist based on individual preference and needs, according to the current standard for patients, similar to the trial sample, at the center [Citation23].
Patients at Vestfold Hospital received a standardized 1200 kcal/day diet plan. Following balloon insertion, patients were advised a liquid diet and to proceed to pureed food at day 2, and gradually introduce solid food.
Anti-diabetic medication was temporary lowered, at the discretion of the endocrinologist, to avoid hypoglycemia.
All patients were followed up with study visits at 4, 16, and 52 weeks after balloon insertion. All visits included a clinical examination with measurements of body weight and composition, anthropometric measures and blood pressure, laboratory analyses, registration of prescription and over-the-counter medications and supplements, and assessment of balloon excretion and adverse events.
Patients at Vestfold Hospital also underwent a validated gastric emptying test (octanoic acid breath test) prior to balloon insertion to assess diabetic gastroparesis [Citation24,Citation25]. The rate of gastric emptying was measured by administering a solid meal of 1050 kJ consisting of 60 g of white bread, 5 g of margarine, a one-egg omelet, and 150 ml of water. The egg yolk included in the meal contained 91 mg of 13C-octanoic acid as a marker of gastric emptying. Breath samples were collected every 15 min until 240 min after meal intake, and 13C content was determined by gas chromatographic purification isotope ratio mass spectrometry. Variables of gastric emptying were estimated according to Ghoos et al. [Citation25]. The parameters used to assess gastric emptying was T1/2 (cut-off value 109.4) and Tlag (cut-off value 78.1). The reference values are based on unpublished data from healthy volunteers.
Ascertainment of outcome measures
Feasibility of the intervention was assessed by the investigators with regard to technical success of insertion, and through adverse event assessment during follow-up visits.
Body weight and composition
We measured body weight with patients wearing light clothing and no shoes, and anthropometric measures with patients in an upright position. Height was measured using wall mounted stadiometers; waist circumference (WC) was measured at the point midway between the lowest rib margin and the iliac crest. Height and circumference were measured to the nearest 0.5 cm and weight to the nearest 0.1 kg.
Diabetes
Anti-diabetic treatment was in accordance with the guidelines of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). During the study follow-up, anti-diabetic treatment was adjusted according to a predefined algorithm, with treatment goal of HbA1c < 53 mmol/mol (see Supplement 1). Diabetes remission was defined as HbA1c < 48 mmol/mol and absence of active pharmacologic therapy.
Ethics and approvals
The study was approved by the Regional Ethics Committee of South-East Norway and the institutional Data Protection Offices at the participating institutions. All patients provided written informed consent before enrolment. The study was registered at clinicaltrials.gov (NCT03576833). The Elipse™ balloon is approved for the EU and EEC market.
Statistical analyses
We analyzed the predefined clinical endpoints for each patient stratified by study center. We used descriptive statistics and calculated means, standard deviations (SD), and 95% confidence intervals (CI) where applicable. No data were imputed for scheduled follow-up visits, which patients did not attend. Spearman coefficient with 95% CI was used to assess the level of correlation between variables. We used R version 4.0.3 (R Foundation for Statistical Computing, Vienna, Austria) for all statistical analyses and figures.
Results
We included 10 participants at Oslo University Hospital from April to May 2018, and 9 patients at Vestfold Hospital from October 2018 to April 2019. Patient characteristics at enrolment are shown in . One patient withdrew consent after enrolment but prior to balloon insertion and was excluded from analyses. Three patients did not attend the week 52 visit despite reminders, and did not provide data for analyses at this time point.
Table 2. Patient characteristics.
Feasibility
All procedures were performed as outpatient procedures of the endoscopy unit at the participating centers by a trained gastroenterologist (CT or TEM) with assistance of one nurse. Balloon insertion was successfully accomplished in all patients. All patients were able to swallow the balloon capsule. No sedation or invasive procedures were needed for successful placement of the balloon. Balloon filling was uncomplicated and X-ray control was technically easy and uneventful.
Weight loss
The mean total body weight loss (TBWL) 16 weeks after balloon insertion was 3.9% (95% CI 2.1–5.7). 52 weeks after insertion, the mean TBWL was 0.8% (95% CI 1.9–3.5). There were large differences in weight loss between the two centers, and between individual patients ( and ); some patients had a clinically significant TBWL of between 5% and 9.6% after 16 weeks, while other patients did not experience any clinically significant weight loss. After 52 weeks, most patients had regained the BMI they had before intervention. Patients treated at Vestfold Hospital had a 2.4% higher mean TBWL at week 16 compared with patients treated at Oslo University Hospital, but the difference was not statistically significant (p = .180).
Table 3. Results.
Diabetes control
Mean HbA1c reduction was 7 (95% CI 4–10) mmol/mol after 16 weeks and 1 (95% CI −6 to 9) mmol/mol after 52 weeks, with large differences between individual patients (). Two patients did not use medication at the start of the study and did not start medication during the study period.
Gastric emptying
Gastric emptying breath test analyses showed significantly delayed gastric emptying in only one patient (no. 12). One patient (no. 19) had slightly delayed gastric emptying, while all other patients had normal rate of gastric emptying (). There was no association between gastric emptying at baseline and balloon efficacy on weight loss after 52 weeks (for GEBT T1/2 r = −0.286, 95% CI −0.855 to 0.595; for GEBT Tlag r = −0.143, 95% CI −0.809 to 0.684).
Adverse events
Adverse events occurred in two patients (10.5%). One patient (no. 19) developed persistent vomiting. An abdominal X-ray performed 15 days after balloon insertion showed a dilated stomach with the balloon impacted in the antrum, consistent with gastric outlet obstruction. A nasogastric tube was placed, and gastroscopy was performed in general anesthesia, with confirmation of balloon impaction in the antrum. The balloon was punctured and removed during the endoscopic procedure, with immediate symptom relief. The postprocedural course was uneventful.
One patient (no. 11) was admitted to hospital 2 days after balloon insertion with vomiting and dehydration. Abdominal X-ray was unremarkable, with the balloon in expected position with no sign of gastric or small bowel dilation. The patient was admitted over night for intravenous fluids and antiemetics with symptom relief, and an uneventful course during the rest of the study period.
Discussion
This first Scandinavian trial of a new intragastric balloon with non-invasive insertion and removal for weight loss therapy demonstrated good feasibility, but varying and transient efficacy on obesity and diabetes control.
The new balloon system is attractive for weight loss therapy, as it does not require invasive procedures for balloon insertion or removal and can be performed as a short outpatient procedure also at non-specialized centers. We confirmed that this is indeed the case.
We did not observe any adverse events regarding balloon deflation and excretion and thus assume that the balloons deflated as designed after approximately 16 weeks and were excreted uneventfully in all patients. However, as reported, we experienced balloon impaction in one patient, which is a previously recognized, but rare, adverse event of balloon treatment [Citation19]. Additionally, one patient had vomiting and dehydration which required hospital admission for administration of iv. fluids and antiemetics. For comparison, in the largest study to date on the Elipse balloon with 1770 participants [Citation19], 52 patients (2.9%) required early balloon removal due to intolerance, 7 patients (0.4%) required endoscopic balloon removal due to adverse events (spontaneous hyperinflation, esophagitis, pancreatitis or gastric outlet obstruction), and 4 patients (0.2%) required laparoscopic surgery due to adverse events (small bowel obstruction or gastric perforation). Thus, we conclude that the Elipse balloon performs uneventful in most patients, but serious complications may occur and competent assistance is required at centers which provide this treatment.
This study was not designed to evaluate the efficacy of the new intragastric balloon. However, our data indicate a lower than expected effect for weight loss. Except for the patient who had the balloon removed at day 15 due to gastric outlet obstruction, all participants had a TBWL of less than 10% at week 16, which is significantly lower than previous studies with the same balloon [Citation20]. The aforementioned Elipse balloon study with 1770 participants [Citation19] showed a mean TBWL of 14.2% at week 16, as compared with our result of 3.9%. The effect on HbA1c reduction in our study was also lower than expected. This may be attributed to a low baseline HbA1c, particularly for the patients at Oslo University Hospital.
Our trial differs from previous studies in several ways: first, all our patients had type 2 diabetes while there were few such patients in other studies. Delayed gastric emptying has been proposed as a significant physiologic mechanism of intragastric balloons [Citation26]. After the 10 first patients had been treated in Oslo, we discussed the possibility for diabetic gastroparesis as a possible impediment for effective balloon treatment in diabetic patients. However, gastric emptying tests performed by the subsequent group of patients treated in Vestfold showed no apparent association of slow gastric emptying with treatment efficacy. Second, we applied real-world nutritional follow-up with nutritionist visits on two occasions prior to week 16, as compared with four occasions in previous studies. A blue-tooth scale and smartphone app was also used to enhance compliance in in other studies. This emphasizes previous suggestions that the balloon needs intensive parallel nutritional counseling to be effective [Citation27]. However, we did not register food intake or habits during balloon therapy and thus do not know if and how these changed due to the balloon. Third, our patients received treatment within the Norwegian public health care system, with no patient co-payments for participation, as in other studies. Thus, our results may be more valid for what can be expected in real life, as compared with other settings with highly motivated patients who have to pay for intervention and follow-up themselves.
In conclusion, this first Scandinavian real-world clinical trial with a new minimally invasive intragastric balloon system did prove feasibility of the balloon, but did not confirm expected efficacy for weight loss and diabetes control. Consequently, we decided not to proceed from this pilot study to the intended randomized controlled trial comparing the Elipse™ balloon with laparoscopic bariatric surgery (sleeve gastrectomy or Roux-en-Y gastric bypass) in patients with type 2 diabetes and body mass index (BMI) of 30.0–39.9 kg/m2.
Supplemental Material
Download PDF (83.6 KB)Disclosure statement
The Elipse™ balloons utilized for this study were granted by Allurion Inc. (Natick, MA).
Additional information
Funding
References
- World Health Organization. Obesity and overweight [Internet]. Geneva (Switzerland): WHO; 2020. Available from: https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight
- Ward ZJ, Bleich SN, Cradock AL, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381(25):2440–2450.
- Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377(9765):557–567.
- Fildes A, Charlton J, Rudisill C, et al. Probability of an obese person attaining normal body weight: cohort study using electronic health records. Am J Public Health. 2015;105(9):e54–e59.
- Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes – 5-year outcomes. N Engl J Med. 2017;376(7):641–651.
- Nguyen NT, Varela JE. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Rev Gastroenterol Hepatol. 2017;14(3):160–169.
- Flum DR, Khan TV, Dellinger EP. Toward the rational and equitable use of bariatric surgery. JAMA. 2007;298(12):1442–1444.
- Jakobsen G, Småstuen M, Sandbu R, et al. Association of bariatric surgery vs medical obesity treatment with long-term medical complications and obesity-related comorbidities. JAMA. 2018;319(3):291–301.
- Wilding JPH, Batterham RL, Calanna S, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384(11):989–1002.
- Cefalu WT, Bray GA, Home PD, et al. Advances in the science, treatment, and prevention of the disease of obesity: reflections from a diabetes care editors’ expert forum. Diabetes Care. 2015;38(8):1567–1582.
- Kotinda A, de Moura DTH, Ribeiro IB, et al. Efficacy of intragastric balloons for weight loss in overweight and obese adults: a systematic review and meta-analysis of randomized controlled trials. Obes Surg. 2020;30(7):2743–2753.
- Genco A, Ernesti I, Ienca R, et al. Safety and efficacy of a new swallowable intragastric balloon not needing endoscopy: early Italian experience. Obes Surg. 2017;28(2):40.
- Raftopoulos I, Giannakou A. The elipse balloon, a swallowable gastric balloon for weight loss not requiring sedation, anesthesia or endoscopy: a pilot study with 12-month outcomes. Surg Obes Relat Dis. 2017;13(7):1174–1182.
- Machytka E, Gaur S, Chuttani R, et al. Elipse, the first procedureless gastric balloon for weight loss: a prospective, observational, open-label, multicenter study. Endoscopy. 2017;49(2):154–160.
- Machytka E, Chuttani R, Bojkova M, et al. Elipse™, a procedureless gastric balloon for weight loss: a proof-of-concept pilot study. Obes Surg. 2016;26(3):512–516.
- Chuttani R, Machytka E, Raftopoulos I, et al. The first procedureless gastric balloon for weight loss: final results from a multi-center, prospective study evaluating safety, efficacy, metabolic parameters, quality of life, and 6-month follow-up. Gastroenterology. 2016;150(4):S26.
- Al-Subaie S, Khalifa S, Buhaimed W, et al. A prospective pilot study of the efficacy and safety of elipse intragastric balloon: a single-center, single-surgeon experience. Int J Surg. 2017;48:16–22.
- Alsabah S, Al Haddad E, Ekrouf S, et al. The safety and efficacy of the procedureless intragastric balloon. Surg Obes Relat Dis. 2018;14(3):311–317.
- Ienca R, Al Jarallah M, Caballero A, et al. The procedureless elipse gastric balloon program: multicenter experience in 1770 consecutive patients. Obes Surg. 2020;30(9):3354–3362.
- Ramai D, Singh J, Mohan BP, et al. Influence of the elipse intragastric balloon on obesity and metabolic profile: a systematic review and meta-analysis. J Clin Gastroenterol. 2020;55(10):836–841. Publish Ahead of Print.
- Crea N, Pata G, Della Casa D, et al. Improvement of metabolic syndrome following intragastric balloon: 1 year follow-up analysis. Obes Surg. 2009;19(8):1084–1088.
- Popov VB, Ou A, Schulman AR, et al. The impact of intragastric balloons on obesity-related co-morbidities: a systematic review and meta-analysis. Am J Gastroenterol. 2017;112(3):429–439.
- Norwegian Directorate of Health. Prevention, assessment and treatment of overweight and obesity in adults. National guidelines for primary health care. (IS-1753 Forebygging, utredning og behandling av overvekt og fedme hos voksne. Nasjonale retningslinjer for primærhelsetjenesten).
- Perri F, Pastore MR, Annese V. 13C-octanoic acid breath test for measuring gastric emptying of solids. Eur Rev Med Pharmacol Sci. 2005;9(5):3–8.
- Ghoos YF, Maes BD, Geypens BJ, et al. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology. 1993;104(6):1640–1647.
- Gómez V, Woodman G, Abu Dayyeh BK. Delayed gastric emptying as a proposed mechanism of action during intragastric balloon therapy: results of a prospective study. Obesity. 2016;24(9):1849–1853.
- Lopez-Nava G, Asokkumar R, Rull A, et al. Bariatric endoscopy procedure type or follow-up: what predicted success at 1 year in 962 obese patients? Endosc Int Open. 2019;07(12): E1691–E1698.

