Abstract
Objectives
To predict how the10-year birth cohort specific prevalence rates of chronic non-atrophic (CG) and atrophic gastritis (AG), related to Helicobacter pylori (Hp) infection, will decline during the 21st century among the native adult Finns.
Materials and methods
The predictions are based as continuums of our earlier observations of gradual and significant declines in birth cohort specific prevalence rates of CG and AG in endoscopic biopsies from gastric antrum and corpus of 2298 adult dyspeptic outpatients or asymptomatic volunteers born 1890–1977 that were endoscopied in 1972–1997 in Finland.
Results and discussion
We could predict that the Hp related CG and AG will gradually disappear in history among the native Finns during the 21st century. From the 2020s onward, the CG and AG would decrease with time in prevalence rate, cohort-by-cohort, and would be more and more highlighted in the middle aged or elderly age groups only. Finally, since all birth cohorts (generations) infected with Hp have passed away by 2080, the Hp related gastrites would not appear anymore in notable counts among the native Finns. Correspondingly, gastric cancers and peptic ulcers (both duodenal and gastric), which are etiopathogenetically linked with Hp gastrites, would similarly become gradually more and more infrequent and rare disorders among native Finns during the 21st century.
Background and aims
According to a study recently published in Scandinavian Journal of Gastroenterology the 10-year birth cohort-specific periodical prevalence rates (relative frequencies/proportions) of chronic non-atrophic (CG) or atrophic (AG) gastritis, considered to be linked with Helicobacter pylori (H. pylori/Hp) infection, have decreased from 90 to 40% among native Finns during the first seven decades of the twentieth century, the rate of the decrease being 10% per every 10-year period on average [Citation1]. The knowledge of the cases with or without CG or AG in the 10-year birth cohort categories was obtained from endoscopic surveys of altogether 2298 native adult Finns born between 1890 and 1977 [Citation1]. All were examined with gastroscopy and multiple endoscopic biopsies from both antrum and corpus in 1972–1997 [Citation1]. All subjects included in analysis were asymptomatic volunteers or dyspeptic outpatients without any abnormal lesions (ulcers, tumours, polyps, etc.) in stomach endoscopy [Citation1].
In above-mentioned study, the category of people with CG and AG are considered to represent people in which the CG or AG (‘diseased’ stomach) is associated to and caused by the past or on-going Hp infection [Citation2–12]. Correspondingly, the category of people without the CG or AG is considered to represent people with ‘normal’ (N) stomach mucosa without any damages related to the Hp. In noting and recording the gastritis related to Hp (CG or AG), gastritis of obvious autoimmune origin were excluded and were identified by serological evidence (presence of parietal cell antibodies) and/or by typical morphological phenotype of the autoimmune gastritis (endoscopy and biopsy evidence of advanced atrophy in gastric corpus and fundus in association with a normal and healthy antrum mucosa) [Citation1].
Goal of the present report is to predict and to estimate roughly when and how the Hp related CG and AG will disappear from native Finnish population by extending the twentieth century observations to forecasts that will also cover the birth cohorts of native Finns born after the year 1997. The predictions are based on assumption that the changes in rates of the Hp related CG-AG follow similar trends in the twenty first century as in the twentieth century.
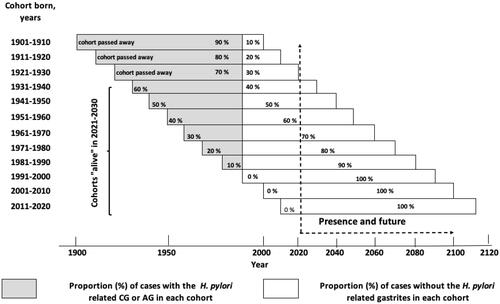
In present report, the birth cohort-specific periodical prevalences of N and those with Hp related CG or AG are presented as proportions (percentages) in 10-year birth cohorts of a hypothetical population with 100 people in each birth cohort, all assumed to live up to age of 100 years, and the whole presentation covering a time span of about 200 years in total ().
Figure 1. Schematic illustration of prevalences (in percentage) of cases with or without the H. pylori related non-atrophic gastritis (CG) or atrophic gastritis (AG) in birth cohorts of native Finns over a time span of 200 years. Each birth cohort is considered to include 100 people that are expected to live 100 years. It is assumed that the cohort-specific proportion of ‘diseased’ stomachs (with H. pylori related CG or AG) decreases with time, cohort-by-cohort, by 10% per every 10-year period.
The predictions of the cohort-specific prevalences, separately for N, CG and AG, are presented, in addition, over a hypothetical population of 800 adult native Finns (age 20 years or more) assumed to be alive in 2021–2030 (). Correspondingly, the estimations are also expressed over an ‘actual’ Finnish born population of adults in which the number of people in each cohort category (altogether 800 subjects in eight 10-year birth cohorts) are adjusted by weights from the age pyramid of Finnish population in 2019 ().
Table 1. Table on predictions of prevalences of cases with normal stomach (N) without H. pylori gastrites) and of the cases with H. pylori related chronic non-atrophic (CG) or atrophic (AG) gastritis in birth cohorts of adult native Finns (800 subjects in eight birth cohorts) in the 2020s.
Background data for present predictions
Scientific background and presumptions for the present predictions are based on following statements [Citation1]: Hp infection is a communicable birth cohort-specific disease (stomach infection) whereby the birth cohort-specific prevalence rates of Hp and subsequent CG and AG are consequences of the extent of Hp infections in each cohort during the cohorts´ childhood and adolescence [Citation2–4]. A CG is an ultimate result of the Hp infection that does not heal spontaneously unless the Hp is actively eradicated but may also spontaneously fade out in cases with advanced AG and stomach hypochlorhydria [Citation5], and that [Citation3] a lifelong CG does not develop without a preceding Hp infection, with exception of chronic gastrites of pure autoimmune origin [Citation4–8]. The cohort-specific prevalence of Hp infection has been 90–100% in Finland in the nineteenth century. Thereafter, in each cohort, the prevalence of Hp infection and the birth cohort specific prevalence of Hp induced CG has been decreasing by 10% per every 10 years on average [Citation1,Citation5]. Within each cohort with aging of the affected subjects, the Hp induced CG cases tend to progress gradually to AG during the cohort´s adulthood (from age 20 years onward), whereby, the relative proportion of the Hp related AG cases increases in each cohort by 10% per every 10 calendar years [Citation1,Citation7–12].
Predictions and discussion
Since the 10-year birth cohort-specific prevalence of ‘diseased’ stomach (cases with the Hp induced CG or AG) tends to decrease by 10% per every 10-year period on average, stomachs with Hp related gastrites (GG or AG) should not appear any more in Finnish birth cohorts born after the year 1990 as illustrated schematically in . Present predictions suggest that the birth cohort born in 1981–1990 is the last one among native Finns in which cases with a ‘diseased’ stomach with Hp gastrites would appear in notable extent ().
The decline in prevalence of the Hp gastrites has been so prompt, and is obviously fast now as well, that only some 10% of people in birth cohort born in 1981–1990 would show Hp gastrites (CG or AG) and that this generation (cohort) would be the last one that markedly suffers of sequels of on-going or past Hp infections. Finally in practice, the medical and economic burden of ‘diseased’ stomachs with Hp gastrites would disappear in the 2080s when all cohorts born before the year 1990 have passed away (). Thereafter, the Hp gastritis and its sequels would not be, anymore, significant medical or economic burdens among the native Finns.
In actual general populations, the relative number of people at age over 70 years is certainly markedly lower compared to other age groups (). Even though being a minority in society, the elderly people are particularly the subgroup of people in the twenty first century that will suffer most from CG and AG caused by the Hp. One may estimate from that some 10–30% of people at age of 70 years or more in 2050–2080 (born 1961–1990) will have a ‘diseased’ stomach mucosa related to the Hp infection. All other (people by age less than 70 years in 2050–2080, born after the year 1990) would have a stomach without the Hp gastritis. Exceptions are certainly the CG and AG cases of pure autoimmune origin that may or may not appear irrespective of the Hp infection. In initial study populations collected in 1972–1997, the prevalence of autoimmune gastritis varied between subgroups of endoscopied people but was 6% at its peak (see reference [Citation1]).
The cohort-specific prevalences of cases with N and Hp related CG or AG are predicted more specifically in for time-period 2021–2030. This is done in framework of 800 ‘hypothetical’ adults (people at age 20 of years or more in eight birth cohorts, 100 subjects in each). The predictions are also done in for ‘actual’ population by readjusting the 800 hypothetical subjects to eight cohorts by weights from the ‘age pyramid’ in Finland in 2019 (). In predictions, it is assumed that the Hp induced CG cases turn to the AG cases by rate of 10% per every 10-year period during the cohorts´ adulthood, that is, during every 10 years’ time periods from the age 21 to the actual calendar age in year 2021 [Citation1,Citation8].
The population-specific periodical prevalence of ‘diseased’ stomach with the Hp induced CG or AG is estimated to be 158 cases per 800 people (198 cases per 1000 adults) in the ‘actual’ native Finnish population in 2021–2030 in total, indicating that the mean population-specific prevalence rate of ‘diseased’ stomach with Hp gastritis would be approximately 20% among all adult native Finns (). Notable counts of cases with the Hp related CG or AG would appear particularly in the middle-aged and elderly age groups only. Among people of age 70–100 years in the 2020s (born 1931–1960), the mean prevalence rate of ‘diseased’ stomach with Hp gastritis (CG or AG) is predicted to be 45% but only 4% among people of age under 50 years (born after 1980).
Noteworthy, particularly the cases with Hp related AG will be emphasized in 2021–2030, in the elderly age groups specially. shows that the mean prevalence rates of AG (AG of any grade) or CG are 25 and 20% in three oldest birth cohorts in 2021–2030 (born 1931–1950), respectively, whereas these prevalences are nil in two youngest cohorts (born 1991–2010). At population level among all adults, the prevalence rates of cases with Hp related AG or CG are predicted to be 9 and 11%, respectively. Altogether 71 people per 800 adult Finns would show an AG caused by Hp in 2021–2030, indicating a rate of 89 cases per 1 000 adults.
Simultaneously with the disappearance of Hp, CG and AG, the most important stomach diseases, like gastric cancers (with exception of cancers bound to inherited gene mutations) or ordinary peptic ulcers (both duodenal and gastric), which are pathogenetically linked to Hp gastritis, would accordingly decrease in incidence and prevalence among the native Finns [Citation5,Citation12]. In fact, gastric cancer was the most frequent type of cancer in Finland in the 1950s, in both men and women, but is now at rank 10 among all malignancies [Citation13]. In strong contrast to other types of malignancies, the age-standardized incidence of gastric cancer has markedly and similarly declined in all Nordic countries, even to one fourth or fifth during a period from 1950 to 2020. This corresponds the trends in declines of the birth cohort and population specific prevalences of Hp gastritis in Finland [Citation13].
The present predictions are certainly hypothetical and concern native Finns and the present demographic population structure in Finland only. They are also rough ones and do not include predictions of course of pure autoimmune gastritis. However, the present predictions on the Hp related gastritis are based on presumptions with acknowledged scientific background, and on objective observations of natural course of chronic gastritis in general populations [Citation1–12].
Overall, the observations published on biology of Hp infection and on Hp related gastritis are surprisingly similar and monolithic worldwide, suggesting that also the observed decline in prevalence rates of Hp related gastritis in Finland is likely more universal than local [Citation14]. The declines observed in Hp incidences and prevalences in general are obviously results of remarkable improvements in socioeconomics, family lifestyle and environmental hygiene during the 20th and 21st centuries, noticeably in developed societies [Citation14]. Hp gastritis and its sequels were presumably extremely common diseases and worldwide health burdens for all people of the nineteenth century but are now shrinking and going down in history. Presumably, the Hp and the Hp induced CG and AG would gradually shrink to more minor and negligible medical and economic problems, even worldwide. Instead of ‘whether’, the question is ‘when’?
Possibly, but unlikely in practice, the evanescence of Hp related gastritis could be accelerated with active population-wide actions by eradication of Helicobacter pylori with antibiotics. Noteworthy, however, the disappearance of Hp, and the consequent disappearance of the Hp gastritis as well, have been spontaneous and developmental events that apparently begun in developed societies early in the twentieth century, much before the time of modern antibiotics [Citation1]. One may assume that the disappearance of the Hp infection will continue still without any active interventions and will gradually take place in developing societies as well.
Author contributions
All three authors participated in execution of the prediction and in writing of the paper.
Disclosure statement
Dr. Pentti Sipponen is a shareholder of Biohit Healthcare Plc, Helsinki, Finland and Repolar Pharmaceuticals Oy, Espoo, Finland. No potential conflict of interest was reported by the author(s).
References
- Sipponen P. Prevalence rates of heathy stomach mucosa, chronic non-atrophic and atrophic gastritis in endoscopic biopsies in adults born in Finland in 1890–1977. Scand J Gastroenterol. 2021;56(8):874–881.
- Sipponen P. Helicobacter pylori: a cohort phenomenon. Am J Surg Pathol. 1995;19(Suppl 1):S30–S6.
- Roosendaal R, Kuipers EJ, Buitenwerf J, et al. Helicobacter pylori and the birth cohort effect: evidence of a continuous decrease of infection rates in childhood. Am J Gastroenterol. 1997;92(9):1480–1482.
- Sipponen P, Helske T, Järvinen P, et al. Fall in the prevalence of chronic gastritis over 15 years: analysis of outpatient series in Finland from 1977, 1985, and 1992. Gut. 1994;35(9):1167–1171.
- Marshall BJ, Warren JR. Unidentified curved bacilli in the stomach of patients with gastritis and peptic ulceration. Lancet. 1984;1(8390):1311–1315.
- IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. IARC Monographic Evaluation of Carcinogenic Risks to Humans. Lyon: International Agency for Research on Cancer; 2019.
- Kusters JG, van Vliet AHM, Kuipers EJ. Pathogenesis of Helicobacter pylori infection. Clin Microbiol Rev. 2006;19(3):449–490.
- Kuipers EJ, Klinkenberg-Knol EC, Vandenbroucke-Grauls CM, et al. Role of Helicobacter pylori in the pathogenesis of atrophic gastritis. Scand J Gastroenterol. 1997;223:28–34.
- Sipponen P, Kekki M, Siurala M. The sydney system: epidemiology and natural history of chronic gastritis. J Gastroenterol Hepatol. 1991;6(3):244–251.
- Ihamäki T, Kekki M, Sipponen P, et al. The sequelae and course of chronic gastritis during a 30- to 34-year bioptic follow-up study. Scand J Gastroenterol. 1985;20(4):485–491.
- Villako K, Maards H, Tammur R, et al. Helicobacter (Campylobacter) pylori infestation and the development and progression of chronic gastritis: results of long-term follow-up examinations of a random sample. Endoscopy. 1990;22(3):114–117.
- Sipponen P, Maaroos H-I. Chronic gastritis. Scand J Gastroenterol. 2015;50(6):657–667.
- Statistics on cancer in Nordic countries; 2020. https://nordcan.iarc.fr/.
- Moayyedi P, Axon ATR, Feltbower R, Leeds HELP Study Group, et al. Relation of adult lifestyle and socioeconomic factors to the prevalence of Helicobacter pylori infection. Int J Epidemiol. 2002;31(3):624–631.
