Abstract
Background
A person’s occupation may increase his/her risk for developing inflammatory bowel disease (IBD). This study investigated the association between risk for later-onset of IBD and both specific occupations and occupational physical activity (OPA) levels.
Materials and methods
A multicenter hospital-based matched case-control study was conducted using the Inpatient Clinico-Occupational Survey database. Cases were patients with Crohn’s disease (CD) and ulcerative colitis (UC) patients admitted for the first time between 2005 and 2015. Four controls matched by age, sex, admission year and hospital were selected for each case. Cases and controls were grouped into the longest-held occupations as classified by the Japanese Standard Occupational Classification and OPA levels. We conducted conditional logistic regressions to estimate odds ratios (ORs) and 95% confidence intervals (CIs) for IBD, CD and UC adjusted for alcohol consumption and smoking status.
Results
There were 564 cases (172 CD, 392 UC) and 2086 controls. The risk for UC was higher among sales workers and carrying, cleaning and packing workers (ORs 2.62 [95%CIs 1.18–5.82], 2.52 [1.04–6.09]). There was no association between occupation type and CD risk. Higher OPA level decreased CD risk (OR 0.51 [95%CIs 0.26–1.00]) and increased UC risk (OR 1.53 [95%CIs 1.02–2.30]).
Conclusions
Our study revealed that the risk for later-onset of UC, but not CD, was associated with longest-held 'service' and 'manufacture' work. The risk by OPA levels was inversely associated between CD and UC. Further studies are needed by follow-up method for long-term effects of physical activity.
Introduction
Inflammatory bowel disease (IBD), which includes disorders such as Crohn’s disease (CD) and ulcerative colitis (UC), is a worldwide disease and an annual increase in IBD burden [Citation1]. In North America and Europe, IBD patients have increased in the twentieth century and now are flat or slightly increasing. In Asia, South America and Africa, there has been a rapid increase in the prevalence of IBD in the twenty-first century [Citation1]. IBD is more common at the age of teens to 20s (younger-onset) but can occur throughout life. Recent analyses from the genome wide association study (GWAS) illustrate multiple loci associated with IBD, and from an international consensus, IBD develops when genetic factors are combined with environmental factors such as inflammation that upsets the homeostatic balance between the gastrointestinal immunity and gut microbiota [Citation2].
Occupational factors are listed among environmental factors contributing to IBD. Several previous studies reported that white-collar workers are at a high risk for developing IBD [Citation3–7]. White-collar workers spend a lot of time in sitting positions and are likely to take part in limited physical activities [Citation4,Citation8,Citation9]. It is possible that IBD pathogenetic mechanisms among such workers are related to prolonged gastrointestinal transit time of foods [Citation4].
However, limited research on specific occupations associated with IBD exists. Sonnenberg [Citation10] documented the occupations of IBD patients German-wide in 1990. From his results, unskilled workers with a high workload had lower cases of IBD suggesting that occupational physical activity (OPA) plays an important role in IBD development. A review of occupational hazards by Leso et al. [Citation9] concurred with the results of Sonnenberg. Similarly, two published meta-analyses reported that persons who engage in more physical activities have a lower risk of developing CD [Citation11,Citation12].
Total physical activity is comprised of daily physical activity (DPA) and leisure-time physical activity (LTPA). Fukushima et al. [Citation13]. reported that DPA, which is related to OPA, differed between white-collar workers and blue-collar workers. Among workers, DPA depends on their occupational characteristics, particularly in jobs with more than a moderate level of OPA. Conversely, Rasmussen et al. [Citation14]. found that LTPA was not associated with a risk of developing IBD (CD/UC). These findings suggest that OPA levels predominantly impact IBD risk among workers.
We hypothesised that environmental factors, such as specific occupations and/or OPA levels, had more influence on IBD development among middle-aged and older people (40 years old and over, later-onset) than among younger people (younger-onset). But most of the previous OPA studies, excluding a Denmark study [Citation14], included patients with both types younger- and later-onset IBD. Therefore, we first examined the association between the risks of developing later-onset IBD in specific occupations using a nationwide database. Second, using the same database, we investigated the association between OPA and IBD risk.
Materials and methods
Study setting and population
This study was a nationwide, multicenter, hospital-based matched case-control study using data from 2005 to 2015 of the Inpatient Clinico-Occupational Survey of Rosai Hospital Group (ICOD-R). Details of this survey have been described elsewhere [Citation15–17]. Briefly, ICOD-R includes the clinical history and the occupational history of all inpatients admitted to the Rosai Hospital Group, which the Japan Organization of Occupational Health and Safety (JOHAS) operates 34 core regional hospitals nationwide in Japan. The clinical history was obtained from the discharge summary written by medical doctors. The occupational history was obtained from an interview by trained registers at each hospital and documented using the Japan Standard Occupational Classification (JSOC). This classification nearly matched the International Standard Classification of Occupations (ISCO).
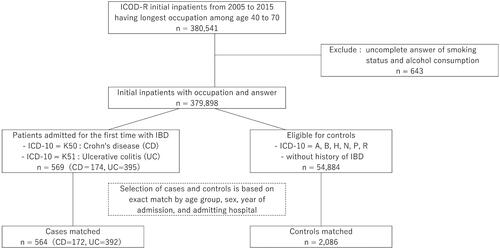
This study enrolled 380,541 participants with complete occupational information aged 40–69 years during the study period. We excluded patients who had missing information on smoking status and drinking status (n = 643), leaving 379,898 participants who were potentially eligible for inclusion. The admission date had to be the patient’s first admission with confirmed IBD. These cases had IBD codes (CD: code K-50 or UC: code K-51, n = 569) on the 10th version of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) as the main definitive diagnosis on their discharge summaries. We chose controls as patients that were hospitalised for reasons unrelated to IBD and who did not have a history of IBD. Diseases unrelated to IBD included the following; ‘certain infectious and parasitic disease (code A and B),’ ‘disease of the eye and ear (code H),’ ‘disease of the genitourinary system (code N),’ ‘certain conditions originating in the perinatal period (code P)’ and ‘symptoms, signs, and abnormal clinical and laboratory findings, not elsewhere classified (code R),’ and diagnoses that exclude ‘symptoms and signs involving the digestive system and abdomen (code R10-19).’ Patients without a history of IBD did not have any codes of IBD in diagnoses documented on their discharge summaries. Finally, 54,884 patients were selected as eligible candidates for the matching process (). We randomly selected four controls for each eligible case matched for age (5 year strata), sex, admission year and hospital. An average number of 3.7 controls were matched to each case; 84.2% of the cases had four controls each (564 cases and 2086 controls).
Occupational categories and occupational physical activity
The participants’ occupational categories used were the large categories on the JSOC codes. There were ‘A: managers,’ ‘B: professionals and technicians,’ ‘C: clerical support workers,’ ‘D: sales workers,’ ‘E: service workers,’ ‘F: police, fire-fighters, and security workers,’ ‘G: agricultural, forestry, and fishery workers,’ ‘H: manufacture, craft, repair, and assemblers,’ ‘I: drivers, crews, transport, and machine operators,’ ‘J: construction and mining,’ ‘K: carrying, cleaning, and packing’ and ‘L: homemaker, inoccupation, and else.’ The mean lengths (mean[±standard deviation]) of the longest-held occupation of all patients, cases and controls were 21.2[±11.7] years, 20.8[±11.3] years and 21.3[±11.8] years, respectively.
We classified occupational categories into three groups based on OPA using OPA levels documented in previous study [Citation15,Citation18]. Specifically, OPA levels were defined by an accelerometer, modified by the National Health and Nutrition Examination Survey 2003–2004 (NHANES) [Citation18]. High OPA groups included the JSOC categories G, J and K. Low OPA groups included the categories A, B, and C. Other occupational categories (categories D, E, F, H and I), excluding the JSOC category L, were in the intermediate OPA group.
The reason we examined the longest-held occupations, but not current occupations, was intended to minimise the possibility of changing and quitting their jobs by developing IBD. We considered that people over 60 years old did not work after retirement during the period of 2005–2015 before the extension of statutory retirement age in 2016.
Covariates
Age (5 year strata), sex, admission year and hospital were controlled using an exact matching procedure. Alcohol consumption (‘standard drink’ based on the amount of pure alcohol [Citation19]; under two standard drinks, 2–6 standard drinks, over six standard drinks) and smoking status (never smoked, former smoker, current smoker) were included as confounding factors in the regression models.
Statistical analysis
We calculated the odds ratios (ORs) and their 95% confidence intervals (CIs) to compare IBD development risk for each occupational category and OPA level using conditional logistic regression analysis. The reference was set as ‘A: managers’ who were the fewest among the occupational categories. The OPA reference group selected was low OPA group based on a previous study [Citation20]. Cases were matched to controls based on age, sex, admission year and admitting hospital (model 1). Alcohol consumption (three levels) was adjusted for in model 2, and smoking status (three groups) was additionally adjusted for in model 3. We also stratified our results by gender to estimate the fully adjusted ORs. We changed the selection of matched cases and controls from three to five controls for each case to reduce random error and overmatching and reanalysed our data. All statistical analyses were carried out using SAS software, version 9.4 (SAS Institute, Cary, NC). p Values were two-sided, and statistical significance was set to <.05.
Ethical considerations
Written informed consent was obtained from each patient prior to the completion of any questionnaires. Access to the dataset was granted by a research agreement between the study investigators and the JOHAS. This study was approved by the JOHAS (protocol no. R1-006) and the Research Ethics Committees of Tokai University School of Medicine (protocol no. 18R-309).
Results
Finally, 564 IBD patients (CD: 172 cases; UC: 392 cases) were analysed. shows the background characteristics of controls and cases, including each type of IBD (Supplementary Table 1 gives a breakdown of the gender of the cases). There were more men among the cases, and mean age of all cases was 51.7[±8.3] years old. There were more former-smokers than never-smokers and current smokers. With regard to drinking status, most participants consumed 2–6 standard drinks/day, and only 3.7% had a high alcohol intake (over 6 standard drinks/day). The commonest longest-held occupation was ‘clerical’ (19.7%), least in number was ‘security’ (0.9%).
Table 1. Baseline characteristics of cases and controls.
Odds of IBD, UC and CD among longest-held occupation
ORs [95%CIs] for each occupational category are shown in and in IBD, CD and UC. Compared with ‘managers’ as reference, the ORs for IBD were higher among ‘service’ (ORs 2.15 [95%CIs 1.12–4.16], 2.15 [1.11–4.16] and 2.30 [1.16–4.56] in model 1, 2 and 3, respectively) and ‘manufacture’ (2.09 [1.14–3.82], 2.00 [1.09–3.67] and 2.17 [1.16–4.09], respectively) in models 1, 2 and 3. The ORs of ‘professional’ were higher in model 1 (1.85 [1.02–3.36]) only and were insignificant after adjusting for alcohol consumption and smoking status. The ORs for CD were not a significant increase or decrease for all models.
Figure 2. Occupational risk of IBD, CD and UC by the longest-held occupational category. The odds ratios (ORs, sign: marker) and 95% confidence intervals (CIs, sign: bar) were estimated by conditional logistic regressions with multiple imputation, matched for age, sex, admission year, hospital, adjusted for smoking status and alcohol consumption. *The 95%CIs did not cross the 1.0 line.
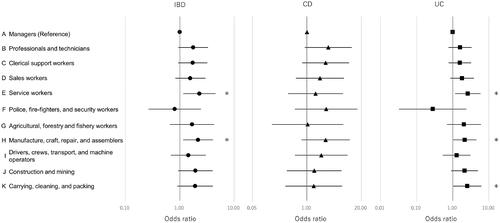
Table 2. Odds ratios (ORs) and 95% confidence intervals (CIs) for IBD, CD and UC by the longest-held occupational category.
For UC, the ORs were higher among ‘service’ (2.62 [1.18–5.82]) and ‘manufacture’ (2.15 [1.04–4.47]) similar to IBD. In addition, the ORs of UC were higher for ‘carrying, cleaning, packing’ in all models (2.36 [1.02–5.45], 2.32 [1.00–5.36] and 2.52 [1.04–6.09], respectively).
Odds of IBD, UC and CD among longest-held occupation by gender
For men, the OR for IBD was higher for ‘manufacture’ (2.11 [1.09–4.05]). Because there were no female managers, ‘homemaker, and inoccupation’ which was the most common category among women, they were divided into two groups; ‘homemaker’ and ‘inoccupation and else’ (see Supplementary Table 1). Changing the reference category to ‘homemaker’ in women increased the ORs of IBD (2.41 [1.37–4.22]) and UC (2.68 [1.39–5.14]) among ‘service.’
Odds of IBD, CD and UC for OPA levels
shows the ORs [95%CIs] for disease for each OPA group. The ORs for IBD did not vary with changing OPA. The ORs for CD decreased with higher OPA levels (p for trend <.05) in all models. Conversely, the ORs for UC were higher (p for trend <.05) in model 3.
Table 3. Odds ratios (ORs) and 95% confidence intervals (CIs) for IBD, CD and UC by OPA levels.
Odds of IBD, CD and UC for OPA levels by gender
When our analyses were limited to men, similar tendencies as those seen when analysing all patients were observed for IBD, CD and UC, and there were no statistically significant differences. Among women, due to the small number of participants in the high OPA group, a similar analysis was not possible. However, the ORs for IBD, CD and UC for the intermediate OPA group after adjusting for alcohol consumption and smoking status were 1.11 [0.76–1.62], 0.40 [0.17–0.96] and 1.53 [1.00–2.35], respectively.
To confirm our findings, changing the controls from three to five gave similar results to those obtained using four controls per case in analyses on both the longest-held occupations and OPA levels (Supplementary Tables 2 and 3).
Discussion
Our case-control study revealed the differential odds of later-onset for CD and UC among longest-held occupations in Japan. The odds for UC were higher among sales workers, and carrying, cleaning, and packing workers; however, the odds for CD did not vary by occupation. Interestingly, higher OPA levels decreased the odds for CD and adversely increased the odds for UC. These results suggest that the OPA level is a determinant for differential occupational risk for developing IBD.
We examined the longest-held occupations and these OPA groups as an ‘exposure’ in this study.
Occupational difference
Our findings were significantly associated with service worker and carrying, cleaning, and packing worker in middle-aged and older people with UC. All adjusted models revealed manufacture workers were at a higher risk for UC. According to a previous study [Citation10], male manufacture workers and female sales, office workers, hairdressers and persons in health occupations had higher prevalence of UC and CD. Our findings also concurred with the results of a previous study [Citation10] regarding UC risk in service workers, which included hairdressers and persons in health occupations. However, with regards to the distribution of occupations among IBD patients, El-Matary et al. [Citation21]. reported that patients with younger-onset IBD tend to attain higher educational levels, and thus are likely to be employed in professional jobs. IBD development in childhood, which could have an impact on job selection, also influences OPA. Therefore, the results of previous studies on occupations with IBD might have been affected by the age at which IBD developed because they included younger-onset of IBD. Whereas in our study, only cases that developed at later-onset were analysed.
Occupational physical activity
Interestingly, the ORs of CD decreased with OPA increase, whereas the ORs of UC increased with OPA levels. CD and UC may have different risk factors about OPA, as is the case that smoking is a risk factor for CD but not for UC [Citation22]. Our results were consistent with the results of previous studies that showed that higher physical activity was associated with a lower risk of CD [Citation20]. Recent molecular evidence suggests that physical activity could induce autophagy involved in the prevention of autoimmune diseases, neurodegenerative diseases and infections [Citation23]. Nucleotide-binding oligomerisation domain containing 2 (NOD2), a genetic variant of CD, was identified as a potent autophagy inducer. It is possible that defects in autophagy inducing factor caused by NOD2 mutation may lead to CD development [Citation24].
Contrarily, in this study, the risk for UC was higher among service workers, manufacture workers, and carrying, cleaning, and packing workers, who were categorised as intermediate and high OPA groups, respectively. Previous epidemiologic studies have not established an association between physical activity and a risk of UC onset [Citation11,Citation20,Citation25]. It is possible that previous studies have failed to provide clear results because of inclusion of patients with both younger- and later-onset of UC. A recent experimental study by Bilski et al. [Citation26] clearly showed that prolonged and extensive exercise could exacerbate the severity of colon damage in mice with 2,4,6-trinitrobenzenesulfonic acid (TNBS)-induced colitis. The phenomena that extensive exercise decreases mucosal microcirculation and induces HIF-1α and proinflammatory genes were mainly clearly in obese mice fed on a high lipid diet. High OPA might cause some detrimental effects such as a fall in mucosal microcirculation and imbalance of oxidative stress on the intestinal mucosa of the colon, particularly in older persons who have more intestinal fat than younger persons.
In our study, professionals and technicians (low OPA groups) had the highest risk for CD (OR [95%CIs] 3.24 [0.90–11.64]), but this did not attain statistical significance. In combination with findings from previous studies, we infer that professionals and technicians with low OPA might be at risk for CD; our study might be caused due to the small number of participants in these occupational categories.
The physical activity paradox
It is possible that high OPA levels correspond to prolonged and high-intensity exercise, which is known as ‘the physical activity paradox.’ Although physical activity improves health, this relationship has been restricted to LTPA. Many epidemiological studies documented that high OPA increases the risk for cardiovascular disease (CVD) and all-cause mortality, even after extensive adjustments for other risk factors, including socioeconomic status, LTPA and other health behaviors [Citation27,Citation28]. The reason why caused this OPA paradox was pointed as follows: (1) OPA is of extremely low intensity or extremely long durations unsuitable for maintenance, (2) OPA elevates 24-hour heart rate and 24-hour blood pressure and (3) OPA is often performed without sufficient recovery time, and so on [Citation29]. The OPA mechanism seems to be different among the onset between CVD and IBD. However, this study shows that the OPA paradox could be capable of adapting to IBD patients.
The difference between UC and CD in our study was only significant in the high OPA group, but not in the intermediate OPA group. A recent study about LTPA with IBD patients reported that repeated moderate-intensity exercises did not affect inflammatory markers in IBD patients, such as cytokine responses [Citation30]. Although this study was for a short period with a small sample size, repeated moderate-intensity exercises could be safe and beneficial in health promotion. The intermediate OPA group may not be significant because intermediate OPA had been equally repeated with moderate-intensity exercises. We cannot deny the possibility that only the long period and high intensity repeated physical activity could be adapted to considering the OPA paradox in IBD.
Further detailed studies are needed as OPA may not be directly and fully representative of DPA.
Strengths and limitations
This study had some strengths. First, we used a large database with more than 300,000 inpatients and their clinical and occupational histories. For this reason, our results are likely to be representative of the entire Japanese population. Second, health information managers (HIMs) qualified in Japan interviewed inpatients or their families about occupational and lifestyle information. HIMs are specialists trained in medical coding and thus could accurately register and code this information. The definitive diagnoses were reliable as they were obtained from summaries written by clinical doctors. Third, this study used the longest-held occupation as an exposure variable to minimise the possibility of occupational change influencing the risk of developing IBD.
There were some limitations. The onset of disease was connected to the date of the first hospitalisation, which might not concur with disease onset due to previous outpatient IBD treatments. As Rosai Hospital Group has played a role as a core hospital in each medical region, even if patients with IBD were admitted to the hospital for the first time, they might have an onset of childhood or adolescence. Therefore, in the cases to be analysed, it is impossible to distinguish between patients with onset after the age of 40 years and those with onset before that, and some patients with younger-onset were included. Next, since they are inpatient cases, even at the first onset, hospitalisation is to apply the first remission therapy to those who have moderate or more systemic symptoms according to IBD treatment guideline [Citation31]. Basically, our findings and interpretation are suitable for IBD patients with moderate or severe grades. Thus, for patients who have been controlled by only outpatient treatments, further outpatient-based studies are needed. Moreover, we were unable to obtain the data on drugs administered, patients’ symptoms, and a history of appendectomy. Psychological stress is associated with an exacerbation of IBD [Citation32]. These information may have been invariably reported, but was not consistently observed.
Conclusions
Our case-control study showed that the risk due to OPA levels was inversely associated between CD and UC. This suggested that long-term effects of physical activity on the onset of IBD could be complex. Future studies are needed to clarify the association between long-term OPA and IBD onset by disease type (CD and UC), age of onset (younger- and later-onset) and disease severity (in- or outpatients).
Author contributions
NK, KH, AT and MT received funding acquisition and collected data. YF, KF and SN designed this study and analysed the data. YF, KF and MT wrote the paper. KF, NK, KH, AT and MT supervised this study and provided critical comments. All authors reviewed the manuscript.
Supplemental Material
Download PDF (82.5 KB)Acknowledgements
The authors express gratitude to all the study staff in JOHAS for their commitment to data collection.
Disclosure statement
The authors report no conflict of interest.
Data availability statement
The datasets are not publicly available due to restrictions used under the license for the current study. There are available on reasonable request from the corresponding author.
Additional information
Funding
References
- Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet. 2017;390(10114):2769–2778.
- Kaplan GG, Ng SC. Understanding and preventing the global increase of inflammatory bowel disease. Gastroenterology. 2017;152(2):313–321.
- Sonnenberg A. Disability from inflammatory bowel disease among employees in West Germany. Gut. 1989;30(3):367–370.
- Bøggild H, Tüchsen F, Orhede E. Occupation, employment status and chronic inflammatory bowel disease in Denmark. Int J Epidemiol. 1996;25(3):630–637.
- Jiang L, Xia B, Li J, et al. Retrospective survey of 452 patients with inflammatory bowel disease in Wuhan city, Central China. Inflamm Bowel Dis. 2006;12:212–217.
- Sonnenberg A, Walker JT. Occupational mortality associated with inflammatory bowel disease in the United States 1984–1998. Inflamm Bowel Dis. 2012;18(7):1249–1253.
- Liu S, Ding J, Wang M, et al. Occupational risk for Crohn's disease: a two-center study. Dig Liver Dis. 2016;48(11):1318–1322.
- Marri SR, Buchman AL. The education and employment status of patients with inflammatory bowel diseases. Inflamm Bowel Dis. 2005;11(2):171–177.
- Leso V, Ricciardi W, Iavicoli I. Occupational risk factors in inflammatory bowel disease. Eur Rev Med Pharmacol Sci. 2015;19:2838–2851.
- Sonnenberg A. Occupational distribution of inflammatory bowel disease among German employees. Gut. 1990;31(9):1037–1040.
- Wang Q, Xu KQ, Qin XR, et al. Association between physical activity and inflammatory bowel disease risk: a meta-analysis. Dig Liver Dis. 2016;48:1425–1431.
- Piovani D, Danese S, Peyrin-Biroulet L, et al. Environmental risk factors for inflammatory bowel diseases: an umbrella review of meta-analyses. Gastroenterology. 2019;157(3):647–659.e4.
- Fukushima N, Kitabayashi M, Kikuchi H, et al. Comparison of accelerometer-measured sedentary behavior, and light- and moderate-to-vigorous-intensity physical activity in white- and blue-collar workers in a Japanese manufacturing plant. J Occup Health. 2018;60(3):246–253.
- Rasmussen NF, Bech BH, Rubin KH, et al. Associations between participation in, intensity of, and time spent on leisure time physical activity and risk of inflammatory bowel disease among older adults (PA-IBD): a prospective cohort study. BMC Public Health. 2021;21(1):634.
- Kaneko R, Zaitsu M, Sato Y, et al. Risk of cancer and longest-held occupations in Japanese workers: a multicenter hospital-based case-control study. Cancer Med. 2019;8(13):6139–6150.
- Fukai K, Kojimahara N, Hoshi K, et al. Combined effects of occupational exposure to hazardous operations and lifestyle-related factors on cancer incidence. Cancer Sci. 2020;111(12):4581–4593.
- Zaitsu M, Kato S, Kim Y, et al. Occupational class and risk of cardiovascular disease incidence in Japan: nationwide, multicenter, hospital-based case-control study. J Am Heart Assoc. 2019;8(6):e011350.
- Steeves JA, Tudor-Locke C, Murphy RA, et al. Classification of occupational activity categories using accelerometry: NHANES 2003–2004. Int J Behav Nutr Phys Act. 2015;12:89.
- Kalinowski A, Humphreys K. Governmental standard drink definitions and low-risk alcohol consumption guidelines in 37 countries. Addiction. 2016;111(7):1293–1298.
- Khalili H, Ananthakrishnan AN, Konijeti GG, et al. Physical activity and risk of inflammatory bowel disease: prospective study from the Nurses’ Health Study cohorts. BMJ. 2013;347(4):f6633.
- El-Matary W, Dufault B, Moroz SP, et al. Education, employment, income, and marital status among adults diagnosed with inflammatory bowel diseases during childhood or adolescence. Clin Gastroenterol Hepatol. 2017;15(4):518–524.
- Mahid SS, Minor KS, Soto RE, et al. Smoking and inflammatory bowel disease: a meta-analysis. Mayo Clin Proc. 2006;81(11):1462–1471.
- He C, Bassik MC, Moresi V, et al. Exercise-induced BCL2-regulated autophagy is required for muscle glucose homeostasis. Nature. 2012;481(7382):511–515.
- Fritz T, Niederreiter L, Adolph T, et al. Crohn's disease: NOD2, autophagy and ER stress converge. Gut. 2011;60(11):1580–1588.
- Ng SC, Tang W, Leong RW, et al. Environmental risk factors in inflammatory bowel disease: a population-based case-control study in Asia-Pacific. Gut. 2015;64(7):1063–1071.
- Bilski J, Mazur-Bialy A, Wojcik D, et al. Effect of forced physical activity on the severity of experimental colitis in normal weight and obese mice. Involvement of oxidative stress and proinflammatory biomarkers. Nutrients. 2019;11(5):1127.
- Quinn TD, Yorio PL, Smith PM, et al. Occupational physical activity and cardiovascular disease in the United States. Occup Environ Med. 2021;78(10):724–730.
- Coenen P, Huysmans MA, Holtermann A, et al. Do highly physically active workers die early? A systematic review with meta-analysis of data from 193 696 participants. Br J Sports Med. 2018;52(20):1320–1326.
- Holtermann A, Krause N, van der Beek AJ, et al. The physical activity paradox: six reasons why occupational physical activity (OPA) does not confer the cardiovascular health benefits that leisure time physical activity does. Br J Sports Med. 2018;52(3):149–150.
- Lamers CR, de Roos NM, Bongers CCWG, et al. Repeated prolonged moderate-intensity walking exercise does not appear to have harmful effects on inflammatory markers in patients with inflammatory bowel disease. Scand J Gastroenterol. 2021;56(1):30–37.
- Hisamatsu T. Research on intractable inflammatory bowel disease. Diagnostic criteria & treatment guidelines of ulcerative colitis and Crohn’s disease. 2021–03; 2021 [cited 2021 Sep 30] (in Japanese). Available from: http://www.ibdjapan.org/pdf/doc01.pdf
- Bernstein CN, Singh S, Graff LA, et al. A prospective population-based study of triggers of symptomatic flares in IBD. Am J Gastroenterol. 2010;105(9):1994–2002.