Abstract
Objective
To study the changes in prevalence of irritable bowel syndrome (IBS), the distribution between the sexes and age groups, and risk factors for the disease and its subtypes.
Material and methods
Every inhabitant of Nord-Trøndelag county, Norway, over 20 years of age was invited to participate in the Trøndelag Health Study (HUNT). In HUNT3 (2006–2008) and HUNT4 (2017–2019), IBS was assessed by a questionnaire. The standardized prevalence was calculated, and risk factors were assessed by multivariable logistic regression, reporting odds ratios (OR) and 95% confidence intervals (CI).
Results
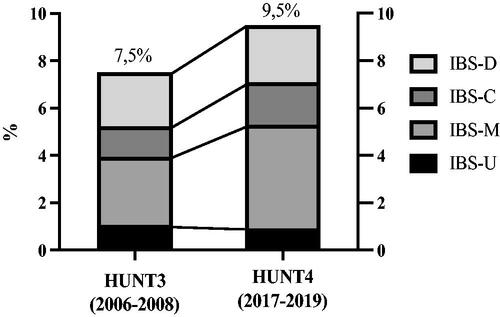
In HUNT3 and HUNT4, 41,198 and 42,669 individuals were included, respectively. The prevalence of IBS was 7.5% in HUNT3 and 9.5% in HUNT4. Both surveys showed higher prevalence among women and among young adults. In HUNT4, the most prevalent subtype was mixed IBS (46.1%). Women had increased risk of IBS compared to men (OR 1.82, 95% CI 1.69–1.96). Age ≥40 years decreased the risk of IBS compared to age <40 years (OR 0.82, 95% CI 0.75–0.90). Being unmarried increased the risk for IBS compared to being married (OR 1.21, 95% CI 1.11–1.32). Both previous (OR 1.28, 95% CI 1.20–1.38) and current (OR 1.35, 95% CI 1.20–1.51) smokers had increased risk of IBS compared to never smokers.
Conclusions
IBS is a prevalent disease, and the prevalence has increased between 2006–2008 and 2017–2019. Risk of IBS was increased among women, young adults, smokers and unmarried participants.
Keywords:
Introduction
Irritable bowel syndrome (IBS) is a chronic functional gastrointestinal disorder which is characterized by abdominal pain and changes in bowel habits (e.g. constipation and/or diarrhoea) [Citation1]. IBS is diagnosed using both inclusion and exclusion criteria. Several symptom-based criteria have been proposed. One of the most used is the ‘Rome criteria’ set forth by the Rome Foundation which are viewed as positive criteria for IBS, meaning that fulfilment of the criteria is sufficient to diagnose the patient. The Rome criteria has been revised several times, and in 1999 the Rome II criteria was released () [Citation2]. The latest set of criteria, the Rome IV criteria, was proposed in 2016 and includes criteria for subgroups of IBS: diarrhoea-predominant IBS (IBS-D); constipation-predominant IBS (IBS-C); IBS with mixed bowel habits (IBS-M); and unsubtyped IBS (IBS-U) () [Citation3]. The criteria for the subgroups are based on the Bristol stool form scale (BSFS) () [Citation4].
IBS has a pooled global prevalence of 11.2% and is more prevalent among women [Citation5]. Most of the studies on IBS have been conducted in European and North-American populations, and few population-based studies following the same population over a longer period have been conducted.
The prevalence of IBS is believed to be increasing for both sexes and in all age groups and the risk is expected to be higher among women and young adults [Citation5,Citation6]. Based on existing research, it is believed that being overweight and being married will decrease the risk of IBS [Citation7,Citation8]. It is also believed that there might be an association between smoking and IBS [Citation9].
The aims of this study were to study the changes in prevalence of IBS and its subtypes over time in the same population, the differences in prevalence between the sexes and different age groups and risk factors of IBS in the general population.
Material and methods
Population and questionnaires
This was a population-based study based on data from the Trøndelag Health Study (HUNT) [Citation10], which is a collaboration between HUNT Research Centre (Faculty of Medicine and Health Sciences, Norwegian University of Science and Technology NTNU), Trøndelag County Council, Central Norway Regional Health Authority, and the Norwegian Institute of Public. The health survey has been repeated four times since the mid-1980s: HUNT1 in 1984–1986, HUNT2 in 1995–1997, HUNT3 in 2006–2008 and HUNT4 in 2017–2019. All inhabitants of the county from 20 years of age have been invited to participate. The participants have completed several questionnaires and anthropometric measurements have been performed. In HUNT3 and HUNT4, the questionnaires included questions based on the Rome II criteria for IBS ().
Study specific definition of IBS
From the questionnaires in HUNT, individuals that met the criteria for an IBS diagnosis were identified. Individuals reporting abdominal pain or discomfort the last 12 months and reporting two or more of the additional symptoms were defined with IBS ().
Box 1. The Rome II criteria.
Box 2. The Rome IV criteria for the subtypes of irritable bowel syndrome (IBS).
Box 3. The Bristol stool form scale (BSFS).
Box 4. The Rome II questions in the HUNT questionnaires.
Study specific definition of IBS subtypes
Based on the participants’ reply about gastrointestinal symptoms () and the Rome IV criteria for subtypes (), the IBS subtypes were defined based on the following algorithm:
IBS-D: ‘a little’ or ‘much’ diarrhoea and ‘never’ obstipation
IBS-C: ‘never’ diarrhoea and ‘a little’ or ‘much’ obstipation
IBS-M: ‘a little’ or ‘much’ diarrhoea and ‘a little’ or ‘much’ constipation, and ‘a little’ or ‘much’ alternating diarrhoea/obstipation
IBS-U: not fulfilling the criteria for IBS-D, IBS-C or IBS-M.
Risk factors
Information on sex and age was collected from the National Population Register. The participants were asked about the marital status, to which they replied unmarried, married, widowed, divorced or separated. They were also asked about smoking habits and replied either never smoked, ex-smoker, daily smoker or occasional smoker. Weight and height, needed to calculate the body mass index (BMI), was taken by trained personnel at screening stations during the HUNT surveys.
Statistical analysis
Sex and age adjusted prevalence was calculated based on data from Statistics Norwegian on the total population of Nord-Trøndelag county in 2011. The prevalence was calculated for each sex and for the different age groups (<30, 30–39, 40–49, 50–59, 60–69, 70–79 and ≥80). Multivariable logistic regression reporting odds ratios (OR) and 95% confidence intervals (CI) was performed for each of the five outcomes (IBS, IBS-D, IBS-C, IBS-M and IBS-U), adjusted for sex, age, marital status, smoking and BMI. In the regression model, age was divided into <40 and ≥40 years of age. Marital status was divided into (1) married; (2) separated, divorced or widowed and (3) single or unmarried. Smoking was categorized into never, previous and current (daily or occasional) smokers. BMI was categorized into underweight (<18.5 kg/m2), normal weight (18.5–25 kg/m2) or overweight (>25 kg/m2).
Results
Characteristics of study population
In HUNT3, there were 50,800 participants (54% of the invited), and in HUNT4, there were 56,042 participants (54%), of whom 33,819 participated in both (). The Rome II questions were answered by 41,198 participants in HUNT3 and 42,669 participants in HUNT4. The distribution of sex, age, marital status and BMI was consistent in the two surveys. Women made up 56.2% of the study population in HUNT3 and 57.2% in HUNT4. The mean age of the population was 54.4 years in HUNT3 and 56.2 years in HUNT4, and 60.7% reported to be married in HUNT3 and 54.9% in HUNT4. There were fewer current smokers in HUNT4 compared to HUNT3 (9.4% and 22.6%, respectively). Mean BMI was 27.2 in both surveys.
Table 1. Characteristics of the study population.
Prevalence of IBS
The sex- and age-adjusted prevalence of IBS was 7.5% (95% CI 7.2–7.7) in HUNT3 (2006–2008) and 9.5% (95% CI 9.2–9.8) in HUNT4 (2017–2019) (). IBS was more prevalent among women (8.9% in HUNT3 and 12.1% in HUNT4) than among men (6.0% in HUNT3 and 7.1% in HUNT4). The prevalence was highest in young adults (11.5%, 95% CI 10.9–12.2 among participants under 40 years) and decreased with advancing age (8.9%, 95% CI 8.6–9.2 among the participants over 40 years) (). Most of the participants with IBS reported not to smoke (72.4% in HUNT3 and 89.0% in HUNT4), and there was a reduction in the number of current smokers between the studies (27.6% in HUNT3 and 11.0% in HUNT4).
Figure 1. Age distribution of IBS in HUNT4. The prevalence of IBS (black line) with 95% confidence interval (grey area) distributed among the different age groups (x-axis). HUNT4: the fourth Trøndelag Health Study; IBS: irritable bowel syndrome.
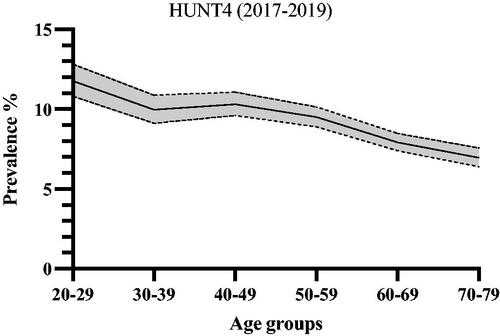
Table 2. Sex- and age-adjusted prevalence of IBS and its subtypes.
The most common subtype of IBS was IBS-M in both surveys (38.6% in HUNT3 and 46.1% in HUNT4), followed by IBS-D (30.3% in HUNT3 and 23.8% in HUNT4) ( and ). IBS-D was more prevalent among men (38.7% in HUNT3 and 32.8% in HUNT4) than women (21.5% in HUNT3 and 17.6% in HUNT4) and IBS-C was more prevalent among women (21.9% in HUNT3 and 23.9% in HUNT4) than men (12.5% in HUNT3 and 14.4% in HUNT4).
Risk of IBS
The risk estimates for IBS were comparable between HUNT3 and HUNT4 ( and ). In HUNT4, the risk of IBS was increased among women compared to men (adjusted OR 1.82, 95% CI 1.69–1.96), and age ≥40 years was associated with decreased risk of IBS (OR 0.82, 95% CI 0.75–0.90). Being unmarried increased the risk of IBS (OR 1.21, 95% CI 1.11–1.32) compared to being married. Both previous (OR 1.28, 95% CI 1.20–1.38) and current (OR 1.35, 95% CI 1.20–1.51) smoking increased the risk of IBS compared to never smoking. The was no significant association between IBS and BMI.
Figure 3. Risk factors for IBS. The adjusted odds ratios with 95% confidence intervals for each risk factor, adjusted for the other risk factors in the figure. Reference values: men, age <40 years, married, non-smoker, normal weight. IBS: irritable bowel syndrome.
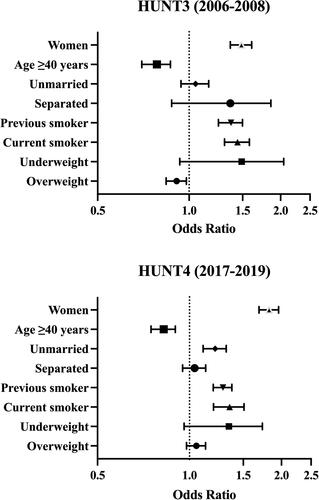
Table 3. Risk factors for IBS.
In contrast to IBS overall, the risk of IBS-D was decreased among women compared to men (OR 0.48, 95% CI 0.41–0.56) () and being unmarried decreased the risk for IBS-C (0.80, 95% CI 0.65–0.99) (). Overweight was associated with decreased risk of IBS-C (OR 0.75, 95% CI 0.64–0.88) () and an increased risk of IBS-M (OR 1.21, 95% CI 1.06–1.39) (). IBS-U was not clearly associated with any of the assessed risk factors ().
Table 4. Risk factors for IBS-D.
Table 5. Risk factors for IBS-C.
Table 6. Risk factors for IBS-M.
Table 7. Risk factors for IBS-U.
Discussion
This population-based cohort study showed that IBS is a common disease with increasing prevalence. IBS was more prevalent among women than men and decreased in prevalence with increasing age. The risk of IBS was increased among women, with age below 40 years, among unmarried participants, and among both current and previous smokers. The risk of IBS-C was increased among women, while the risk of IBS-D was increased among men. The risk of IBS-C was decreased in overweight participants, while the risk of IBS-M was increased in women, current smokers and overweight participants.
The population-based study design reduced the risk of selection bias and made the study representative for the general population. The high number of participants and information on relevant covariables made analyses of IBS subtypes and adjustment for confounders possible. The use of the validated Rome II criteria for IBS reduced misclassification. However, as the Rome II criteria is one of the stricter of all the different criteria for IBS, the prevalence might be underestimated compared to studies that utilize other revisions of the criteria (see below). Of limitations, the low response rate might increase the risk of selection bias. However, as the study was a general health study, the selection was probably non-differentially related to IBS. The study also lacked information about other gastrointestinal disorders with similar symptoms among the participants. However, the Rome criteria are considered positive criteria for IBS. In the Rome IV criteria, the BSFS is used to subtype IBS, while the present study used data on the subjective perception of symptoms reported by the participants only. However, the grade of which the participants reported diarrhoea, constipation and mixed symptoms was converted into a score which corresponds to the BSFS.
A few studies have assessed the differences between the Rome II, III and IV criteria and their effects on epidemiologic studies. One study from 2007 on an Israeli population found that the Rome II criteria produced a significantly lower prevalence of IBS compared to the Rome III criteria [Citation11]. The Rome III criteria also increases the prevalence compared to the Rome IV criteria [Citation12]. The severity of symptoms was higher in the groups that kept the diagnosis when the Roma IV-criteria was used, compared to using the Rome III criteria [Citation13,Citation14]. Thus, the present study using the Rome II criteria might present a conservative estimate of the prevalence of IBS. One study from 2003 suggests a pooled overall prevalence of IBS of 11.5% in eight European countries with a wide geographical variation [Citation15]. In a population-based study from 2006 with 4622 participants from Oppland County in Norway, the prevalence was estimated to 8.4% utilizing the Rome II criteria [Citation16]. A meta-analysis based on publications between 2006 and 2020 of 53 studies with a total of 395,385 participants found a pooled prevalence of 9.2% when the Rome III criteria was used [Citation12]. These studies of prevalence are well in line with the results from the present study; however, none of these have assessed the change in prevalence over time in the same population while also stratifying for the subtypes for IBS.
The meta-analysis from 2020 also found higher prevalence and increased risk of IBS among women (OR 1.46, 95% CI 1.33–1.59) [Citation12]. Comparable odds ratios have also been found in a meta-analysis utilizing the Rome II criteria [Citation6]. These results resonate well with our findings of observed prevalence and the impact of sex on the diagnosis. In a meta-analyses of 80 studies with a total of 260,960 participants, the risk of IBS was reduced with increasing age (OR 0.75, 95% CI 0.62–0.92 with age above 50) [Citation5]. This is comparable with the results of the present study. Reasons for this difference in risk of IBS with age is not clear, but suggestions have been made regarding stress and uncertain life situations as possible causes of the increased risk in younger age groups [Citation7]. A Korean study from 2006 with 1066 participants found that being married reduced the risk of IBS compared to being single or divorced (OR 0.59, 95% CI 0.35–0.99) [Citation7]. However, this association was not found in the study of 3022 participants from Olmsted county in Minnesota, USA [Citation17]. Different cultural and social settings between Eastern and Western countries could, in part, explain this geographical difference in terms of risk. The present study showed that being unmarried increased the risk of IBS when compared to married participants. Being separated, divorced or widowed, however, did not have a significant effect on risk when compared to being married. Our hypothesis was therefore not confirmed. A small cross-sectional study conducted in Karachi, Pakistan, looked specifically on the occurrence of IBS in a selection of smokers and non-smokers. The study found that non-smokers were more likely to have IBS (OR 3.00, 95% CI 1.23–7.30) [Citation18]. However, a Lebanese study of 553 participants could not find an association between smoking and IBS [Citation19]. A systematic review published in 2017 compared smoking prevalence between subjects with and without IBS in 33 publications and could not find an association between the two, but the authors suggested that stratifying for the subtypes of IBS is needed to better understand the connection [Citation9]. In the present study, a dimensional analysis was conducted on smoking, including never, previous and current smoking, on IBS and all its subgroups. These analyses showed that current and previous smoking increased the risk of IBS overall and IBS-M compared to never smoking, thus supporting the hypothesis of an association between smoking and IBS. The data on smoking habits was only qualitative and the quantitative association between amount of smoking and IBS was not assessed. A Swedish study from 2021 studied smoking as a potential risk factor, including information on the number of cigarettes smoked a day. They found a significantly increased risk for IBS-D among heavy smokers (≥20 cigarettes/day) but no association between number of cigarettes smoked a day and IBS-C or IBS-M [Citation20]. In a Japanese study from 2021, a small decreased risk of IBS was found with increasing BMI (OR 0.92, 95% CI 0.88–0.95, for each unit increase in BMI) [Citation8]. In the present study, overweight did not have an impact on the risk of IBS overall, but increased the risk of IBS-M and decreased the risk of IBS-C.
IBS has negative effects on health-related quality of life [Citation21] and is associated with psychiatric and somatic comorbidities [Citation16]. It is generally underdiagnosed [Citation22] and has the potential to cause extensive use of medical resources [Citation23], but a better understanding of the epidemiologic characteristics of IBS will help the clinicians in the diagnostic process. The present study shows that the disease is common, that it is getting more prevalent, and that the prevalence of IBS and its subtypes is dependent on sex and age. Smoking was associated with IBS and prevention of smoking or smoking cessation could be beneficial for the prevalence of IBS. The risk factors acted differently on the different subtypes of IBS, which could imply that the subtypes might be fundamentally different conditions that should be managed differently.
Conclusion
The prevalence of IBS was high and seems to be increasing in this general population followed over time. The risk was higher among women, young adults, smokers and unmarried participants. The risk factors differed between the IBS subtypes, which could imply that the subtypes are fundamentally different conditions that should be managed differently.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Longstreth GF, Thompson WG, Chey WD, et al. Functional bowel disorders. Gastroenterology. 2006;130(5):1480–1491.
- Drossman DA. The functional gastrointestinal disorders and the Rome II process. Gut. 1999;45(Suppl 2):II1–5.
- Drossman DA, Hasler WL. Rome IV-Functional GI disorders: disorders of gut-brain interaction. Gastroenterology. 2016;150(6):1257–1261.
- Lewis SJ, Heaton KW. Stool form scale as a useful guide to intestinal transit time. Scandinavian Journal of Gastroenterology. 1997;32(9):920–924.
- Lovell RM, Ford AC. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol. 2012;10(7):712–721.e4.
- Lovell RM, Ford AC. Effect of gender on prevalence of irritable bowel syndrome in the community: systematic review and meta-analysis. Am J Gastroenterol. 2012;107(7):991–1000.
- Han SH, Lee OY, Bae SC, et al. Prevalence of irritable bowel syndrome in Korea: population-based survey using the Rome II criteria . J Gastroenterol Hepatol. 2006;21(11):1687–1692.
- Kubo M, Fujiwara Y, Shiba M, et al. Differences between risk factors among irritable bowel syndrome subtypes in Japanese adults. Neurogastroenterol Motil. 2011;23(3):249–254.
- Sirri L, Grandi S, Tossani E. Smoking in irritable bowel syndrome: a systematic review. J Dual Diagn. 2017;13(3):184–200.
- Krokstad S, Langhammer A, Hveem K, et al. Cohort profile: the HUNT study, Norway. Int J Epidemiol. 2013;42(4):968–977.
- Sperber AD, Shvartzman P, Friger M, et al. A comparative reappraisal of the Rome II and Rome III diagnostic criteria: are we getting closer to the ‘true’ prevalence of irritable bowel syndrome? Eur J Gastroenterol Hepatol. 2007;19(6):441–447.
- Oka P, Parr H, Barberio B, et al. Global prevalence of irritable bowel syndrome according to Rome III or IV criteria: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(10):908–917.
- Vork L, Weerts Z, Mujagic Z, et al. Rome III vs Rome IV criteria for irritable bowel syndrome: a comparison of clinical characteristics in a large cohort study. Neurogastroenterol Motil. 2018;30(2):e13189.
- Aziz I, Törnblom H, Palsson OS, et al. How the change in IBS criteria from Rome III to Rome IV impacts on clinical characteristics and key pathophysiological factors. Am J Gastroenterol. 2018;113(7):1017–1025.
- Hungin AP, Whorwell PJ, Tack J, et al. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment Pharmacol Ther. 2003;17(5):643–650.
- Vandvik PO, Lydersen S, Farup PG. Prevalence, comorbidity and impact of irritable bowel syndrome in Norway. Scand J Gastroenterol. 2006;41(6):650–656.
- Talley NJ, Zinsmeister AR, Melton LJ. 3rd. Irritable bowel syndrome in a community: symptom subgroups, risk factors, and health care utilization. Am J Epidemiol. 1995;142(1):76–83.
- Mahmood K, Riaz R, U, Haq MS, et al. Association of cigarette smoking with irritable bowel syndrome: a cross-sectional study. Med J Islam Repub Iran. 2020;34:72.
- Chatila R, Merhi M, Hariri E, et al. Irritable bowel syndrome: prevalence, risk factors in an adult Lebanese population. BMC Gastroenterol. 2017;17(1):137.
- Talley NJ, Powell N, Walker MM, et al. Role of smoking in functional dyspepsia and irritable bowel syndrome: three random population-based studies. Aliment Pharmacol Ther. 2021;54(1):32–42.
- El-Serag HB. Impact of irritable bowel syndrome: prevalence and effect on health-related quality of life. Rev Gastroenterol Disord. 2003;3 Suppl 2 (Suppl 2):S3–S11.
- Heaton KW, O'Donnell LJ, Braddon FE, et al. Symptoms of irritable bowel syndrome in a British urban community: consulters and nonconsulters. Gastroenterology. 1992;102(6):1962–1967.
- Sandler RS, Everhart JE, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122(5):1500–1511.