Abstract
Introduction
Congenital diaphragmatic hernias (CDHs) in adults remain rare, with limited data on them available. However, CDHs can cause respiratory and gastrointestinal symptoms in adults, even resulting in the strangulation of the bowel when incarcerated. Here, we aimed to analyze surgical outcomes among adult patients. The primary outcome of interest was the complication rate, reoperations and 90-day mortality after laparoscopic and open hernia repair.
Methods
We identified all adult patients diagnosed with a Morgagni or Bochdalek hernia treated operatively between 2010 and 2019 in a single tertiary care hospital. Data on patient demographics, surgical characteristics, mortality and morbidity were collected.
Results
In total, we identified 37 patients (67.6% female; average age, 57 years). Overall, 78.4% patients underwent minimally invasive operations, while 35.1% underwent emergency operations. A Clavien–Dindo grade II–V complication was experienced by 18.9% of patients. No deaths occurred within 90 days of surgery, and we detected no recurrences in short-term or long-term follow-up. A minimally invasive technique correlated with a shorter hospital stay of 3.6 days versus 6.8 days in the open surgery group (p = .007, t = 3.3, 95% confidence interval = 1.04−5.21).
Conclusion
Our findings indicate that the laparoscopic repair of a congenital diaphragmatic hernia is safe and effective, offering short hospital stay and a low amount of complications.
Introduction
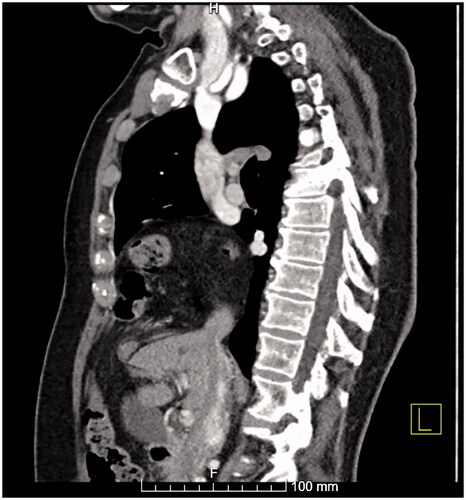
Congenital diaphragmatic hernias (CDHs) arise when the fusion of the diaphragm remains incomplete during embryologic development. A Bochdalek hernia (), situated in the posterolateral location, accounts for about 95% of CDHs occurring in infants [Citation1]. Bochdalek hernias often present as acute respiratory distress during the neonatal period due to a large hernia sac displacing the lung in the thoracic cavity. Clinical incidence in adult populations is low, with prevalence in the adult population reaching 0.17% to 12.7% given estimates from imaging study reviews [Citation2–5].
Figure 1. A sagittal view of a left-sided Bochdalek hernia from a CT scan. Omental fat as well as the left kidney can be seen herniating through the posterolateral hernia defect in the diaphragm.

A Morgagni hernia (), comprising only 2% to 4% of all CDHs, occurs in the anteromedial part of the diaphragm [Citation6]. Although predominantly diagnosed during infancy, a Morgagni hernia often remains undiagnosed during childhood due to less severe symptoms [Citation7]. An incidental asymptomatic hernia is occasionally discovered during radiological imaging, although the prevalence of Morgagni hernias in the adult population is unconfirmed [Citation8].
Figure 2. A sagittal view of a Morgagni hernia from a CT scan showing the defect in the anteromedial part of the diaphragm and the bowel herniated into the thoracic cavity.
In cases where an adult patient is diagnosed with a Morgagni or Bochdalek hernia, surgical treatment is typically recommended in order to avoid medical emergencies such as incarceration or strangulation of the bowel [Citation7,Citation9,Citation10]. Furthermore, the hernia sac tends to enlarge over time, causing symptoms to exacerbate [Citation9].
Several operative approaches to repair CDHs have been described. In addition to traditional open surgery through thoracotomy, sternotomy or laparotomy, minimally invasive repair may be performed employing either thoracoscopy or laparoscopy [Citation7,Citation11–14].
Because of the rarity of these conditions, research concerning the surgical treatment of CDHs in adults is sparse, with evidence largely stemming from case reports and series [Citation15,Citation16]. In a recent study, laparoscopic repair resulted in a shorter hospital stay and a recurrence rate comparable to open repair [Citation9].
Thus, we aimed to examine a large cohort of patients operated on for CDH in adulthood. In addition, we sought to compare results from open and minimally invasive surgical procedures and identify features leading to adverse events.
Patients and methods
In this retrospective case series, we examined adult patients operated on for CDH between 2010 and 2019 in a single tertiary care hospital, Helsinki University Hospital. From the electronic medical records (EMRs), we identified all patients operated on for a Morgagni or Bochdalek hernia, including patients who underwent both elective and emergency operations. We excluded acquired paraesophageal hernias and traumatic diaphragmatic hernias.
From the patients identified, we extracted the following demographic data: age at the time of surgery, gender, medical comorbidities, smoking status, preoperative body mass index (BMI) and presenting symptoms. Operative reports were collectively reviewed to determine the surgical approach, the duration of the operation, the contents of the hernia sac, the use of mesh during repair and the extent of hernia sac dissection. Data on hospital stay, complications, readmissions, reoperations and mortality were also collected. We used the Clavien–Dindo classification to categorize complications [Citation17]. Follow-up consisted of a postoperative visit with chest radiograph at 6 weeks from the operation. After that point, additional follow-up visits and imaging were arranged based on referrals to our clinic for recurring symptoms. For asymptomatic or non-referred patients, the researchers evaluated imaging studies of the patients (chest radiographs, computed tomography scans) and symptomology from the national health records.
Preoperative imaging was analyzed collectively for the size of the intrathoracic hernia sac, defined as the longest length of the defect in a computed tomography (CT) scan. If a CT scan was unavailable, we reviewed the surgical report to determine the hernia size. Postoperative follow-up reports and imaging were studied for possible recurrence.
The operating surgeon chose the approach for each patient. Obesity, previous abdominal surgeries, signs of bowel incarceration and/or perforation were possible reasons for the open approach.
We analyzed all data using IBM SPSS Statistics, version 24. In our statistical analyses, we used the Fisher’s exact test to compare categorical variables and the two-sample t-test or Wilcoxon-Mann Whitney test, depending on the normality of the data, to compare continuous variables between groups, Kruskal Wallis test was used to compare the relationship between two continuous variables. Logistic regression allowed us to determine pre-existing conditions possibly associated with treatment outcomes.
Results
Between 2009 and 2019 a total of 37 patients underwent surgical repair for CDH: 30 with a Morgagni hernia and 7 with a Bochdalek hernia. The mean preoperative BMI was lower in the open surgery group (mean = 30.3; range = 21–59) than the minimally invasive group (mean = 23.2, range = 17–30), but the groups were similar across all other patient demographic characteristics ().
Table 1. Patient demographics.
Most patients with hernia-related symptoms presented with gastrointestinal symptoms, including abdominal pain (n = 15), acute bowel occlusion (n = 4), vomiting (n = 4) or constipation (n = 1) as shown in . The hernia was found incidentally in a CT scan in seven patients (18.9%). Preoperative diagnosis was confirmed through a CT scan in 94.6% (n = 35) of cases. The remaining 5.4% (n = 2) were identified incidentally during laparoscopy for another indication and subsequently repaired. Emergency operations accounted for 36.1% (n = 13) of all CDH cases. All emergency patients experienced CDH symptoms and two patients (5.4%) underwent a small bowel resection. Most patients undergoing emergency operations (76.9%, n = 10) were unaware of the CDH. Among the three patients (23.1%) who were aware, two were awaiting operative treatment and one opted for conservative treatment ().
Table 2. Hernia and operative characteristics in minimally invasive and open repairs.
Most operations involved minimally invasive procedures, with 73.0% (n = 27) involving laparoscopic and 2.7% (n = 1) thoracoscopic operations. One laparoscopic repair also required thoracoscopy to identify the hernia and another was converted to laparotomy. Robotic-assisted repair was performed in one case. Laparotomy was used in four (10,8%) cases, as was thoracotomy.
In addition to omental fat, the hernia sac contained the large intestine in 67.1% (n = 25), small intestine in 18.9% (n = 7), stomach in 10.8% (n = 4) and kidney in 5.4%, (n = 2), as well as the spleen, tail of the pancreas, and part of the liver all respectively in 2.7% of cases, (n = 1) ().
Nonabsorbable mesh was utilized in the repair when primary tissue closure could not be achieved without tension (51.4%, n = 19). Attachment to the abdominal wall was achieved using nonabsorbable tackers (42.1%, n = 8) or sutures (57.9%, n = 11).
The overall complication rate was 18.9% (n = 7), with the rate after elective surgery being 20.8% (n = 5) and after emergency surgery 15.4% (n = 2), (p = .526). Postoperative complications included postoperative infections in three patients (one pneumonia, one empyema and one surgical site infection), pleural effusion in two patients, one cardiac tamponade and one incisional hernia (). The cardiac tamponade was a result of tackers placed through the pericardium during laparoscopic repair of a Morgagni hernia. The rate of complications did not differ statistically between minimally invasive and open surgeries (17.2% vs. 25%, p = 1). Emergency surgery had a complication rate of 20.8% with the rate being 15.4% for elective surgery, with no statistical significance (p = 1).
Table 3. Adverse events.
Intensive care unit was required for two patients postoperatively. Two reoperations were performed within 30 days, once for cardiac tamponade and once for empyema. Later reoperations were a repair of a port-site incisional hernia in one patient and an exploratory laparoscopy and adhesiolysis due to intractable chronic abdominal pain in another patient.
The mean length of hospital stay was 3.6 (range: 1–13) days after laparoscopic repair and 6.8 (range: 4–11) days after open repair (p = .007, t = 3.3, 95% confidence interval = 1.04−5.21). The median follow-up time was 48 months (range, 1–116), with a follow-up of at least 11 months for 86.5%. No short- or long-term recurrences were discovered in any of the patients.
A binomial multiple logistic regression model was used to examine factors contributing to complication rate. None of the factors included into the model (age, gender, emergency operation, minimally invasive surgery, use of mesh augmentation and Charlson Comorbidity Index) were statistically significantly correlated with complication rate. The results can be seen in .
Table 4. Logistic regression analysis of factors affecting complication rate.
Discussion
In this study, our primary finding was that the laparoscopic repair of Morgagni and Bochdalek hernias is effective, safe and leads to a shorter hospital stay than an open repair. Laparoscopy represented the most common surgical approach, used in 71% of cases.
Although some complications occurred in our patients, severe complications remained rare, with an overall complication rate (18.9%) comparable with previous studies [Citation8,Citation9,Citation18]. The complication rate in a review of Morgagni hernias by Horton et al. was 17% for laparotomy, 6% for thoracotomy and 5% for laparoscopy [Citation8]. However, most of the individual studies included in that review featured small patient sample sizes, accompanying a possible reporting bias. The use of tackers resulted in cardiac tamponade in one patient. This complication has been associated with tacker use in diaphragmatic hernia repair before and therefore tackers should not be used in repair of diaphragmatic hernia to avoid this catastrophic complication [Citation19].
The rate of complications did not differ statistically between minimally invasive and open surgeries (17.2% vs. 25%, p = 1), however minimally invasive repair of CDH resulted in a statistically significantly shorter hospital stay in our study compared to open repair (3.5 days vs. 6.8 days, p = .002). Previous research identified a shorter hospital stay as one of the benefits of minimally invasive surgery [Citation7,Citation12,Citation13]. Minimally invasive surgery should thus be viewed as the primary approach in skilled centers.
In our cohort, emergency operations comprised 36.1% of all surgeries, a rate similar to some previous studies with an emergency surgery rate of around 35% [Citation18]. However, in a review by Horton et al., the emergency surgery rate was as low as 14%, while in a retrospective study by Young et al., no emergency operations were performed [Citation8,Citation9,Citation18]. This wide variety in rate of emergency operations probably reflects the differences in healthcare structure and referral practices, as in our center, most of the patients (76.9%) undergoing emergency surgery were unaware of the presence of a CDH and as a tertiary center in a public healthcare system, our center provides care to all of the emergency CDH patients in our area. We found no statistical difference in the complication rate between emergency and elective operations (15.4% vs. 20.8%, p = 1) and no patients required intensive care after surgery.
A major strength of our study is the relatively large number of patients for such a rare disease. We identified all patients operated in our institution between a certain time period, compared to previous studies which are mostly case reports or case series’ with fewer patients. Most patients in our study had a long follow-up after surgery, and thus good data on long-term complications related to CDH repair, given Finland’s centralized national patient data registry.
There are several limitations to our study. As a retrospective case series, this type of study is susceptible to information and selection bias. However, we still serve as the only thoracic surgery unit for the Helsinki metropolitan area and Uusimaa Municipality area and work as a tertiary care center for general thoracic surgery for other university hospitals in Finland.
To conclude, our study supports the claim that the operative treatment of congenital diaphragmatic hernia is safe and effective. All surgical approaches appear to bring about a lasting result. Thus, minimally invasive repair represents a good option for experienced surgeons, accompanying a shorter hospital stay and minimal morbidity. Still, further research is required on the long-term results among CDH patients.
Ethical approval
The Helsinki University Hospital Institutional Review Board approved the study protocol as part of the rare hernias study (HUS/60/2019).
Consent form
The consent to participate was waived by the ethics committee. All authors have provided consent for publication.
Author contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Henriikka Hietaniemi and Tommi Järvinen. The first draft of the manuscript was written by Henriikka Hietaniemi, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data are available from the author. Code availability (software application or custom code).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Losanoff JE, Sauter ER. Congenital posterolateral diaphragmatic hernia in an adult. Hernia. 2004;8(1):83–85.
- Temizoz O, Genchellac H, Yekeler E, et al. Prevalence and MDCT characteristics of asymptomatic Bochdalek hernia in adult population. Diagn Interv Radiol. 2009;16(1):52–55.
- Kinoshita F, Ishiyama M, Honda S, et al. Late-presenting posterior transdiaphragmatic (Bochdalek) hernia in adults: prevalence and MDCT characteristics. J Thorac Imaging. 2009;24(1):17–22.
- Gale ME. Bochdalek hernia: prevalence and CT characteristics. Radiology. 1985;156(2):449–452.
- Mullins ME, Stein J, Saini SS, et al. Prevalence of incidental Bochdalek’s hernia in a large adult population. AJR Am J Roentgenol. 2001;177(2):363–366.
- Comer TP, Clagett OT. Surgical treatment of hernia of the foramen of Morgagni. J Thorac Cardiovasc Surg. 1966;52(4):461–468.
- Sanford Z, Weltz AS, Brown J, et al. Morgagni hernia repair: a review. Surg Innov. 2018;25(4):389–399.
- Horton JD, Hofmann LJ, Hetz SP. Presentation and management of Morgagni hernias in adults: a review of 298 cases. Surg Endosc. 2008;22(6):1413–1420.
- Young MC, Saddoughi SA, Aho JM, et al. Comparison of laparoscopic versus open surgical management of Morgagni hernia. Ann Thorac Surg. 2019;107(1):257–261.
- Brown SR, Horton JD, Trivette E, et al. Bochdalek hernia in the adult: demographics, presentation, and surgical management. Hernia. 2011;15(1):23–30.
- Pousios D, Panagiotopoulos N, Piyis A, et al. Transthoracic repair of asymptomatic Morgagni hernia in an adult. Indian J Surg. 2012;74(5):431–433.
- Richardson WS, Bolton JS. Laparoscopic repair of congenital diaphragmatic hernias. J Laparoendosc Adv Surg Tech A. 2002;12(4):277–280.
- Machado NO. Laparoscopic repair of Bochdalek diaphragmatic hernia in adults. N Am J Med Sci. 2016;8(2):65–74.
- Kuster GG, Kline LE, Garzo G. Diaphragmatic hernia through the foramen of Morgagni: laparoscopic repair case report. J Laparoendosc Surg. 1992;2(2):93–100.
- Loong TP, Kocher HM. Clinical presentation and operative repair of hernia of Morgagni. Postgrad Med J. 2005;81(951):41–44.
- Zhou Y, Du H, Che G. Giant congenital diaphragmatic hernia in an adult. J Cardiothorac Surg. 2014;9(1):31.
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–196.
- Leeflang E, Madden J, Ibele A, et al. Laparoscopic management of symptomatic congenital diaphragmatic hernia of Morgagni in the adult. Surg Endosc. 2022;36(1):216–221.
- Frantzides CT, Welle SN. Cardiac tamponade as a life-threatening complication in hernia repair. Surgery. 2012;152(1):133–135.
