Abstract
Objectives
Updated population-based studies on acute pancreatitis (AP) in Finland are lacking. Our aim was to evaluate the current data for AP in Helsinki.
Materials and methods
We performed an electronic health care records (EHRs) search on AP patients treated at Helsinki University Hospital between the years 2016 − 2018. Incidence was calculated, etiological and potential risk factors, as well as severity of AP were documented and analyzed.
Results
Between 2016 and 2018 we found 1378 AP episodes on 1084 patients, 35% of the patients had several AP episodes, i.e., recurrent AP (RAP). The domicile-adjusted incidence was 42.2/100 000. 47% of the patients had alcohol etiology (59% men, 27% women) and 23% had biliary etiology, 21% were idiopathic and 2.9% were post-ERCP pancreatitis. 13.1% of the patients had passed at the end of September 2021. 45% of the patients were currently smoking, 11% were ex-smokers, and the highest percentage of smokers was in the group of alcohol-caused AP with 74% ever-smokers. Biliary AP had the highest amount of overweight patients. 24% of the patients used anticoagulation (AC) medication, and the percentage was significantly higher with idiopathic AP (48%). RAP, female sex and normal BMI associated with a mild form of AP.
Conclusions
Incidence of AP and the percentage of alcohol etiology are lower than earlier reported for Finland although still higher than in other Nordic countries. Smoking and the use of AC medication associate with AP.
Introduction
Acute pancreatitis (AP) continues to be a common cause for hospitalization [Citation1] and contributes substantially to health care expenditure although 75–80% of the patients have a relatively mild clinical course [Citation2]. The diagnosis of AP is based on clinical presentation, level of plasma or serum amylase or lipase activity and/or typical radiological findings. The 2012 revised Atlanta Classification defines the severity of AP into mild, moderate or severe according to the local or systemic complications and transient or persistent organ failure [Citation3].
An earlier population-based study in Finland between 1970 and 1989 reported an increasing incidence of AP from 46.6 to 73.4/100,000 but as a registry study, this study included also re-admissions for the same AP attack thus inflating the calculated incidence [Citation4]. Alcohol has been reported to be the etiological factor in 70% of the AP cases in Finland [Citation5,Citation6]. However, these previous studies were performed in selected study groups and not in the entire population attributing somewhat to the remarkably high percentage of alcohol-related AP compared with other European countries [Citation2]. The reported incidence of first-time AP is increasing in Sweden being 38/100,000 [Citation7] and 49% of the cases were gallstone-related [Citation8]. The incidence is rising in Denmark as well, being 39/100,000 with women and 37/100,000 with men [Citation9].
The aim of this study was to analyze AP cases in Helsinki University Hospital in a three-year period investigating incidence, etiology, potential risk factors and severity of AP. Mortality and pancreatic cancer cases were also recorded in this cohort.
Materials and methods
Patients
In this retrospective study, we analyzed 1378 consecutive AP episodes treated in Helsinki University Hospital in Meilahti with a discharge date between January 2016 and December 2018. The patients were identified by performing an EHR search based on the ICD-10 discharge codes of K85 and K86 in order to include all the AP patients because some cases might have been miscoded in the discharge report. The clinical data were collected from EHR. Cases that did not meet the set criteria for AP diagnosis or showed the signs of chronic pancreatitis (CP) were excluded from the analyses of our study. We collected information on the patients’ sex, age, smoking and drinking habits, body mass index (BMI), the place of residence, long-term antithrombotic medication and previous history of AP and CP. In addition, we recorded the duration of the hospital stay, possible ICU treatment, laboratory results upon admission, radiological findings, the signs of organ dysfunction, invasive procedures performed and the patients’ discharge condition. The etiology of AP was reanalyzed based on information from the electronic patient journals and clinical test results. Survival and follow-up data on the possible diagnosis of pancreatic tumors was recorded. Children treated for pancreatitis during 2016 − 2018 were included only in the incidence calculation, all the other analyses were done on the adult population.
Etiology
The etiology of AP was defined as one of the following: (1) alcohol related, (2) biliary, (3) other causes and (4) idiopathic. Some patients had been using alcohol and had biliary findings. They were defined as biliary only if they met the criteria listed below, otherwise they were categorized as alcohol related.
Alcohol-related AP was diagnosed if either regular alcohol consumption or an isolated episode of alcohol consumption of at least seven standard drinks was present in patient history. Symptoms had to occur within seven days from last alcohol consumption and other etiologies had to be excluded.
We defined biliary AP based on the findings of the patient's plasma alkaline phosphatase and/or bilirubin levels (at least twice over the upper limit of the normal range), when other possible causes were excluded and preferably also when there was a radiological confirmation of gallstones/dilated biliary ducts.
Other causes of AP were postoperative and treatment-related complications, genetic and congenital susceptibility, drug-induced AP, trauma, hypertriglyceridemia, hypercalcemia and neoplasia including intraductal papillary mucinous neoplasm of the pancreas (IPMN).
Cases that fit none of the above-mentioned etiologies were deemed idiopathic.
Statistical analysis
The data was analyzed using linear regression, ANOVA and chi-square test with the statistical program SPSS version 27.0 (SPSS Inc., Chicago, IL).
Results
Incidence of AP
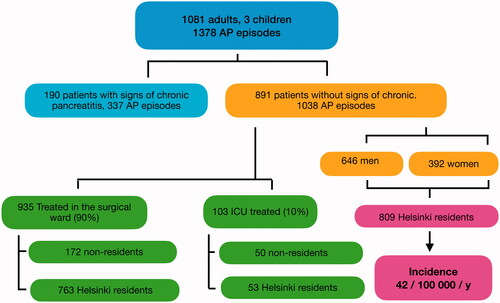
Our department serves as a referral center for a population of approximately 640,000 inhabitants. In addition, Helsinki University Hospital serves as a terriatry center and receives complicated pancreatitis patients in need of surgery, ERCP or ICU treatment from all over Finland. Our search identified 1378 consecutive AP episodes. As some patients suffered from recurrent AP (RAP), the patient material consisted of 1081 adult patients and 3 children. 65% of the episodes on adults (n = 899) were on men and 35% (n = 476) on women. Of the patients with AP, 337 showed radiological signs of CP and these patients were excluded yielding 1038 AP episodes on adults for analysis, 62% (n = 646) on men and 38% (n = 392) on women.
In addition to serving as a teritiary center for severe AP (SAP), as the capital of Finland, Helsinki has many visitors who may need medical attention during their stay. Calculating the incidence for the residents of Helsinki only, resulted in 42.2/100,000 as the average domicile-adjusted incidence of AP in Helsinki. The flow-chart of the patient groups is shown in .
Etiology of AP
Alcohol-related etiology was identified in 46.8% and biliary etiology in 23.4% of the patients. Among other etiologies we found 4 AP patients with a genetic predisposition, 2 patients with autoimmune pancreatitis (AIP), 4 hypertriglyceridemia AP cases and 20 AP caused by neoplasms or metastasis. Of the AP episodes, 11 were considered to be drug-induced: 5 were caused by chemotherapy, 4 by anti-inflammatory medication for inflammatory bowel disease, 1 by azithromycin antibiotic and 1 by zonisamide medicine for epilepsy. Marked differences were observed in etiology between males and females, the etiological diagnoses are shown in more detail in .
Table 1. Etiology of 1038 AP episodes.
A total of 366 cases (35%) were recurrent attacks of AP (RAP). A total of 139 patients had endured one previous AP attack, 39 patients had had two attacks. Of 61.7% of the RAP episodes had alcohol etiology, the second most common was idiopathic AP 23.0% whereas only 9.0% of the RAP had biliary etiology.
As a comparison, we have summarized the incidences, etiologies and trends of AP in the Nordic countries in .
Table 2. Incidence, etiology, and AP trends in the Nordic countries.
Severity of AP episodes
The majority of patients, 71.3% had mild AP, 19.1% of the patients had moderate and 9.5% SAP. CRP value at admission associated with the severity of the AP, 18.4% of the mild AP patients had CRP value greater than 100 compared with 33.7% of the moderate AP patients and 39% of the SAP patients (p < .001). Nearly half of the SAP episodes, 47 out of 99, were alcohol-related and 21.2% of the SAP had biliary etiology. Female sex associated with a milder course of AP compared with males (OR = 2.4, p < .001). Obese patients experienced more moderate or SAP episodes compared with patients with normal BMI who had a higher percentage of mild AP. The etiological group of ‘other causes’ had the highest percentage of SAP. The severity of AP in different etiologies is shown in . The first-time AP episodes were more often severe in comparison with RAP (11.3 vs. 6.3% %) hence 11.5% of the first-time AP episodes and 7.1% of the RAP required ICU treatment.
Table 3. The severity of AP in different etiology groups.
The length of hospital stay for AP patients ranged from 0 to 190 d with a median of 4 d. The average hospital stay was 7.7 d for alcohol-caused AP episodes, 9.8 d for biliary and 5.5 d for idiopathic AP.
Mortality
Of the AP cases, 30-d mortality was 3.9% (n = 40) and 90-d mortality 4.6% (n = 48), including the in-hospital mortality. Of the 40 cases with 30-d mortality, the etiology of the AP was alcohol in seven cases, seven cases were biliary AP, 16 were in the group of idiopathic pancreatitis and 10 in the group with other causes of AP. By September 2021, 13.3% of the cases in our cohort had deceased. The overall mortality was 8.6% in alcohol-related AP group, 15.2% in biliary, 12.6% in idiopathic and 31.9% in the group with ‘other causes’ of AP. It is noteworthy that the latter group included the patients with pancreatic tumors or metastasis.
Smoking habits
Information on tobacco use was missing from 109 AP cases (10.5%). Of the AP cases with smoking status available, 45% were on smokers and 11% were on ex-smokers. Of 68% of the alcohol-related AP cases were on smokers while for biliary AP 36% and for idiopathic AP 45% were on smokers or ex-smokers (). Of the first-time AP episodes 38.0% were on smokers in comparison with the RAP episodes of which 56.9% were on smokers (p < .001).
Table 4. Smoking habits for different etiological groups.
Body mass index
The weight of the patient was documented only in 56.0% of the cases in the electronic patient journal. Of the AP cases with patient weight available, 28.1% of the patients were overweight and 46.1% were obese. In the cases with alcohol-related AP or in the group of other causes of AP, about 72% of the patients had a BMI greater than 25 whereas the corresponding figures for AP cases with biliary and idiopathic etiology were 79.2 and 74.1%. There was a significant positive correlation between the risk of getting an idiopathic AP with high BMI (p < .001) and an even stronger correlation for biliary AP (p < .001).
Anticoagulation medication
After reviewing the medication history for each patient, we found the use of anticoagulation (AC) medication to be 25.1% in all AP cases and it was significantly higher in the group of idiopathic AP (47.9%) compared with biliary etiology (31.7%, p < .001). The risk of developing an idiopathic AP is higher for those using AC medication with an OR 3.87 (p < .001), with a slightly higher risk for women (OR 1.69, p = .041). Antiplatelet therapies (ASA, clopidogrel and dipyridamol) were the most common anticoagulants in 63.2% of the cases and 19.9% of the cases had Vitamin K agonist (warfarin) therapy. Direct oral anticoagulants (DOAC) and low molecular weight heparin (LMWH) were used by 7.3 and 4.2% of the cases, and 5.4% had various AC medications simultaneously. The type of anticoagulant lacked significant association with the etiology of AP (data not shown). shows the proportion of AC use in the etiological groups and Supplementary Table S1 the distribution of etiology of AP on patients with AC medications.
Table 5. Use of anticoagulation medication in the etiological groups.
Pancreatic cancer cases
Out of 1081 patients in our material, 11 were diagnosed with pancreatic cancer by the end of the year 2020, all 11 patients have since passed. Two patients got drug-induced AP caused by chemotherapy. Three of the cancer cases were diagnosed at the first admission for AP. Three tumors did not show on the diagnostic work-up at the first admission but were found later in the control CECT with the so-called pancreas protocol (intravenous contrast in arterial, venous and pancreas phases). One patient had multiple CT scans and ERCP procedures, yet the tumor emerged after 18 months and by then it was locally advanced. One case of AP had a CT scan without iv contrast at first admission showing no indication of a tumor. The AP was determined as alcohol caused, and no control work-up was planned. The following year a CT was performed due to abdominal pain revealing intrapancreatic cholangiocarcinoma with liver metastases. Pancreatic cancer contributed to 8.1% of the mortality.
Discussion
A previous report has shown Finland to have one of the highest incidences of AP in Europe [Citation2]. In this retrospective study, we found an incidence of 42.2/100,000 of AP in Helsinki which is markedly lower than earlier reported 73.4/100,000 [Citation4]. In our study, we also showed that alcohol induced AP is not as common as it was in the earlier decades in Finland [Citation5,Citation6] and that smoking is a prominent risk factor for alcohol-related AP and AC medication for idiopathic AP.
The incidence of AP increases worldwide [Citation1] which could be related to more frequent radiological imaging with CT scans and the current routine of laboratory testing for abdominal pain in the emergency setting. The previous report on the incidence of AP in Finland [Citation4] was a registry study which has its limitations with the possible miscoding of discharge diagnoses and with entering re-admission of the same AP attack as a separate new case. The growing rates of obesity and gallstone disease may contribute to rising AP incidence. The frequencies of obesity and being overweight are increasing also in Finland; 71.9% of men and 63.3% of women have a BMI above 25 [Citation19]. We found a biliary cause of AP in 23.4% of the cases compared with earlier reports of 21% [Citation5] and 13.2% [Citation6] of biliary etiology in Finland although in the latter report, the study population was limited to the working age population and the biliary pancreatitis is notably the most common etiology of AP in the elderly. The biliary group has the highest proportion of obese and overweight patients, albeit the information about patients’ weight is lacking surprisingly often from the health care records.
Alcohol consumption is decreasing in Finland [Citation18,Citation19] which may contribute to the decreasing incidence of AP in Finland. Alcohol-related AP remained the most common etiology in our material although being less frequent than earlier reported for Finnish population, 46.8% compared with 70% [Citation5] and 71.4% [Citation6]. Previous studies were performed either on SAP patients [Citation5] or on working-age population [Citation6], hence study populations are not entirely comparable. Also in our material, alcohol-related AP patients were younger than patients with other etiologies. The frequency of alcohol-related AP in Finland is still much higher than reports from Denmark, where alcohol is reported being the cause of AP in 21 − 34% [Citation10,Citation11] even though Denmark reports as high or higher alcohol consumption levels [Citation20]. Sweden has reported 17% of the AP cases to be alcohol-related but only the first attack AP cases were included in the study [Citation8]. In Finland, we may have a lower threshold for deeming the AP to be alcohol-related although there could be several factors and co-morbidities contributing. In this retrospective study, we are confined to the evaluations performed at the time, as well as to the documented conclusions in the EHR. In addition, we have included the recurrent episodes in this study which affects our figures to some extent since most of the RAP cases were caused by alcohol.
Of the other more uncommon etiologies of AP, our patient material had only four patients with AP caused by hypertriglyceridemia which could be related to the timing of the testing, namely the following morning of the admission to the hospital. For the purpose of more accurate diagnosis, testing should be performed immediately at the emergency setting [Citation21].
In our material, 20.7% of the patients lacked an etiological diagnosis and were reported as idiopathic AP which is a higher percentage than in other reports [Citation6]. The idiopathic AP patients had more often AC medication (47.9%) compared with other etiological groups and our data suggests that the AC medication increases the risk of an idiopathic AP (p < .001). Antithrombotic drugs, such as acetylsalicylic acid (ASA) have been previously linked to AP [Citation22,Citation23]. In our material, the type on AC medication lacked association with the etiology of AP. There was a significant positive correlation between the risk of getting an idiopathic AP and a higher BMI. This could be related to microlithiasis or biliary sludge causing AP or to a high BMI in itself as a risk factor for AP which requires further investigation [Citation18,Citation24]. Laparoscopic cholecystectomy LCC and endoscopic ultrasound EUS or ERCP is recommended for idiopathic AP patients to exclude sludge and microlithiasis as causes for the AP [Citation25].
Our results show that the risk of getting AP is higher if the patient is a current or an ex-smoker compared with non-smokers, which is in concordance with previous reports [Citation17,Citation26]. The proportion of smokers in the Finnish population has been reported being 14% [Citation27]. Our results show that the proportion of current smokers was the highest among alcohol-related AP (68%) and it has been shown that the combination of alcohol and cigarette smoke triggers an even more extensive acinar cell death [Citation28]. 35% of the cases were RAP attacks, the majority of which (62%) were alcohol related, and the proportion of current smokers in the RAP group was higher than for the first-time AP patients, the risk of getting RAP is higher if the patient is currently smoking. Idiopathic AP patients were also more often smokers (28%) or ex-smokers (17%) than biliary AP (20 and 16%). We could include ‘tobacco induced AP’ as an alternative or as an additional etiology, yet remarkably often the current and former smoking habits are not documented in the health care records. Indeed, we should encourage health care professionals to inquire about smoking habits and to educate patients on the benefits of smoking cessation, also in relation to the risk of AP.
RAP, female sex and normal BMI correlate with getting a mild AP. A first-time AP increases the risk of enduring a SAP compared with RAP (p < .002).
To assess mortality, we examined the AP cases from the years 2016 − 2018 in 2021 to find out how many patients had died. We found a 30-d mortality of 3.9% and an overall mortality of 13.3%. Pancreatic cancer contributed to 8.1% of the mortality; therefore, it is recommended that AP patients should undergo a contrast-enhanced CT scan (arterial, venous and pancreas phases) to exclude pancreatic cancer as the cause of AP, especially in the cases of unknown or uncertain etiology. An association between AP and risk of pancreatic cancer has been shown previously [Citation11] and an advantage in survival has been reported for pancreatic cancer patients with AP [Citation10]. In our current material, unfortunately the cancer cases diagnosed after an episode of AP were all borderline resectable or inoperable at the time of the diagnosis. Therefore, we did not observe survival benefit with the AP showing as the first symptom of pancreatic cancer.
Determining and diagnosing the etiological factors of AP has become more complex recently, various more uncommon causes of AP were overlooked in the past. On the other hand, the practice of coding and recording of diagnoses has changed somewhat. The documented information is more readily available to the patients and the physicians take more into consideration how the etiological factors of AP are recorded in the health care records which may demote the proportion of AP categorized as alcohol related. An objective biochemical laboratory test measured at every admission of a first AP could be the proverbial golden mean. CDT (9.95€ price of HUSLAB of Helsinki University Hospital) has been used occasionally, but a more specific alternative is B-PETh (44.5€ price of HUSLAB).
Conclusions
Incidence of AP and alcohol etiology is lower than earlier reported for Finland though still higher than in other Nordic countries. The etiology of AP should be determined by a detailed history including smoking habits, BMI, the family history of pancreatitis and pancreas cancer, AC medication, IBD history and diabetes. Possible biliary etiology should be explored with adequate radiological or endoscopic methods. Some idiopathic AP may be caused by microlithiasis or biliary sludge, but further investigation is warranted to explore if obesity is a risk factor or co-factor. RAP, female sex and normal BMI correlate with getting a mild AP. We have identified smoking and AC medication as possible risk factors for AP.
Author contributions
The study was planned by JL and LK. HB participated in the design of the study. HB and EL collected the data from the EHR. HB, EL, LK and JL drafted the manuscript.
Supplemental Material
Download PDF (69.8 KB)Acknowledgments
Aki Saukkonen is acknowledged for great help in the early phases of data collection. Sandra Bladh is warmly acknowledged for the skillful assistance in performing the statistical analyses.
Disclosure statement
The authors report there are no relevant competing interests to declare.
Additional information
Funding
References
- GBD. Disease and injury incidence and prevalence collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1789–1858.
- Roberts SE, Morrison-Rees S, John A, et al. The incidence and aetiology of acute pancreatitis across Europe. Pancreatology. 2017;17(2):155–165.
- Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102–111.
- Jaakkola M, Nordback I. Pancreatitis in Finland between 1970 and 1989. Gut. 1993;34(9):1255–1260.
- Puolakkainen P, Valtonen V, Paananen A, et al. C-reactive protein (CRP) and serum phospholipase A2 in the assessment of the severity of acute pancreatitis. Gut. 1987;28(6):764–771.
- Karjula H, Saarela A, Ohtonen P, et al. Long-term outcome and causes of death for working-age patients hospitalized due to acute pancreatitis with a median follow-up of 10 years. Ann Surg. 2019;269(5):932–936.
- Oskarsson V, Hosseini S, Discacciati A, et al. Rising incidence of acute pancreatitis in Sweden: national estimates and trends between 1990 and 2013. United Eur Gastroenterol J. 2020;8(4):472–480.
- Bertilsson S, Kalaitzakis E. Acute pancreatitis and use of Pancreatitis-Associated drugs: a 10-Year Population-Based cohort study. Pancreas. 2015;44(7):1096–1104.
- Knudsen JS, Heide-Jørgensen U, Mortensen FV, et al. Acute pancreatitis: 31-Year trends in incidence and mortality - A Danish population-based cohort study. Pancreatology. 2020;20(7):1332–1339.
- Kirkegård J, Gaber C, Lund JL, et al. Acute pancreatitis as an early marker of pancreatic cancer and cancer stage, treatment, and prognosis. Cancer Epidemiol. 2020;64:101647.
- Kirkegård J, Cronin-Fenton D, Heide-Jørgensen U, et al. Acute pancreatitis and pancreatic cancer risk: a nationwide Matched-Cohort study in Denmark. Gastroenterology. 2018;154(6):1729–1736.
- Nøjgaard C, Bendtsen F, Matzen P, et al. The aetiology of acute and chronic pancreatitis over time in a hospital in Copenhagen. Dan Med Bull. 2010;57(1):A4103.
- Hauksson K, Arnardottir M, Agustsson AS, et al. Increase in the incidence of alcoholic pancreatitis and alcoholic liver disease in Iceland: impact of per capita alcohol consumption. Scand J Gastroenterol. 2020;55(5):615–620.
- Vidarsdottir H, Möller PH, Vidarsdottir H, et al. Acute pancreatitis: a prospective study on incidence, etiology, and outcome. Eur J Gastroenterol Hepatol. 2013;25(9):1068–1075.
- Omdal T, Dale J, Lie SA, et al. Time trends in incidence, etiology, and case fatality rate of the first attack of acute pancreatitis. Scand J Gastroenterol. 2011;46(11):1389–1398.
- Gislason H, Horn A, Hoem D, et al. Acute pancreatitis in bergen, Norway. A study on incidence, etiology and severity. Scand J Surg. 2004;93(1):29–33.
- Lindkvist B, Appelros S, Manjer J, et al. A prospective cohort study of smoking in acute pancreatitis. Pancreatology. 2008;8(1):63–70.
- Koponen P, Borodulin K, Lundqvist A, et al. Terveys, toimintakyky ja hyvinvointi Suomessa: FinTerveys 2017-tutkimus' Helsinki:THL; 2018. Available from: https://urn.fi/URN:ISBN:978-952-343-105-8
- WHO. Nordic alcohol market report. 2021. Available from: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/alcohol-recorded-per-capita-(15-)-consumption-(in-litres-of-pure-alcohol).
- Häkkinen E. Helsinki. 2021. Available from: https://www.alko.fi/INTERSHOP/static/WFS/Alko-OnlineShop-Site/-/Alko-OnlineShop/en_US/pdf_t/NordicAlcoholMarket2021_VALMIS.pdf
- Berberich AJ, Ziada A, Zou GY, et al. Conservative management in hypertriglyceridemia-associated pancreatitis. J Intern Med. 2019;286(6):644–650.
- Jones MR, Hall OM, Kaye AM, et al. Drug-induced acute pancreatitis: a review. Ochsner J. 2015;15(1):45–51.
- Stevenson DD, White AA, Simon RA. Aspirin as a cause of pancreatitis in patients with aspirin-exacerbated respiratory disease. J Allergy Clin Immunol. 2012;129(6):1687–1688.
- Aune D, Mahamat-Saleh Y, Norat T, et al. High body mass index and Central adiposity is associated with increased risk of acute pancreatitis: a Meta-Analysis. Dig Dis Sci. 2021;66(4):1249–1267.
- Pereira R, Eslick G, Cox M. Endoscopic ultrasound for routine assessment in idiopathic acute pancreatitis. J Gastrointest Surg. 2019;23(8):1694–1700.
- Ye X, Lu G, Huai J, et al. Impact of smoking on the risk of pancreatitis: a systematic review and Meta-analysis. PLoS One. 2015;10(4):e0124075.
- Jääskeläinen M, Virtanen S. Tilastoraportti 44, Päihdetilastollinen vuosikirja 2019, THL. Helsinki. 2020. Available from: https://urn.fi/URN:ISBN:978-952-343-438-7
- Lugea A, Gerloff A, Su HY, et al. The combination of alcohol and cigarette smoke induces endoplasmic reticulum stress and cell death in pancreatic acinar cells. Gastroenterology. 2017;153(6):1674–1686.