Abstract
Background
Diabetes type 1 and type 2 may develop gastrointestinal complications e.g., gastroparesis and gastroenteropathy. Concomitant celiac disease and pancreatic exocrine insufficiency occur with high prevalence in diabetes and with symptomatic overlap. Consequently, it is a challenge to disentangle symptoms of these conditions and separate them from functional dyspepsia. We aim to develop a clinical decision-support tool to differentiate the underlying disease in a plethora of gastrointestinal symptoms.
Methods
An internet-based computerized survey will collect basic characteristics (diabetes type, age, gender, duration, HbA1c, treatment) and patient reported outcomes by validated questionnaires focusing on (1) gastroparesis using Gastroparesis Cardinal Symptom Index; (2) gastroenteropathy using Gastrointestinal Symptom Rating Scale; (3) celiac disease using Celiac Symptom Index and (4) pancreatic exocrine insufficiency with Pancreatic Exocrine Insufficiency Questionnaire. Logistic regression and multiple regression analyses will identify risk factors and gastrointestinal complications. Cluster analyses and machine learning will classify different symptoms and co-existing presentations, into a likely diagnosis. We seek biomarkers for autonomic neuropathy by characterizing development of retinopathy using the Visual Function Questionnaire-25 and peripheral neuropathy by the Michigan neuropathy questionnaire. Participants are re-examined yearly for disease progression over time.
Results
From focus group studies gastrointestinal symptoms are of major concern in diabetes. Potentially, estimates of symptom prevalence, risk factor identification and classifications of gastrointestinal complications can be unraveled for feedback to health care providers.
Conclusion
The web-based DICODI project will open up possibilities to detect gastrointestinal complications of diabetes in a societal setting, benefitting people living with diabetes, health care professionals, and society.
Introduction
Over the last two decades, advances in our understanding of gastrointestinal physiology and systematic classification of symptoms have revealed that people with diabetes often have a considerable burden of gastrointestinal symptoms, known as diabetic gastro-enteropathy, which encompasses the cumulative impact that diabetes exerts on the entire gastrointestinal tract [Citation1]. The underlying pathophysiology is incompletely understood, but impaired autonomic regulation, compromised microvascular blood supply, combined with loss of the cells of Cajal and smooth muscle myopathy, are associated with gastroenterological sensory and motor abnormalities. The most outspoken upper gastrointestinal symptom associated with diabetes is intractable vomiting, ascribed to delayed gastric emptying or gastroparesis. Slow gastric emptying in diabetes was first described a century ago by Boas [Citation2] in 1925 and Kassander in 1958 who coined the term ‘gastroparesis diabeticorum’ [Citation3]. It is commonly accepted that diabetes-induced gastrointestinal dysfunction may affect the whole alimentary tract, known as pan-enteric dysfunction, presented with a plethora of symptoms including reflux, early satiety, bloating, abdominal pain, constipation and fecal incontinence [Citation4–6]. However, these symptoms cannot be ascribed as a consequence of diabetes without excluding other relevant causes, such as celiac disease or pancreatic exocrine insufficiency [Citation4]. Hence, the work-up of diabetic patients with gastrointestinal symptoms should involve full medical background and physical examination, followed by the pertinent investigations; same as would be done for any person with similar symptoms.
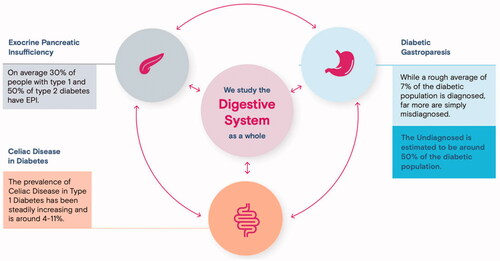
This position paper of the study DIgestive COmplications in DIabetes with the acronym DICODI discourses the common under-recognition of gastrointestinal symptoms in diabetes by use of patient-related outcomes (PROs) in a systematic and prospective way. We search to delimitate our presentation to the diabetic context in order to differentiate symptoms with a specific bearing on diabetic complications from those of functional dyspepsia. Herein, we particularly focus on diabetic gastroparesis, celiac disease and pancreatic exocrine insufficiency which commonly co-exist and can complicate the management of metabolic control in diabetes.
Prevalence and identification of risk factors
Despite large variations, community-based studies have provided us with data of the high prevalence of upper gastrointestinal symptoms in diabetes. For instance, is it largely overlooked that up to 14% of people with diabetes suffer from abdominal pain or discomfort [Citation7]. Furthermore, cardinal symptoms of gastroparesis appears to be more common in people with type 1 diabetes than in those with type 2 diabetes, and delayed gastric emptying has been found in 27–58% of people with long-standing type 1 diabetes [Citation8] and in up to 30% of people with type 2 diabetes [Citation9]. However, studies also range from those reporting large increases in the prevalence of only upper gastrointestinal symptoms [Citation10] to others reporting increased frequency of all different gastrointestinal symptoms [Citation11–14] ().
Figure 1. Intermingled symptoms with upper gastrointestinal upset commonly seen in the plethora of late complications and concurrent diseases of diabetes mellitus.
The disease duration has been reported as an independent risk factor of symptoms in diabetes [Citation12], whilst others do not observe this association [Citation7]. It has been assumed that gastrointestinal symptoms are secondary to autonomic neuropathy in the gut [Citation15,Citation16], but epidemiological studies do not support this assumption [Citation17]. Another risk factor is hyperglycemia, which may precipitate dysfunction throughout the alimentary tract [Citation18–21]. In line with this, plasma glucose excursions show association to gastrointestinal symptoms [Citation7]. Taken together, a recent review indicates that gastrointestinal discomfort could be 70% higher in people with diabetes, describing that 25% experience gastrointestinal symptoms [Citation22]. To further expand on this, population studies of people living with diabetes are needed, but currently hampered by the lack of a reliable internet-based survey instrument designed to collect data. This can now be achieved by implementing validated questionnaires operated by internet-based computer technology in order to characterize and disentangle the diverse gastrointestinal symptom profiles.
Methods
People diagnosed with diabetes mellitus registered at the diabetes patient organizations in Denmark, Norway and Sweden will be informed and asked to participate in the study, starting late 2022. An internet-based computerized survey will collect basic characteristics (diabetes type, age, gender, duration, HbA1c, treatment) and PROs from diabetes populations in Denmark, Norway and Sweden by use of the validated questionnaires for gastroparesis; (1) gastroenteropathy; (2) celiac disease and; (3) pancreatic exocrine insufficiency. Using logistic regression and multiple regression analyses risk factors and gastrointestinal complications will be identified. Cluster analyses and machine learning will classify different symptoms and co-existing presentations, into the likely diagnosis. To achieve longitudinal data, participants will be yearly re-examined for progression of symptoms.
Inclusion criteria are diabetes mellitus type 1 or type 2 plus membership in patient organization for diabetes. Exclusion criteria are renal or hepatic insufficiency, planned abdominal surgery over the forthcoming year, not capable to use computer for login.
Main symptoms of upper gastrointestinal dysfunction in diabetes
In the clinical setting we emphasize that people with diabetes presenting with different types of upper gastrointestinal problems need a detailed anamnesis as well as diagnostic work-up in order to differentiate their symptoms and complications. However, this is seldomly done in full. In the clinic, symptoms referred to as dyspepsia, anemia or vomiting usually lead to an upper endoscopy with biopsies from the duodenum and stomach, or a fecal Helicobacter antigen test, but outside of that other diagnostic procedures are not routinely done. Hence, a diagnosis of functional dyspepsia or Helicobacter-induced dyspepsia, as well as celiac disease can be made after the above mentioned tests [Citation23], but seldom the medical work-up is seldomly carried forward beyond this point. As a supplement, we advocate the use of validated questionnaires in order to disentangle the most likely disorder underlying various upper gastrointestinal symptoms. For patients with constant nausea and repeat vomiting in addition to early satiety, loss of hunger and abdominal distension after a meal, the Gastroparesis Cardinal Symptom Index (GCSI) [Citation24] could be used. In cases with diarrhea or constipation as dominant symptoms the Gastrointestinal Symptom Rating Scale (GSRS) would be more appropriate [Citation25] along with added questions on dry mouth, swallowing, loss of appetite, nausea/vomiting, constipation and micturition. This in turn can then lead to further diagnostic steps called upon by the patient-related outcomes (PROs) of the questionnaires.
For differential diagnostic purposes we have to keep in mind that more than one in twenty patients with type 1 diabetes (e.g., 6%) have a biopsy-proven celiac disease [Citation26]. Evidence regarding the role of celiac disease in type 2 diabetes is less clear. Some studies have linked the intake of a gluten-free diet to reduced obesity and type 2 diabetes, suggesting a role in reducing leptin and insulin-resistance with increasing beta-cell volume. Even if celiac disease may not be found in more than 2.8% of people with type 2 diabetes [Citation27], current knowledge indicates that gluten may be an etiopathogenic factor for the development of type 2 diabetes [Citation28]. The prevalence of celiac disease is high enough in both types of diabetes to motivate the use of a diagnostic questionnaire, the celiac symptom index (CSI), in order to disclose celiac as a concomitant disease, especially in patients with poor metabolic control.
Impairment of the pancreatic exocrine function is a frequent complication of diabetes mellitus. Abdominal symptoms such as nausea, bloating, diarrhea, steatorrhea, and weight loss can often be over-looked in diabetic patients. Using pancreatic elastase 1 activity, 51.1% of type 1 and 35.4% of type 2 diabetics were found to have reduced fecal elastase 1 activity, along with gastrointestinal symptoms [Citation29]. In brief, also pancreatic exocrine function can often be affected in diabetes why we advocate the use of the pancreatic exocrine insufficiency questionnaire (PEIQ) for diagnostic purposes employing PROs.
With these differential diagnostic challenges in mind, we established a focus group in order to clarify the most common worries and burdens that people with diabetes experience, be it type 1 or type 2 diabetes ().
Table 1. Questions raised by the Scandinavian focus group of people with diabetes type 1 or type 2.
The results of the Focus Group data indicated that symptoms from the upper gastrointestinal tract was a major concern among diabetics, while symptoms from the lower gastrointestinal tract were of less prominence, though not eligible. Against this background we chose to use a collection of validated diagnostic questionnaires in order to distinctly separate various diabetic complications and coherent diseases that can develop as late complications with the help of the patient’s own reports. The questionnaires to be used are:
Gastroparesis Cardinal Symptom Index (GCSI)
Gastrointestinal Symptom Rating Scale (GSRS)
Celiac Symptom Index (CSI)
Pancreatic Exocrine Insufficiency Questionnaire (PEIQ)
These indices will primarily be used in a cross-sectional study to differentiate between different upper gastrointestinal symptoms in type 1 and type 2 diabetes. Additionally, the following questionnaires will be used to seek for a prognostic marker of early small fiber neuropathy:
Visual Function Questionnaire-25 (VFQ-25)
Michigan Neuropathy Questionnaire
We believe this will enable a longitudinal follow-up of gastrointestinal complications in diabetes with progressive systemic small and large fiber neuropathy along with diagnostic differentiation between gastroparesis, celiac disease and pancreatic exocrine insufficiency. We intend to use internet-based survey programming as the basis for computerized handling of PROs as measures of disease activity with future diagnostic end-points.
Importance of the study
Recently, it has become increasingly clear that gastrointestinal symptoms are common in the diabetic population. We need large population studies to provide detailed estimates of the symptom prevalence and symptomatic overlap between the underlying causes. Hence, appearance of symptoms can be associated with motility abnormalities of the stomach, duodenum and jejunum as well as celiac disease or pancreatic exocrine insufficiency. Understanding the pathophysiology of gastrointestinal complications in diabetes is still in its early stages. While waiting for an ultimate diagnostic test, we have to rely on the medical history interview. These interviews can be optimally structured for PROs and validated to obtain adequate results for diagnostic purposes and initiation of specific treatments tailored for each specific physiological abnormality. The complexity of gastric, intestinal and pancreatic functions and the multiple anatomical levels at which these organs can be affected in diabetes offers many therapeutic challenges.
As with all other late complications in diabetes, tight control of plasma glucose is the most useful and effectful intervention. Identification of independent risk factors, could lead to early recognition and improved preventive initiatives, and ultimately impact future clinical guidelines. Consequently, results of our population-based survey will benefit the future life for Scandinavians living with diabetes, health care professionals, and the surrounding society.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Meldgaard T, Keller J, Olesen AE, et al. Pathophysiology and management of diabetic gastroenteropathy. Therap Adv Gastroenterol. 2019;12:1756284819852047.
- BO-Thieme.pdf [Internet]. [cited 2022 Feb 14]. Available from: https://www.thieme.de/statics/dokumente/thieme/final/de/dokumente/corporate_thieme-gruppe/BO-Thieme.pdf.
- Kassander P. Asymptomatic gastric retention in diabetics (gastroparesis diabeticorum). Ann Intern Med. 1958;48(4):797–812.
- Abid S, Rizvi A, Jahan F, et al. Poor glycaemic control is the major factor associated with increased frequency of gastrointestinal symptoms in patients with diabetes mellitus. JPMA J Pak Med Assoc. 2007;57(7):345–349.
- Almogbel RA, Alhussan FA, Alnasser SA, et al. Prevalence and risk factors of gastroparesis-related symptoms among patients with type 2 diabetes. Int J Health Sci. 2016;10(3):397–404.
- Fujishiro M, Kushiyama A, Yamazaki H, et al. Gastrointestinal symptom prevalence depends on disease duration and gastrointestinal region in type 2 diabetes mellitus. WJG. 2017;23(36):6694–6704.
- Bytzer P, Talley NJ, Leemon M, et al. Prevalence of gastrointestinal symptoms associated with diabetes mellitus: a population-based survey of 15,000 adults. Arch Intern Med. 2001;161(16):1989–1996.
- Horowitz M, Maddox AF, Wishart JM, et al. Relationships between oesophageal transit and solid and liquid gastric emptying in diabetes mellitus. Eur J Nucl Med. 1991;18(4):229–234.
- Horowitz M, Harding PE, Maddox AF, et al. Gastric and oesophageal emptying in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia. 1989;32(3):151–159.
- Schvarcz E, Palmér M, Ingberg CM, et al. Increased prevalence of upper gastrointestinal symptoms in long-term type 1 diabetes mellitus. Diabet Med. 1996;13(5):478–481.
- Enck P, Rathmann W, Spiekermann M, et al. Prevalence of gastrointestinal symptoms in diabetic patients and non-diabetic subjects. Z Gastroenterol. 1994;32(11):637–641.
- Ko GT, Chan WB, Chan JC, et al. Gastrointestinal symptoms in Chinese patients with type 2 diabetes mellitus. Diabet Med J Br Diabet Assoc. 1999;16(8):670–674.
- Ricci JA, Siddique R, Stewart WF, et al. Upper gastrointestinal symptoms in a U.S. national sample of adults with diabetes. Scand J Gastroenterol. 2000;35(2):152–159.
- Spångéus A, El-Salhy M, Suhr O, et al. Prevalence of gastrointestinal symptoms in young and Middle-aged diabetic patients. Scand J Gastroenterol. 1999;34(12):1196–1202.
- Drewes VM. Mechanical and electrical activity in the duodenum of diabetics with and without diarrhea. Pressures, differential pressures and action potentials. Am J Dig Dis. 1971;16(7):628–634.
- Whalen GE, Soergel KH, Geenen JE. Diabetic diarrhea. A clinical and pathophysiological study. Gastroenterology. 1969;56(6):1021–1032.
- Clouse RE, Lustman PJ. Gastrointestinal symptoms in diabetic patients: lack of association with neuropathy. Am J Gastroenterol. 1989;84(8):868–872.
- de Boer SY, Masclee AA, Lamers CB. Effect of hyperglycemia on gastrointestinal and gallbladder motility. Scand J Gastroenterol Suppl. 1992;194:13–18.
- Rayner CK, Verhagen MA, Hebbard GS, et al. Proximal gastric compliance and perception of distension in type 1 diabetes mellitus: effects of hyperglycemia. Am J Gastroenterol. 2000;95(5):1175–1183.
- Rayner CK, Samsom M, Jones KL, et al. Relationships of upper gastrointestinal motor and sensory function with glycemic control. Diabetes Care. 2001;24(2):371–381.
- Russo A, Sun WM, Sattawatthamrong Y, et al. Acute hyperglycaemia affects anorectal motor and sensory function in normal subjects. Gut. 1997;41(4):494–499.
- Concepción Zavaleta MJ, Gonzáles Yovera JG, Moreno Marreros DM, et al. Diabetic gastroenteropathy: an underdiagnosed complication. World J Diabetes. 2021;12(6):794–809.
- Koletzko L, Macke L, Schulz C, et al. Helicobacter pylori eradication in dyspepsia: new evidence for symptomatic benefit. Best Pract Res Clin Gastroenterol. 2019;40–41:101637.
- Revicki DA, Rentz AM, Dubois D, et al. Development and validation of a patient-assessed gastroparesis symptom severity measure: the Gastroparesis Cardinal Symptom Index. Aliment Pharmacol Ther. 2003;18(1):141–150.
- Dimenäs E, Glise H, Hallerbäck B, et al. Well-being and gastrointestinal symptoms among patients referred to endoscopy owing to suspected duodenal ulcer. Scand J Gastroenterol. 1995;30(11):1046–1052.
- Elfström P, Sundström J, Ludvigsson JF. Systematic review with meta-analysis: associations between coeliac disease and type 1 diabetes. Aliment Pharmacol Ther. 2014;40(10):1123–1132.
- Kylökäs A, Kaukinen K, Huhtala H, et al. Type 1 and type 2 diabetes in celiac disease: prevalence and effect on clinical and histological presentation. BMC Gastroenterol. 2016;16(1):76.
- Haupt-Jorgensen M, Holm LJ, Josefsen K, et al. Possible prevention of diabetes with a gluten-FREE diet. Nutrients. 2018;10(11):1746.
- Domínguez-Muñoz JE, D Hardt P, Lerch MM, et al. Potential for screening for pancreatic exocrine insufficiency using the fecal elastase-1 test. Dig Dis Sci. 2017;62(5):1119–1130.
