Abstract
Objectives
The introduction of anti-TNF therapy has revolutionized the management of inflammatory bowel disease (IBD). This study aimed to investigate the impact of anti-TNF therapy on emergency subtotal colectomy rates in patients with IBD (ulcerative colitis, Crohn’s disease or indeterminate colitis) during two time periods.
Methods
IBD patients treated with emergency subtotal colectomy for acute severe colitis at Skåne University Hospital, Sweden, during two six-year windows were included. The two time-windows represented pre- and introductory (2004–2009) versus post-introductory (2012–2017) anti-TNF therapy usage. The two periods were compared in terms of the proportion of patients who received anti-TNF therapy, rates of emergency subtotal colectomy, and local IBD prevalence numbers.
Results
In total 91 patients were included, 42 (2004–2009) and 49 (2012–2017) patients, respectively. The proportion of patients that received anti-TNF therapy prior to admission was increased from 29% (2004–2009) to 63% (2012–2017) (p = .001). Despite this no significant difference was found in the emergency subtotal colectomy rates between the time periods considering the population at risk (IBD patients living in Skåne county); 1.44/1000 person years versus 1.37/1000 person years (p = .83).
Conclusion
Despite an increased proportion of patients with IBD that received anti-TNF therapy prior to admission, no significant decrease in emergency subtotal colectomy rates was noted. Further research is warranted, and a prospective study design would facilitate a better causal understanding.
Introduction
Inflammatory bowel disease (IBD) has an increasing incidence and prevalence worldwide including Europe and Sweden [Citation1–4]. Recent studies might indicate a plateauing in the West [Citation5], but also report a rapid increase in the East and other newly industrialized geographical regions [Citation2,Citation5]. IBD can present as a highly severe and potentially mortal emergency in the form of acute severe colitis (ASC), irrespective of whether the underlying disease is ulcerative colitis (UC), Crohn’s disease (CD) or indeterminate colitis (IC). The vast majority of IBD-ASC are caused by UC. Up to 25% of patients with UC develop at least one episode of ASC [Citation6].
Historically, management of ASC comprised in-hospital surveillance and high dose steroid treatment, with subsequent colectomy in steroid refractory cases. In the mid 2000s, when studies had shown that anti-TNF therapy could induce disease remission and a reduction in colectomy rates in steroid refractory patients [Citation7], rescue treatment with anti-TNF therapy was added to the algorithm for ASC management [Citation6]. In some countries cyclosporine is viewed as a feasible alternative for rescue therapy, but due to toxicity concerns its use is not as widespread as anti-TNF therapy [Citation6]. Although studies have shown varying results, consensus is that anti-TNF therapy and other biologicals has led to a decline in surgery, hospitalizations and colectomies among the IBD patient population [Citation8–10]. Yet the effect of anti-TNF therapy on emergency colectomy rates is still uncertain.
This study aimed to investigate the impact of anti-TNF therapy on the rates of emergency subtotal colectomy for IBD-ASC, by comparing two time periods. Moreover, a secondary aim was to compare postoperative complications between the time periods. We hypothesized that emergency subtotal colectomy rates would decrease as a function of an increased proportion of patients being treated with anti-TNF therapy, with an increase in postoperative complications.
Material and methods
This retrospective comparative study was carried out at Skåne University Hospital, Sweden during 2020–2021. Two six-year windows were chosen for the study cohort, 2004–2009 as the pre- and introductory period for anti-TNF therapy and 2012–2017 served as the post introductory cohort. The pre- and introductory period was chosen as far back as digital medical chart records could be obtained. Earlier periods than 2004 would have required data extraction from paper medical charts and was not deemed feasible.
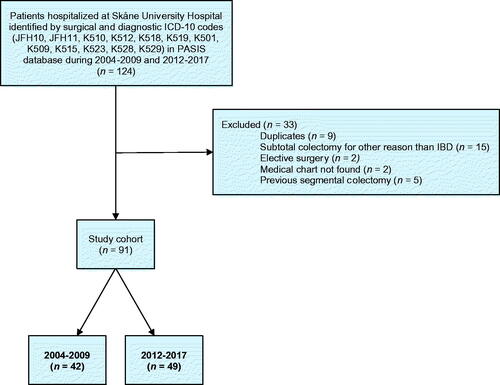
Patients hospitalized at Skåne University Hospital, Malmö and Lund, Sweden, were identified by the PASIS administration system and the ICD10 surgical procedure codes JFH10 and JFH11 (open or laparoscopic subtotal colectomy). The ICD-diagnosis codes K510 (total ulcerative colitis), K512 (ulcerative proctitis), K518 (other specified ulcerative colitis), K519 (ulcerative colitis), K501 (Crohn’s disease regional enteritis), K509 (Crohn’s disease), K515 (left sided colitis), K523 (indeterminate colitis), K528 (other non-specified non-infectious colitis), and K529 (non-infectious non-specified gastroenteritis/colitis) were included. Patient data were manually extracted from digital medical records. Comorbidities and pharmaceutical lists were validated through review of admission and discharge medical notes.
Prevalence data on IBD in Skåne county, Sweden, were extracted from the government agency Statistics Sweden and its affiliate the Statistical Database. The data represents the number of patients diagnosed with IBD in the specialized out-patient setting in Skåne county and serves as a proxy for the total IBD population at risk. Emergency subtotal colectomy was defined as subtotal colectomy due to ASC in patients with IBD that had been hospitalized. Emergency subtotal colectomy rates are reported as the number of emergency subtotal colectomies performed at Skåne University Hospital, Malmö and Lund, per 1000 person years of IBD in Skåne county in order to control for changes in prevalence numbers.
Statistical analysis was performed using IBM® SPSS® Statistics version 23.00 for Windows® (IBM Corp, Armonk, NY). Categorical variables are presented as numbers with percentages, and differences were calculated using Fisher’s exact test. The ordered categorical variables were analyzed with Linear-by-Linear Association. Continuous variables are presented as median with interquartile range, and differences were calculated using Mann-Whitney U-test. Statistical significance was defined as p ≤ .05. Ethical approval was granted from the national Swedish ethical committee (2020-07256). The regional quality database (KVB) also approved permission for data extraction.
Results
Ninety-one patients operated for IBD-ASC with emergency subtotal colectomy were included, 42 and 49 patients during 2004–2009 and 2012–2017, respectively ().
Clinical characteristics
No differences were found between the study cohorts regarding age, sex, comorbidity, length of hospital stay or length of postoperative hospital stay. UC was the most frequent histopathological diagnosis, followed by IC and CD, with no differences between the time periods (). Laparoscopic surgery was more commonly performed in 2012–2017 (; p = .001).
Table 1. Overview of clinical characteristics of patients who underwent emergency subtotal colectomy for inflammatory bowel disease acute severe colitis at Skåne University Hospital, Sweden, during 2004–2009 and 2012–2017.
Proportion of patients that received intravenous corticosteroids and anti-TNF therapy
Eighty percent of all patients received intravenous corticosteroids upon admission, without any difference between the study periods (79% versus 78%; p = .61). There was no difference between the number of days with intravenous corticosteroid treatment (p = .24).
A larger proportion of patients had been treated with anti-TNF therapy before hospital admission (29% versus 63%; p = .001). No significant differences were shown between the periods regarding the proportion of patients that received anti-TNF therapy after admission. Drug administration and characteristics are shown in .
Table 2. Administration, drug regimen and timing of anti-TNF therapy in patients who underwent emergency subtotal colectomy for inflammatory bowel disease acute severe colitis at Skåne University Hospital, Sweden, during 2004–2009 and 2012–2017.
Colectomy rates
The colectomy rates were 1.44/1000 person years versus 1.37/1000 person years for 2004–2007 and 2012–2017 respectively, with an incidence rate ratio of 0.95 (95% CI: 0.61–1.46, p = .83). There was an increase in IBD prevalence with 6770 person years from 2004–2009 to 2012–2017 ().
Table 3. Number of emergency subtotal colectomies performed at Skåne University Hospital in relation to disease prevalence of inflammatory bowel disease in Skåne county during 2004–2009 and 2012–2017.
Postoperative complications
No differences were detected pertaining overall postoperative complications within 30 days (p = .68) nor in infectious, cardiovascular, neurological or surgical complications. Furthermore, no differences were found in unplanned reoperations, re-admissions, nor postoperative mortality ().
Table 4. Postoperative complications within 30 days in patients who underwent emergency subtotal colectomy for inflammatory bowel disease acute severe colitis at Skåne University Hospital, Sweden, during 2004–2009 and 2012–2017.
Discussion
Our study found a statistically significant increase in the proportion of patients receiving anti-TNF therapy prior to admission during 2012–2017 as compared with 2004–2009. Despite this, emergency subtotal colectomy rates were unaltered and postoperative complications unchanged. This suggests that anti-TNF therapy does not impact emergency colectomy rates but appears safe in terms of postoperative complications.
Our study focused on emergency subtotal colectomies as they are the end results of failed rescue therapy. Disease severity might have served as a selection bias in our study population, and there is a possibility that there is a reduction in colectomy rates, but for less aggressive disease progression [Citation11]. We did however observe an increase of nearly 7000 person years of IBD prevalence in the studied region, Skåne county, consistent with other observations [Citation1–5,Citation12]. A decrease in colectomy rates might therefore be statistically difficult to prove in a retrospective cohort. To elucidate a true causal relationship between anti-TNF therapy and emergency colectomy rates for IBD-ASC, one would require a randomized clinical trial which may be ethically problematic.
Our findings are opposite to a similar study conducted in Finland [Citation12]. In contrast to their study, we only studied emergency subtotal colectomies i.e., patients with steroid refractory disease whereas Kolehmainen et al. included patients with dysplasia and chronic disease [Citation12]. Only emergency subtotal colectomies performed at Skåne University Hospital were included in this study, and since other hospitals in Skåne county also perform this treatment for ASC the total rate of emergency subtotal colectomy in Skåne county could not be presented. This is reflected in the low ratio of emergency subtotal colectomies per 1000 person years presented. Furthermore, the catchment area for Skåne University Hospital changed during the studied periods and might have affected the results.
A higher proportion of patients received anti-TNF therapy prior to admission in the latter study period. There is a possibility that the post-introductory cohort to a higher extent consisted of anti-TNF non-responders, or loss-of-response patients. It stands to be argued that if a patient that is already treated with anti-TNF, is hospitalized due to ASC, the chances of clinical remission with further anti-TNF therapy would be diminished. For these patients, perhaps a different mode of action should be tried, such as cyclosporine, tofacitinib or ustekinumab, either alone or in combination with anti-TNF [Citation13,Citation14]. However, increased risks for adverse events with combination therapies must be considered.
The short- and long-term effects on colectomy rates after the introduction of anti-TNF therapy have been studied with conflicting results. Some studies have shown decreased colectomy rates, while others have suggested both increased and non-significant differences in colectomy rates [Citation8–10,Citation12,Citation15–25]. These studies have been somewhat confounded by heterogeneity in disease severity, indication for surgery, treatment protocol and the overall increasing incidence of IBD worldwide, making causal statements regarding the true effect on surgical rates challenging to infer. However, a global trend toward decreased colectomy rates irrespective of anti-TNF therapy has been described [Citation6,Citation23,Citation24]. It is thus possible that the increased proportion of patients having received anti-TNF therapy prior to admission in the more recent cohort (63% versus 29%) impacted the rate of elective colectomies (not investigated in this study), while the rates of emergency colectomies remained unchanged.
We did not find any significant differences in 30-day postoperative complications despite the higher proportion of patients having received anti-TNF therapy in the latter cohort. This is in accordance with a large population-based study in the UK that found no association between preoperative anti-TNF use and postoperative complications after subtotal colectomy for UC-ASC [Citation26]. Earlier studies have mainly pointed to a higher risk for anastomotic insufficiency and septic complications in relation to one-stage restorative proctocolectomy [Citation27]. Our results imply that regardless of the underlying type of IBD, anti-TNF therapy appears safe. Additionally, other factors such as surgical method, subtotal colectomy and ileostomy instead of one-stage restorative proctocolectomy compounded by an increased percentage of laparoscopic operations, may have influenced postoperative outcomes.
In both cohorts we found that a small percentage (12% and 18%, respectively) of patients had received unconventional rescue treatment with adalimumab. All such instances were due to a loss-of-response to infliximab in the outpatient setting, allergic reactions to infliximab or obstacles to intravenous administration.
This study had some inherent weaknesses in its retrospective design including the inability to assert causality and that the study cohort was small. Causality is further obscured by the lack of data on other medical treatments than anti-TNF therapy and corticosteroids in the cohorts, which could have affected the outcomes. Strengths of the study include that data extraction was internally validated with few missing data. The study cohorts were comparable in their constitution and represented the specific patient population adequately.
Conclusion
Despite an increased proportion of patients with IBD that received anti-TNF therapy prior to admission in the outpatient setting, no significant decrease in emergency subtotal colectomy rates for IBD-ASC was observed. This suggests that anti-TNF therapy might not be effective for reducing the need for emergency subtotal colectomies at the group-level. There are questions as to unintentional selection biases for non-responding patients in the latter cohort, which could have had an impact on the results. We observed no increase in postoperative complications despite higher proportions of IBD-patients being treated with anti-TNF therapy prior to admission, as such anti-TNF therapy seems to be safe in relation to surgery. Further research is warranted on both emergency and elective colectomy populations, with special focus on anti-TNF therapy non-responders and loss-of-response patients.
Previous communication
This paper was presented as a poster at the virtual Annual Meeting of the European Society of Coloproctology, 22–24 September 2021.
Disclosure statement
JM has served as a speaker, consultant or advisory board member for AbbVie, Bayer, Bristol-Myers Squibb, Ferring, Hospira, Janssen, MSD, Otsuka, Pfizer, Sandoz, Svar, Takeda, Tillotts and UCB Pharma, and has received grant support from AbbVie, Calpro AS, Ferring, Fresenius Kabi, Pfizer and Takeda. SS, RSN, ER, ST and PB report no conflict of interest.
Data availability statement
The data that support the findings of this study are available from the corresponding author, SS, upon reasonable request.
References
- Sairenji T, Collins KL, Evans DV. An update on inflammatory bowel disease. Prim Care. 2017;44(4):673–692.
- Kaplan GG. The global burden of IBD: from 2015 to 2025. Nat Rev Gastroenterol Hepatol. 2015;12(12):720–727.
- Busch K, Ludvigsson JF, Ekstrom-Smedby K, et al. Nationwide prevalence of inflammatory bowel disease in Sweden: a population-based register study. Aliment Pharmacol Ther. 2014;39(1):57–68.
- Burisch J, Jess T, Martinato M, et al. The burden of inflammatory bowel disease in Europe. J Crohns Colitis. 2013;7(4):322–337.
- Mak WY, Zhao M, Ng SC, et al. The epidemiology of inflammatory bowel disease: East meets west. J Gastroenterol Hepatol. 2020;35(3):380–389.
- Hindryckx P, Jairath V, D’Haens G. Acute severe ulcerative colitis: from pathophysiology to clinical management. Nat Rev Gastroenterol Hepatol. 2016;13(11):654–664.
- Jarnerot G, Hertervig E, Friis-Liby I, et al. Infliximab as rescue therapy in severe to moderately severe ulcerative colitis: a randomized, placebo-controlled study. Gastroenterology. 2005;128(7):1805–1811.
- Reich KM, Chang HJ, Rezaie A, et al. The incidence rate of colectomy for medically refractory ulcerative colitis has declined in parallel with increasing anti-TNF use: a time-trend study. Aliment Pharmacol Ther. 2014;40(6):629–638.
- Khoudari G, Mansoor E, Click B, et al. Rates of intestinal resection and colectomy in inflammatory bowel disease patients after initiation of biologics: a cohort study. Clin Gastroenterol Hepatol. 2022;20:e974–e983.
- Barnes EL, Jiang Y, Kappelman MD, et al. Decreasing colectomy rate for ulcerative colitis in the United States Between 2007 and 2016: a time trend analysis. Inflamm Bowel Dis. 2020;26 (8):1225–1231.
- Candido FD, Fiorino G, Spadaccini M, et al. Are surgical rates decreasing in the biological era In IBD? Curr Drug Targets. 2019;20(13):1356–1362.
- Kolehmainen S, Lepisto A, Farkkila M. Impact of anti-TNF-alpha therapy on colectomy rate and indications for colectomy in ulcerative colitis: comparison of two patient cohorts from 2005 to 2007 and from 2014 to 2016. Scand J Gastroenterol. 2019;54(6):707–711.
- Honap S, Pavlidis P, Ray S, et al. Tofacitinib in acute severe ulcerative colitis-A real-world tertiary center experience. Inflamm Bowel Dis. 2020;26(11):e147–e149.
- Ochsenkühn T, Tillack C, Szokodi D, et al. Clinical outcomes with ustekinumab as rescue treatment in therapy-refractory or therapy-intolerant ulcerative colitis. United European Gastroenterol J. 2020;8(1):91–98.
- Devaraj B, Kaiser AM. Surgical management of ulcerative colitis in the era of biologicals. Inflamm Bowel Dis. 2015;21(1):208–220.
- Kin C, Kate Bundorf M. As infliximab use for ulcerative colitis has increased, so has the rate of surgical resection. J Gastrointest Surg. 2017;21(7):1159–1165.
- Moore SE, McGrail KM, Peterson S, et al. Infliximab in ulcerative colitis: the impact of preoperative treatment on rates of colectomy and prescribing practices in the province of British Columbia, Canada. Dis Colon Rectum. 2014;57(1):83–90.
- Narula N, Marshall JK, Colombel JF, et al. Systematic review and meta-analysis: infliximab or cyclosporine as rescue therapy in patients with severe ulcerative colitis refractory to steroids. Am J Gastroenterol. 2016;111(4):477–491.
- Oh SJ, Shin GY, Soh H, et al. Long-term outcomes of infliximab in a real-world multicenter cohort of patients with acute severe ulcerative colitis. Intest Res. 2021;19(3):323–331.
- Patrick D, Doecke JD, Irwin J, et al. Short‐term colectomy is avoided in over half of regional patients failing medical therapy for acute severe ulcerative colitis with co‐ordinated transfer and tertiary care. Intern Med J. 2020;50(7):823–829.
- Rajan R, Trinder MW, Lo J, et al. Assessing the efficacy of TNF-alpha inhibitors in preventing emergency and emergent colectomies. JGH Open. 2020;4(2):140–144.
- Szemes K, Soos A, Hegyi P, et al. Comparable long-term outcomes of cyclosporine and infliximab in patients with steroid-refractory acute severe ulcerative colitis: a meta-analysis. Front Med (Lausanne). 2019;6:338.
- Argollo MC, Kotze PG, Spinelli A, et al. The impact of biologics in surgical outcomes in ulcerative colitis. Best Pract Res Clin Gastroenterol. 2018;32-33:79–87.
- Kaplan GG, Seow CH, Ghosh S, et al. Decreasing colectomy rates for ulcerative colitis: a population-based time trend study. Am J Gastroenterol. 2012;107(12):1879–1887.
- Verdon C, Reinglas J, Coulombe J, et al. No change in surgical and hospitalization trends despite higher exposure to anti-tumor necrosis factor in inflammatory bowel disease in the Québec provincial database FROM 1996 to 2015. Inflamm Bowel Dis. 2021;27(5):655–661.
- Ward ST, Mytton J, Henderson L, et al. Anti-TNF therapy is not associated with an increased risk of post-colectomy complications, a population-based study. Colorectal Dis. 2018;20(5):416–423.
- Billioud V, Ford AC, Tedesco ED, et al. Preoperative use of anti-TNF therapy and postoperative complications in inflammatory bowel diseases: a meta-analysis. J Crohns Colitis. 2013;7(11):853–867.