Abstract
Objective
To establish a generally accepted Danish definition of dysphagia to enhance collaboration across sectors and professions.
Methods
The study was initiated by a multi-professional group of experienced researchers and board members of the Danish Society for Dysphagia. We used a modified Delphi methodology to achieve consensus among experienced health care professionals from different professions and contexts. The initial stage consisted of a literature search leading to the draft of different definitions followed by two Delphi rounds between professionals and a stakeholder consultation round.
Results
We conducted two Delphi rounds until one definition was clearly preferred. A total of 194 participants responded in round one, and 279 in round two. Both rounds had a broad representation of sectors and geography and most participants had worked with dysphagia for more than four years.
Conclusion
The preferred definition was ‘Dysphagia is a functional impairment that either prevents or limits the intake of food and fluids, and which makes swallowing unsafe, inefficient, uncomfortable or affects quality of life’. The definition was widely accepted among different health professional groups, patients and across sectors.
Introduction
Dysphagia is a common symptom in many patients and elderly with a prevalence ranging from <5% in healthy individuals [Citation1] to 50–87% in geriatric patients and nursing home residents [Citation2,Citation3]. The word dysphagia comes from Greek: dys = difficulty and fagi = eating, and dysphagia is often referred to as difficulty in swallowing [Citation4] but there is no clear definition of dysphagia. In the previous mentioned papers, definition of dysphagia ranged from self-reported answer to the question 'In the last year, how often have you had difficulty swallowing’ to performing screening tests for dysphagia. Dysphagia has significant consequences for both the individual, and for society. Individuals experiencing dysphagia are at risk of e.g. malnutrition, social isolation, reduced quality of life, aspiration pneumonia and death leading to several contacts with both the healthcare system, and municipal healthcare each year [Citation4,Citation5]. The complexity of dysphagia, which has many different expressions, causes and consequences, combined with poor communication and misunderstandings among health professionals may negatively affect the individual’s likelihood of receiving the appropriate assessments and treatments [Citation4,Citation5]. For example, if an elderly otherwise healthy individual adjusts intake of food and water based on a functional decline, disagreements or unawareness whether this is dysphagia may prolong the referral to appropriate assessment and treatment. A national standardized definition of dysphagia will allow for a common language and understanding of dysphagia among health professionals, care providers and researchers which is pivotal to facilitate and improve quality of care and patient safety.
The aim of this study was to establish a generally accepted Danish definition of dysphagia for application across different specialties, sectors and professions working with dysphagia to enhance the collaboration between sectors and professions.
Methods
In this study we used a modified Delphi methodology [Citation6–9] to achieve consensus among experienced health care professionals from different professions and contexts. The study was initiated by a multi-professional group of experienced researchers and board members of the Danish Society for Dysphagia and was led by a work group of four authors (SJE, JD, HM, and DM). A Danish protocol for the process was drafted a priori and can be retrieved upon request.
The modified Delphi process
A multi-professional panel of experts advised the work group throughout the Delphi process [Citation6,Citation8–10]. Members of the expert panel were identified by the board of the Danish Society of Dysphagia. In addition to the use of snowball recruitment to achieve maximum variation in professions and medical fields, members of the expert panel suggested additional members for the expert panel e.g. if a relevant expert in an area was not already represented. The final expert panel consisted of six physicians, a dietitian, a nurse, three occupational therapists, a physical therapist and a speech therapist. The expert panel represented a broad range of specialities (intensive care, oto-rhino-laryngology, gastroenterology, neurology, oncology, geriatrics, paediatrics) and sectors (universities, university hospitals, regional hospitals, general practice and municipal healthcare).
Literature search
The initial stage consisted of a literature search for definitions of dysphagia in the electronic bibliographic databases: PubMed, Embase, Cochrane Library. Selected key words were: ‘dysphagia’; ‘deglutition disorder′; ‘swallowing disorder′; ‘mastication′; ‘chewing disorder’; and ‘definition’; ‘define’; ‘defines’; ‘defined’. The search was limited to records in English, German, Danish, Norwegian, or Swedish. A total of 104 records were identified and imported into Covidence, which is an electronic tool supporting the workflow of screening, and independently assessing papers for inclusion. All records were in English, German or Danish.
Four authors (SJE, JD, HM, and DM) independently screened title and abstracts of all retrieved citations for eligibility, all citations were screened by two authors. Eligibility was based on whether the paper had a delimitation of dysphagia, even if vague. Disagreements were solved through discussion until consensus was reached. Subsequently, eight eligible articles were reviewed in full-text [Citation11–18]. No limits for year of publication were set, and as only eight articles were identified, they were all included for further review. All full-text articles were discussed in the work group until consensus was achieved. None of the articles contained an exact definition of dysphagia. In addition to the retrieved literature, definitions from the International Classification of Disease (ICD-10), World Health Organization (WHO) and European Society for Swallowing Disorders (ESSD) white paper in Geriatrics [Citation19] were included. All articles and definitions were presented in a consensus meeting aimed at drafting proposals for the Danish definition of dysphagia by the work group.
In the first meeting, the expert panel was presented with the drafts of seven definitions from the working group and these were discussed in depth and subsequently refined.
The two survey rounds
For the first round, a survey consisting of the seven definitions () was set up in the Research Electronic Data Capture system (REDCap) [Citation20]. In the survey, participants were asked to rate each definition on a visual analogue scale (VAS) from 0 (not suitable) to 100 (perfect) and to point out key words contained in that definition. Participants were encouraged to propose changes to the initial proposed definitions. No level of consensus was specified a priori.
Table 1. Definitions of dysphagia.
Before distribution, the functionality of the survey was piloted by the members of the expert panel. The first round was distributed by e-mail to all members of the Danish Society for Dysphagia on 8 June 2021. Members were encouraged to forward the survey through other relevant channels, networks, forums, work place and colleagues. The survey was also shared on social media and on the webpage of the society. A reminder to respond to the survey was issued after 45 days; the survey was closed on 9 October 2021.
The expert panel reviewed and discussed findings from round one of the survey and planned round two of the survey. All comments on aspects of the definitions were discussed and considered, this resulted in minor refinements that were made for round two. On 13 October 2021 a second survey containing the four highest ranking definitions were distributed to the participants who responded to the first round via e-mail and all members of the Danish Society for Dysphagia, as well as other identified relevant forums and members were encouraged to distribute the survey throughout their network. As a result of the skewness of professions responding to the survey in round one, special attention was paid to elicit responses from a broader range of professionals. After round two, the expert panel identified the definition, which consistently ranked highest among all professionals across both rounds as the final definition.
Analysis of data from round 1 and 2 was led by JRJ, who was not a board member of the Danish Society for Dysphagia. Prior to publication, all proposed definitions were translated into English by SJE and AHN and back-translated to Danish by a Danish speech language therapist residing in the United Kingdom and compared for accuracy. Original Danish definitions are available as online supplement (Supplementary Table 1).
Patient and public involvement
A final stakeholder round was attempted to capture patients’ perceptions of the final definition. A total of 10 patient organizations and patient networks were contacted for identification of patient representatives willing to participate in the stakeholder round. A short electronic questionnaire was issued to patients by e-mail asking them to reflect on the suitability of the final definition.
Ethical considerations
Participation in the Delphi study was voluntary. All data were anonymised before being shared with the expert panel. Patients received written information about the study and gave written consent to participation before completing the questionnaire of the stakeholder round. Patients were allowed to save a copy of their responses and withdraw their data afterwards if so desired although no one chose to. The study was conducted in accordance with the Helsinki Declaration [Citation21] and reported using the CREDES guideline for reporting Delphi studies [Citation22].
Results
A total of 194 participants responded in round one and 279 in round two. A wide range of different health care professions were represented, though most participants were occupational therapists (). This probably reflects that in Denmark health care occupational therapists are the main profession in diagnosing and rehabilitating patients with dysphagia. Nurses were not well-represented in round one and special efforts were made to recruit nurses for round two. Both rounds had a broad representation of sectors and geography and most participants had worked with patients with dysphagia for more than four years ().
Table 2. Characteristics of respondents.
Results of round one
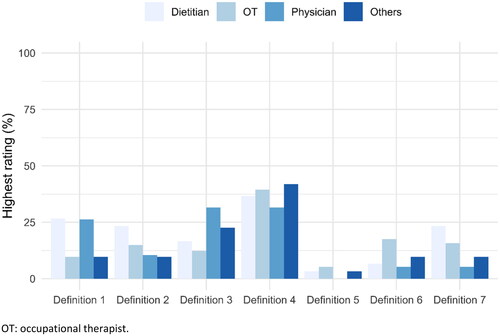
shows the distribution of rating for each of the seven definitions in round one as boxplots with surrounding violin plots (blue area). Six of the seven definitions received a median score above 50 mm on the VAS (except definition 5) (). For an overview of definitions, see . Definition four received the highest rating in round one. Most professions favored definition four, however physicians favored definition three ().
Figure 1. Distribution of rating for each of the seven definitions in round one. VAS: Visual Analogue Scale.
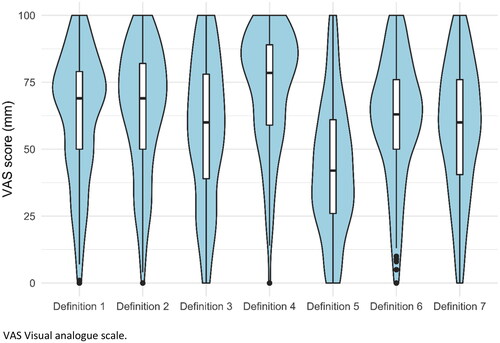
Figure 2. Highest rated definition in round one according to profession. OT: occupational therapist.
There was no systematic pattern in free text comments and selections of keywords that gave rise to changes in the definitions. The expert panel decided that a second round was required, as there was no definition clearly outperforming any of the others. The four best performing definitions (1–4) were retained for round two. Definitions one, two, and four were chosen due to their overall score, while definition three was chosen as it was the most favored definition among physicians.
Results of round two
More participants favored definition four as the best definition in round two (46%) () and the median VAS score for this definition was 82 (interquartile range 62–93). All professions favored definition four in round two (data not shown).
Figure 3. All participants’ ranking of definitions in round two. 1 = highest ranking; 4 = lowest ranking.
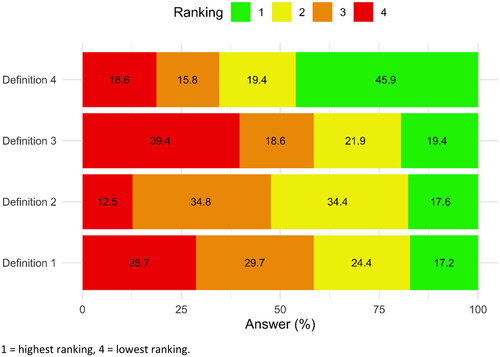
The consensus committee decided that there was no need for a third round as definition four () was unanimously favored across and between professions in both rounds. Furthermore, there were no systematic pattern in free text comments that gave rise to changes in the definitions or repeated rounds in the Delphi procedure.
Only three patients and two health care professionals from 10 patient organizations replied to the short survey. Most of them found the definition to adequately cover their perception of dysphagia although one patient found it difficult to relate to the question as the patient had not yet experienced problems related to swallowing.
Discussion
In this Delphi study, 279 health care professionals favored the definition in which dysphagia was a functional impairment that either prevents or limits the intake of food and fluids, and which makes swallowing unsafe, inefficient, uncomfortable or affects quality of life. This definition omits etiologies of dysphagia and focuses primarily on symptoms and experience of dysphagia. Although, in the first round, physicians favored the simplest definition most similar to the ICD-10 diagnostic criteria for unspecified dysphagia, they accepted the broader definition brought by the multi-professional approach in round 2.
As swallowing is a complex process, there are many causes of dysphagia. Reasons for developing dysphagia may depend on the patient’s medical history, general constitution and precipitating factors. Within geriatrics, dysphagia is considered a part of the geriatric syndrome, which is closely linked to a functional decline [Citation19]. In other words, development of dysphagia may be related to growing old and frail. Within oncology, dysphagia may be related to the cancer, surgery, chemo-radiation therapy of head and neck, or esophagus. In this case, dysphagia may be related to altered anatomical structures or/and xerostomia [Citation23,Citation24], whereas development of dysphagia in patients suffering from stroke or Parkinson’s disease is primarily neurological [Citation25]. As such, reasons for developing dysphagia are multiple and diverse and it may be impossible to include a comprehensive list of reasons for dysphagia for a generally accepted definition of dysphagia. Leslie and Smithard [Citation26] addressed this gap between a broad, general definitions of dysphagia and more specific definitions targeting dysphagia of particular etiologies in an online, cross-sectional survey of self-reported dysphagia. Leslie and Smithard [Citation26] used a 10 items questionnaire (EAT-10) to estimate dysphagia, and found a discrepancy between participants’ EAT-10 scores suggesting dysphagia and participants stating in free text that they did not experience swallowing problems. According to Leslie and Smithard [Citation26] this may suggest that dysphagia is either under-diagnosed or that normal swallowing is more varied than previously assumed. This shows that since dysphagia is both complex and subtle, there is a need for a clear comprehensive definition of dysphagia but also clearly delineated subtypes of dysphagia to support research purposes [Citation26].
The definition from this study, however, clearly puts experience of dysphagia at the center, which is supported by responses from the involved patient organizations. Moreover, focusing on the clinical presentation of dysphagia could establish some common ground between health care professionals from different professions, specialties and across sectors. A review by Donovan et al. [Citation27] on interprofessional care and teamwork in the intensive care unit distinguishes between (1) multi-professional care where different professional groups work alongside to care for the patient and (2) inter-professional care, where a higher level of integration between the activities of each professional group is established. According to Donovan, inter-professional care is guided by mutual goals for the patient and appreciation for how each team member may contribute to help the patient [Citation27]. Also Hall [Citation28] describes how collaboration between health professionals can provide a positive synergistic influence on patient care when team members are prepared to share skills and acknowledge the contribution from other groups. However, history of professional cultures have often had a hierarchical structure that has limited collaboration between professional groups [Citation28]. On this background, a structured consensus process such as the Delphi process among different healthcare professions, may provide a common ground for discussing dysphagia and for working towards better and more coordinated approaches to provide care for patients with dysphagia across sectors and professions.
Strengths and limitations
A majority of participants in this study were occupational therapists, which reflects clinical practice in Denmark. For the second round a variation and more equal distribution of professions was prioritized, however this limited new participants’ opportunity to reflect on previous positions. The first round of the Delphi study did not elicit any responses that could have prompted other definitions or refined phrasings of the definitions and therefore, focus came to be on agreement among participants. However, the chosen definition was supported equally in different professional groups. An a priori limit on agreement or preferability of definitions could have been set, however the method of discussion and subsequent consensus in the expert panel was chosen to provide opportunity for analysis beyond a pre-set cut off percentage.
Conclusion
The Delphi study resulted in a Danish definition of dysphagia which translated to English was ‘A functional impairment that either prevents or limits the intake of food and fluids, and which makes swallowing unsafe, inefficient, uncomfortable or affects quality of life’. The definition was widely accepted among patients and Danish health professionals from all sectors, and it may be useful when developing multi-professional guidelines or pathways across sectors for patients with dysphagia. For research purposes, more clearly defined subtypes of dysphagia may be necessary to discriminate between subtle symptoms of dysphagia and their causes.
Ethical approval
Ethical approval for the study was not sought as Danish law does not require ethical approval for questionnaire studies, nor give the option for this.
Supplemental Material
Download PDF (36.3 KB)Acknowledgements
Paediatrician Iben Møller Jønsson, Department of Paediatrics and Adolescent Medicine, Aarhus University Hospital, Denmark; Speech therapist Signe Grøn, Rigshospitalet Glostrup, Denmark and Physical therapist Signe Secher, Hammel Neuro-Rehabilitation and Research Centre, Denmark for participating in the expert panel. Speech and language therapist Janne Schack, Dorset HealthCare University, United Kingdom for help with translation of the definitions.
Additional information
Funding
References
- Cho SY, Choung RS, Saito YA, et al. Prevalence and risk factors for dysphagia: a USA community study. Neurogastroenterol Motil. 2015;27(2):212–219.
- Melgaard D, Rodrigo-Domingo M, Mørch MM. The prevalence of oropharyngeal dysphagia in acute geriatric patients. Geriatrics. 2018;3(2):15.
- Cook IJ. Oropharyngeal dysphagia. Gastroenterol Clin North Am. 2009;38(3):411–431.
- Philipsen BB, Mortensen HR, Melgaard D. Dysphagia. Ugeskr Laeger. 2019;181(9):V09180594.
- McCarty EB, Chao TN. Dysphagia and swallowing disorders. Med Clin North Am. 2021;105(5):939–954.
- Hsu C, Sandford BA. The delphi technique: making sense of consensus. Pract Assess Res Eval. 2007;12:10.
- Murphy MK, Black NA, Lamping DL, et al. Consensus development methods, and their use in clinical guideline development: a review. Health Technol Assess. 1998;2(3):i.
- Keeney S, Hasson F, McKenna H. Consulting the oracle: ten lessons from using the Delphi technique in nursing research. J Adv Nurs. 2006;53(2):205–212.
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–1015.
- Jones J, Hunter D. Consensus methods for medical and health services research. BMJ. 1995;311(7001):376–380.
- Aggarwal N, Lopez R, Gabbard S, et al. Spectrum of esophageal dysmotility in systemic sclerosis on high-resolution esophageal manometry as defined by Chicago classification. Dis Esophagus. 2017;30(12):1–6.
- Bredenoord AJ, Fox M, Kahrilas PJ, International High Resolution Manometry Working Group, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(Suppl 1):57–65.
- Cichero JA, Altman KW. Definition, prevalence and burden of oropharyngeal dysphagia: a serious problem among older adults worldwide and the impact on prognosis and hospital resources. Nestle Nutr Inst Workshop Ser. 2012;72:1–11.
- Eypasch EP, Stein HJ, DeMeester TR, et al. A new technique to define and clarify esophageal motor disorders. Am J Surg. 1990;159(1):144–151.
- Nicholls D, Bryant-Waugh R. Eating disorders of infancy and childhood: definition, symptomatology, epidemiology, and comorbidity. Child Adolesc Psychiatr Clin N Am. 2009;18(1):17–30.
- Phillips SF. Dysmotility syndromes: what can be defined? Ir J Med Sci. 1994;163(12):552–554.
- Rateitschak KH, Fistarol AF, Wolf HF. Parafunctions (definition, incidence, causes, sequelae, diagnosis, therapy). SSO Schweiz Monatsschr Zahnheilkd. 1966;76(3):289–309.
- Zerbib F, Roman S. Current therapeutic options for esophageal motor disorders as defined by the Chicago classification. J Clin Gastroenterol. 2015;49(6):451–460.
- Baijens LW, Clavé P, Cras P, et al. European society for swallowing disorders – European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging. 2016;11:1403–1428.
- Harris PA, Taylor R, Minor BL, REDCap Consortium, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
- The World Medical Association. WMA Declaration of Helsinki – ethical principles for medical research involving human subjects; 2013 [cited 2022 Nov 27]. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
- Jünger S, Payne SA, Brine J, et al. Guidance on conducting and REporting DElphi studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med. 2017;31(8):684–706.
- Baijens LWJ, Walshe M, Aaltonen LM, et al. European white paper: oropharyngeal dysphagia in head and neck cancer. Eur Arch Otorhinolaryngol. 2021;278(2):577–616.
- Yuen MTY, Tsang RK, Wong IYH, et al. Long-term pharyngeal dysphagia after esophagectomy for esophageal cancer–an investigation using videofluoroscopic swallow studies. Dis Esophagus. 2019;32:1–9.
- Takizawa C, Gemmell E, Kenworthy J, et al. A systematic review of the prevalence of oropharyngeal dysphagia in stroke, Parkinson’s disease, Alzheimer’s disease, head injury, and pneumonia. Dysphagia. 2016;31(3):434–441.
- Leslie P, Smithard DG. Is dysphagia Under diagnosed or is normal swallowing more variable than we think? Reported swallowing problems in people aged 18–65 years. Dysphagia. 2021;36(5):910–918.
- Donovan AL, Aldrich JM, Gross AK, et al. Interprofessional care and teamwork in the ICU. Crit Care Med. 2018;46(6):980–990.
- Hall P. Interprofessional teamwork: professional cultures as barriers. J Interprof Care. 2005;19(Suppl 1):188–196.
