Abstract
Background
Endoscopic management of large bile duct stones may be challenging and refractory to standard endoscopic retrograde cholangiopancreatography (ERCP) techniques. To this end, per-oral cholangioscopy (POC)-guided electrohydraulic lithotripsy (EHL) or laser lithotripsy (LL) has been increasingly utilized during ERCP. There are limited data, however, comparing EHL and LL in the management of choledocholithiasis. Therefore, the aim was to analyze and compare the efficacy of POC-guided EHL and LL for the treatment of choledocholithiasis.
Methods
A database search on PubMed was performed selecting prospective English-language articles published by September 20th, 2022, in accordance with PRISMA guidelines. Studies selected included bile duct clearance as an outcome.
Results
A total of 21 prospective studies (15 using LL, 4 using EHL, and 2 both) including 726 patients were included for analysis. Complete ductal clearance was achieved in 639 (88%) patients with 87 (12%) patients having incomplete ductal clearance. Patients treated with LL had an overall median stone clearance success rate of 91.0% (IQR, 82.7–95.5), whereas EHL achieved a median stone clearance success rate of 75.8% (IQR, 74.0–82.4), [p = .03].
Conclusions
LL is a highly effective form of POC-guided lithotripsy for the treatment of large bile duct stones, particularly when compared to EHL. However, direct, head-to-head randomized trials are needed to identify the most effective form of lithotripsy for treating refractory choledocholithiasis.
Introduction
For the last several decades, endoscopic retrograde cholangiopancreatography (ERCP) with the use of a basket catheter, balloon catheter, or mechanical lithotripter following endoscopic sphincterotomy and/or endoscopic papillary large-balloon dilation has become first-line therapy for managing choledocholithiasis [Citation1]. Complete stone clearance may not be achieved in a single procedure, and multiple ERCP sessions may be required to manage large, multiple, impacted, intrahepatic, or cystic duct stones [Citation2,Citation3]. Moreover, if stone clearance of the bile ducts is not achieved using standard techniques, patients may need to undergo percutaneous transhepatic biliary drainage (PTBD) or surgical bile duct exploration [Citation2,Citation3]. Therefore, in order to maximize endoscopic stone clearance and avoid the need for more invasive procedures, per-oral cholangioscopy (POC) has been increasingly utilized during ERCP, providing the endoscopist with direct visualization of the stones and the ability to perform stone fragmentation with either electrohydraulic lithotripsy (EHL) or laser lithotripsy (LL) [Citation4,Citation5].
The development of the mother-daughter choledochoscope (cholangioscope) in the 1990s revolutionized intraductal lithotripsy, permitting direct visualization and control of the fiber [Citation6–11]. To overcome the need for two trained endoscopists to perform the procedure, single-operator cholangioscopy (SOC) was developed in the late 2000s, greatly simplifying the practice of cholangioscopy [Citation5]. Regarding the lithotripsy modalities, EHL systems work through a bipolar probe and a charge generator; transmitting a charge across the electrodes at the tip of the probe generates a spark. This determines the expansion of the surrounding fluid and finally results in an oscillating shock wave of pressure that fragments the stones [Citation12]. Under direct visualization, the probe is directed at the stone positioned at least 5 mm from the tip of the cholangioscope and 1–2 mm from the stone. On the other hand, LL systems work by focusing laser light (typically holmium) of a high-power density on the surface of a stone. The concentrated high power creates a plasma composed of a gaseous collection of ions and free electrons that oscillates and induces waves fracturing the stone surface [Citation12].
Choosing between EHL and LL, however, remains a topic of debate. In clinical practice, endoscopist preferences and expertise along with resource availability play a key role in the decision-making process of the therapeutic strategy. Each of these modalities has its own advantages and disadvantages. For example, although EHL utilizes less expensive equipment, ductal perforation rates have been traditionally higher than LL [Citation12,Citation13]. On the other hand, LL enables more precise targeting of stones but requires additional resources such as a laser-safe procedure room and a separate technician to operate the laser machine [Citation14]. In light of these increasingly utilized lithotripsy modalities, this systematic review aimed to analyze and compare the efficacy of POC-guided EHL and LL for the treatment of choledocholithiasis.
Methods
Clinical question
Through this systematic review, we sought to address the following clinical question: In patients with refractory choledocholithiasis, how does POC-guided LL compare with POC-guided EHL in facilitating bile duct stone clearance? Refractory choledocholithiasis was defined as the presence of stones in the bile ducts that was not successfully removed with ERCP using conventional methods including sphincterotomy with or without sphincteroplasty, balloon extraction, and basket extraction.
Literature search strategy
A systematic database search on PubMed was conducted for this review. A Boolean search strategy combined the search terms ‘Choledocholithiasis’, ‘Laser lithotripsy’, ‘Electrohydraulic lithotripsy’, ‘Bile duct stone’, ‘Stone clearance’ and ‘Cholangioscopy’.
We searched relevant English-language articles published by September 20th, 2022 with no restriction on the earliest publication date. The search strings were stone clearance and each of the following: choledocholithiasis, ‘Choledocholithiasis/therapy’[Mesh] choledocholithiasis treatment, bile duct stones, large bile duct stones, laser lithotripsy, electrohydraulic lithotripsy, cholangioscopy guided lithotripsy, endoscopic retrograde cholangiopancreatography.
Eligibility criteria
This systematic review was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guidelines [Citation15]. We assessed the studies by examining the title, abstract, and/or full text of the studies. References of included studies were also examined to possibly identify additional studies.
Studies included met the following eligibility criteria: (1) Studies involving POC-guided LL or EHL that included bile duct stone clearance as an outcome; (2) Prospective studies published in a peer-reviewed journal; (3) Publication in the English language; (4) Availability of the full text; and (5) Publication date by September 20th, 2022. Studies were excluded for the following criteria: (1) Non-original studies including reviews, editorials, commentaries, and study protocols; (2) Insufficient data; (3) Duplicate studies (i.e., conference abstract and full-text manuscript); (4) Non-human studies.
All generations of the POC device, including the mother-daughter system and subsequent generations of the SOC device were included. Studies comparing POC procedures with other stone clearance techniques were included only if outcomes specific to POC-guided lithotripsy were delineated. The same was done with studies describing both biliary and pancreatic stones, which were excluded if individual biliary outcomes werenot reported.
Complete ductal stone clearance was defined as the removal of all stones from the bile ducts. Adverse events were identified in accordance with criteria previously determined by the American Society for Gastrointestinal Endoscopy [Citation16].
Study selection
All articles returned from the formal search strategy were imported into Covidence, a web-based software, which is designed to aid in systematic review management and recommended by Cochrane [Citation17]. Title and abstract reviews were completed by two investigators (AA and WH) independently. In addition, two investigators (AA and WH) independently retrieved the full texts of potentially eligible articles and assessed the articles for inclusion. Discrepancies were resolved by consensus and if no resolution was achieved, a third investigator (SH) adjudicated.
Statistical analysis
Continuous variables were presented as medians with inter-quartile range (IQR) and compared with the Kruskal–Wallis or Wilcoxon rank–sum test, as appropriate. Categorical variables were reported as frequencies and percentages and compared using the chi-square test, or Fisher exact test. Logistic regressions were performed to examine the association of EHL and LL with the achievement of bile duct stone clearance and occurrence of adverse events from extracted data, and results were reported as Odds ratio (OR) and 95% confidence intervals (CI). Pooled ORs with 95% CI were utilized to estimate the overall effects. Statistical significance was defined as p < .05. All statistical analyses were performed using SPSS version 28.0 (IBM Corporation, Armonk, NY).
Results
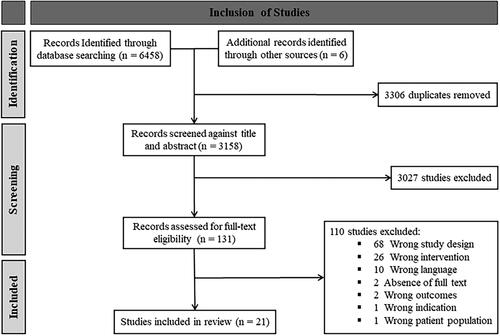
The literature search flow diagram is presented in . The initial PubMed database search yielded a total of 6458 articles and 6 records were identified through other sources. After exclusions from the title and abstract review, the full text of 131 articles was reviewed. From those, a final selection of 21 studies was included, reporting a total of 718 patients undergoing POC-guided EHL or LL for bile duct stones (). In the majority of these studies, conventional ERCP techniques failed to achieve stone clearance due to the size and/or position of stones.
Table 1. Description of studies utilizing per-oral cholangioscopy-guided lithotripsy.
Electrohydraulic lithotripsy
A total of 6 (29%) studies analyzed the use of EHL through POC using a mother-daughter system. In one of the earliest studies, Leung et al. achieved 100% stone clearance by performing peroral EHL in patients with very large stones (mean diameter of 3.1 cm) [Citation18]. Adamek et al. in two different studies, compared the use of EHL with extracorporeal shock-wave lithotripsy (ESWL) and found no significative difference in stone clearance rates between the two therapies (76.5% EHL vs 72.0% ESWL, p > .5 and 74.0% EHL vs 78.5% ESWL, p > .1, respectively) [Citation19,Citation20]. To address the uncertainty of repeating endoscopic procedures on high-risk patients, Hui et al. compared EHL with long-term biliary stenting (7 Fr double pigtail stent left indefinitely) for the treatment of refractory choledocholithiasis [Citation21]. The authors demonstrated that the EHL group had a high success rate (76.5%) and a low rate of post-ERCP pancreatitis (7.7%), even among elderly patients. However, during a median follow-up period of 21.9 months (IQR: 5.9–32.5), a major difference was seen in the rate of recurrent acute cholangitis (63.2% stenting vs. 7.7% EHL, p = .002), for which the practice of long-term biliary stenting is no longer commonly performed.
Laser lithotripsy
In early studies, Cotton et al. and Ponchon et al. found that fluoroscopy-directed LL was less effective than POC-guided LL due to several technical problems, most notably the difficulty in precisely positioning the laser fiber [Citation6,Citation22]. The fluoroscopic approach was also associated with a higher risk of bile duct damage. Notably, an early study highlighted the importance of saline irrigation through the choledochoscope working channel to enhance visibility and improve stone fragmentation [Citation7].
A total of four studies compared POC-guided LL with percutaneously performed LL, finding high stone clearance success rates (80–100% percutaneous, 36%–84.6% POC) with the percutaneous approach, although this approach was found to be more time-consuming [Citation6–8,Citation22].
Neuhaus et al. also compared POC-guided LL with ESWL, finding that LL achieved complete stone clearance more frequently than ESWL (97% LL vs. 73% ESWL, p < .05) [Citation10]. Kim et al. evaluated LL using an ultra-slim endoscope, which provides similar visualization to that of a gastroscope with better water irrigation and suction than a choledochoscope [Citation23]. The authors found a high success rate of 84.6% (11/13 patients) despite the considerable instability of the endoscope’s position during lithotripsy.
Tissue stone detection system
To help avoid bile duct damage incurred by lithotripsy, a laser lithotripter with automatic stone recognition was developed with the ability to interrupt laser pulses in case of tissue contact [Citation10]. Three prospective studies utilized this system, finding no meaningful increase in stone clearance (80–97%) compared to other types of lasers [Citation9–11]. With the development of more modern cholangioscopes, this detection system is no longer utilized.
Single-operator cholangioscopy (SOC)
From 2011 onwards, all of the articles selected reported using a single-operator cholangioscope. High overall stone clearance rates (91–100%) have been found with the use of SOC with one study finding an 83.3% complete stone clearance rate on index attempt of lithotripsy [Citation24–26].
Several randomized controlled trials (RCTs) have compared SOC-guided LL with different endoscopic treatment modalities. Buxbaum et al. compared LL with conventional therapy (mechanical lithotripsy or papillary balloon dilation), showing that LL achieved a 92.9% (39/42 patients) success rate in complete stone clearance compared to 67% (12/18 patients) of those treated with conventional therapy only [Citation27]. Angsuwatcharakon et al. compared LL with mechanical lithotripsy finding that LL had a significantly higher stone clearance rate (100% LL vs. 63% mechanical lithotripsy) and all patients who underwent LL had complete stone clearance in a single session [Citation28]. In a comparison of SOC-guided LL with large balloon sphincteroplasty, Bang et al. also found a higher treatment success rate for those undergoing LL (93.9% vs 72.7%) [Citation29]. Lastly, a recent RCT from Li et al. compared LL with laparoscopic common bile duct exploration [Citation30]. Although the first-session stone removal rate with LL was significantly lower than surgical exploration (83.3% LL vs. 96.2% laparoscopic), LL was not inferior to laparoscopic common bile duct exploration in terms of complete stone clearance rates (92.3% LL vs. 96.2% laparoscopic) and was associated with a shorter hospital stay (5.65 ± 0.94 d LL vs. 8.84 ± 1.54 d laparoscopic).
Two non-randomized prospective studies have compared LL with EHL for refractory stones [Citation31,Citation32]. In both studies, higher rates of stone clearance were identified with LL. Canena et al. found a 100% success rate, all during the first session, for LL vs. a 75% success rate for EHL. In the case of failure with EHL, cross-over to LL resulted in complete ductal clearance with two additional sessions [Citation31]. Maydeo et al. reported a complete stone clearance rate in the first procedure of 82% with LL compared to 74% with EHL, with an 87.2% overall success rate that did not distinguish between LL and EHL [Citation32].
Adverse events
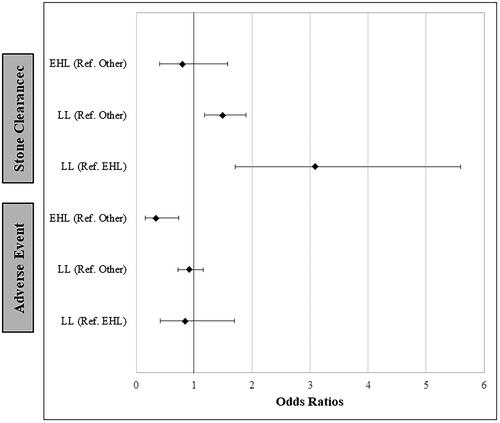
Comparing the adverse event rates for EHL and LL between the selected studies, we found a 12.9% adverse event rate (11/85 patients) for EHL and an 11.2% adverse event rate (53/471 patients) for LL with no difference between the two modalities (OR: 0.85, 95% CI: 0.42–1.70, , Supplementary Table 1). Post-ERCP pancreatitis and post-sphincterotomy bleeding accounted for the majority of reported adverse events, which are challenging to directly attribute to POC-guided lithotripsy within the context of performing an ERCP.
Stone clearance
Overall, an 88% rate (n = 639) of complete ductal stone clearance was found with these intraductal lithotripsy modalities. The stone clearance success rate of LL was 90.9% while EHL had a stone clearance success rate of 76.5% (OR: 3.09, 95% CI: 1.71–5.59, , Supplementary Table 1). The exact number of patients with complete ductal clearance was unable to be determined in 2 studies [Citation6,Citation32].
Discussion
ERCP remains the primary therapeutic modality in managing choledocholithiasis [Citation1,Citation33]. Ten to fifteen % of patients, however, have stones unamenable to conventional ERCP techniques and require alternative and/or additional therapies [Citation34]. These ‘difficult’ bile duct stones encompass a wide variety of cases including large (> 1 cm), multiple or peculiarly-shaped stones (e.g., barrel-shaped), stones located above a stricture or impacted, intrahepatic stones, altered distal bile duct anatomy (oblique, narrowed, sigmoid-shaped), periampullary diverticula, and surgically altered anatomy, among others [Citation35,Citation36]. Alternative advanced techniques typically include mechanical lithotripsy, which is widely available and effective, with success rates ranging between 76% and 91% [Citation2,Citation3,Citation37]. With a first-case success rate of only 50–70%, however, mainly related to stone impaction, stone size > 30 mm, and stone size/bile duct diameter ratio >1.0, a significant proportion of patients require additional procedures [Citation38,Citation39]. Additionally, potential entrapment of the basket within the bile duct can deter endoscopists from attempting the removal of very large stones with this technique [Citation40]. Endoscopic papillary large balloon dilation (EPLBD) represents another commonly utilized advanced technique with dilation typically performed for a duration between 30 and 60 s from the disappearance of the balloon waist [Citation33,Citation41]. Compared to sphincterotomy alone, EPLBD with a limited sphincterotomy reduces the need for mechanical lithotripsy (15% vs. 32%) and is associated with fewer adverse events (11% vs. 18%) [Citation42]. Therefore, European guidelines currently recommend a limited sphincterotomy with EPLBD as the first-line therapeutic approach if large bile duct stones are seen on cholangiography or cross-sectional images [Citation33]. While a set algorithm for the management of these cases does not currently exist, the definition of ‘difficult’ stones has changed in response to technological advances, intraductal lithotripsy being the foremost innovation in this arena.
While the advent of the SOC system has spurred the use of POC-guided intraductal lithotripsy as a primary modality for the treatment of difficult bile duct stones, the lack of prospective studies directly comparing LL and EHL served as the impetus for this systematic review. Prior systematic reviews have included a large number of retrospective studies, which introduce selection bias to their findings [Citation4,Citation34]. Analysis of the 21 prospective studies for this review found a high rate of complete ductal clearance (88%, n = 639) with these intraductal modalities. It is important to note that many more prospective studies (LL:17, EHL:6) have been performed for LL despite the easier accessibility to EHL. In comparing LL with EHL, the overall stone clearance success rate was higher among patients undergoing LL in comparison to EHL [OR: 3.09, 95% CI: 1.71–5.59). The high stone clearance rates seen in the recent randomized studies [Citation27–30] utilizing LL with the SOC systems appear to corroborate these findings and a previous meta-analysis reported similar data with Veld et al. finding that LL had a higher complete stone clearance rate (95.1%) compared with EHL (88.4%) [Citation4]. Similarly, McCarty et al. showed a significantly higher single-session success rate for LL compared to EHL (82.97% vs. 70.85%) [Citation34]. In contrast, a large, international, retrospective multicenter study including patients treated with SOC-guided lithotripsy for difficult biliary stones reported similar overall success rates for EHL and LL (96.7% vs. 99%, respectively), although a non-significant trend in favor of LL was noted for single session clearance rates (74.5% EHL vs. 86.1% LL) [Citation43].
Several limitations of this study warrant further discussion as the choice between EHL and LL remains a debatable topic. In addition to the lack of a randomized trial directly comparing the two methods, data regarding the cost-effectiveness of either therapy are lacking. Additionally, the lack of randomized studies examining SOC-guided EHL limits our understanding of the efficacy of EHL, especially considering the paucity of studies examining SOC-guided EHL. Another major limitation of the literature centers around the ambiguity in the settings utilized for both EHL and LL. Regarding EHL, settings can be adjusted for power and frequency, while in LL, energy and frequency are adjustable. The number of shocks administered during EHL is infrequently reported, as is the number of EHL probes utilized during a treatment session. For LL, there is significant heterogeneity in the types of laser being utilized, although recent randomized studies have largely utilized holmium:yttrium aluminum garnet (YAG). Similar to EHL, the total power utilized is under-reported in LL studies and studies have not compared the different fiber diameters (ranging from 365 µm to 1000 µm) in stone clearance. In line with this, an investigation is needed to determine ideal settings for effective stone fragmentation within an acceptable safety profile for both EHL and LL. Importantly, we utilized bile duct stone clearance as our primary outcome, which while widely reported is limited in determining the clinical impact of these lithotripsy modalities and does take into account patient-centered outcomes such as pain. Lastly, studies are also needed to determine the learning curve of performing cholangioscopy-directed lithotripsy as the majority of studies reflect the experience of expert endoscopists.
This systematic review represents one of the few attempts to report on the success of POC-guided LL and EHL for the treatment of choledocholithiasis. As prior reviews did not distinguish between biliary and pancreatic stone treatment and included alternative fluoroscopic or percutaneous approaches, as well as retrospective studies, this review provides a comprehensive overview of the two intraductal lithotripsy modalities with an emphasis on prospective studies [Citation4,Citation34,Citation44].
In conclusion, the results of this systematic review suggest that POC-guided LL is a highly effective form of lithotripsy for the treatment of choledocholithiasis, even when compared to EHL. The advent of SOC, in particular, has enabled higher rates of bile duct clearance with low adverse events. Further prospective studies and randomized control trials are needed, however, to define the most successful and cost-effective form of lithotripsy for the treatment of refractory bile duct stones. Additionally, on a practical level, the field will benefit from studies focusing on identifying optimal settings for both EHL and LL in bile duct stone fragmentation.
Supplemental Material
Download PDF (66.1 KB)Acknowledgements
Author S.H. was supported by the Path to K award from the Ohio State University College of Medicine Office of Research and the Center for Clinical and Translational Science through the Richard P. & Marie R. Bremer Medical Research Fund and William H. Davis Endowment for Basic Medical Research.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Buxbaum JL, Abbas Fehmi SM, Sultan S, et al. ASGE guideline on the role of endoscopy in the evaluation and management of choledocholithiasis. Gastrointest Endosc. 2019;89(6):1075–1105.e15.
- Chang WH, Chu CH, Wang TE, et al. Outcome of simple use of mechanical lithotripsy of difficult common bile duct stones. World J Gastroenterol. 2005;11(4):593–596.
- Garg PK, Tandon RK, Ahuja V, et al. Predictors of unsuccessful mechanical lithotripsy and endoscopic clearance of large bile duct stones. Gastrointest Endosc. 2004;59(6):601–605.
- Veld JV, van Huijgevoort NCM, Boermeester MA, et al. A systematic review of advanced endoscopy-assisted lithotripsy for retained biliary tract stones: laser, electrohydraulic or extracorporeal shock wave. Endoscopy. 2018;50(9):896–909.
- Shah RJ. Innovations in intraductal endoscopy: cholangioscopy and pancreatoscopy. Gastrointest Endosc Clin N Am. 2015;25(4):779–792.
- Cotton PB, Kozarek RA, Schapiro RH, et al. Endoscopic laser lithotripsy of large bile duct stones. Gastroenterology. 1990;99(4):1128–1133.
- Neuhaus H, Hoffmann W, Zillinger C, et al. Laser lithotripsy of difficult bile duct stones under direct visual control. Gut. 1993;34(3):415–421.
- Prat F, Fritsch J, Choury AD, et al. Laser lithotripsy of difficult biliary stones. Gastrointest Endosc. 1994;40(3):290–295.
- Jakobs R, Maier M, Kohler B, et al. Peroral laser lithotripsy of difficult intrahepatic and extrahepatic bile duct stones: laser effectiveness using an automatic stone-tissue discrimination system. Am J Gastroenterol. 1996;91(3):468–473.
- Neuhaus H, Zillinger C, Born P, et al. Randomized study of intracorporeal laser lithotripsy versus extracorporeal shock-wave lithotripsy for difficult bile duct stones. Gastrointest Endosc. 1998;47(5):327–334.
- Panpimanmas S, Chantawibul S, Ratanachu-Ek T. Pulse dye laser lithotripsy for large biliary tract stones. J Med Assoc Thai. 2000;83:433–438.
- Watson RR, Parsi MA, Aslanian HR, et al. Biliary and pancreatic lithotripsy devices. VideoGIE. 2018;3(11):329–338.
- Trikudanathan G, Navaneethan U, Parsi MA. Endoscopic management of difficult common bile duct stones. World J Gastroenterol. 2013;19(2):165–173.
- Larizgoitia I, Pons JM. A systematic review of the clinical efficacy and effectiveness of the holmium: YAG laser in urology. BJU Int. 1999;84(1):1–9.
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
- Chandrasekhara V, Khashab MA, Muthusamy VR, et al. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85(1):32–47.
- Kellermeyer L, Harnke B, Knight S. Covidence and rayyan. jmla. 2018;106(4):580–583.
- Leung JW, Chung SS. Electrohydraulic lithotripsy with peroral choledochoscopy. BMJ. 1989;299(6699):595–598.
- Adamek HE, Buttmann A, Wessbecher R, et al. Clinical comparison of extracorporeal piezoelectric lithotripsy (EPL) and intracorporeal electrohydraulic lithotripsy (EHL) in difficult bile duct stones. A prospective randomized trial. Dig Dis Sci. 1995;40(6):1185–1192.
- Adamek HE, Maier M, Jakobs R, et al. Management of retained bile duct stones: a prospective open trial comparing extracorporeal and intracorporeal lithotripsy. Gastrointest Endosc. 1996;44(1):40–47.
- Hui CK, Lai KC, Ng M, et al. Retained common bile duct stones: a comparison between biliary stenting and complete clearance of stones by electrohydraulic lithotripsy. Aliment Pharmacol Ther. 2003;17(2):289–296.
- Ponchon T, Gagnon P, Valette PJ, et al. Pulsed dye laser lithotripsy of bile duct stones. Gastroenterology. 1991;100(6):1730–1736.
- Kim HI, Moon JH, Choi HJ, et al. Holmium laser lithotripsy under direct peroral cholangioscopy by using an ultra-slim upper endoscope for patients with retained bile duct stones (with video). Gastrointest Endosc. 2011;74(5):1127–1132.
- Goenka MK, Shah BB, Rodge GA, et al. Efficacy and safety of cholangioscopy guided laser lithotripsy for difficult bile duct stones – A prospective study from a tertiary care centre in Eastern India. Arab J Gastroenterol. 2021;22(2):111–114.
- Maydeo A, Kwek BE, Bhandari S, et al. Single-operator cholangioscopy-guided laser lithotripsy in patients with difficult biliary and pancreatic ductal stones (with videos). Gastrointest Endosc. 2011;74(6):1308–1314.
- Wong JC, Tang RS, Teoh AY, et al. Efficacy and safety of novel digital single-operator peroral cholangioscopy-guided laser lithotripsy for complicated biliary stones. Endosc Int Open. 2017;5(1):E54–e58.
- Buxbaum J, Sahakian A, Ko C, et al. Randomized trial of cholangioscopy-guided laser lithotripsy versus conventional therapy for large bile duct stones (with videos). Gastrointest Endosc. 2018;87(4):1050–1060.
- Angsuwatcharakon P, Kulpatcharapong S, Ridtitid W, et al. Digital cholangioscopy-guided laser versus mechanical lithotripsy for large bile duct stone removal after failed papillary large-balloon dilation: a randomized study. Endoscopy. 2019;51(11):1066–1073.
- Bang JY, Sutton B, Navaneethan U, et al. Efficacy of single-operator cholangioscopy-guided lithotripsy compared with large balloon sphincteroplasty in management of difficult bile duct stones in a randomized trial. Clin Gastroenterol Hepatol. 2020;18(10):2349–2356.e3.
- Li G, Pang Q, Zhai H, et al. SpyGlass-guided laser lithotripsy versus laparoscopic common bile duct exploration for large common bile duct stones: a non-inferiority trial. Surg Endosc. 2021;35(7):3723–3731.
- Canena J, Lopes L, Fernandes J, et al. Outcomes of single-operator cholangioscopy-guided lithotripsy in patients with difficult biliary and pancreatic stones. GE Port J Gastroenterol. 2019;26(2):105–113.
- Maydeo AP, Rerknimitr R, Lau JY, et al. Cholangioscopy-guided lithotripsy for difficult bile duct stone clearance in a single session of ERCP: results from a large multinational registry demonstrate high success rates. Endoscopy. 2019;51(10):922–929.
- Manes G, Paspatis G, Aabakken L, et al. Endoscopic management of common bile duct stones: european society of gastrointestinal endoscopy (ESGE) guideline. Endoscopy. 2019;51(5):472–491.
- McCarty TR, Gulati R, Rustagi T. Efficacy and safety of peroral cholangioscopy with intraductal lithotripsy for difficult biliary stones: a systematic review and meta-analysis. Endoscopy. 2021;53(2):110–122.
- Yasuda I, Itoi T. Recent advances in endoscopic management of difficult bile duct stones. Dig Endosc. 2013;25(4):376–385.
- Anderloni A. Difficult common bile duct stones: still “difficult” or just… “different”. Endoscopy. 2020;52(6):429–430.
- Shaw MJ, Mackie RD, Moore JP, et al. Results of a multicenter trial using a mechanical lithotripter for the treatment of large bile duct stones. Am J Gastroenterol. 1993;88(5):730–733.
- Cipolletta L, Costamagna G, Bianco MA, et al. Endoscopic mechanical lithotripsy of difficult common bile duct stones. Br J Surg. 1997;84(10):1407–1409.
- Lee SH, Park JK, Yoon WJ, et al. How to predict the outcome of endoscopic mechanical lithotripsy in patients with difficult bile duct stones? Scand J Gastroenterol. 2007;42(8):1006–1010.
- Troncone E, Mossa M, De Vico P, et al. Difficult biliary stones: a comprehensive review of new and old lithotripsy techniques. Medicina. 2022;58(1):120.
- Kim TH, Kim JH, Seo DW, et al. International consensus guidelines for endoscopic papillary large-balloon dilation. Gastrointest Endosc. 2016;83(1):37–47.
- Madhoun MF, Wani S, Hong S, et al. Endoscopic papillary large balloon dilation reduces the need for mechanical lithotripsy in patients with large bile duct stones: a systematic review and meta-analysis. Diagn Ther Endosc. 2014;2014:309618.
- Brewer Gutierrez OI, Bekkali NLH, Raijman I, et al. Efficacy and safety of digital single-operator cholangioscopy for difficult biliary stones. Clin Gastroenterol Hepatol. 2018;16(6):918–926.e1.
- Korrapati P, Ciolino J, Wani S, et al. The efficacy of peroral cholangioscopy for difficult bile duct stones and indeterminate strictures: a systematic review and meta-analysis. Endosc Int Open. 2016;4(3):E263–E275.