Abstract
Objective
To investigate cognitive function in patients with irritable bowel syndrome (IBS) and its relation to anxiety/depression and severity of gastrointestinal (GI) symptoms.
Methods
Patients with IBS (n = 65) and healthy controls (HCs, n = 37) performed the ten subtests of the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS). Age-normed index scores of five cognitive domains (Immediate memory, Visuospatial function, Language function, Attention, Recall) and a total (Fullscale) score were derived from the performance. Emotional function was assessed using the Hospital Anxiety and Depression Scale (HADS), and the IBS Symptom Scoring System (IBS-SSS) was used to define the severity of GI symptoms.
Results
Patients with IBS reported significantly higher scores than the HC group on symptom measures of anxiety and depression, and significantly lower scores on the Immediate memory, Recall, and Fullscale RBANS indexes. Approximately 30% of the IBS patients obtained index scores at least one standard deviation below the population mean, and more than 50% scored above the screening threshold for an anxiety disorder. The severity of GI symptoms was significantly correlated with the severity level of anxiety symptoms (p=.006), but neither the severity level of emotional nor GI symptoms was significantly correlated with the RBANS index scores in the IBS group.
Conclusion
Cognitive and emotional function were more severely affected in patients with IBS than in HCs. The weak correlation between the two functional areas suggests that both should be assessed as part of a clinical examination of patients with IBS.
PRACTITIONERS’ POINTS
Cognitive and emotional function should be assessed in patients with IBS.
Cognitive impairment was less closely related to symptoms of anxiety/depression and severity of GI symptoms than expected.
An independent contribution of both emotional symptoms and cognitive function should be considered when developing treatment programs for patients with IBS.
Introduction
Irritable Bowel Syndrome (IBS) is a prevalent disorder, reported to affect one in ten people globally [Citation1]. The disorder is characterized by a high frequency of recurrent abdominal pain and changes in bowel habits over time in the absence of a known detectable organic cause [Citation2]. Historically, symptoms outside the gastrointestinal (GI) system have been described as secondary or comorbid to gastrointestinal (GI) symptoms, and the diagnosis is still primarily based on the gut-restricted Rome-IV criteria [Citation3]. However, there has been a growing awareness within the field to broaden the definition of clinical symptoms associated with IBS. This shift suggests that emotional problems should be considered when assessing and selecting treatment approaches for patients with IBS [Citation4]. Indeed, 30 – 40% of IBS patients fulfill the diagnostic criteria of anxiety and/or depression, respectively [Citation5,Citation6]. Some of these patients are shown to respond better to psychological treatment than to interventions aimed directly at alleviating the GI symptoms [Citation7]. A recent study further supported a close co-existence between emotional and GI symptoms by showing that anxiety and IBS share a genetic vulnerability that affects both the enteric and central nervous system, causing gut-brain disturbances in IBS [Citation8].
Several studies have confirmed the importance of the rich communication between the gut and the brain in patients with IBS [Citation9–12] and other diseases defined as disorders of the gut-brain interaction (DGBI). In a bidirectional pathway between the gut and the brain, the gut microbiota and its interaction with the enteric nervous system, the enteroendocrine system, and the gut-associated immune system are suggested to affect brain structure [Citation13,Citation14] and function [Citation12,Citation15], and vice versa. This so-called gut-brain axis has fueled an interest in investigating cognitive impairment in patients with IBS and other DGBIs [Citation4,Citation16]. Assumptions about cognitive impairment in patients with IBS are indicated by studies including brain imaging data and measures of gut microbiota. Brain imaging studies comparing IBS patients with healthy controls have shown smaller volumes in brain regions associated with stress [Citation17], visceral stimulation [Citation18], sensory integration [Citation19,Citation20], affective processing [Citation21], somatic pain [Citation11] as well as cognitive/executive functions [Citation22]. Other studies have shown that alterations in gut microbiota affect cognitive performance in both human and animal models [Citation23–25]. Further, so-called “brain fog”, characterized by forgetfulness, confusion, a lack of concentration and mental clarity, is a prevalent state reported by IBS patients, a state that has been linked to disturbances in the gut microbiota [Citation26]. Thus, when it comes to ameliorating the assessment and treatment of patients with IBS, our understanding of cognitive features related to the gut-brain axis should be of key importance [Citation27,Citation28].
However, results from previous studies on cognitive function in patients with IBS are far from conclusive. In a systematic review based on 12 studies, Lam et al. (2019) reported that an attentional bias toward words with emotionally negative content was the most consistent finding in IBS patients [Citation4]. The results gave no clear evidence for the effect on memory and executive function and pointed to several methodological limitations that prevented the authors from presenting firm conclusions. First, the clinical heterogeneity between the studies was large, and results have been presented without considering co-existing factors like anxiety, depression, and the severity of IBS. Second, the selection of neuropsychological tools has been arbitrary and narrow. Therefore, the authors called for future studies including measures covering a wide range of cognitive domains and covariates. The results from Wong et al. (2019) partly followed these recommendations. They presented results showing impairment on psychometric tests of attention (a continuous performance test) and executive function (a card sorting test) in a group of patients with IBS (N = 40) [Citation16], and showed that their performances were impaired and closely related to comorbid anxiety. A close relation between self-reported symptoms of anxiety and self-reported executive function in IBS patients was supported in a recent study [Citation29], and impaired cognitive test performance in patients with anxiety [Citation30–32] and depression [Citation30,Citation33,Citation34] has been shown in several previous studies. The relation between self-reported symptoms of depression and anxiety and performance on psychometrically sound neuropsychological tests covering a wide range of cognitive domains has, as far as we know, not been studied in patients with IBS. Knowing the implication of aberrations in neural circuitries, systemic stress response, immune activation, and gut microbiota composition on patients with IBS, it is plausible to assume that the malfunction in these biological systems also affects performance on neuropsychological tests of cognition.
The results outlined above should show that more studies are essential to draw firm conclusions about cognitive function and its relation to anxiety and depression in patients with IBS. This motivated the present study to ask participants in the Norwegian multidisciplinary Bergen Brain-Gut project to perform the subtests included in the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS) [Citation35] and to complete a questionnaire with items assessing symptoms of anxiety and depression. Based on prior findings we expected to find more severe symptoms of anxiety and depression and lower performance on cognitive tests in patients with IBS than in HCs, and that cognitive and emotional function would be closely related [Citation16]. Finally, we included a measure of the severity of GI symptoms to investigate its effect on the included cognitive and emotional measures. By this, we responded to the call for studies including measures of a broad range of cognitive domains and essential covariates.
Materials and methods
Participants
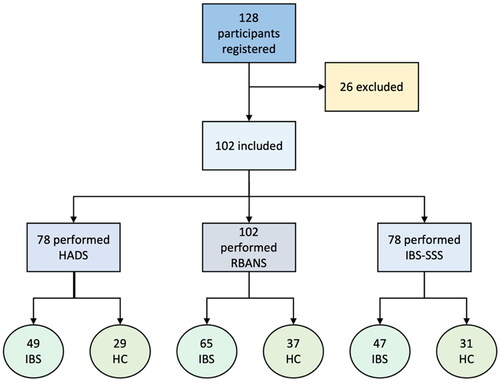
The present study is part of the Norwegian Brain-Gut project, conducted at Haukeland University Hospital, Bergen, Norway [Citation36]. The aim of this project was to obtain a better understanding of the etiology of IBS by running a multidisciplinary study including psychometric tests and a wide range of questionnaires to assess symptom severity of GI- and coexistent symptoms [Citation36]. A group of patients with IBS and healthy controls (HCs) (total n = 128) were included. Approximately half of the IBS patients were recruited through the outpatient clinic at the hospital and the other half through media and flyers. All HCs were recruited through media and flyers. All participants were asked to read the more detailed information provided on the project’s website (www.braingut.no). Thereafter, all participants were interviewed by a study nurse (phone call). The patients were screened according to the list of inclusion and exclusion criteria () and offered additional clinical examinations (ultrasonography, sigmoidoscopy, gastroscopy, and blood tests). The HCs were above 18 years old and were screened by a study nurse according to the same exclusion criteria as the patients. For more information on the study design, see Berentsen et al. 2020 [36].
Table 1. Exclusion and inclusion criteria for patients with IBS.
Measures
Repeatable Battery for the Assessment of Neuropsychological Status (RBANS)
The participants completed the Norwegian version of RBANS [Citation35]. From the ten tests included in RBANS, five age-corrected index scores are calculated to measure Immediate memory, Visuospatial abilities, Verbal skills, Attention, and Recall, and a total (Fullscale) index score is calculated from performance on all ten tests (). The index scores are adjusted according to Scandinavian norms, with 100 as the mean value and 15 as one standard deviation (SD), where higher scores equal higher performances. The A-version of the test was presented to all participants according to the standardized instructions presented in the manual. The test takes about 20-30 min to complete.
Figure 1. The five cognitive domains, each with two subtests, and the total Fullscale score calculated from performance on the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS). Inspired by a figure presented by Randolph et al. [Citation35].
![Figure 1. The five cognitive domains, each with two subtests, and the total Fullscale score calculated from performance on the Repeatable Battery for the Assessment of Neuropsychological Status (RBANS). Inspired by a figure presented by Randolph et al. [Citation35].](/cms/asset/c62096a6-07f0-4640-89ed-86ca6fd9f374/igas_a_2256916_f0001_c.jpg)
The Hospital Anxiety and Depression Scale (HADS)
The participants were asked to complete the HADS, a self-assessment scale used to assess severity of symptoms used to define anxiety and depression, calculated as the sum across 14 questions related to mood disorders, with a max total score of 42 [Citation37]. The questions are related to emotions and behaviors experienced during the previous week. The 14 questions are divided into two subscales, one for anxiety (HADS-A) and one for depression (HADS-D), with 7 questions included in each. Each subscale provides a maximum score of 21. According to the results on each of the two subscales, the participants were categorized as either a non-case (<8), a doubtful case (8-11), or a case (>11). The HADS questionnaire was completed on an online platform within the same week as the participants performed the RBANS.
IBS-Severity Scoring System (IBS-SSS)
IBS-SSS [Citation38] was included to determine the severity level of GI symptoms associated with IBS. The questionnaire consists of 5 items related to IBS symptoms, with measures of frequency and intensity of abdominal pain, the severity of abdominal distension, dissatisfaction with bowel habits, and the interference of IBS with daily life, each with a maximum score of 100 points. The severity level of an IBS case is defined according to the IBS-SSS score as normal (0 – 74), mild (75-175), moderate (175-300) and severe (>300) and is shown to be valid and sensitive to change. Most participants answered the questions on an online platform, except for the first six, who completed a paper version. The inclusion criteria for IBS patients in the Bergen Brain-Gut project was an IBS-SSS score ≥175 (). In the control group, the IBS-SSS scores were primarily in the normal range, with only a few HCs reporting a score within the lower range of the mild IBS-SSS category. The two groups were by this clearly separated by their IBS-SSS score.
Statistical analysis
Jamovi, version 2.3.21.0 was used to conduct the statistical analyses. An independent samples t-test was used to compare the results in the two groups, with the assumption that the IBS-group would perform at a lower level on the RBANS tests and that they would report higher scores on the included questionnaires (HADS and IBS-SSS) compared to the HC group. The significance level was set to p = .05, and Cohen’s d was defined as small when d ≤ 0.2, moderate when d = 0.5 and high when d ≥ 0.8 [Citation39]. A correlation analysis was computed to investigate relations between the RBANS indexes and the self-reported symptoms on the HADS and the IBS-SSS scales.
Results
Demographics
Of the 128 participants included in the Bergen Brain-Gut project, 102 participants performed all RBANS subtests, 65 with an IBS diagnosis (see for more details). Of the 102 participants, 26 were males and 76 were females. The overall mean age 38 was (SD = 11.49) in the IBS group and 35 (SD = 12.3) in the HC group. The group differences in gender and age were statistically non-significant (p >.05). In total, 128 participants were registered at the beginning of the study, and 26 participants were excluded from the study during the interview with the study nurse. The remaining 102 participants performed the RBANS tests, while 78 of the 102 also completed the items of the HADS and IBS-SSS questionnaires. Among the 61 patients with IBS who completed the IBS-SSS, 22 were defined as IBS with predominant diarrhea (IBS-D), 8 with predominant constipation (IBS-C), and 31 with a mix of the two (IBS-M).
Cognitive function
The IBS group obtained a significantly lower score on the Fullscale index than the HC group (see ). When the results within the five domains were analyzed separately, significant results with moderate effect sizes were shown for the two memory indexes (Immediate memory and Recall). A more detailed analysis defined impairment as a score of at least one standard deviation below the age-corrected normative mean on each of the indexes. shows that the percentage of participants with such a low score was almost 40% for the Immediate memory index in the IBS group, with higher percentages in the IBS relative to the HC group also on the Attention and Recall indexes. The Gaussian distribution of RBANS scores gives an expected percentage of ∼ 16% falling one standard deviation (SD) below the population mean on each subscale. Almost all HCs obtained a score above this cut-off score on the Fullscale index, while the percentage below this score was much higher for the IBS than the HC group (33.8 versus 16.2%). Among the patients with such a low Fullscale RBANS score, we found that 77% had IBS-M. Further, the mean IBS-SSS score in this group was as high as 280 (SD = 81).
Figure 3. Percentage of IBS patients and HCs with scores equal to or below 85 on the RBANS indexes. According to a Gaussian distribution, 15.8% of the participants are expected to obtain such a score on each bar, illustrated by the dotted line.
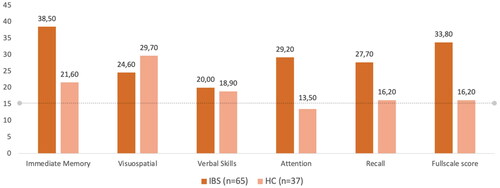
Table 2. Results on the RBANS indexes and self-reported symptom scores on the HADS and the IBS-SSS scale.
Emotional function
The HADS questionnaire was completed by 78 participants, 49 patients with IBS and 29 HCs. The IBS group reported significantly higher scores, with large effect sizes, on the HADS compared to the HC group (see ). Within the IBS group, 10 patients were defined as doubtful cases of anxiety and 5 with depression, while 16 and 2 patients were defined as severe cases of anxiety and depression, respectively. All cases with depression were also defined as doubtful (n = 2) or severe cases (n = 5) of anxiety. Within the group of 16 patients defined as severe cases of anxiety, the mean IBS-SSS score was 306 (SD = 77). When the doubtful cases were included, the mean IBS-SSS score was 296 (SD = 69). In the doubtful/severe anxiety group, 59% were defined as IBS-M. No cases of anxiety and depression were identified in the control group.
IBS severity and its relation to emotional and cognitive function
In order to assess severity of GI symptoms, the IBS-SSS questionnaire was completed by 78 participants, 47 patients with IBS and 31 HCs. shows that the IBS-SSS score was, as expected, much higher in the IBS than in the HC group (d = 4.15), with a mean score = 35.1 and a maximum score = 108. Within the IBS group, the IBS-SSS score correlated at a statistically significant level with the HADS Anxiety score (r = .38, p = .004) and at a somewhat weaker level with the total HADS score (r = .31, p = .021). The IBS-SSS score did not correlate significantly with any of the RBANS index scores (see ).
Figure 4. Scatter- and density-plots showing the associations between IBS-SSS score and the emotional and cognitive test scores for each group (green: IBS group, orange: HC). within the IBS group, only the correlations between IBS-SSS and HADS Anxiety (r =.38, p =.004), and IBS-SSS and HADS Total Score (r =.31, p =.021) were statistically significant. Abbreviations: HADS: the Hospital Anxiety and Depression Scale, RBANS: Repeatable Battery for the Assessment of Neuropsychological Status, IBS-SSS: IBS-Severity Scoring System.
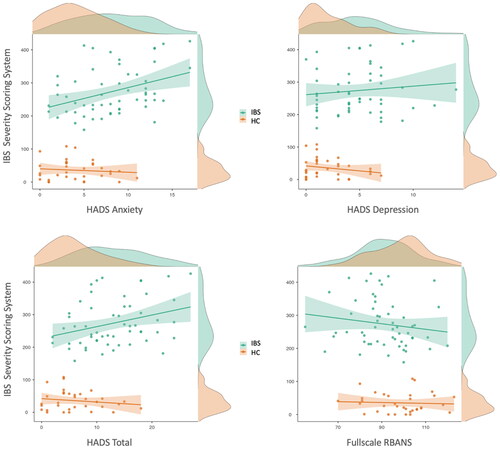
When both groups were included in a correlation analysis, the results showed statistically significant correlations between the IBS-SSS score and the Fullscale (r = .31, p = .003), the Immediate memory (r = .26, p = .013) and the Recall (r = .23, p = .026) RBANS indexes. A stronger correlation was found between the IBS-SSS and the total HADS score (r = .55, p <.001), at a similar level both for the HADS Anxiety (r = .54, p <.001) and the HADS Depression subscales (r = .42, p <.001).
Correlations between emotional and cognitive function
Within the IBS group, neither the Fullscale RBANS score nor any of the domain specific RBANS indexes correlated significantly with any of the HADS scores. The correlations were somewhat stronger for the HADS Depression score in the HC group for the Immediate memory (r = .35, p =.044) and the Visuospatial indexes (r = .37, p = .036). The distributions of results within the two groups are illustrated by the regression lines in .
Figure 5. Scatter- and density-plots showing the correlations between the Fullscale RBANS index and the HADS Anxiety score and the Fullscale RBANS index and the HADS Depression score. The blue dots show the scores of the IBS patients and the yellow dots show the score of the HCs. The correlations are statistically significant (p <.05) when both groups were included in the analysis, but not when the IBS and the HC group were analyzed separately.
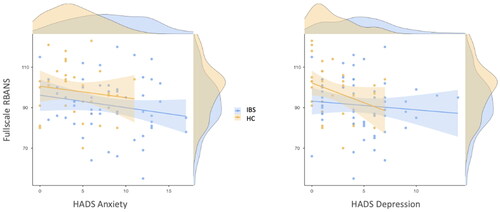
The correlations were also weak, but at a level of significance <.05 between the RBANS and HADS scores when all participants (IBS and HCs) were included in the analyses. This was found both between the Fullscale RBANS index and the HADS Anxiety (r = .26, p = .012), the HADS Depression (r = .24, p = .021), and the Total HADS score (r = .28, p = .007), between the Immediate memory index and the HADS Anxiety (r = .23, p = .031) and the HADS Total score (r = .21, p = .045), and between the Recall index and the HADS Anxiety (r = 0.22, p = .039), HADS Depression (r = 0.24, p = .024) and the HADS Total score (r = .25, p = .018).
Discussion
The current study showed that the group of patients with IBS obtained lower performances than the HC group on a battery of psychometric tests assessing core cognitive domains. A large percentage of the IBS patients were categorized as impaired, meaning their performance was one standard deviation below the population mean on the total RBANS Fullscale index. The IBS patients also reported higher scores on a questionnaire assessing symptoms of anxiety and depression, with 45% being defined as severe or doubtful cases. Notably, correlations between the cognitive and emotional measures were unexpectedly low within the IBS group. Associations with the severity of GI symptoms, as assessed by the IBS-SSS, were strong for the emotional, but weak for the cognitive measures.
The high incidence of anxiety in the IBS group aligns with results from several previous studies. Presently, the Rome criteria used to diagnose IBS tend to overlook the large number of IBS patients meeting the diagnostic criteria for anxiety and depression, and vice versa. However, detailed patient histories disclose symptoms of abdominal discomfort paired with anxiety and psychological distress, sometimes tracing back to early childhood [Citation14]. A recent genetic epidemiological study provides a compelling rationale for the simultaneous presence of abdominal and psychological distress in IBS patients. The study identified a robust genome-wide correlation between the risk of IBS and anxiety, neuroticism, and depression [Citation8]. These new findings support the idea that genetic predispositions can affect both the central and enteric nervous systems. This challenges the notion that emotional factors may directly cause IBS symptoms or that chronic IBS gut symptoms lead to anxiety and depression. Instead, the findings favor a shared pathophysiology between IBS (or gut microbiota) and psychiatric disorders [Citation6,Citation14].
The main contribution of the present study was to show that IBS patients may show impaired results on a psychometric test battery that evaluates core domains of cognitive function. Weak correlations between emotional and cognitive function were among the most unexpected findings, partly in conflict with results reported by Wong et al. [Citation16] and Lundervold et al. [Citation29]. The results rather suggest a kind of independence between emotional and cognitive function, at least when the latter is assessed by a neuropsychological test battery. In that impairment of each is expected to pose challenges in the everyday life of a patient with IBS, we advocate for the inclusion of both in clinical examinations. The weak correlations between severity of GI symptoms and performance on cognitive tests in the IBS group stand in contrast to the strength of the correlation between GI severity and severity of anxiety symptoms.
The notable high IBS-SSS scores among patients with IBS defined with an impairment on the Fullscale RBANS index should inspire further identification of subgroups of patients with IBS. Furthermore, the results could have been improved by inclusion of participants along the full spectrum of IBS-SSS scores. In the present study, most participants in the HC group reported from zero to symptoms at a very mild severity level, while patients with IBS were all defined with more severe symptom scores. A spectrum view is well supported by studies showing that even otherwise healthy individuals tend to have some degree of gut discomfort. The impact of this discomfort on cognition is shown in studies on pain, where GI symptoms commonly interfere with cognitive functions [Citation40] and influence how pain is coped with [Citation41]. It is also well-established that GI symptoms in otherwise healthy adults are associated with poorer cognitive performance [Citation42]. Further studies designed to cover the full spectrum of IBS-SSS scores are thus called for. Such studies may not only show stronger associations between IBS severity, cognitive and emotional function, but may also provide insights into their interplay. Such information would be crucial to facilitate more personalized treatment of patients with IBS. For dietitians and other healthcare professionals, being aware of possible cognitive limitations and their interactions with emotional and GI-related symptoms in a patient would be vital when introducing new treatment. Although psychological interventions, such as cognitive behavioral therapy (CBT), have been effective in treating patients with IBS [Citation43], one might speculate that the efficacy partly depends on the cognitive function of the participant [Citation44]. This consideration should also apply to other treatment options.
IBS is recognized as a multifaceted and highly heterogeneous disorder. Our results show the broad array of responses and performances in the IBS group on the questionnaire and the cognitive test, respectively. This underlines the importance of comprehensive clinical phenotyping. Subgrouping IBS patients could address the disorder’s inherent heterogeneity, moving beyond a definition primarily anchored in GI symptoms and encompassing cognitive and emotional function.
Strengths and limitations
To the best of our knowledge, this is the first study directly investigating results on a psychometric instrument like RBANS in patients with IBS. With a subgroup of patients performing at a level indicating impairment, there should be strong arguments for assessing cognitive function, at least before deciding on an appropriate treatment for a patient with IBS.
Several limitations should be mentioned. The sample size is an obvious limitation in a study of a disorder where several factors and mixtures thereof are shown to influence symptom reports [Citation45,Citation46]. Future studies are thus indeed needed to further explore the implications of cognitive and emotional problems suggested by the present data from the Bergen Brain-Gut project. It is worth considering the presence of sex bias against males as another limitation, although this likely reflects the overall higher prevalence of females among IBS patients. Another limitation is the absence of data on fatigue, sleep, and other psychological stressors, factors with obvious potentials to influence symptom reports. When it comes to IBS symptoms, the study implemented strict criteria for inclusion and exclusion, resulting in a sample where the IBS-SSS score could effectively differentiate the IBS versus HC group. The conclusions may therefore be restricted to patients with the most severe gastrointestinal symptoms. Lastly, it should be noted that the RBANS norms are estimated from a sample of participants with high levels of education and IQ [Citation47] This means that the RBANS norms will be most accurate when the participants have high levels of education. In our study, the participants on average have 16 years of education, which aligns with the normative data. By including only two tests within each cognitive domain, the RBANS cannot assess more fine-graded characteristics of cognitive function in our patients.
Conclusion
Our study showed that at least a subgroup of patients with IBS exhibits impaired performance on psychometric tests of cognitive function. Interestingly, this performance level was only weakly associated with the symptoms of anxiety and depression that characterize this patient group. Consequently, the findings contribute to underscore the importance of addressing both emotional and cognitive issues when assessing and treating patients with IBS. Future studies should build on these findings by assessing cognitive and emotional function in a larger cohort of patients with IBS, incorporating a broader spectrum of measures linked to the disease, and including statistical methods to identify subgroups and further evaluate the generalizability of the results.
Informed consent statement
Informed consent was obtained from all subjects involved in the study.
| Abbreviations | ||
| RBANS | = | Repeatable Battery for the Assessment of Neuropsychological Status |
| HADS | = | Hospital Anxiety and Depression Scale |
| IBS | = | Irritable Bowel Syndrome |
| IBS-SSS | = | Irritable Bowel Syndrome Severity Scoring System. |
Acknowledgements
We sincerely thank all patients and healthy volunteers for their participation in the Bergen Brain–Gut Microbiota (B-BGM) project. We also thank the research nurses for their help in collecting data.
Disclosure statement
The authors declare no conflicts of interest.
Additional information
Funding
References
- Sperber AD, Bangdiwala SI, Drossman DA, et al. Worldwide prevalence and burden of functional gastrointestinal disorders, results of Rome Foundation Global Study. Gastroenterology. 2021;160(1):99–114.e3.
- Drossman DA, Hasler WL. Rome IV – functional GI disorders: disorders of gut-brain interaction. Gastroenterology. 2016;150(6):1257–1261.
- Black CJ, Ng CE, Goodoory VC, et al. Novel symptom subgroups in individuals with irritable bowel syndrome predict disease impact and burden. Clin Gastroenterol Hepatol. 2023. Epub ahead of print.
- Lam NCY, Yeung HY, Li WK, et al. Cognitive impairment in irritable bowel syndrome (IBS): a systematic review. Brain Res. 2019;1719(January):274–284.
- Hu Z, Li M, Yao L, et al. The level and prevalence of depression and anxiety among patients with different subtypes of irritable bowel syndrome: a network meta-analysis. BMC Gastroenterol. 2021;21(1):23.
- Tarar ZI, Farooq U, Zafar Y, et al. Burden of anxiety and depression among hospitalized patients with irritable bowel syndrome: a nationwide analysis. Ir J Med Sci. 2023. Epub ahead of print.
- Kinsinger SW. Cognitive-behavioral therapy for patients with irritable bowel syndrome: current insights. Psychol Res Behav Manage. 2017;10:231–237.
- Eijsbouts C, Zheng T, Kennedy NA, et al. Genome-wide analysis of 53,400 people with irritable bowel syndrome highlights shared genetic pathways with mood and anxiety disorders. Nat Genet. 2021;53(11):1543–1552.
- Elsenbruch S. Abdominal pain in irritable bowel syndrome: a review of putative psychological, neural and neuro-immune mechanisms. Brain Behav Immun. 2011;25(3):386–394.
- Mayer EA, Labus J, Aziz Q, et al. Role of brain imaging in disorders of brain-gut interaction: a Rome Working Team Report. Gut. 2019;68(9):1701–1715.
- Hong JY, Naliboff B, Labus JS, et al. Altered brain responses in subjects with irritable bowel syndrome during cued and uncued pain expectation. Neurogastroenterol Motil. 2016;28(1):127–138.
- Rogers GB, Keating DJ, Young RL, et al. From gut dysbiosis to altered brain function and mental illness: mechanisms and pathways. Mol Psychiatry. 2016;21(6):738–748.
- Mayer EA, Tillisch K, Gupta A. Gut/brain axis and the microbiota. J Clin Invest. 2015;125(3):926–938.
- Mayer EA, Ryu HJ, Bhatt RR. The neurobiology of irritable bowel syndrome. Mol Psychiatry. Published online February 2023;28(4):1451–1465.
- Labus JS, Hollister EB, Jacobs J, et al. Differences in gut microbial composition correlate with regional brain volumes in irritable bowel syndrome. Microbiome. 2017;5(1):49.
- Wong KMF, Yuen SSY, Mak ADP. Neurocognitive characteristics of individuals with irritable bowel syndrome. East Asian Arch Psychiatry. 2019;29(2):48–56.
- Blankstein U, Chen J, Diamant NE, et al. Altered brain structure in irritable bowel syndrome: potential contributions of pre-existing and disease-driven factors. Gastroenterology. 2010;138(5):1783–1789.
- Nan J, Yang W, Meng P, et al. Changes of the postcentral cortex in irritable bowel syndrome patients. Brain Imaging Behav. 2020;14(5):1566–1576.
- Seminowicz DA, Labus JS, Bueller JA, et al. Regional gray matter density changes in brains of patients with irritable bowel syndrome. Gastroenterology. 2010;139(1):48–57.e2.
- Ma X, Li S, Tian J, et al. Altered brain spontaneous activity and connectivity network in irritable bowel syndrome patients: a resting-state fMRI study. Clin Neurophysiol. 2015;126(6):1190–1197.
- Qi R, Liu C, Ke J, et al. Abnormal amygdala resting-state functional connectivity in irritable bowel syndrome. AJNR Am J Neuroradiol. 2016;37(6):1139–1145.
- Aizawa E, Sato Y, Kochiyama T, et al. Altered cognitive function of prefrontal cortex during error feedback in patients with irritable bowel syndrome, based on fMRI and dynamic causal modeling. Gastroenterology. 2012;143(5):1188–1198.
- Bagga D, Reichert JL, Koschutnig K, et al. Probiotics drive gut microbiome triggering emotional brain signatures. Gut Microbes. 2018;9(6):486–496.
- Lew LC, Hor YY, Yusoff NAA, et al. Probiotic Lactobacillus plantarum P8 alleviated stress and anxiety while enhancing memory and cognition in stressed adults: a randomised, double-blind, placebo-controlled study. Clin Nutr. 2019;38(5):2053–2064.
- Tillisch K, Labus J, Kilpatrick L, et al. Consumption of fermented milk product with probiotic modulates brain activity. Gastroenterology. 2013;144(7):1394–1401.e4.
- Rao SSC, Rehman A, Yu S, et al. Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis article. Clin Transl Gastroenterol. 2018;9(6):162.
- Tooley KL. Effects of the human gut microbiota on cognitive performance, brain structure and function: a narrative review. Nutrients. 2020;12(10):3009.
- Salami M. Interplay of good bacteria and central nervous system: cognitive aspects and mechanistic considerations. Front Neurosci. 2021;15:613120.
- Lundervold AJ, Hillestad EMR, Lied GA, et al. Assessment of self-reported executive function in patients with irritable bowel syndrome using a machine-learning framework. J Clin Med. 2023;12(11):3771.
- Lee SP, Sung IK, Kim JH, et al. The effect of emotional stress and depression on the prevalence of digestive diseases. J Neurogastroenterol Motil. 2015;21(2):273–282.
- Zamani M, Alizadeh-Tabari S, Zamani V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment Pharmacol Ther. 2019;50(2):132–143.
- Simpson CA, Mu A, Haslam N, et al. Feeling down? A systematic review of the gut microbiota in anxiety/depression and irritable bowel syndrome. J Affect Disord. 2020;266:429–446.
- Mudyanadzo TA, Hauzaree C, Yerokhina O, et al. Irritable bowel syndrome and depression: a shared pathogenesis. Cureus. Published online August 2018;10(8):e3178.
- Liu Y, Zhang L, Wang X, et al. Similar fecal microbiota signatures in patients with diarrhea-predominant irritable bowel syndrome and patients with depression. Clin Gastroenterol Hepatol. 2016;14(11):1602–1611.e5.
- Randolph C, Tierney MC, Mohr E, et al. The repeatable battery for the assessment of neuropsychological status (RBANS): preliminary clinical validity. J Clin Exp Neuropsychol. 1998;20(3):310–319.
- Berentsen B, Nagaraja BH, Teige EP, et al. Study protocol of the Bergen brain-gut-microbiota-axis study. Medicine (Baltimore). 2020;99(37):e21950. No(e21950)(July).
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370.
- Francis CY, Morris J, Whorwell PJ. The irritable bowel severity scoring system: a simple method of monitoring irritable bowel syndrome and its progress. Aliment Pharmacol Ther. 1997;11(2):395–402.
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillside (NJ): Lawrence Erlbaum; 1988.
- Moore DJ, Eccleston C, Keogh E. Cognitive load selectively influences the interruptive effect of pain on attention. Pain. 2017;158(10):2035–2041.
- Moriarty O, McGuire BE, Finn DP. The effect of pain on cognitive function: a review of clinical and preclinical research. Prog Neurobiol. 2011;93(3):385–404.
- Patrick KS, Sanborn V, Gunstad J, et al. Poorer cognitive performance is associated with gastrointestinal symptoms in otherwise healthy young adults. Dig Dis. 2023;41(1):74–79.
- Sugaya N, Shirotsuki K, Nakao M. Cognitive behavioral treatment for irritable bowel syndrome: a recent literature review. Biopsychosoc Med. 2021;15(1):23.
- Sarter L, Heider J, Kirchner L, et al. Cognitive and emotional variables predicting treatment outcome of cognitive behavior therapies for patients with medically unexplained symptoms: a meta-analysis. J Psychosom Res. 2021;146:110486.
- Leeming ER, Johnson AJ, Spector TD, et al. Effect of diet on the gut microbiota: rethinking intervention duration. Nutrients. 2019;11(12):2862.
- Thaiss CA, Zeevi D, Levy M, et al. Transkingdom control of microbiota diurnal oscillations promotes metabolic homeostasis. Cell. 2014;159(3):514–529.
- Raudeberg R, Iverson G L, Hammar Å. Norms matter: U.S. normative data under-estimate cognitive deficits in Norwegians with schizophrenia spectrum disorders. Clin Neuropsychol. 2019;33(sup1):58–74.