Abstract
Aims
To evaluate outcomes of ERCP as first-line management in patients with malignant biliary obstruction (MBO) of all causes and stages, reflecting a real-life setting.
Methods
Retrospective observational study of patients with ERCP as the first-line management of MBO at Oslo University Hospital between 2015 and 2021. Primary outcome measure was a ≥ 50% decrease from the pre-procedural bilirubin within 30 days after ERCP. Secondary outcome measures were technical success of ERCP, complications and overall mortality.
Results
A total of 596 patients were included, median age 70 years. ASA score was ≥ III in 67% of patients. The most common cancers causing MBO were pancreatic cancer (52%), metastatic lesions (20%) and cholangiocarcinoma (16%). The primary outcome measure was achieved in 62% of patients. With endoscopic access, overall technical success was 80% with 85% for the distal extrahepatic group, 71% for the perihilar, 40% for the intrahepatic and 53% for multiple level MBOs. Reinterventions were performed in 27% of the patients. Complications occurred in 15% of the patients, including post-ERCP pancreatitis in 9%. Most complications were of minor/moderate severity (81%). Overall mortality was 33% within the first 90 days. Patients deceased by the end of the study period (83%) had median survival of 146 days (range 1–2,582 days).
Conclusions
ERCP has a high rate of clinical effect and technical success in the management of both distal extrahepatic and perihilar MBO. Our data indicate that ERCP is a valid option in the first-line management of MBO.
Introduction
Malignant biliary obstruction (MBO) is a cancer-related narrowing of the bile ducts. There are two principal categories, ductal infiltration and external compression [Citation1]. Pancreatic cancer (PC) and cholangiocarcinoma (CCA) are the most common causes of internal infiltration of the bile ducts while external compression is typically seen in metastatic disease as well as in PC [Citation2–4]. The site of obstruction is categorized anatomically as distal extrahepatic, perihilar or intrahepatic. Some patients have obstruction at multiple levels.
MBO may lead to chronic cholestasis with jaundice, malaise and increased risk of cholangitis [Citation5,Citation6]. These are debilitating symptoms, and may limit treatment options, leaving patients ineligible for e.g., chemotherapy, due to cholestasis and/or reduced performance status [Citation7]. Overall, MBO is associated with high morbidity and mortality. Optimal management of MBO is therefore essential.
The European Society for Gastrointestinal Endoscopy (ESGE) recommends endoscopic retrograde cholangiopancreatography (ERCP) with stenting as the first-line therapy for distal MBO [Citation8], whereas percutaneous transhepatic biliary drainage (PTBD) and endoscopic ultrasound-guided biliary drainage (EUS-BD) represent second-line methods [Citation9–11]. For hilar MBO, the ESGE guidelines are less absolute and the recommendation differs based on the Bismuth-Corlette classification (type I-II: ERCP, type III-IV: PTBD). In the American Society for Gastrointestinal Endoscopy (ASGE) guidelines, ERCP and PTBD are considered equivalent for unresectable malignant hilar obstruction [Citation12]. Hence, the choice of modality is debated and often influenced by local expertise [Citation8].
To our knowledge, there are no recent studies reporting on outcomes of ERCP-related treatment in an unselected, large cohort of patients with MBO. Our aim was to evaluate ERCP as first-line management in patients with MBO, including distal, perihilar and intrahepatic, in a real-life hospital cohort in Norway, with all stages of malignant disease.
Methods
Study design and study population
We conducted a retrospective observational study including patients who underwent ERCP-based treatment as the first-line management for MBO at Oslo University Hospital (OUH) in a seven-year period. OUH serves both as a hospital for the local catchment area and as a tertiary referral centre for about 2.9 million inhabitants of the South-Eastern region of Norway.
The endoscopy database (EndoBase®, Olympus) was retrospectively reviewed to identify patients who underwent ERCP in the period between January 1st 2015 and December 31st 2021. Mortality data were collected until 175 days after the latest patient inclusion (June 24th 2022).
Patients aged ≥18 years, scheduled for ERCP as the first-line management of MBO and with a confirmed diagnosis by histology and/or imaging, were eligible for inclusion. Clinical jaundice and/or an elevated total bilirubin >25 µmol/L were required for inclusion in the study. Both distal and proximal biliary obstructions were included, the latter was also further specified as perihilar, intrahepatic or multiple levels. If the scheduled ERCP could not be completed due to no endoscopic access to the papilla of Vater, the patients were still included. Patients were only excluded if a previous drainage procedure had been performed for the same indication. All eligible ERCP procedures were included, also balloon-assisted-enteroscopy ERCP (BAE-ERCP).
Data on demographics, clinical presentation, aetiology, imaging, procedural aspects, technical success, clinical outcome, complications and mortality were registered by review of the electronic medical records. Biochemical measurements were obtained from the laboratories at OUH or at the referring hospitals. Pre-procedural morbidity was classified according to the American Society of Anesthesiologists (ASA) score. Perihilar CCA was classified according to Bismuth-Corlette classification [Citation13].
Outcomes
The primary outcome measure was defined as a ≥ 50% decrease from the pre-procedural bilirubin within 30 days after the primary ERCP, which we chose as a surrogate for clinical effect. In cases of multiple bilirubin measurements until 30 days after primary ERCP, the lowest bilirubin level registered during the period was used.
Secondary outcome measures were technical success of ERCP, complications and overall mortality. Technical success was defined as adequate biliary drainage of all intended parts of the bile ducts. Successful cannulation of the papilla of Vater was defined as access to the common bile duct (CBD) including initial cannulation. Deep cannulation was defined as further selective access to the desired bile ducts. Patient records were reviewed for complications during the first 30-day period after the initial ERCP, and for 90-day mortality. Post-ERCP adverse events, including acute pancreatitis, bleeding, biliary infection, perforation or any other adverse outcomes requiring hospital admission or prolonged hospital stay, were registered. Severity of complications were graded as mild, moderate and severe according to the Cotton criteria [Citation14]. Patients who had a complication not defined in the Cotton classification (other), were graded according to the consequence (hospital stay and/or need of another treatment or intervention). The most severely graded complication was registered in cases with more than one complication. Lack of clinical effect from ERCP included persisting cholestatic symptoms or bilirubin elevation. If re-intervention was performed, the first procedure within the first 30 days period after initial ERCP was registered. The outcome measures were evaluated for all levels of biliary obstruction combined, as well as for each different obstruction level (distal, perihilar, intrahepatic, multiple levels).
Statistical analysis
Continuous variables are presented as median (range) or mean (SD), depending on data distribution. The chi-square test was used to compare frequencies. Comparison between continuous variables was performed using the t test or the Kruskal-Wallis test, as appropriate. Survival was calculated by using the Kaplan-Meier’s method, and differences between groups were assessed by the log-rank test. A p-value < 0.05 was considered statistically significant. Missing follow-up data were regarded as missing at random. Statistical analysis were performed using IBM SPSS Statistics version 28 (IBM Corp. Armonk, NY, USA).
Ethical approval
The study was approved by the hospital review board (PVO 20/20311) according to the general guidelines provided by the Norwegian authorities.
Results
Patient characteristics
In the seven-year study period, 7,960 ERCP procedures were performed at OUH. Among these, 596 ERCPs were included for final analysis (). Patient demographics at inclusion are presented in . The patients were 55% men (n = 328), predominantly elderly with median age 70 years (range 21–104) and a median bilirubin level of 215 µmol/L (range 28–935 µmol/L). They had advanced co-morbidity based on evaluation of ASA-score ≥ III (66.6%) and need for in-hospital treatment (88.8%) at time of ERCP. Only 118 patients (19.8%) underwent potentially curative cancer surgery after the primary ERCP, leaving most patients in a palliative setting. The main indication for ERCP was cholestatic symptoms and signs (n = 332, 55.7%). The majority of patients had extrahepatic MBO (n = 436, 73.2%), and PC (n = 308, 51.8%) was the dominant cancer type.
Figure 1. Flowchart for identification of primary ERCP procedures for malignant biliary obstruction (MBO) performed at Oslo University Hospital in the period 2015–2021. ERCP: Endoscopic retrograde cholangiopancreatography. PTBD: Percutaneous transhepatic biliary drainage.
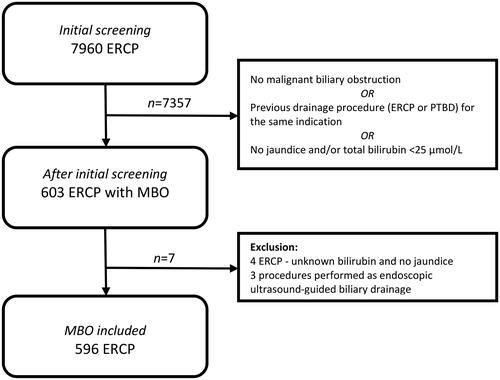
Table 1. Baseline characteristics of individuals and ERCP procedures (n = 596).
ERCP procedure
Endoscopic access to the papilla was achieved in 565/596 procedures (94.8%). In this group, successful cannulation of the papilla of Vater was achieved in 503/565 patients (89.0%) and selective deep access after successful cannulation in 491/565 patients (86.9%). One or more stents were placed in 474 procedures (474/596, 79.5%). Fully covered metal stents dominated for distal extrahepatic MBO, while the majority of patients with hilar and intrahepatic MBOs received plastic stents (). In total, 122/596 patients did not receive a stent (20.5%). Of these, 12 procedures were considered to be a technical success without the use of stent (Table S3, supplementary material). The remaining 110/122 patients that did not receive a stent, included 31 patients with no endoscopic access to the papilla, and 79 patients where ERCP was technical unsuccessful.
Table 2. ERCP procedural data (n = 596) as first-line management of malignant biliary obstruction.
Non-steroidal anti-inflammatory drugs (NSAID) to avoid post-ERCP pancreatitis (PEP) were administered in 71.8% of the procedures. In 504 cases (84.6%), the endoscopy team administered conscious sedation using midazolam and fentanyl or alfentanil. In 9/596 procedures (1.5%), the ERCP was terminated because of inadequate sedation. Balloon-assisted enteroscopy ERCP was performed in 11/596 procedures (1.8%), details on these procedures are described in Table S4 (supplementary material).
Primary outcome
The primary outcome measure with a ≥ 50% decrease in bilirubin levels within the first 30 days after the primary ERCP was achieved in 372 (62.4%) patients (, ). Bilirubin levels in the 30 day follow-up period were missing for 58/596 patients (9.7%). For the patients not reaching the primary outcome measure compared to those who did, fewer had technical success (68.1% vs 77.2%, p = 0.027) and a higher frequency of reintervention was noted (36.9% vs 26.1%, p = 0.013). In further detail, a total of 520/596 patients (87%) had baseline bilirubin levels ≥80 µmol/L. Of these, bilirubin levels after ERCP was missing in 48 patients, leaving 472 patients. In total, 284 patients (284/472, 60.2%) achieved bilirubin levels <80 µmol/L within the first 30 days after the primary ERCP.
Figure 2. Bilirubin levels at baseline, after primary ERCP for all patients combined, for the patients without reintervention and for the patients undergoing reintervention (before and after). Baseline bilirubin missing for six patients. Bilirubin levels in the 30 days follow-up period was missing for 58 patients.
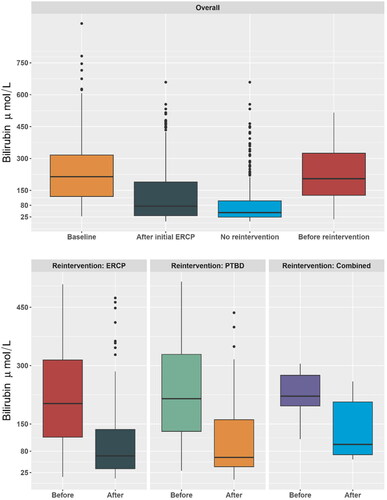
Table 3. Reintervention and decrease in bilirubin levels ≥ 50% (n = 596 ERCP procedures).
Technical success and need of reinterventions
In patients with endoscopic access to the papilla, the majority of procedures were considered a technical success (n = 450/565, 79.6%). Technical success was achieved in 85.4% (n = 350/410) of patients with distal extrahepatic MBO, and in 70.6% (n = 77/109) of patients with perihilar MBO Successful cannulation of the papilla was achieved in 88.0% (n = 361/410) of distal extrahepatic MBO and in 94.5% (n = 103/109) of perihilar MBO. Further details are presented in .
Within the first 30 days, 161 patients (27.0%) underwent reintervention (., Figure S1, supplementary material). Of the 146 patients with no technical success, 113 (77.4%) underwent reintervention, and of the 450 patients with technical success, 48 (10.7%) underwent reintervention. In the group of patients with no technical success (n = 146), the need for reintervention was acknowledged during the primary ERCP for 106 patients. Causes of reinterventions were lack of clinical effect of the first ERCP procedure (n = 130, 80.7%), post-ERCP complications (n = 13, 8.1%) and other causes (n = 18, 11.2%) such as equipment failure or need for a different sedation strategy. Complications resulting in reinterventions were perforations at any level (five patients), cholangitis (four patients) and bleeding (two patients). For reintervention, 52.8% (n = 85) of the patients had PTBD, 43.5% (n = 70) had a new ERCP and 3.7% (n = 6) underwent a combined procedure. Neither the level of obstruction nor the cancer type differed in terms of reintervention modality.
ERCP-related complications
A total of 104 post-ERCP complications occurred in 91 patients (15.3%) within the first 30 days ( and ). Complications were mainly minor or moderate (81.3%). Pancreatitis occurred as complication in 56 (9.4%) of the patients and was registered as mild (hospitalization <4 days) in 21/56 patients, moderate (hospitalization 4–10 days) in 24/56 patients, and severe (hospitalization more than ten days or the need for an intervention) in 11/56 patients.
Table 4. Frequency and severity of complications after ERCP (n = 596).
Two patients with severe procedure-related complications died within 30 days. One of these patients died from cholecystitis after having received a metal stent for MBO related to a locally advanced pancreatic cancer. The other patient died of multi organ failure in a situation with post-ERCP pancreatitis four days after the ERCP for MBO with underlying pancreatic cancer (classified as a severe pancreatitis, ).
Overall mortality
Overall mortality was 15.6% (n = 95) within the first 30 days and 32.7% (n = 195) within the first 90 days. At the end of the study period, 99 patients (16.6%) were still alive. Only one patient was lost to follow-up (non-resident). Patients deceased at the end of the study period (n = 497) had a median survival of 146 days (range 1–2,582 days). Patients with metastatic cancer as cause of obstruction had a higher 90-day mortality (49.6%) compared to all other cancer types (28.6%, p < 0.001). Also, patients with technical success in the primary ERCP had a lower 90-day mortality (28.9%) compared to patients without technical success in the primary procedure (50.5%, p < 0.001). The ASA score was significantly higher in patients who died within the first 90 days (p < 0.001). For the patients undergoing reintervention, there was a higher 90-day mortality (41.6% vs 28.2%, p = 0.002), see .
Discussion
The present real world study demonstrates that intervention with ERCP is an efficient and safe treatment option of both distal extrahepatic and perihilar MBO. Based on our results, intervention with ERCP should be considered as first line management of MBO.
Figure 3. Kaplan-Meier overall survival plot of patients with or without reintervention after their primary ERCP due to MBO.
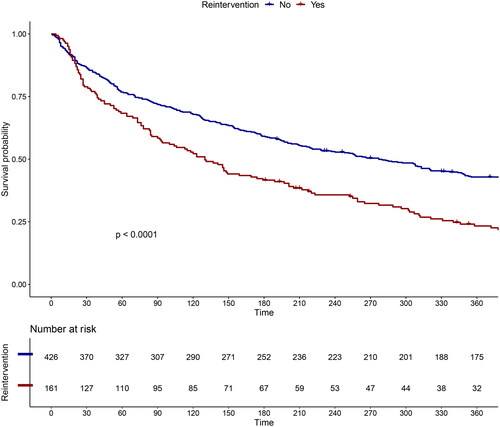
Table 5. Complications and level of malignant biliary obstruction in 596 procedures.
The primary outcome measure of clinical effect defined by a ≥ 50% decrease in bilirubin within 30 days was reached in 62.4% of all patients. The rate of bilirubin regression after stenting will be dependent on the baseline bilirubin level [Citation15]. Thus, to be able to reveal something about the effect of the primary intervention other than reintervention within 30 days, we chose this pragmatic variable. In the setting of MBO, ERCP has clear benefits over biliary drainage by PTBD, which often leads to added reduction in quality of life due to pain and increased risk of infection at the puncture site for the external catheter [Citation16–18]. Importantly, a similar proportion of patients (60.2%) achieved bilirubin levels of <80 µmol/L within the first 30 days after the primary ERCP, leaving the majority of these patients eligible for active palliative treatment with chemotherapy.
Technical success was achieved in 79.6% of the ERCP procedures with endoscopic access to the papilla, slightly higher than the clinical effect rate of 62.4%. This number might seem to be below the quality indicators for ERCP according to ASGE and ESGE criteria [Citation19,Citation20]. However, the definition of technical success is based on the strict subjective assessment of the endoscopist, which may account at least in part for the difference [Citation15]. Our cannulation rate was 89%, similar to the key performance measure (for expert centers) in the ESGE guidelines [Citation20]. In these procedures stent placement was achived in >95%, in line with the mentioned guidelines.
The rate of technical success was in general lower for perihilar (70.6%) and multiple level (52.8%) MBO compared to distal MBO (85.4%), which is in accordance with available data [Citation21,Citation22]. However, our rate of technical success is comparable to others [Citation23]. Recent reports indicate that for distal MBO, difficult biliary cannulation (DBC) can be an underestimated problem [Citation21]. In our study, technical success was 85.4% in patients with distal MBO, and the failure of cannulation in these patients was 12.0% (n = 49/410). These numbers are comparable with previous reports evaluating DBC in distal MBO [Citation21]. Correspondingly, reinterventions were more frequent in patients with proximal MBO (perihilar and intrahepatic) or multiple level MBO, compared to the distal MBO. Also, in perihilar CCAs, reinterventions were more common compared to other cancer types. This likely reflects the technical and anatomical challenges of ERCP in the patients with perihilar MBO, and is consistent with the results of others [Citation24]. In obtaining biliary drainage, a meta-analysis has shown that primary PTBD was superior to primary ERCP in patients with perihilar MBO [Citation25]. This finding could suggest that PTBD should be the procedure of choice in these patients. Interestingly, an RCT comparing ERCP versus PTBD in patients with resectable perihilar CCA was prematurely stopped because of higher all-cause mortality in the PTBD group [Citation24].
In recent years, EUS-BD has also been an alternative for biliary drainage of MBO. A systematic review and meta-analysis comparing PTBD and EUS-BD after failed ERCP, concluded that EUS-guided interventions showed significantly better clinical effect, lower rate of adverse event and less need of reintervention [Citation26]. Another advantage is the possibility to convert to EUS-BD when one realizes that there is not access to the papilla during ERCP. In our material, this could have been a valid option in about 5% of the patients. However, when discussing EUS-BD for MBO, one must keep in mind that this is mainly an option in expert centers and for distal MBO, since data on hilar MBO is limited [Citation27,Citation28]. The modality of choice for drainage of perihilar MBO is still debated and more studies are needed. Our study supports that ERCP can be chosen as first line management also in this subgroup of patients [Citation12,Citation29]. Nevertheless, choosing between PTBD and ERCP will still depend on local expertise.
Post-ERCP complications occurred in about 15% of the procedures, the majority being of minor or moderate severity. Pancreatitis was the most common adverse event. In the literature, incidence rates of post-ERCP pancreatitis range from 3.5% in standard-risk patients to 14.7% in high-risk patients [Citation30]. A systematic review and meta-analysis comparing ERCP and EUS-guided biliary drainage for the management of MBO, found that 9.5% of the patients in the ERCP-group developed procedure-related pancreatitis [Citation31]. Another study evaluating ERCP in patients with distal MBO reported overall adverse events in 15.6% of the patients [Citation21]. Our rate of complications is comparable to previous reports.
The patients in the present study had an overall mortality of 32.7% within the first 90 days. A recent study found mortality of 19.1% in the 30-day period after ERCP for the palliation of MBO, and the median survival from the first ERCP was 4 months, compared to a median survival of 4.7 months in our study [Citation32]. A different study, looking at unresectable pancreatobiliary cancers in palliative treatment, found a 90-day mortality of 46.9% after ERCP [Citation33]. In our study, we only identified two probable procedure-related deaths, and the rate of post-ERCP complications was as expected. Thus, the relatively high 90-day mortality rate likely reflects the poor prognosis of the underlying cancers leading to MBO, and not the risk of the ERCP procedure [Citation34–36]. As expected, advanced disease reflected by high ASA score and MBO from metastatic cancer significantly predicted poor survival.
Strengths of our study includes the large number of patients from a real-life cohort, comprising all patients in our institution undergoing ERCP for the initial management for MBO in a 7-year period. All grades of morbidity, as well as levels of biliary obstruction and stage of the cancer disease were included, reflecting the variety of patients in a clinical practice. All endoscopy reports followed a structured system of reporting, and procedures were performed by an experienced team of endoscopists.
Our study has some important limitations. First, the retrospective design led to some missing data, but completeness of data were adequate for the main primary and secondary outcome measures of the study. Second, as a tertiary referral center, there may have been a referral bias, where more complex cases were referred to our institution, this may influence the generalizability of the results. Third, we did not register data on advanced cannulation techniques, which could have provided more detailed information in situations where technical success was not achieved and about endoscopic risk factors for complications.
Patients with MBO have a high morbidity and mortality, with most ERCP procedures performed in a palliative setting. Therefor it is of relevance to have an up to date study showing the results of primary ERCP treatment in such an unselected cohort. In conclusion, our study provides important experience from a large real world cohort on the clinical management of patients with MBO, and demonstrates that ERCP is a valuable and safe option in the first-line management of distal extrahepatic and perihilar MBO.
Abbrevations
| MBO | = | Malignant biliary obstruction |
| ESGE | = | European Society for Gastrointestinal Endoscopy |
| ASGE | = | American Society for Gastrointestinal Endoscopy |
| ERCP | = | Endoscopic Retrograde Cholangiopancreatography |
| PTBD | = | Percutaneous Transhepatic Biliary Drainage |
| EUS-BD | = | Endoscopic Ultrasound-guided Biliary Drainage |
| OUH | = | Oslo University Hospital |
| BAE-ERCP | = | Balloon-assisted enteroscopy ERCP |
| ASA | = | American Society of Anesthesiologists |
| PC | = | Pancreatic Cancer |
| CCA | = | Cholangiocarcinoma |
| GBC | = | Gallbladder Carcinoma |
| CBD | = | Common bile duct |
| EPT | = | Endoscopic papillotomy |
| PEP | = | Post-ERCP pancreatitis |
| TS | = | Technical success |
| DBC | = | Difficult biliary cannulation |
Supplemental Material
Download Zip (225.9 KB)Disclosure statement
Medhus AW has received an unrestricted research grant from Takeda. None of the other authors reports any conflicts of interest to disclose.
References
- Tsetis D, Krokidis Μ, Negru D, et al. Malignant biliary obstruction: the current role of interventional radiology. Ann Gastroenterol. 2016;29(1):33–36.
- Kapoor BS, Mauri G, Lorenz JM. Management of biliary strictures: state-of-the-art review. Radiology. 2018;289(3):590–603. doi: 10.1148/radiol.2018172424.
- Jarosova J, Macinga P, Hujova A, et al. Endoscopic radiofrequency ablation for malignant biliary obstruction. World J Gastrointest Oncol. 2021;13(10):1383–1396. doi: 10.4251/wjgo.v13.i10.1383.
- Banales JM, Cardinale V, Carpino G, et al. Expert consensus document: cholangiocarcinoma: current knowledge and future perspectives consensus statement from the European Network for the Study of Cholangiocarcinoma (ENS-CCA). Nat Rev Gastroenterol Hepatol. 2016;13(5):261–280. doi: 10.1038/nrgastro.2016.51.
- Park W, Chawla A, O’Reilly EM. Pancreatic cancer: a review. JAMA. 2021;326(9):851–862. doi: 10.1001/jama.2021.13027.
- Kiriyama S, Kozaka K, Takada T, et al. Tokyo guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25(1):17–30. doi: 10.1002/jhbp.512.
- Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 2011;364(19):1817–1825. doi: 10.1056/NEJMoa1011923.
- Dumonceau JM, Tringali A, Papanikolaou IS, et al. Endoscopic biliary stenting: indications, choice of stents, and results: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline – updated October 2017. Endoscopy. 2018;50(9):910–930. doi: 10.1055/a-0659-9864.
- Pereiras RV, Jr., Rheingold OJ, Huston D, et al. Relief of malignant obstructive jaundice by percutaneous insertion of a permanent prosthesis in the biliary tree. Ann Intern Med. 1978;89(5 Pt 1):589–583. doi: 10.7326/0003-4819-89-5-589.
- Soehendra N, Reynders-Frederix V. Palliative bile duct drainage – a new endoscopic method of introducing a transpapillary drain. Endoscopy. 1980;12(1):8–11. doi: 10.1055/s-2007-1021702.
- Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy. 2001;33(10):898–900. doi: 10.1055/s-2001-17324.
- Qumseya BJ, Jamil LH, Elmunzer BJ, et al. ASGE guideline on the role of endoscopy in the management of malignant hilar obstruction. Gastrointest Endosc. 2021;94(2):222–234.e22. doi: 10.1016/j.gie.2020.12.035.
- Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet. 1975;140(2):170–178.
- Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37(3):383–393. doi: 10.1016/s0016-5107(91)70740-2.
- Weston BR, Ross WA, Wolff RA, et al. Rate of bilirubin regression after stenting in malignant biliary obstruction for the initiation of chemotherapy: How soon should we repeat endoscopic retrograde cholangiopancreatography? Cancer. 2008;112(11):2417–2423. doi: 10.1002/cncr.23454.
- Asadi H, Hollingsworth R, Pennycooke K, et al. A review of percutaneous transhepatic biliary drainage at a tertiary referral Centre. Clin Radiol. 2016;71(12):1312.e7–e11. doi: 10.1016/j.crad.2016.05.013.
- Nennstiel S, Weber A, Frick G, et al. Drainage-related complications in percutaneous transhepatic biliary drainage: an analysis over 10 years. J Clin Gastroenterol. 2015;49(9):764–770. doi: 10.1097/MCG.0000000000000275.
- Lee TH, Moon JH, Stuart S. Role of ERCP in malignant hilar biliary obstruction. Gastrointest Endosc Clin N Am. 2022;32(3):427–453. doi: 10.1016/j.giec.2022.01.003.
- Adler DG, Lieb JG, 2nd, Cohen J, et al. Quality indicators for ERCP. Gastrointest Endosc. 2015;81(1):54–66. doi: 10.1016/j.gie.2014.07.056.
- Domagk D, Oppong KW, Aabakken L, et al. Performance measures for ERCP and endoscopic ultrasound: a European Society of Gastrointestinal Endoscopy (ESGE) quality improvement initiative. Endoscopy. 2018;50(11):1116–1127. doi: 10.1055/a-0749-8767.
- Fugazza A, Troncone E, Amato A, et al. Difficult biliary cannulation in patients with distal malignant biliary obstruction: An underestimated problem? Dig Liver Dis. 2022;54(4):529–536. doi: 10.1016/j.dld.2021.07.010.
- Shanmugarajah I, Solhaug M, Aslam O, et al. Efficacy and safety assessment of ERCP in patients with malignant biliary obstruction. Acta Gastroenterol Belg. 2017;80(4):487–491.
- Keulen AV, Gaspersz MP, van Vugt JLA, et al. Success, complication, and mortality rates of initial biliary drainage in patients with unresectable perihilar cholangiocarcinoma. Surgery. 2022;172(6):1606–1613. doi: 10.1016/j.surg.2022.06.028.
- Coelen RJS, Roos E, Wiggers JK, et al. Endoscopic versus percutaneous biliary drainage in patients with resectable perihilar cholangiocarcinoma: a multicentre, randomised controlled trial. Lancet Gastroenterol Hepatol. 2018;3(10):681–690. doi: 10.1016/S2468-1253(18)30234-6.
- Zhao XQ, Dong JH, Jiang K, et al. Comparison of percutaneous transhepatic biliary drainage and endoscopic biliary drainage in the management of malignant biliary tract obstruction: a meta-analysis. Dig Endosc. 2015;27(1):137–145. doi: 10.1111/den.12320.
- Sharaiha RZ, Khan MA, Kamal F, et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc. 2017;85(5):904–914. doi: 10.1016/j.gie.2016.12.023.
- Nakai Y, Kogure H, Isayama H, et al. Endoscopic ultrasound-guided biliary drainage for unresectable hilar malignant biliary obstruction. Clin Endosc. 2019;52(3):220–225. doi: 10.5946/ce.2018.094.
- Sundaram S, Dhir V. EUS-guided biliary drainage for malignant hilar biliary obstruction: a concise review. Endosc Ultrasound. 2021;10(3):154–160. doi: 10.4103/EUS-D-21-00004.
- Mocan T, Horhat A, Mois E, et al. Endoscopic or percutaneous biliary drainage in hilar cholangiocarcinoma: When and how? World J Gastrointest Oncol. 2021;13(12):2050–2063. doi: 10.4251/wjgo.v13.i12.2050.
- Andriulli A, Loperfido S, Napolitano G, et al. Incidence rates of post-ERCP complications: a systematic survey of prospective studies. Am J Gastroenterol. 2007;102(8):1781–1788. doi: 10.1111/j.1572-0241.2007.01279.x.
- Kakked G, Salameh H, Cheesman AR, et al. Primary EUS-guided biliary drainage versus ERCP drainage for the management of malignant biliary obstruction: a systematic review and meta-analysis. Endosc Ultrasound. 2020;9(5):298–307. doi: 10.4103/eus.eus_10_20.
- Harvey PR, Baldwin S, Mytton J, et al. Higher volume providers are associated with improved outcomes following ERCP for the palliation of malignant biliary obstruction. EClinicalMedicine. 2020;18:100212. doi: 10.1016/j.eclinm.2019.11.005.
- Termsinsuk P, Charatcharoenwitthaya P, Pausawasdi N. Development and validation of a 90-day mortality prediction model following endobiliary drainage in patients with unresectable malignant biliary obstruction. Front Oncol. 2022;12:922386. doi: 10.3389/fonc.2022.922386.
- Latenstein AEJ, van der Geest LGM, Bonsing BA, et al. Nationwide trends in incidence, treatment and survival of pancreatic ductal adenocarcinoma. Eur J Cancer. 2020;125:83–93. doi: 10.1016/j.ejca.2019.11.002.
- Izquierdo-Sanchez L, Lamarca A, La Casta A, et al. Cholangiocarcinoma landscape in Europe: Diagnostic, prognostic and therapeutic insights from the ENSCCA registry. J Hepatol. 2022;76(5):1109–1121. doi: 10.1016/j.jhep.2021.12.010.
- Tavakkoli A, Elmunzer BJ, Waljee AK, et al. Survival analysis among unresectable pancreatic adenocarcinoma patients undergoing endoscopic or percutaneous interventions. Gastrointest Endosc. 2021;93(1):154–162.e5. doi: 10.1016/j.gie.2020.05.061.
