Abstract
Background
The natural history of symptomatic uncomplicated gallstone disease is largely unknown. We examined the risk of progressing from symptomatic uncomplicated to complicated gallstone disease in a large regional cohort of patients, where disruptions in elective surgical capacities have led to the indefinite postponement of surgery for benign conditions, including cholecystectomies.
Methods
Patients with radiologically diagnosed incident symptomatic and uncomplicated gallstone disease were identified from outpatient clinics and emergency departments on the Island of Funen, Denmark. The absolute risk of complications (cholecystitis, cholangitis, pancreatitis, acute cholecystectomy for unremitting pain) was calculated using death and elective cholecystectomies as competing risks using the Aalen-Johansen method. Cox proportional hazards regression analysis was used to estimate hazard ratios (HRs) of gallstone complications associated with patient and gallstone characteristics.
Results
Two hundred eighty-six patients diagnosed with incident symptomatic, uncomplicated gallstone disease from 1 January 2020 to 1 July 2023 were identified. During 79,170 person-years of observation, 176 (61.5%) patients developed a gallstone-related complication. The 6-, 12- and 24-month risk of developing gallstone-related complications were 36%, 55% and 81%. The risk of developing complications related to common bile duct stones was lowest with larger stones (aHR per millimeter increase = 0.89 (0.82–0.97), p < 0.01), while no covariates were statistically significantly associated with the risk of cholecystitis. Eighty-five (30%) patients underwent elective laparoscopic cholecystectomy, with one patient (1.2%) developing a gallstone-related complication afterward.
Conclusions
The risk of developing complications to symptomatic gallstones in a general Scandinavian population is high, and prophylactic cholecystectomy should be considered.
Introduction
Symptomatic uncomplicated gallstone disease is generally considered a harmless condition with a low risk of progressing to complications such as cholecystitis, cholangitis, and pancreatitis [Citation1]. In Denmark, approximately 9000 cholecystectomies are performed annually, many for debilitating biliary colic and to prevent gallstone-related complications from occurring [Citation2]. Disruptions in elective surgery capacities brought on by the COVID-19 pandemic [Citation3] and later a nationwide nursing shortage led to the indefinite postponement of many surgeries for benign conditions, including uncomplicated gallstone disease. Although these disruptions may have had a negative effect on the health-related quality of life for the individual patient [Citation4], it has provided a unique opportunity to examine the spontaneous, clinical course of uncomplicated gallstone disease. A better understanding of the absolute risk of developing complications to symptomatic gallstones based on a contemporary population consisting of individuals from an unselected background population will, in turn, help clinicians and patients in their shared decision-making when considering elective cholecystectomy to prevent recurrent symptoms or complications to gallstones.
The primary aim of this study was to examine the absolute risk of developing gallstone-related complications to symptomatic and initially uncomplicated gallstone disease. The secondary aim was to investigate risk factors associated with the progression from uncomplicated to complicated gallstone disease.
Methods
Setting
This study was conducted as a population-based cohort study using data from medical charts for patients with a diagnosis of gallstone disease admitted to the Department of Surgery at Odense University Hospital. The hospital has three locations in Odense, Svendborg and Nyborg on the island of Funen. To treat gallstone disease, the department has a catchment area of approximately 500,000 inhabitants, which corresponds to the entire population of Funen. All outpatient contacts and in-hospital treatment directly related to gallstone disease are tax-funded. This study was approved by the local health board and legal department at Odense University Hospital under journal number 23/32374.
Identification of patients
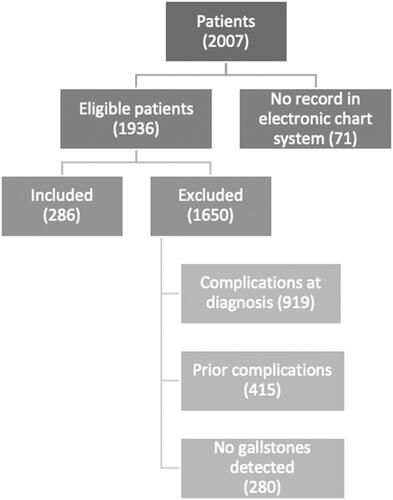
We identified all patients registered with any gallstone-related diagnosis, International Classification of Diseases (ICD)-10 codes DK8-DK858D, at the Department of Surgery at Odense University Hospital from 1 January 2020 to 1 July 2023. From this source population of all patients diagnosed with any gallstone disease, hospital charts were reviewed, and only patients with incident uncomplicated gallstone disease defined as a first diagnosis of simple cholecystolithiasis on either ultrasound (US), computed tomography (CT) or magnetic resonance cholangiopancreatography (MRCP), during the study period were included. The date of radiological diagnosis was defined as the index date. The clinical setting in which patients were diagnosed with gallstones varied, with some being diagnosed as outpatients, having initially been referred to surgical counsel from their general practitioner. Others were diagnosed in the emergency department after an acute admission with severe right upper quadrant pain. Any indication of complications to the gallstones at or before the index date was an exclusion criterion. A flowchart of the inclusion of patients is provided in .
Definition of outcomes and covariates
The primary aim of this study was to examine the absolute risk of developing complications to gallbladder stones necessitating urgent hospital care (radiological investigation or surgical/endoscopic intervention). For this purpose, we defined calculous cholecystitis, biliary pancreatitis, cholangitis, and unremitting biliary colic requiring urgent cholecystectomy as relevant outcomes. A diagnosis of calculous cholecystitis was based on relevant upper right quadrant pain and elevated temperature or c-reactive protein or leucocytes in a patient with known gallbladder stones. CT or MRI to confirm the presence of cholecystitis is not common practice in Denmark and was therefore not included in our definition of cholecystitis. Pancreatitis was defined by epigastric pain and 1) serum amylase elevated > 3 times upper limit and/or 2) radiological signs of pancreatitis on either US, CT, or MRCP. Cholangitis was defined as elevated liver function tests with elevated temperature, c-reactive protein, or leucocytes in a patient with known gallbladder stones. An MRCP with evidence of CBD stones or an endoscopic retrograde cholangiopancreatography (ERCP) with the extraction of common bile duct (CBD) stones in a patient with a clinical suspicion of cholangitis was deemed equivalent to a diagnosis of cholangitis, as defined above. An urgent cholecystectomy performed on a patient with right upper quadrant pain, but no signs of cholecystitis, cholangitis, or pancreatitis was defined as being performed for unremitting biliary colic. In equivocal cases, the discharge diagnosis defined the presence of a complication.
Because death and elective cholecystectomy performed before any gallstone-related complication prevent such complications from arising, these events were included as censoring events for Cox regressions and competing events for estimating cumulative incidences.
Covariates and definitions
We recorded data on age at examination, gender (male, female), BMI, range of total cholesterol (<5.0, 5.0–6.4, 6.5–7.9, >7.9), pregnancy (current or previous), number of prior childbirths, liver disease (cirrhosis, hepatitis, etc.), bowel disease (cancer, inflammatory bowel disease, etc.), alcohol consumption, smoking history, number of gallstones, size of gallstones in millimeters, and estrogenic affecting medicine (hormone replacement therapy, oral contraceptives, etc.).
Statistical analysis
Categorical data are presented as numbers (proportion), while continuous data are presented as means (standard deviation; SD) or median (interquartile range; IQR), depending on the distribution.
Patients were followed from the index date of the first radiological diagnosis of uncomplicated gallstone disease to either a gallstone-related complication, elective cholecystectomy, death, or the end of follow-up in November 2023, whichever occurred first. We treated elective cholecystectomies and death as competing risks and calculated cumulative incidences of complications at 6, 12, and 24 months using the Aalen-Johansen method.
We used Cox proportional hazards regression analysis to estimate hazard ratios of gallstone-related complications as a measure of relative risk. We estimated crude hazard ratios for all patient and gallstone covariates and performed adjusted analyses, including covariates associated with gallstone-related complications at a significance level of <0.1. In the adjusted analyses, we considered a p-value <0.05 statistically significant. The assumption of proportional hazards was tested using Schoenfeld residuals.
Because data on BMI were missing in 24% of patients and since BMI is a well-established risk factor for gallstone disease [Citation5], we chose to impute missing values using nearest neighbor multiple imputations based on age, gender, and ethnicity to create 100 new imputations. For this purpose, we assumed that BMI data were missing at random.
Results
We identified 286 patients (flowchart, ) with symptomatic uncomplicated gallstone disease. The cohort consisted of 85 (29.7%) males with a median age of 52 (IQR 32–68 years) and a mean BMI of 31.4 (SD 18.9). 22% had a total cholesterol level above >5 mmol/L, 37% had a smoking history, and 9% consumed more alcohol than recommended. Fifty-eight of the women were in hormone replacement therapy or used oral contraceptives, and 12 were pregnant during the observational period ().
During a median of 11.8 (3.4–44.5) months of follow-up, 176 (61.5%) experienced a complication to or progression of their disease necessitating acute or urgent intervention, of these, 73 (26% of the entire population) experienced cholecystitis, 46 (16%) experienced unremitting biliary colic, 33 (12%) experienced pancreatitis, 17 (6%) experienced CBD stones or ERCP without cholangitis or pancreatitis and 7 (2%) experienced cholangitis (). Gallstone-related complications were diagnosed at a median of 5 (IQR: 1.6–12) months after the index date. Six months after the index date, the cumulative risk of developing complications to the gallstones was 36% (95% CI: 30%–42%) increasing to 55% (95% CI: 48%–61%) at 12 months, and 81% (73%-86%) at 24 months (). Results of the crude and adjusted Cox proportional hazards regression analyses are listed in . Because of an exceedingly low number of patients with liver or bowel disease, we chose to exclude these variables from the analyses. In the Cox regression analysis for any gallstone-related complication, increasing age and increasing gallstone size were associated with a lower risk. In comparison, multiple gallstones were associated with a higher risk in crude analyses at a significance level of 10%. In the adjusted analysis, neither covariate was significantly related to gallstone-related complications.
Figure 2. Cumulative incidence of gallstone complications for individuals diagnosed with symptomatic, uncomplicated gallstone disease on the island of Funen in Denmark in the period 1 January 2020 to 1 July 2023.
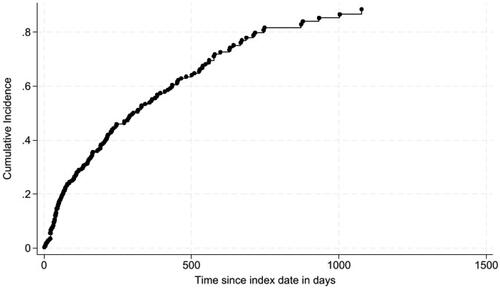
Table 1. Characteristics of individuals diagnosed with symptomatic uncomplicated gallstone disease on Funen from 1 January 2020 to 1 July 2023.
Table 2. Risk factors associated with any gallstone-related complication for patients with incident symptomatic uncomplicated gallstone disease on funen from 1 January 2020 – 1 July 2023.
Table 3. Risk factors associated with cholecystitis for patients with incident symptomatic uncomplicated gallstone disease on Funen from 1 January 2020 – 1 July 2023.
Table 4. Risk factors associated with common bile duct stones for patients with incident symptomatic uncomplicated gallstone disease on funen from 1 January 2020 – 1 July 2023.
When outcomes were stratified in cholecystitis and CBD stones (the latter including pancreatitis, cholangitis and CBD stones discovered on radiological examination and/or ERCP), male gender, increasing age and increasing gallstone size were associated with an increased risk of cholecystitis on crude analysis, while multiple stones increased the risk of CBD stones. Increasing gallstone size was associated with a lower risk of CBD stones. On adjusted analyses, only increasing gallstone size was associated with a lower risk of CBD stones (aHR = 0.89 (95% CI: 0.82–0.97), p < 0.01). In contrast, none of the examined covariates for cholecystitis were significantly associated with this outcome.
Five patients (2%) developed gallstone-related complications within 7 days of the index date. Excluding these patients did not materially affect the associations.
During follow-up, 85 (29.7%) patients underwent elective laparoscopic cholecystectomy. Intraoperatively, 34 (40%) had macroscopic signs of acute or chronic gallbladder inflammation. After elective laparoscopic cholecystectomy, 1 (1.2%) patient experienced a gallstone-related complication with a CBD stone three days after laparoscopic cholecystectomy. In two cases (2.3%), a gallstone-related complication was diagnosed on the day of elective cholecystectomy (one case of pancreatitis and one case of suspected CBD stone on intraoperative cholangiography).
Discussion
Symptomatic and uncomplicated gallstone disease has long been considered a relatively harmless condition with a low risk of developing complications [Citation6]. With this study, we found that a high proportion of patients referred to surgical counseling with abdominal pain from uncomplicated gallbladder stones progressed to cholecystitis, pancreatitis, or cholangitis after a median of five months, with four of five patients developing complications within two years of initial diagnosis of uncomplicated gallstone disease. This finding contrasts with earlier longitudinal cohort studies that report 1-3% [Citation7] annual progression rates. Several factors likely cause these differences in risk estimates and progression rates, most importantly population characteristics, where several risk factors for gallstone complications, such as high BMI and older age [Citation5, Citation8], are highly prevalent in this unselected, general Danish population. Many previous studies on the risk of complications to gallbladder stones are based on southern European populations [Citation9], where Mediterranean dietary habits and other lifestyle factors likely contribute to a low risk of progressing to complications.
Further to this, the spectrum of symptomatic uncomplicated gallstone disease is wide. It includes mildly symptomatic cases with little to no impact on quality of life and severely symptomatic cases necessitating specialist counseling, with the latter likely constituting most of our cohort. Our finding of macroscopic acute or chronic cholecystitis in 40% of patients undergoing elective laparoscopic cholecystectomy for uncomplicated gallstone disease is somewhat expected in an unselected population with uncomplicated gallstone disease since histopathological examination of gallbladder specimens following elective cholecystectomies in most cases shows signs of acute or chronic inflammation [Citation10,Citation11]. Although none of the patients undergoing elective laparoscopic cholecystectomy for uncomplicated gallstone disease in our study had any anamnestic or radiological signs of cholecystitis before surgery, this finding may also corroborate the observation that a general Danish population with gallstone disease should be considered at high-risk of complications. Unsurprisingly, our study’s risk of gallstone-related complications after elective laparoscopic cholecystectomy in our study was low at approximately 1% and underscores the potential of offering elective cholecystectomies to more patients earlier in their disease course to prevent gallstone-related complications.
A Norwegian randomized controlled trial [Citation1] of surgical versus expectant management of symptomatic uncomplicated gallstone disease found that non-surgical management was associated with an acceptably low risk of developing complications within a median follow-up of 67 months. However, the most recent follow-up of this cohort revealed that more than half of patients initially randomized to conservative management crossed over to surgery after 14 years of follow-up [Citation3]. Curiously, the risk of developing complications to gallstones in the study’s control arm was still significantly lower than in our study for patients with uncomplicated gallstone disease. This discrepancy may indicate a significant selection of patients in the randomized study.
A population-based cohort study from 2009 [Citation6] based on 793 patients with gallstone disease stratified patients into three groups: asymptomatic patients (73.1%), patients with mild symptoms (11.3%) and patients with severe symptoms (15.1%). After a median follow-up period of 8.7 years, 17% of patients with mild symptoms progressed to severe symptoms. The study concluded that expectant management represents a valid therapeutic approach in most patients. However, the cohort consisted of healthy subjects who underwent an ultrasound of the gallbladder and a questionnaire concerning abdominal symptoms, which potentially skewed the estimates toward a relatively low risk.
Our findings of an increased risk of CBD stones associated with multiple and small gallbladder stones are intuitive and corroborate the findings from previous studies [Citation12, Citation13]. Male gender, age and larger stones were positively associated with the development of cholecystitis. A study from 2011 reported similar findings, showing that male gender and age >50 years were significant risk factors for developing acute cholecystitis when diagnosed with gallbladder disease, with a 27% higher risk for males and 77% higher for patients with an age over 50 years [Citation8].
Results from our study can aid clinicians when counseling patients on the optimal approach to managing gallstone disease. Considering our findings, it could be relevant to offer preemptive elective cholecystectomies within a few months after diagnosis of gallstones to a higher extent than practised in this historical cohort and reserve expectant management to selected patients with an estimated low risk of developing complications. It is, however, relevant to underscore that we did not compare outcomes following cholecystectomy performed for complicated versus uncomplicated gallstone disease. If postoperative outcomes are similar, this would support expectant management as a feasible and safe approach. In fact, two recent randomized trials of conservative versus surgical management of symptomatic gallstone disease found that conservative management [Citation14] and a restrictive approach to offering laparoscopic cholecystectomies [Citation15] did not result in worse outcomes than standard elective laparoscopic cholecystectomy in terms of health-related quality of life and total costs to the healthcare system. The patients randomized in these trials were however also highly selected, as evidenced by inclusion rates of 16% [Citation14] and 48% [Citation15] respectively. Still, the results do indicate that the decision to undergo laparoscopic cholecystectomy should be individualized and based on a weighting of the risks of surgery against the potential risks of conservative management.
The strengths of this study lie in the use of prospectively maintained data from electronic hospital charts, where record linkage to hospital systems in other regions allows complete capture of data with low risk of attrition. Wide inclusion criteria and sampling from a large, unselected background population have minimized selection bias and increased transferability to areas with similar demographics.
The retrospective data collection meant that a significant proportion of data were missing for several covariates. These missing data impaired the robustness of both crude and adjusted analyses, potentially leading to a type 2 error in interpreting the results. Furthermore, missing data may have introduced a bias to the analyses if the ‘missingness’ was related to the outcome: Theoretically, data on BMI may have been missing for more patients who were obese, as they may have felt more reluctant to state their weight. As BMI was positively associated with the risk of developing CBD stones (although not at a statistically significant level), we may have underestimated the association of BMI with gallstone-related complications in our analysis. We sought to minimize this bias by imputing missing BMI values, but these imputed values may have been lower than the true values. The opposite scenario, where BMI was systematically missing for those with a normal BMI, is however also a possibility. Missing data on other covariates, e.g., gallstone size, were likely random and not associated with gallstone-related complications and were therefore unlikely to introduce bias. There is also a potential bias relating to misclassification of exposure, where patients who were current smokers or drank excessively categorized themselves as former smokers or with normal alcohol consumption, respectively. The paradoxical situation, with tobacco and alcohol use being systematically underreported for those with no use of tobacco or alcohol, is equally likely. Because there was no clear association between smoking history, or alcohol consumption, the direction or magnitude of such a bias is difficult to ascertain.
An additional, relevant perspective of surgical versus conservative management of uncomplicated gallstone disease is the economic aspect. We found that 61.5% of the patients who were not offered an elective surgery, experienced a complication and of these patients, 83.0% underwent an acute cholecystectomy. From a public health perspective, it would be relevant to estimate cost differences between acute and elective cholecystectomies. A qualitative study reported that patients with symptomatic gallstone disease experienced a significant increase in their quality of life after laparoscopic cholecystectomy [Citation16]. It is unlikely that conservative management in itself leads to increased quality of life, and up to one-fourth of patients managed expectantly have been found to regret their decision to not undergo surgery [Citation17]. A prospective cost-benefit analysis and qualitative comparison of conservative management versus surgery for symptomatic uncomplicated gallstone disease in addition to a comparative analysis of acute versus elective cholecystectomy in terms of postoperative morbidity seems warranted at this point.
Conclusion
In conclusion, we found that more than half of patients referred to surgical counseling for symptomatic, uncomplicated gallstone disease experienced disease progression necessitating urgent treatment within a year. Prospective studies are needed to identify risk factors for progression and to assess the efficacy and cost-benefit of early surgical intervention compared to conservative management in this patient population.
Authors’ contributions
NK, SKMR, SM, AK, and AMC contributed to the concept and design of the study. NK and SKMR collected data, which was analyzed by SM and AMC. All authors contributed to interpreting results, and NK and SKMR drafted the manuscript, which was reviewed and ultimately approved by all authors.
Dislosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Vetrhus M, Søreide O, Solhaug JH, et al. Liver and biliary tract symptomatic, non-complicated gallbladder stone disease. Operation or observation? Scand J Gastroenterol. 2002;37(7):834–839. doi: 10.1080/gas.37.7.834.839.
- Shabanzadeh DM, Christensen DW, Ewertsen C, et al. National clinical practice guidelines for the treatment of symptomatic gallstone disease: 2021 recommendations from the danish surgical society. Scand J Surg. 2022;111(3):11–30. doi: 10.1177/14574969221111027.
- 2021-22 UfF. Tidslinje over udviklingen og håndteringen af covid-191 2022Bilag 6:[Available from: https://www.ft.dk/samling/20211/almdel/ufo/spm/1/svar/1824050/2472975.pdf.
- Schmidt M, Søndenaa K, Vetrhus M, et al. A randomized controlled study of uncomplicated gallstone disease with a 14-year follow-up showed that operation was the preferred treatment. Dig Surg. 2011;28(4):270–276. doi: 10.1159/000329464.
- Yuan S, Gill D, Giovannucci EL, et al. Obesity, type 2 diabetes, lifestyle factors, and risk of gallstone disease: a mendelian randomization investigation. Clinical Gastroenterol Hepatol. 2022;20(3):e529–e537. doi: 10.1016/j.cgh.2020.12.034.
- Festi D, Reggiani MLB, Attili AF, et al. Natural history of gallstone disease: expectant management or active treatment? Results from a population-based cohort study. J Gastroenterol Hepatol. 2009;25(4):719–724. doi: 10.1111/j.1440-1746.2009.06146.x.
- Gutt C, Schläfer S, Lammert F. The treatment of gallstone disease. Dtsch Arztebl Int. 2020;117(9):148–158. doi: 10.3238/arztebl.2020.0148.
- Lee S, Chung CW, Ko KH, et al. Risk factors for the clinical course of cholecystitis in patients who undergo cholecystectomy. Korean J Hepatobiliary Pancreat Surg. 2011;15(3):164–170. doi: 10.14701/kjhbps.2011.15.3.164.
- Attili AF, De Santis A, Capri R, et al. The natural history of gallstones: the GREPCO experience. The GREPCO group. Hepatology. 1995;21(3):655–660. doi: 10.1002/hep.1840210309.
- Basak F, Hasbahceci M, Canbak T, et al. Incidental findings during routine pathological evaluation of gallbladder specimens: review of 1,747 elective laparoscopic cholecystectomy cases. Ann R Coll Surg Engl. 2016;98(4):280–283.
- Benkhadoura M, Elshaikhy A, Eldruki S, et al. Routine histopathological examination of gallbladder specimens after cholecystectomy: is it time to change the current practice? Turk J Surg. 2019;35(2):86–90. doi: 10.5578/turkjsurg.4126.
- Diehl AK, Holleman DR, Jr, Chapman JB, et al. Gallstone size and risk of pancreatitis. Arch Intern Med. 1997;157(15):1674–1678. doi: 10.1001/archinte.1997.00440360088009.
- Venneman NG, Buskens E, Besselink MG, et al. Small gallstones are associated with increased risk of acute pancreatitis: potential benefits of prophylactic cholecystectomy? Am J Gastroenterol. 2005;100(11):2540–2550.
- Ahmed I, Hudson J, Innes K, et al. Effectiveness of conservative management versus laparoscopic cholecystectomy in the prevention of recurrent symptoms and complications in adults with uncomplicated symptomatic gallstone disease (C-GALL trial): pragmatic, multicentre randomised controlled trial. BMJ. 2023;383:e075383. doi: 10.1136/bmj-2023-075383.
- van Dijk AH, Wennmacker SZ, de Reuver PR, et al. Restrictive strategy versus usual care for cholecystectomy in patients with gallstones and abdominal pain (SECURE): a multicentre, randomised, parallel-arm, non-inferiority trial. Lancet. 2019;393(10188):2322–2330.
- Atif QAA, Khan MA, Nadeem F, et al. Health-related quality of life after laparoscopic cholecystectomy. Cureus. 2022;14(7):e26739. doi: 10.7759/cureus.26739.
- L. Erritzøe FH. ‘Watchful waiting’ strategi af ukompliceret galdesten er ikke uden omkostninger. Dansk Kirurgisk Selskab. 2023.