ABSTRACT
Cardiac hypertrophy can be appreciated microscopically by assessing for myocyte hypertrophy. Features of myocyte hypertrophy include increased myocyte diameter, together with increase in nuclear hyperchromicity, size and irregularity, and an increase in binucleated myocytes. There is limited literature to demonstrate whether these features are uniform within the myocardium in the post mortem setting. This study compared the myocyte diameter, myocyte nuclear length, and proportion binucleated myocytes between the free wall of the left ventricle and interventricular septum in 21 post mortem cases. It showed regional variation in myocyte hypertrophy parameters between the free walls of the left ventricle and intraventricular septum. Over 75% of cases showed significant differences in myocyte nuclear length and myocyte diameter (ANOVA one-way, p < 0.05), whereas binucleated myocyte nuclei did not show any significant difference. The result of this study has implication in sampling and assessing myocyte hypertrophy. Further studies are recommended to explore the reasons why this variation occurred and whether it is clinically significant.
Introduction
Hypertrophy of the heart (or cardiac hypertrophy) is commonly encountered in both forensic and clinical pathology and is among others an anatomic finding which can be used to identify a cause of deathCitation1–3. Cardiac hypertrophy can be appreciated macroscopically and microscopically. Macroscopically, increased heart weight and increased dimensions, is considered the defining feature of cardiac hypertrophy with documented reference range(s)Citation3. However, heart weight is innately not reviewable after the post mortem examination and heart dimensions are unreliable when taken from a post mortem photographsCitation4. These short coming may be addressed microscopically by the assessment of myocyte hypertrophy (microscopic feature of cardiac hypertrophyCitation3,Citation5,Citation6, which is, despite being commonly assessed in post mortem examination, relatively understudied in the forensic pathology literature.
Myocyte hypertrophy is assessed by examining the myocyte size and nuclear featuresCitation3. It is diagnosed by an increased myocyte diameter, together with increase in nuclear hyperchromicity, size and irregularity, and an increase in binucleated myocytesCitation3,Citation5,Citation6. The only widely agreed threshold for myocyte hypertrophy is having a myocyte diameter of >15 µm, which needs to be validated using digital microscopyCitation3. It is suggested that measuring at least 100 randomly selected myocytes is required to have a reliable figure, without any further specifics on whether it can be measured at a single region of the heartCitation5,Citation6. However, there is no study that has investigated whether there is any regional variation in different areas of the heart.
This study, therefore, investigated whether there is any variation in three microscopic features used to diagnose myocyte hypertrophy (myocyte diameter, myocyte nuclear size/length, and binucleation) between the free walls of the left ventricle and the interventricular septum. Documenting any variation (or the absence of) would have implication on sampling and subsequent assessment of myocytes for hypertrophy in daily practice.
Materials and methods
A 2-year retrospective study was performed at Gold Coast University Hospital, Queensland, Australia (2021–2022 inclusive). Cases where an internal post mortem examination which sampled all the free walls (anterior, lateral, and posterior) and interventricular septum of the heart were included in the study. The age (years), sex (M or F), anthropometrics (height in centimetres/cm, and weight in kilograms/kg) and heart weight (in grams/g) were retrieved from the post mortem case files. The cause of death and cardiac pathologies listed were also recorded.
Exclusion criteria
Non-Caucasian population, due to limitations in ethics approval.
Paediatric population (less than 18 years old).
Cases with incomplete data set.
Suspicious and/or homicidal deaths due to potential legal implications.
Cases where previous heart surgery was performed due to altered anatomy.
Cases showing gross decomposition.
Heart weight
At post mortem examination, the heart was removed from the pericardial sac following the European guideline published in 2017Citation7. Due to individual practice preferences, not all hearts were weighed dissected as recommended in the very recent literature Citation8–10. As broad delineators, a heart weight of >400 g and >500 g in females and males respectively were considered as having an increased heart weightCitation3,Citation11,Citation12.
Myocyte hypertrophy
For each case, the anterior, lateral, and posterior free wall of the left ventricle and interventricular septum were individually sampled fresh along the short axis plane at the mid ventricular level during post mortem examination for diagnostic purposes. This was performed by qualified forensic pathologist(s). These samples were placed into histology cassettes and immersed in 10% buffered formalin shortly after the conclusion of the post mortem examination. The right ventricle was not examined (despite routinely sampled) as, in the authors experience, most myocyte hypertrophy assessment in forensic pathology casework is in the left ventricle. No sections were retained for further examination/research in formalin stock jars.
The samples were processed by a National Association of Testing Authority (NATA, Australia) accredited local histopathology laboratory They were embedded into a standard paraffin block, sectioned to 3 µm thick, stained with haematoxylin and eosin, and viewed using a calibrated microscope with 40× magnification objective (high power field). For each section, the site where it was sampled was cross checked by the histology blocking sheet and confirmed by histological features of the section (i.e. prominent papillary muscle in the anterior wall, lack of papillary muscle in the lateral wall, less prominent papillary muscle in the posterior wall, and lack of epicardial fat and presence of endocardium in the interventricular septum). A random area that showed the myocyte sectioned longitudinally, and away from focal pathology and intramural blood vessels was selected to maximize myocyte visualization. The area chosen within the slide was random, but commonly in the middle of the myocardial wall.
For the area chosen for each section, a digital image was acquired through a Nikon Eclipse Ci microscope with Plan Fluor 40× objective (Nikon Corporation, Japan). The digital image was captured using a MIchrome 20 digital camera and analysed using Mosaic 2.3 (Tucsen, China). The images were randomized and an assessed by a qualified forensic pathologist with more than 5 years’ experience who did not undergo the post mortem examination and blinded by the post mortem information. Multiple raters and multiple rating were not undertaken due to previous study showing a high inter and intra rater reliability in myocyte binucleationCitation13.
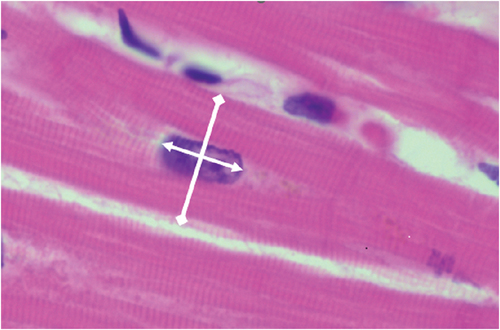
Using the digital image, the myocytes where the nuclei were clearly visible and at the centre of the myocyte were assessed. The longitudinal nuclear length (myocyte nuclear length) and transverse width of the myocyte at the cross section of the nucleus (myocyte diameter) were measured for each myocyte illustrated (). To access binucleation, the total number of myocytes on the field and the number of myocytes showing binucleation (≥2 nuclei) were counted similar to a previous studyCitation13,Citation14. Nuclei hyperchromicity and irregularity (or squaring) were not assessed due to potential variation in baseline staining intensity between each case, autolysis resulting in loss of staining and higher subjectivity.
Statistical analysis
Statistical analysis was performed using packages in R (open source, R studio 2022.07.01, Build 554, R version 3.6.3, using inbuilt statistic commands statistical analysis). A p-value of <0.05 was considered significant.
For summary statistics, continuous variables were presented as mean, median, minimum, maximum and standard deviation (s.d). Discrete variables were represented as counts.
For comparative statistics, for each case, one-way ANOVA (followed by post hoc Tukey) and Chi-square exact tests were used to explore whether there was any variation in continuous variable (myocyte diameter and myocyte nuclear length) and categorical (proportion of binucleated myocytes), respectively. The null hypothesis was that there would be no variation in myocyte diameter, myocyte nuclear length and proportion of myocyte binucleation within different areas of one heart.
Ethics
This study was approved by the Forensic Scientific Services Human Ethics Committee (HEC 22–18).
Results
During the study period, approximately 1000 cases were admitted to the department in which 21 cases were included in the study period. Many cases which had undergone internal post mortem examination were strictly excluded due to a lack of sampling of all the free wall of the left ventricle and intraventricular septum. The number of cases (n > 12) was considered sufficient for a pilot/exploration studyCitation15.
Sample population characteristics
The mean age was 47 years (min: 25, max: 83, median: 48, s.d: 14.7) and a male predominance (male:female = 17:4), and no case was identified as transgender/other. The mean weight and height were 173 cm (min: 158, max: 190, median: 174, s.d: 9.4) and 84 kg (min: 50, max: 124, median: 87, s.d: 19.2) respectively. Four cases were considered sudden cardiac death (ischaemic heart disease), and 17 cases were non-sudden cardiac death (seizure, infection/sepsis, pulmonary thromboembolism, asthma, complications of malignancy, haemorrhage related, drugs and alcohol related, drowning and asphyxia).
Heart weight and heart pathology
The mean heart weight was 431 g (min: 210, max: 655, median: 410, s.d: 110.0). Eight cases were considered to have macroscopic cardiac hypertrophy (heart weight >400 g in female, or > 500 in male). Five cases had at least one coronary artery showing severe atherosclerotic narrowing, and five cases had microscopic ischaemic changes (acute/subacute/remote myocardial infarction). The hearts of nine cases were considered normal (no evidence of macroscopic cardiac hypertrophy, less than severe coronary artery atherosclerosis, and no pathology in the myocardium).
Myocyte hypertrophy variations
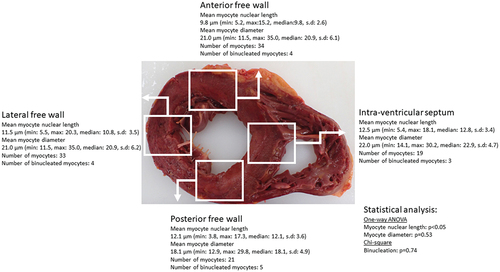
The mean number of myocytes examined for each case was 110 (min: 61, max: 230, median: 105, s.d: 37.5). An illustration on how each case was analysed is shown in .
Figure 2. An illustration of statistical analysis for each case this case was a death from non-cardiac cause and the heart had cardiac hypertrophy (heart weight >600 g) without severe coronary artery atherosclerosis and other pathology. There was significant difference (ANOVA one-way p < 0.05) myocyte nuclear length only between the areas sampled. It is noted the mean myocyte diameter were above 15 µm in over 100 myocytes. The deidentified photograph is for illustration purposes and is not from the aforementioned case.
In the cases examined, only one case showed no significant difference in the three myocyte hypertrophy parameters between three free walls and intraventricular septum. This case had underlying ischaemic heart disease (severe coronary artery atherosclerosis and microscopic ischaemic changes but did not have macroscopic cardiac hypertrophy).
For myocyte nuclear length, 18 out of 21 cases (86%) showed significant difference between the three free walls and intraventricular septum (ANOVA one-way, p < 0.05). In the three cases showing no significant difference, two were normal hearts and the other one had ischaemic heart disease (same case described in the previous paragraph).
For myocyte diameter, 16 out of 21 (76%) cases showed significant difference between three free walls and intraventricular septum (ANOVA one-way, p < 0.05). In the five cases showing no significant difference, two cases had normal hearts, two cases had macroscopic cardiac hypertrophy with no other cardiac pathology and one case had ischaemic heart disease (again, same case described in the previous paragraph).
Post hoc Tukey test did not show any general bias to any particular region of the heart for both myocyte nuclear length and myocyte diameter (i.e. there is no one region consistently showing significant difference).
For myocyte binucleation, all cases showed no significant difference between three free walls and intraventricular septum (Chi-square, p = 0.15–0.98).
Discussion
This study showed regional variation in myocyte hypertrophy parameters between the free walls of the left ventricle and intraventricular septum. Over 75% of cases showed significant differences in myocyte nuclear length and myocyte diameter, whereas binucleated myocyte nuclei did not show any significant difference.
Cardiac hypertrophy can be used to identify a cause of death and it is critical to correctly diagnose it. Histologically, cardiac hypertrophy can be assessed by myocyte hypertrophyCitation3,Citation5,Citation6. The presence of myocyte hypertrophy is routinely assessed in post mortem examination when sections of the heart are takenCitation1,Citation2,Citation16,Citation17. Myocyte hypertrophy is diagnosed by increase in cardiac myocyte diameter, together with nuclei that are increased in size, irregularity and hyperchromicity, and increased DNA ploidy (binucleation)Citation3. However, in the authors experience, it is common to see post mortem reports recording myocyte hypertrophy as a generalized comment without much specification where this was observed (apart from adjacent to focal pathology or in hypertrophic obstructive cardiomyopathy), what myocyte features were involved, and lacking quantification. Even when a pathologist decides to describe and quantify myocyte hypertrophy, the only widely agreed threshold is having a myocyte diameter of >15 µm which is currently unvalidated in the post mortem settingCitation3,Citation5,Citation6. It is suggested for myocyte diameter, measuring at least 100 randomly selected myocytes is required to have a reliable figureCitation3,Citation5,Citation6, without any further specifics on whether to sample one or multiple regions. A recent single centre preliminary study suggested counting binucleation is a reproducible and repeatable method which is associated with increased heart weight but did not address any potential regional variationsCitation13,Citation14.
In the post mortem examination context, it is reasonable to assume that myocytes are globally and uniformly hypertrophied or normal in the left ventricle and intraventricular septum (apart from focal pathologies). Thus, features used to assess myocyte hypertrophy should demonstrate relative uniformity in all areas/regions. However, there is no evidence to support this assumption, and to the best of our knowledge, no post mortem studies have ever investigated whether regional variations exist. This study showed that only one (nuclear binucleation) out of the three parameters studied showed overall no significant difference between the regions sampled.
The reason for the variations in myocyte nuclei length and myocyte diameter may be multiple. Although it could be due to innate variation in these parameters, the post mortem nature, the process used to obtain these sections, and the reliability in assessment may also provide some explanations. In the post mortem setting, the effects and possible uneven breakage of rigour mortis may account for the change of dimensions of the myocytes. During evisceration, examination, dissection, and sectioning without fixation may subject the heart to different amount and type of force (tensile/compression) which may again alter the microscopic dimensions of the myocytes. This would need further investigation, probably in using animal models by obtaining and fixing the whole heart immediately after death and before dissection. Furthermore, the variation may be due to the reproducibility of the measurements (i.e. inter and intra rater reliability) and can be further investigated by multi raters and muti rating of the sections. For myocyte binucleation, this study showed no significant regional difference. Binucleation is a process where myocytes transitions from mononucleate to a mature binucleate phenotype in which binucleation is a terminally differentiated cell that is unable to proliferateCitation18. Given the pathophysiology, it is probable that myocyte binucleation is more robust to post mortem changes and examination technique, thus showing less detectable regional variation
The result of this study showed significant regional variation in myocyte hypertrophy parameters and has implications in assessing myocyte for hypertrophy, and subsequent cardiac hypertrophy in the post mortem setting. Despite having a suggested threshold in literature, myocyte nuclear length (size) and myocyte diameter varies between regions which may render the diagnosis of myocyte hypertrophy unreliable depending on the region sampled and favour for a histological diagnosis by using more than one pre-selected area within the left ventricle. Myocyte binucleation appeared to be less variable, however, there is no widely agreed threshold. Further study is needed in the post mortem population to clarify whether the observed regional differences are clinically significant and to establish a robust method in assessing myocyte for hypertrophy and corresponding thresholds, with the addition of the right ventricle. Despite being a reviewable method, this study demonstrates that myocyte hypertrophy can exhibit high regional variation in the post mortem setting, thus great caution is needed to use it as a determinate for cardiac hypertrophy.
Limitation
Investigating regional variation and not establishing thresholds
The aim of this study was to investigate whether there is any regional variation in myocyte nuclei length, myocyte diameter and myocyte binucleation, and not to establish any reference range or threshold in the post mortem population. Unless the regional variations can be controlled for in the post mortem setting, it may be challenging in establishing a normal range, especially for myocyte nuclei length and myocyte diameter. It is possible that these variations are only statistically and not clinically significant. This study does not have sufficient sample size to clarify this and would require further and larger studies. The data collected in this study can potentially be used in future studies to establish a threshold for myocyte hypertrophy.
Study population and using heart weight as an indicator of macroscopic cardiac hypertrophy
Apart from being a single centre study, the cases were exclusively adult Caucasians due the limitation in ethics approval. It is probable the variations would also be observed in other ethnic groups.
The definition of increased heart weight was based solely on recommended thresholds (i.e. height and weight) to characterize the study population. There was no further sub-analysis between hearts that were categorized as cardiac hypertrophy or not, thus would not affect the overall results of this study.
Microscopic features myocyte hypertrophy
This study only used three parameters to assess myocyte hypertrophy in the left ventricle. Nuclear hyperchromicity and irregularity/squaring were not assessed for reasons mentioned above. It is possible that these features may show no statistical difference between different regions of the heart, but in our opinion would be technically hard to quantified/assess. The right ventricle was not examined in this study, as the left ventricle is more commonly assessed in the forensic post mortem examination.
Acknowledgments
This study was dedicated to the late Associate Professor and Eminent Pathologist, Alex Olumbe who left in peace during the conception of the project. His presence, friendship, proud Kenyan heritage, dedication to forensic pathology, generosity, kindness, unique and colourful dress sense, contagious smile, laughter and sense of humour will be enormously missed.
The authors would also like to thank administrative staff (Cassey May Dawson and Amanda Thorley), forensic pathology technicians (Kristian Knight, Nicky Rogers and Tanya Rancic), Forensic Scientific Services Human Ethics Committee (Kate Angus and Helene Jacmon), and Department of Anatomical Pathology, Pathology Queensland Gold Coast Group for their assistance.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Dolinak D, Matshes E, Lew E. Forensic pathology. Murlington MA: Elsevier; 2005.
- Saukko P, Knight B. Knight’s forensic pathology. 4rd ed. Boca Raton: CRC Press, Taylor & Francis Group; 2015.
- Basso C, Michaud K, d’Amati G, Banner J, Lucena J, Cunningham K, Leone O, Vink A, van der Wal AC, Sheppard MN, et al. Cardiac hypertrophy at autopsy. Virchows Arch. 2021;479(1):79–94. doi:10.1007/s00428-021-03038-0
- Gadsby Z, Martin J, Thompson M, Ondruschka B, Da Broi U, Tse R. Cardiac dimensions measured from post-mortem photographs: are they accurate? Aust J Forensic Sci. 2023;1–9. doi:10.1080/00450618.2023.2283414
- Sheppard MN. Practical cardiovascular pathology. 2nd ed. London: Hodder Arnold; 2011.
- Sheppard MN. Approach to the cardiac autopsy. J Clin Pathol. 2012;65(6):484–495. doi:10.1136/jclinpath-2011-200366
- Basso C, Aguilera B, Banner J, Cohle S, d’Amati G, de Gouveia RH, di Gioia C, Fabre A, Gallagher PJ, Leone O, et al. Guidelines for autopsy investigation of sudden cardiac death: 2017 update from the association for european cardiovascular pathology. Virchows Arch. 2017;471(6):691–705. doi:10.1007/s00428-017-2221-0
- Lohner L, Sinning C, Suling AI, Tse R, Garland J, Ondruschka B. Heart weight must not be measured before dissection during autopsies. Int J Legal Med. 2023;137(6):1751–1755. doi:10.1007/s00414-023-03089-9
- Loper N, Garland J, Ondruschka B, Glenn C, Kesha K, Stables S, Tse R. Significant differences in postmortem heart weight before and after dissection using the short-axis dissecting method. J Forensic Sci. 2020;65(5):1563–1567. doi:10.1111/1556-4029.14451
- Garland J, Kesha K, Glenn C, Morrow P, Stables S, Ondruschka B, Lohner L, Tse R. The effects of drying the rinsed dissected heart on postmortem heart weight. J Forensic Sci. 2022;67(1):251–256. doi:10.1111/1556-4029.14858
- Molina DK, DiMaio VJ. Normal organ weights in men: part i-the heart. Am J Forensic Med Pathol. 2012;33(4):362–367. doi:10.1097/PAF.0b013e31823d298b
- Molina DK, DiMaio VJ. Normal organ weights in women: part i-the heart. Am J Forensic Med Pathol. 2015;36(3):176–181. doi:10.1097/PAF.0000000000000174
- Gadsby Z, Garland J, Martin J, Thompson M, Ondruschka B, Da Broi U, Tse R. Validating counting binucleated myocytes: addendum to “Binucleated myocytes and heart weight: a preliminary study linking cardiac hypertrophy and myocyte hypertrophy”. Am J Forensic Med Pathol. 2023;44(4):362–363. doi:10.1097/PAF.0000000000000892
- Gadsby Z, Garland J, Thompson M, Ondruschka B, Da Broi U, Tse R. Binucleated myocytes and heart weight: a preliminary study linking cardiac hypertrophy and myocyte hypertrophy. Am J Forensic Med Pathol. 2023;44(4):273–277. doi:10.1097/PAF.0000000000000869
- Lewis M, Bromley K, Sutton CJ, McCray G, Myers HL, Lancaster GA. Determining sample size for progression criteria for pragmatic pilot rcts: the hypothesis test strikes back! Pilot Feasibility Stud. 2021;7(1):40. doi:10.1186/s40814-021-00770-x
- Dettmeyer RB. Forenisc histopathology: fundementals and perspectives. Verlag Berlin Heidelberg: Springer; 2018.
- DiMaio V, DiMaio D. Forensic pathology. 2nd ed. Boca Raton, Florida: CRC Press; 2001.
- Li F, Wang X, Capasso JM, Gerdes AM. Rapid transition of cardiac myocytes from hyperplasia to hypertrophy during postnatal development. J Mol Cell Cardiol. 1996;28(8):1737–1746. doi:10.1006/jmcc.1996.0163