ABSTRACT
This research introduces and validates the Comprehensive Model of Vaccination Intention (CMVI) to offer a holistic understanding of COVID-19 vaccination uptake in New Zealand. The CMVI excels by presenting a highly explanatory model, incorporating trust in the government's vaccination policy along with and a spectrum of social, cognitive, contextual, and affective variables from theories of Interpersonal Behavior, Planned Behavior, and Health Belief Model. A nationally representative sample of 993 participants was analyzed using confirmatory factor analysis and structural equation modeling. The findings underscore the positive impact of subjective norms and societal perceptions of vaccination, attitude toward vaccination, trust in government, and vaccination habits on COVID-19 vaccination intention. This study highlights the importance of normalizing vaccination to boost intention and shows how emotions shape attitudes. It also finds that better vaccine accessibility and trust in the government lower perceived costs and raise perceived benefits, improving overall attitude and strengthening vaccination intention.
Introduction
The COVID-19 pandemic is one of the most significant public health crises in recent history (Rahmani et al., Citation2021). The virus spread rapidly around the globe, with a surge in hospitalizaztions and lockdowns. The unprecedented disruption from COVID-19 led to a race to develop a safe and efficient vaccine to reduce severe forms of sickness, therefore reducing the toll on healthcare systems and the avoidance of lockdowns. The urgency of the need for a vaccine led to one of the fastest rollouts of a vaccine campaign in history in high-income nations (Glassman et al., Citation2022). Despite the significance of the vaccine for individuals and the collective, enacting mass vaccination campaigns and communicating effectively posed significant challenges for authorities as they grappled with public concerns over the speed of vaccine development and the rise of misinformation on social media (Lazarus et al., Citation2022), leading to a rise in vaccine hesitancy (Loomba et al., Citation2021). To respond to the COVID-19 threat and similar health crises, authorities need to know what factors impact vaccine intention. Combining elements from the Theory of Interpersonal Behavior (TIB), the Health Belief Model (HBM), and the Theory of Planned Behavior (TPB), this research uses an integrated model to investigate which major factors explain the intention to vaccinate among New Zealanders. Particularly, this study offers a distinctive perspective on COVID-19 vaccination by examining how trust in the government’s vaccination program along with social, cognitive, contextual, and affective variables from these three theories influence the intention to receive the COVID-19 vaccine. The model uniquely explains 80 percent of the variance. Empirically, this framework can be helpful in formulating effective communication strategies. Sharing research results from investigating New Zealand’s unique national context could contribute to insights that aid in developing effective prevention and treatment procedures elsewhere.
The concept of vaccine hesitancy has received much attention in health communication research (Ashwell et al., Citation2022). As the SAGE Working Group on Vaccine Hesitancy concludes, vaccine hesitancy can be defined as a ‘delay in acceptance or refusal of vaccination despite the availability of vaccination services’ (MacDonald, Citation2015, p. 4163). The reasons behind vaccine hesitancy are complex, and vaccine-hesitant individuals can sit on a continuum from accepting some vaccines and refusing others to an outright denial of all vaccines. Declared by the World Health Organization (WHO) as one of the greatest threats to global health in 2019 (World Health Organizatoin, Citationn.d.), vaccine hesitancy was exacerbated during the rise of COVID-19 when misinformation spread quickly on social media (Troiano & Nardi, Citation2021). Understanding what elements influence vaccine hesitancy necessitates further investigating vaccine intention, as vaccine hesitancy and vaccine intention are part of a continuum of responses to vaccination campaigns. Previous research has revealed a number of different factors that feed into the intention to vaccinate, such as politicization (Ward et al., Citation2020), socio-political factors and trust (Baumgaertner et al., Citation2018), vaccine-related attributes, such as efficacy, duration, and adverse effects (Pogue et al., Citation2020), demographic factors, such as age, education level, ethnicity and employment status (Troiano & Nardi, Citation2021), and religiosity (Olagoke et al., Citation2021). Previous research has shown that the factors influencing vaccination intention vary in their significance across different countries. Contributing to this variance is the way different authors use different measurements to examine vaccination intent. This variability has led some authors to propose models for measuring the factors that influence vaccine intention such as the HBM (Wong et al., Citation2020) and TPB (Shmueli, Citation2021). Although these models offer important insight, there is still the need for a more comprehensive model that incorporates the role of trust along with the affective, social, and cognitive factors in shaping vaccination intent.
To address this research gap, this study investigates factors that motivate vaccine intention. We apply a novel Comprehensive Model of Vaccination Intention (CMVI) based on the TIB, TPB, and HBM theories to a sample from the New Zealand population. New Zealand is an interesting case study as it began its vaccination campaign in February 2021, well after misinformation had taken hold. As an island nation, New Zealand’s response was to shut its borders to all but returning citizens and pursue an elimination strategy (Baker et al., Citation2020). An initial seven-week lockdown from 24 March 2020 and quarantine measures at the border enabled the government to eliminate the community transmission of COVID-19, allowing citizens to live free of the virus for several months. Compared to other countries, New Zealand was successful in keeping low levels of cases and deaths, recording only 1815 cases and 26 deaths by 13 February 2021 (Timeline - Coronavirus, Citation2023). Support for the elimination strategy was initially high, with 88% of the population supporting lockdown measures (Manhire, Citation2022a). The border closures meant the country had low levels of COVID-19 experience during the vaccination process compared to other countries with significant outbreaks and death tolls, but also misinformation had time to take hold. New Zealand was also unique in offering a single kind of vaccine – Pfizer.
Our study’s results can serve as a model for researchers and practitioners seeking to assess the complex factors that feed into the intention to vaccinate against COVID-19. This study extends the TIB model (Triandis, Citation1977) by incorporating trust and provides comprehensive insights into vaccination decision--making, contributing to the understanding of pandemic communicative practices (Dutta, Citation2022). It offers practical implications for public health interventions, aiding stakeholders in designing effective strategies to enhance vaccine uptake based on the proposed model. While this research is specifically on the New Zealand context, the model we develop may offer insight into vaccination intent when applied to other countries. Increasingly research in health communication regarding COVID-19 has shown that effective communication is critical in fostering trust, combating fear and misinformation, and promoting vaccine intention (Ashwell et al., Citation2022; Chou & Budenz, Citation2020; Corbu et al., Citation2021; Croucher et al., Citation2022; Li & Samp, Citation2022; Tong et al., Citation2022; Wright et al., Citation2022). Critical to vaccine intention is the link between behaviors and communication, which this study explicates.
Background
Achieving a high vaccination rate is crucial for reducing the severity of adverse health outcomes, stress on the health system (Conner & Norman, Citation2005). In the case of some infectious diseases, high vaccination levels can lead to ‘herd immunity,’ where the high percentage of people vaccinated shields others from catching the disease (Luyten et al., Citation2019). The urgency of the public health emergency presented by COVID-19 saw scientists around the world work quickly on developing a vaccine using the new messenger ribonucleic acid (mRNA) technology, where an enzyme primes the gene on how to respond (Pérez-Peña, Citation2020). Officials had to build public support for vaccination quickly against a backdrop of disrupted lives due to lockdowns and assuage the concerns of some over the fast pace of vaccine development and new technology. Exacerbating these concerns was the interplay of vaccination with public policy, where in some countries, vaccination was mandated for citizens to re-engage with their normal lives. In this environment, misinformation spreads quickly on channels such as social media, fueling hesitancy (Wilson & Wiysonge, Citation2020).
New Zealand’s approach to COVID-19 was relatively unique – being an island nation, they were able to shut the country’s borders to all but returning citizens and pursue an elimination strategy. Like many other countries, as the pandemic wore on, support for government measures such as vaccination became more fragmented. In early February in 2021, New Zealand approved the Pfizer/BioNTech vaccine for rollout as primary doses (Beehive.govt.nz, Citation2021). However, this vaccination rollout was blighted by a series of outbreaks largely based in Auckland that saw the city enter restrictions between August and December 2021, with a border staffed by police containing residents within the city. In late October 2021, the New Zealand government announced that regions around New Zealand would progressively shift to minimal restrictions and larger events as they reached the 90% vaccinated benchmark and entered a new ‘traffic light’ system (Cooke, Citation2021), which was achieved by 16 December. The ‘traffic light’ system also provided different levels of restriction to those who were vaccinated versus those who were not vaccinated, with entry to restaurants and bars restricted for those unvaccinated, as well as the number of people they could gather with (Cooke, Citation2021). While restrictions for the unvaccinated were eased on 4 April 2022 (Moodie, Citation2022), mandates for vaccination still existed if working in certain industries such as healthcare or education. The introduction of mandates stoked tensions for some groups who were hesitant or did not believe people should lose their jobs over being unvaccinated. As an Omicron outbreak in January 2022 led to a shift in government policy from elimination to ‘living with the virus,’ these tensions came to a head with localized protests on the lawns of Parliament House (Cornish & O’Dwyer, Citation2022).
Protests in New Zealand manifest vaccine hesitancy, driven also by less obvious factors like religious beliefs or distrust of health professionals (Ashwell et al., Citation2022). Increasing vaccine hesitancy can also be seen in the drop in booster uptake: only 73% of eligible people above 18 years old have had their first booster (COVID-Citation2023 data and statistics, Citation2023), and less than half of those eligible for a second booster have taken up this offer (Morton, Citation2023). Reduced vaccine uptake may stem from declining trust in the vaccine or government, the realization that the vaccine doesn’t halt transmission, or the absence of mandatory requirements for public activities. Understanding what shapes intention to get vaccinated is not only relevant for considering primary doses but also is helpful in encouraging people to get booster vaccinations for ongoing protection against COVID-19.
Vaccine hesitancy and intention
Vaccine intention and hesitancy sit on a continuum, and there is a complex range of reasons that can impact one’s intention to vaccinate (WHO, Citationn.d.; Troiano & Nardi, Citation2021). One might be hesitant to vaccinate against one infectious disease and not another, or one may falsely believe they are medically unable to get vaccinated (Ashwell et al., Citation2022). Reactions can range from mildly hesitant to anti-vaccination. Exposure to misinformation can reduce the intention to vaccinate (Loomba et al., Citation2021; Wiysonge et al., Citation2022) and increase distrust of healthcare workers and the ability for collective action on health emergencies. Existing research on COVID-19 vaccine intention has yielded contradictory findings regarding the determinants of decision-making processes surrounding vaccine uptake (Ashwell et al., Citation2022; Olagoke et al., Citation2021; Pogue et al., Citation2020; Troiano & Nardi, Citation2021; Ward et al., Citation2020). Acceptance rates for the COVID-19 vaccine differ across high-income countries, even when there are high rates of acceptance for other vaccines, meaning the results of COVID-19 research often differ from previous studies on viruses like influenza and HPV (Lazarus et al., Citation2022). While previous research elucidates some of the factors that feed into vaccine hesitancy, there is a need for the development of models that can account for the complex range of issues that affect the intention to vaccinate.
Health belief model
The HBM is a model that uses behavioral science to explain health behavior and decision-making. The HBM specifies six independent factors of behavior: (1) susceptibility to illness, (2) severity of illness, (3) costs of carrying out behavior, (4) perceived threat, (5) cues to action, and (6) benefits of action (Tawfiq et al., Citation2023). Previous research has applied the HBM (Rosenstock et al., Citation1988) as a useful theoretical behavioral change model in understanding the intention to vaccinate against COVID-19 (Wong et al., Citation2020) and influenza vaccine uptake among healthcare workers (Hopman et al., Citation2011; Shahrabani et al., Citation2009). The HBM relates health behavior to people’s specific beliefs, namely the perceived severity and susceptibility of the disease and the perceived benefits (i.e. health benefits) and risk of the vaccine (i.e. costs). Despite its popularity, the HBM has several shortcomings. For example, it does not consider people’s attitude or social and contextual elements that give rise to the intention to vaccinate. The HBM has also been criticized for its lack of causality and listing six independent variables (Armitage & Conner, Citation2000). Meta-analyses have shown that the mean effect sizes are statistically significant for costs and health benefits, but small for perceived severity, and that while the HBM is good at predicting retrospective behavior, it is not as accurate at predicting future behaviors (Harrison et al., Citation1992).
Theory of planned behavior
The TPB extends the HBM by including the individual’s perceived behavioral control and intention as key determinants of behavior. According to TPB, a person’s intentions to engage in behavior are influenced by their attitudes, subjective norms, and perceived behavioral control (Ajzen, Citation2002). Previously, TPB has been used to explain intention to vaccinate among student nurses (Cornally et al., Citation2013) and healthcare workers (Godin et al., Citation2010). Recent research into the COVID-19 vaccine combines the TPB with the HBM to model vaccination intent, including variables such as attitudes and the social elements of norms, and the contextual element of facilitating conditions (Shmueli, Citation2021). While the combined TPB-HBM model offers significant improvements on HBM in terms of causality and its ability to explain variance, it still does not consider important contextual elements such as habit (i.e. previous vaccination/health behaviors). The model has limitations (Moody et al., Citation2018) as its social component only considers subjective norms and does not account for other social factors, such as how an individual's behavior may be influenced by both their social network's perception of them, encompassing their social roles, and their own self-perception of social status.. Additionally, the model does not consider affect, which refers to an ‘emotional response to a particular situation that is based on instinctive and unconscious processes in the mind’ (Moody & Siponen, Citation2013). Social factors and affects seem particularly relevant to shaping vaccine intention for COVID-19, as the rollout of the vaccine and accompanying health measures has been affectedby misinformation that is often communicated emotionally across social networks (Chou & Budenz, Citation2020).
Theory of interpersonal behavior
The TIB suggests that to adequately explain behaviors, various social, cognitive, affective, and contextual elements should be considered (Triandis, Citation1977). According to Triandis (Citation1977), behavior is the result of an interaction among intention, habits, and facilitating conditions related to the behavior. The formation of intention within the TIB is a multifaceted process encompassing several key elements. These include attitude, which is characterized by a combination of belief and evaluation of an outcome. Additionally, affective factors play a crucial role in shaping intention, reflecting one’s emotional responses and moods in relation to the behavior in question. Furthermore, social factors are integral components, encompassing subjective norms, roles within one’s social context (defined by their social position), and self-concept, which pertains to an individual’s perception of the appropriateness of the intended behavior within their personal framework of values and identity. Together, these elements within TIB intricately contribute to the development of behavioral intention. Previous research shows that TIB is an appropriate theory to investigate medical student’s ethical decision-making (Li et al., Citation2020), physicians’ telemedicine adaptation (Gagnon et al., Citation2003), and American nurses’ decision to vaccinate against influenza (Johansen et al., Citation2012). TIB has demonstrated promising potential in explaining COVID-19 vaccination intentions, but it could be further improved by incorporating the role of trust in government. This addition could provide a more comprehensive understanding of the factors that influence vaccination behavior and strengthen the model’s overall efficacy. In this specific COVID-19 vaccination context, governments played a central role in distributing information on vaccination during the crisis due to the speed required for the vaccine rollout and the desire to end lockdowns. Moreover, a lack of trust in government has been shown to increase the likelihood of vaccine hesitancy or refusal (Trent et al., Citation2022). In sum, despite their common use in predicting health behavior, the TPB and HBM could be further complemented to better explain critical health behavior, particularly vaccine intention. In contrast, the TIB seems to be better at explaining health behavior; yet is lacking the critical component of trust in government. While there are many ways of conceptualizing trust, previous research on the H1N1 pandemic highlights that in health emergency situations where communications are centralized, trust in government and elected officials in providing accurate information has an important impact on vaccination intention (Jamison et al., Citation2019; Quinn et al., Citation2013). Therefore, the TIB can be further developed by the inclusion of trust in the vaccination policies of the government, which has proved to be an important variable in shaping individuals’ decision to vaccinate (Bollyky et al., Citation2022). Hence, a novel model of vaccine hesitancy is needed that captures a more holistic fulsome picture of the critical elements involved in predicting vaccination intention.
Model development
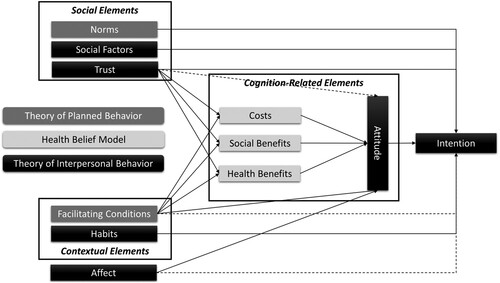
Our study introduces and empirically tests an innovative model that combines elements from the TIB, HBM, and TPB. CMVI aims to bridge these gaps and provide a more comprehensive framework for understanding Covid-19 vaccination intentions. CMVI proposes intention to vaccinate is influenced by (a) cognition-related elements, including attitude (which itself is shaped by cost and benefit), (b) affect, (c) social elements, encompassing social factors (the impact of one’s social relationships on vaccination intention), subjective social norms, and trust in government’s vaccination policies, and (d) contextual elements, including facilitating conditions and habit.
Extensive research has demonstrated the substantial impact of trust on various COVID-related behaviors and attitudes, including vaccination acceptance (Bollyky et al., Citation2022), compliance with social distancing measures (Fridman et al., Citation2020), and attitudes toward vaccines (Caso et al., Citation2022). It has also been used as a moderator and mediator in several HBM and TPB models exploring factors that influence COVID-related behaviors, attitudes, and communication (Barattucci et al., Citation2022; Liu et al., Citation2022; Plohl & Musil, Citation2021; Servidio et al., Citation2022; Siegrist & Zingg, Citation2014). In this study, we define trust in the government’s vaccination policies within a social context. In our conceptualization, trust refers to the perception of reliability and credibility attributed to entities like the government providing information or guidance. Here, trust focuses on the trustworthiness of the individuals or organizations offering information, rather than the trust placed directly in the information itself.
Expanding upon the theoretical frameworks of the TIB and HBM, we incorporate the TIB concept of costs and benefits concerning vaccination intention. We posit that the interplay between the perceived costs and benefits of vaccination significantly shapes one’s attitude toward vaccination. While attitude can encompass both cognitive and affective dimensions (Haddock & Maio, Citation2019), we are focusing on the cognitive aspect composed by the interplay of vaccination costs and benefits (Verhallen & Van Raaij, Citation1986). Moreover, by incorporating affect as an independent variable, operationlized in this context as negative–postive emotion (Moody & Siponen, Citation2013; Triandis, Citation1977), our model effectively mitigates the influence of affect on the intention to undergo vaccination. This underscores the study’s emphasis on cognitive facets of attitude, in contrast to the affective facets. Additionally, the incorporation of affect into our model aligns with the TIB and represents an enhancement compared to the HBM. While the HBM acknowledges the role of psychological variables, such as fear, in influencing perceptions related to healthcare behaviors, these elements do not hold a central position within this model. In contrast, TIB posits an individual’s affection or emotional disposition toward a behavior significantly shapes their intention to engage in that behavior (Triandis, Citation1977). Previous research shows that affect influences attitudes toward behaviors. Positive affect, such as hope and joy, fosters positive behavior and attitude, while negative affect, such as fear and shame, hinders them (Brooks et al., Citation2023; Heddy et al., Citation2017).
Moreover, in alignment with TPB, our model investigates the influence of attitude, subjective norms, and facilitating conditions on the intention to vaccinate. Facilitating conditions of getting vaccinated, as denoted in the TIB, shares notable similarities with the notion of perceived behavioral control in TPB and barriers in the HBM, as they all reflect internal and external factors (i.e. time-consuming and inconvenient) that may impact someone’s ability to perform a behavior (Ajzen, Citation2002). Facilitating conditions cover aspects such as the accessibility of healthcare, the availability of necessary equipment and supplies, which contribute to individuals perceiving health as a priority and actively engaging in behaviors that promote their well-being (Mannava et al., Citation2015; McIntyre et al., Citation2009). Additionally, previous investigations on Covid-19 vaccination in lower and lower-middle-income countries have revealed that facilitating conditions are pivotal in influencing healthcare providers’ attitudes toward telemedicine (Shiferaw et al., Citation2021).
Moreover, our model incorporates the influence of habitual behavior, particularly the habit of receiving previous vaccines, on individuals’ intentions to vaccinate against COVID-19. This inclusion aligns with the hypothesis proposed in the TIB and finds support in prior research. Earlier studies have consistently demonstrated a positive correlation between habits and the intention to engage in a particular behavior (Ouellette & Wood, Citation1998). The study model is presented in .
Method
After receiving ethics approval, we fielded a nationally representative Web-based survey from Qualtrics. Previous research has shown samples from data collection firms such as Qualtrics to be reliable and representative (Boas et al., Citation2020). The survey participants were randomly selected from a nationally representative group of adults aged 18 years and over living in New Zealand. The sample was matched to the NZ census for age, education, and sex. The survey was fielded from February to March 2022. To reduce systematic error variance and random noise and to provide more accurate and powerful tests (Meyvis & Van Osselaer, Citation2018), Qualtrics excluded speeders and participants who failed two attention tests. We received a complete sample of 993 participants (males = 480 (48.3%), females = 500 (50.4%), other = 13 (1.3%), 18 ≤ age ≥ 88, Mage = 39.35, SDage = 14.79, see ). In terms of age, the largest cohort falls within the 30–39 age group, comprising 28.8% of the sample. The 18–29 and 40–49 age groups contribute significantly as well, accounting for 27.7% and 25.8% of the participants, respectively. Individuals aged 50 and above constitute 17.7% of the sample. Also, participants with educational backgrounds below a high school diploma constitute 9.3% of the sample, while those with a high school diploma make up a substantial portion at 36.3%. The study includes individuals with diverse higher education achievements, with 44% holding a bachelor's degree, 8.9% having attained a master's degree, and 1.6% possessing a doctorate. Qualtrics provides financial compensation for participants upon completing the questionnaire. We did not exclude participants once we received the data set from Qualtrics.
Table 1. Demographic information of participants (N = 993) and included measurements.
Measures
Measurements included perception of vaccination benefit and cost, emotions, and mood toward vaccination (i.e. affect) and attitude, intention to vaccinate, vaccination habits, facilitating conditions for vaccination, and existing social norms, and trust and social factors. Current residence in New Zealand was the inclusion criterion. The details of the included scales are presented in .
Table 2. Included measurement scales.
Statistical analysis results
Factor analysis results
To investigate the validity of the measurements, we conducted confirmatory factor analysis (CFA) using AMOS (v26), which confirmed the factorial structure of the study via an excellent model fit: χ2 = 4161.328, DF = 1483, CFI = .953, TLI = .95, SRMR = .052, RMSEA = .043 and Pclose = 1 (Hair et al., Citation2014). The statistics obtained from the CFA were assessed in accordance with established thresholds for model fit. An excellent fit is indicated by values within the following ranges: CMIN/DF between 1 and 3, CFI > 0.95, SRMR < 0.08, RMSEA < 0.06, and PClose > 0.05. Alternatively, a fit is considered acceptable if it falls within the range of CMIN/DF between 3 and 5, CFI between .90 and .95, SRMR between .08 and .1, RMSEA between .06 and .08, and PClose between .01 and .05 (Hu & Bentler, Citation1999). These criteria provide a robust framework for evaluating the goodness of fit in our model. The details of CFA loadings are in .
Table 3. Validity and invariance measurements of the study models.
Validity and reliability analysis results
To investigate the discriminant and convergent validity of the data, the average variance extracted (AVE), √AVE, maximum shared variance (MSV), and maximum likelihood estimation of inter-construct correlation were calculated. AVE values were >.5, proving the resulted factors’ convergent validity. Also, for each factor, the √AVE was higher than the correlation of the factor with other included factors, and MSV was lower than AVE, which proves the discriminant validity of the factors (Hair et al., Citation2014). Also, the values of construct reliability, maximal reliability (MaxR(H)), and Cronbach α were calculated to test the reliability of the factors, which all were >.7; thus, the current measurements are reliable.
We used Structural Equation Modeling (SEM) to test the study hypothesis, which established an acceptable model fit χ2 = 4332.134, DF = 1448, CFI = .948, TLI = .945, SRMR = .076, RMSEA = .045, and Pclose = 1 (Hair et al., Citation2014). The details of the model fit, validity, and SEM measurements are presented in .
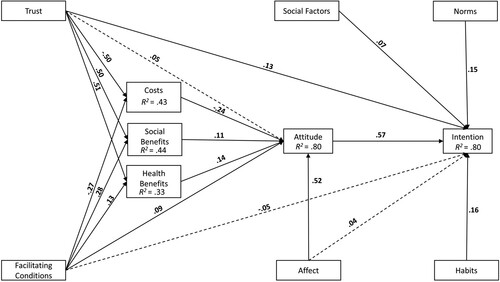
Path model results
The SEM model explained 80% variance in intention to vaccination with significant impact by attitude (βstandardized = .56, βunstandardized = .62, p < .001), trust (βstandardized = .13, βunstandardized = .15, p < .001), norm (βstandardized = .15, βunstandardized = .17, p < .001), social factors (βstandardized = .07, βunstandardized = .08, p < .05), and habit (βstandardized = .16, βunstandardized = .18, p < .001). The effects of facilitating condition on intention was insignificant (βstandardized = −.05, βunstandardized = −.06, p = .06), yet it significantly explained attitude (βstandardized = .09, βunstandardized = .1, p < .001). The effect of facilitating condition on attitude was partially mediated through cost (βstandardized = −.27, βunstandardized = −.16, p < .001), health benefits (βstandardized = .13, βunstandardized = .23, p < .001), and social benefits (βstandardized = .28, βunstandardized = .4, p < .001). The impact of affect on intention (βstandardized = .04, βunstandardized = .04, p = .31) was fully mediated by attitude (βstandardized = .52, βunstandardized = .54, p < .001). Along with affect, perceptions of social benefits (βstandardized = .11, βunstandardized = .08, p < .001), health benefits (βstandardized = .14, βunstandardized = .08, p < .001) positively, and costs (βstandardized = −.24, βunstandardized = −.41, p < .001) negatively explained 80% of variance in attitude. The impact of trust on attitude (βstandardized = .05, βunstandardized = .05, p = .08) was fully mediated positively by perceptions of social benefits (βstandardized = .51, βunstandardized = .70, p < .001), health benefit (βstandardized = .51, βunstandardized = .92, p < .001) and negatively by cost (βstandardized = -.50, βunstandardized = −.30, p < .001). Our model explained 44%, 34%, and 43%, respectively, in perceptions of social benefit, health benefit, and cost. The analysis results are presented in .
Discussion
This research proposed and validated CMVI to investigate COVID-19 vaccination uptake in New Zealand. Our proposed model attains significant theoretical achievements for several reasons. First, our model explained 80% of variance of vaccination intention in this nationally representative, cross-sectional survey. This finding underscores the imperative of adopting a more holistic approach that encompasses various individual, social, and political factors to understand vaccine intention. Also, our study utilizes a large sample size comparative to the overall population of New Zealand (5.084 million) and includes a nationally representative sample, allowing a more precise estimate of our effect and generalizability of our results. While further testing across different environments is needed to further verify the model, the results show that CMVI has the potential to inform public health communications and campaigns. Second, unlike other studies incorporating trust in the government, we investigated the effect of trust along with several other social, cognition-related, contextual, and affective elements of vaccination uptake and explained a high percentage of variance in the model. CMVI demonstrates that affect and cognition-related elements may have a significant impact on shaping vaccine intention. This is important as vaccine intention is often considered in models such as HBM and TPB as a rational decision.
Our results show trust in vaccination policies positively impacts the cognition-related elements – perceived costs and benefits (social and health) of the vaccine and indirectly affects attitude. While researchers have previously found that trust in the government impacts adherence to health guidelines (Quinn et al., Citation2013), this finding links trust in the government to positive vaccination intent (Bollyky et al., Citation2022; Larson et al., Citation2018). Previous studies in economics have shown the effect of trust on attitude is mediated by perceptions of costs and benefits (Moon & Balasubramanian, Citation2004). Integrated into our comprehensive model, we show that trust in government also has a considerable impact on intention to vaccinate by reducing perceived costs and perceived social and health benefits, which impacts attitude.
Additionally, the impact of facilitating conditions, such as the accessibility of vaccination clinics, on the intention to vaccinate was indirect. Nevertheless, they exhibited a robust positive influence on the perception of the social benefits of taking the vaccine, concurrently decreasing the perceived costs of vaccination. It also demonstrated a less pronounced positive effect on the perceived health benefits of vaccination. This supports the WHO’s definition of vaccine hesitancy as being influenced by convenience, which refers to how easy the vaccine is to access and how much it costs (Troiano & Nardi, Citation2021).
Our findings also show affect, or the emotions and mood toward vaccination, has a significant effect on attitudes toward vaccination and an indirect effect on intention. Vaccination has long been an emotional issue in many countries, and anti-vaccination campaigns draw heavily on emotion (Chou & Budenz, Citation2020). Moreover, affect plays an essential role in communications campaigns, many of which are influenced by inoculation theory, which, through preemptive exposure to weakened forms of persuasive arguments, aims to bolster individuals’ resistance against subsequent, more potent persuasive attempts such as misinformation, thereby motivating citizens to take desired actions (van der Linden et al., Citation2020). Research has also shown that emotion is a vital factor for healthcare workers in recommending vaccination (Ledda et al., Citation2021).
Finally, the study emphasizes the significance of normalization and habitualization of vaccination to increase the intention to vaccinate against future incidents of viral diseases. This finding is in accordance with previous studies showing vaccination habits and positive social attitude toward vaccination could determine the decision to vaccinate (Maridor et al., Citation2017). However, it is worth noting that despite routine vaccination habits and positive social attitudes toward vaccination, various factors, which may vary across different countries, could influence individuals’ decisions, and further investigation into these specific contextual elements is warranted.
Implications for practice
These findings have significant implications for public health stakeholders and practice. The study showed how building confidence in government trust and performance is critical to shaping the perception of the costs and benefits of vaccination. Building trust early as an initial response to new pandemics may have ongoing benefits that last much longer after a vaccine has been developed, even after this initial trust begins to wane due to crisis fatigue or misinformation. For instance, New Zealand was unique globally for maintaining high trust in the government’s COVID-19 measures. A global Gallup Poll in late 2020 showed trust in scientists was also high, with 63% of New Zealanders reporting they trusted scientists compared to the global average of 41% (McClure, Citation2022). While this perception of performance (governance trust) had dropped to 66% at the time this survey was taken (Manhire, Citation2022b), the initial trust built benefited vaccination uptake (90% of the population over the age of 12 years old received their primary dose) (COVID-Citation2022: Vaccine data, Citation2022). The high rates of vaccination New Zealand recorded once it undertook its mass vaccination campaign signals that building popular consensus at the outset of the outbreak may also have an inoculating effect against misinformation for some. Overall, our findings show building confidence in government trust and performance is critical to shaping the perception of the costs and benefits of vaccination and vaccine intention. This may be relevant for other countries when planning their health responses.
Also, the impact of facilitating conditions on the perception of the cost and benefit of vaccination might be explained by the way access to COVID-19 vaccines was much easier than other vaccines available in New Zealand, such as the influenza vaccine. The influenza vaccine costs at least $20 per dose, unless people fall into a vulnerable group, or the vaccine is covered by the employer (Edwards, Citation2022). For COVID-19, vaccination clinics were available across New Zealand, and the country even ran a nationwide vaccine event called ‘Super Saturday.’ Employers were encouraged in briefings from the Director General of Health and the Prime Minister to take paid time off work to get the COVID-19 vaccine. Some vaccination centers incentivized people to get the vaccine with the provision of free food or vouchers (Ling, Citation2022). This was accompanied by a significant media push to get vaccinated through government updates and advertising. These incentives and the support from employers potentially contributed to the perceived reduction in costs. The perceived social benefits may have also been stimulated by vaccine mandates in New Zealand. This impacted the numbers allowed in cafes and restaurants and the ability to work in certain frontline roles (such as health, aged care, and teaching). This created resistance from some who did not want to be vaccinated and an environment where vaccination was framed as the key to maintaining a normal life and social benefits.
Overall, moving forward, policymakers in the future can employ the research insights to shape targeted interventions, invest in trust-building measures, communicate both social and health benefits, and address perceived costs. These findings can also inform public health practitioners to develop and implement relevant communication strategies by incorporating localized and socially sensitive approaches. Training programs for healthcare providers should be implemented to enhance their ability to address vaccine hesitancy concerns and effectively communicate the safety and benefits of COVID-19 vaccines.
Also, our results show affect has a considerable impact on attitudes to vaccination intention. This finding underscores the need for tailored communication strategies in public health campaigns. Policymakers should acknowledge and address the emotional dimensions surrounding vaccination by integrating emotional impact assessments into vaccination campaign evaluations (Chou & Budenz, Citation2020) and considering the emotional nature of anti-vaccination campaigns (van der Linden et al., Citation2020). Also, healthcare worker training programs should enhance emotional intelligence to leverage their crucial role in positively shaping public attitudes (Rossettini et al., Citation2021). Targeted communications campaigns that enhance the positive affects of citizens are also a critical component in fighting vaccine hesitancy. Collaboration with community leaders might be a helpful venue, as they can help mitigate negative emotions and create more trust, which enhances vaccine take-up overall.
Eventually, the significant impact of habit on intention to vaccination implies building up narratives about vaccination as a social responsibility and promoting vaccinations against endemic and seasonal diseases such as influenza by making vaccines free of charge or more accessible can boost the intention to vaccinate against diseases in the future.
Future research directions
This study has some limitations that offer opportunities for future research. First, since our data was cross-sectional, we could not control for unobserved confounding factors such as personality traits or medical preconditions. Thus, randomization or elimination of stable confounding variables was impossible. Our data demonstrates vaccine intention for this moment in time. Future research might want to use longitudinal data to verify our results over a longer time. Second, we developed and tested a model based on TIB, TPB, and HBM variables, which achieved high predictive values. However, other behavioral theories such as the protection motivation theory and the cognitive model of empowerment, could serve as a base for understanding COVID-19 vaccination intention. Also, there is a debate amongst scholars on the relationship between attitude, cognition, and affect. Future research might want to investigate different configurations of the relationships between those key constructs. Third, our model is specific to COVID-19, which limits the applicability of these results to other vaccines. As the results of vaccine intention may differ across different vaccines like influenza and HPV, our model cannot be transferred to different vaccines without additional testing. Last, part of our model investigates trust and its impact on Intention to vaccinate. Importantly, political polarization and misinformation is influencing trust in government globally. This is an important development, and future research should further look at the impact of misinformation in the context of trust and vaccine intention. This opens a great opportunity for future research to apply and test CMVI to different vaccines. Also, to ensure its generalizability to other countries, future research should further test our model across countries with different social and economic structures.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Ajzen, I. (2002). Perceived behavioral control, self-efficacy, locus of control, and the theory of planned behavior. Journal of Applied Social Psychology, 32(4), 665–683. https://doi.org/10.1111/j.1559-1816.2002.tb00236.x
- Armitage, C. J., & Conner, M. (2000). Social cognition models and health behaviour: A structured review. Psychology & Health, 15(2), 173–189. https://doi.org/10.1080/08870440008400299
- Ashwell, D., Cullinane, J., & Croucher, S. M. (2022). COVID-19 vaccine hesitancy and patient self-advocacy: A statistical analysis of those who can and can’t get vaccinated. BMC Public Health, 22(1), https://doi.org/10.1186/s12889-022-13661-4
- Baker, M. G., Kvalsvig, A., & Verrall, A. J. (2020). New Zealand’s COVID-19 elimination strategy. Medical Journal of Australia, 213(5), 198–200. https://doi.org/10.5694/mja2.50735
- Barattucci, M., Pagliaro, S., Ballone, C., Teresi, M., Consoli, C., Garofalo, A., De Giorgio, A., & Ramaci, T. (2022). Trust in science as a possible mediator between different antecedents and COVID-19 booster vaccination intention: An integration of health belief model (HBM) and theory of planned behavior (TPB). Vaccines, 10(7), 1099. https://doi.org/10.3390/vaccines10071099
- Baumgaertner, B., Carlisle, J. E., & Justwan, F. (2018). The influence of political ideology and trust on willingness to vaccinate. PLoS ONE, 13(1), e0191728. https://doi.org/10.1371/journal.pone.0191728
- Beehive.govt.nz. (2021). First Covid-19 vaccine approved. The New Zealand Government. Retrieved 20/2/23 from https://www.beehive.govt.nz/release/first-covid-19-vaccine-approved.
- Boas, T. C., Christenson, D. P., & Glick, D. M. (2020). Recruiting large online samples in the United States and India: Facebook, mechanical Turk, and qualtrics. Political Science Research and Methods, 8(2), 232–250. https://doi.org/10.1017/psrm.2018.28
- Bollyky, T. J., Hulland, E. N., Barber, R. M., Collins, J. K., Kiernan, S., Moses, M., Pigott, D. M., Reiner, R. C., Jr., Sorensen, R. J. D., Abbafati, C., Adolph, C., Allorant, A., Amlag, J. O., Aravkin, A. Y., Bang-Jensen, B., Carter, A., Castellano, R., Castro, E., Chakrabarti, S., … Dieleman, J. L. (2022). Pandemic preparedness and COVID-19: An exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, from January 1, 2020, to September 30, 2021. The Lancet, 399(10334), 1489–1512. https://doi.org/10.1016/S0140-6736(22)00172-6
- Brooks, C., Sangiorgi, I., Saraeva, A., Hillenbrand, C., & Money, K. (2023). The importance of staying positive: The impact of emotions on attitude to risk. International Journal of Finance & Economics, 28(3), 3232–3261. https://doi.org/10.1002/ijfe.2591
- Caso, D., Capasso, M., Fabbricatore, R., & Conner, M. (2022). Understanding the psychosocial determinants of Italian parents’ intentions not to vaccinate their children: An extended theory of planned behaviour model. Psychology & Health, 37(9), 1111–1131. https://doi.org/10.1080/08870446.2021.1936522
- Chou, W.-Y. S., & Budenz, A. (2020). Considering emotion in COVID-19 vaccine communication: Addressing vaccine hesitancy and fostering vaccine confidence. Health Communication, 35(14), 1718–1722. https://doi.org/10.1080/10410236.2020.1838096
- Conner, M., & Norman, P. (2005). Predicting health behaviour: A social cognition approach. In M. Conner, & P. Norman (Eds.), Predicting health bahaviour: Research and practice with social cognition theory (2nd ed, pp. 28–80). Open University Press.
- Cooke, H. (2021). Covid-19 NZ: Government sets 90% vaccine target to move to traffic-light system with no national lockdowns. Stuff.co.nz. Retrieved 22/2/23 from https://www.stuff.co.nz/national/politics/300436239/covid19-nz-government-sets-90-vaccine-target-to-move-to-trafficlight-system-with-no-national-lockdowns.
- Corbu, N., Negrea-Busuioc, E., Udrea, G., & Radu, L. (2021). Romanians’ willingness to comply with restrictive measures during the COVID-19 pandemic: Evidence from an online survey. Journal of Applied Communication Research, 49(4), 369–386. https://doi.org/10.1080/00909882.2021.1912378
- Cornally, N., Deasy, E. A., McCarthey, G., McAuley, C., Moran, J., & Weathers, E. (2013). Student nurses’ intention to get the influenza vaccine. British Journal of Nursing, 22(21), 1207–1211. https://doi.org/10.12968/bjon.2013.22.21.1207
- Cornish, S., & O’Dwyer, E. (2022). Police say more force on Wellington streets as protest enters second week. stuff.co.nz. Retrieved 22/2/2023 from https://www.stuff.co.nz/national/127763055/police-say-more-force-on-wellington-streets-as-protest-enters-second-week.
- COVID-19 data and statistics. (2023). The New Zealand government. Retrieved 22/2/23 from https://covid19.govt.nz/news-and-data/covid-19-data-and-statistics/.
- COVID-19: Vaccine data. (2022). Ministry of health New Zealand. Retrieved 10/10/2022 from https://www.health.govt.nz/covid-19-novel-coronavirus/covid-19-data-and-statistics/covid-19-vaccine-data.
- Croucher, S. M., Murray, N., Ashwell, D., Cullinane, J., & Nguyen, T. (2022). Predicting vaccine confidence: Patient self-advocacy and fear of COVID-19 in the United States. Southern Communication Journal, 87(4), 348-360. https://doi.org/10.1080/1041794X.2022.2099569
- Dutta, M. J. (2022). Pandemic communication as transformation. Journal of Applied Communication Research, 50(6), 593–594. https://doi.org/10.1080/00909882.2022.2153001
- Edwards, J. (2022). Flu season: Doctors call for free influenza vaccinations. Retrieved 10/10/2022 from https://www.rnz.co.nz/news/national/468282/flu-season-doctors-call-for-free-influenza-vaccinations.
- Fridman, I., Lucas, N., Henke, D., & Zigler, C. K. (2020). Association between public knowledge about COVID-19, trust in information sources, and adherence to social distancing: Cross-sectional survey. JMIR Public Health and Surveillance, 6(3), e22060. https://doi.org/10.2196/22060
- Gagnon, M. P., Godin, G., Gagne, C., Fortin, J. P., Lamothe, L., Reinharz, D., & Cloutier, A. (2003). An adaptation of the theory of interpersonal behaviour to the study of telemedicine adoption by physicians. International Journal of Medical Informatics, 71(2-3), 103–115. https://doi.org/10.1016/S1386-5056(03)00094-7
- Glassman, A., Kenny, C., & Yang, G. (2022). Covid-19 vaccine development and rollout in historical perspecitve. Center for global development https://www.cgdev.org/publication/covid-19-vaccine-development-and-rollout-historical-perspective.
- Godin, G., Vézina-Im, L.-A., & Naccache, H. (2010). Determinants of influenza vaccination among healthcare workers. Infection Control & Hospital Epidemiology, 31(7), 689–693. https://doi.org/10.1086/653614
- Haddock, G., & Maio, G. R. (2019). Chapter two - inter-individual differences in attitude content: Cognition, affect, and attitudes. In J. M. Olson (Ed.), Advances in experimental social psychology (Vol. 59, pp. 53–102). Academic Press. https://doi.org/10.1016/bs.aesp.2018.10.002
- Hair, J. F., Black, W. C., Babin, B. J., & Anderson, R. E. (2014). Multivariate data analysis (7th ed.). Prentice Hall.
- Harrison, J. A., Mullen, P. D., & Green, L. W. (1992). A meta-analysis of studies of the health belief model with adults. Health Education Research, 7(1), 107–116. https://doi.org/10.1093/her/7.1.107
- Heddy, B. C., Danielson, R. W., Sinatra, G. M., & Graham, J. (2017). Modifying knowledge, emotions, and attitudes regarding genetically modified foods. The Journal of Experimental Education, 85(3), 513–533. https://doi.org/10.1080/00220973.2016.1260523
- Hopman, C. E., Riphagen-Dalhuisen, J., Looijmans-van den Akker, I., Frijstein, G., Van der Geest-Blankert, A. D. J., Danhof-Pont, M. B., De Jager, H. J., Bos, A. A., Smeets, E., De Vries, M. J. T., Gallee, P. M. M., Lenderink, A. F., & Hak, E. (2011). Determination of factors required to increase uptake of influenza vaccination among hospital-based healthcare workers. Journal of Hospital Infection, 77(4), 327–331. https://doi.org/10.1016/j.jhin.2010.10.009
- Hu, L. t., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
- Jamison, A. M., Quinn, S. C., & Freimuth, V. S. (2019). “You don’t trust a government vaccine”: narratives of institutional trust and influenza vaccination among African American and white adults. Social Science & Medicine, 221, 87–94. https://doi.org/10.1016/j.socscimed.2018.12.020
- Johansen, L. J., Stenvig, T., & Wey, H. (2012). The decision to receive influenza vaccination among nurses in North and South Dakota. Public Health Nursing, 29(2), 116–125. https://doi.org/10.1111/j.1525-1446.2011.00966.x
- Larson, H. J., Clarke, R. M., Jarrett, C., Eckersberger, E., Levine, Z., Schulz, W. S., & Paterson, P. (2018). Measuring trust in vaccination: A systematic review. Human Vaccines & Immunotherapeutics, 14(7), 1599–1609. https://doi.org/10.1080/21645515.2018.1459252
- Lazarus, J. V., Wyka, K., White, T. M., Picchio, C. A., Rabin, K., Ratzan, S. C., Parsons Leigh, J., Hu, J., & El-Mohandes, A. (2022). Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nature Communications, 13(1), 3801. https://doi.org/10.1038/s41467-022-31441-x
- Ledda, C., Costantino, C., Cuccia, M., Maltezou, H. C., & Rapisarda, V. (2021). Attitudes of healthcare personnel towards vaccinations before and during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 18(5), 2703. https://doi.org/10.3390/ijerph18052703
- Li, H., Novack, D. H., Duke, P., Gracely, E., Cestone, C., & Davis, T. (2020). Predictors of medical students’ ethical decision-making: A pilot study using the theory of interpersonal behavior. Patient Education and Counseling, 103(12), 2508–2514. https://doi.org/10.1016/j.pec.2020.05.026
- Li, Y., & Samp, J. A. (2022). The impact of the COVID-19 pandemic on sexual orientation disclosure and post-disclosure depression among U.S. LGBQ individuals. Journal of Applied Communication Research, 50(5), 515–532. https://doi.org/10.1080/00909882.2022.2044503
- Ling, C. (2022). Northland tops list of big spenders for dishing out freebies during Covid-19 vaccination drive. New Zealand Herald. Retrieved 10/10/2022 from https://www.nzherald.co.nz/northern-advocate/news/northland-tops-list-of-big-spenders-for-dishing-out-freebies-during-covid-19-vaccination-drive/MITBQQQVK62DYEXFYB4OQUWFY4/.
- Liu, R., Huang, Y.-H. C., Sun, J., Lau, J., & Cai, Q. (2022). A shot in the arm for vaccination intention: The media and the health belief model in three Chinese societies. International Journal of Environmental Research and Public Health, 19(6), 3705. https://doi.org/10.3390/ijerph19063705
- Loomba, S., de Figueiredo, A., Piatek, S. J., de Graaf, K., & Larson, H. J. (2021). Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nature Human Behaviour, 5(3), 337–348. https://doi.org/10.1038/s41562-021-01056-1
- Luyten, J., Bruyneel, L., & van Hoek, A. J. (2019). Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine, 37(18), 2494–2501. https://doi.org/10.1016/j.vaccine.2019.03.041
- MacDonald, N. E. (2015). Vaccine hesitancy: Definition, scope and determinants. Vaccine, 33(34), 4161–4164. https://doi.org/10.1016/j.vaccine.2015.04.036
- Manhire, T. (2022a). Almost 90% of New Zealanders back Ardern government on Covid-19 – poll. The Spinoff. Retrieved 10/10/2022 from https://thespinoff.co.nz/politics/08-04-2020/almost-90-of-new-zealanders-back-ardern-government-on-covid-19-poll.
- Manhire, T. (2022b). One in four say NZ Covid restrictions too harsh, one in four say too weak – poll. The Spinoff. Retrieved 10/10/2022 from https://thespinoff.co.nz/politics/20-02-2022/one-in-four-say-nz-covid-restrictions-too-harsh-one-in-four-say-too-weak-poll.
- Mannava, P., Durrant, K., Fisher, J., Chersich, M., & Luchters, S. (2015). Attitudes and behaviours of maternal health care providers in interactions with clients: A systematic review. Globalization and Health, 11(1), https://doi.org/10.1186/s12992-015-0117-9
- Maridor, M., Ruch, S., Bangerter, A., & Emery, V. (2017). Skepticism toward emerging infectious diseases and influenza vaccination intentions in nurses. Journal of Health Communication, 22(5), 386–394. https://doi.org/10.1080/10810730.2017.1296509
- McClure, T. (2022). Trust in scientists soared in Australia and New Zealand during Covid pandemic, poll finds. The Guardian. Retrieved 10/10/2022 from https://www.theguardian.com/world/2021/nov/29/trust-in-scientists-soared-in-australia-and-new-zealand-during-covid-pandemic-poll-finds.
- McIntyre, D., Thiede, M., & Birch, S. (2009). Access as a policy-relevant concept in low- and middle-income countries. Health Economics, Policy and Law, 4(2), 179–193. https://doi.org/10.1017/S1744133109004836
- Meyvis, T., Van Osselaer, S. M. J. (2018). Increasing the power of your study by increasing the effect size. Journal of Consumer Research, 44(5), 1157-1173. https://doi.org/10.1093/jcr/ucx110
- Moodie, K. (2022). Mandate to sight Covid-19 vaccine passes ends at midnight. rnz.co.nz. Retrieved 22/2/2023 from https://www.rnz.co.nz/news/national/464578/mandate-to-sight-covid-19-vaccine-passes-ends-at-midnight.
- Moody, G. D., & Siponen, M. (2013). Using the theory of interpersonal behavior to explain non-work-related personal use of the internet at work. Information & Management, 50(6), 322–335. https://doi.org/10.1016/j.im.2013.04.005
- Moody, G. D., Siponen, M., & Pahnila, S. (2018). Toward a unified model of information security policy compliance. MIS Quarterly, 42(1), 285–311. https://doi.org/10.25300/MISQ/2018/13853
- Moon, W., & Balasubramanian, S. K. (2004). Public attitudes toward agrobiotechnology: The mediating role of risk perceptions on the impact of trust, awareness, and outrage. Review of Agricultural Economics, 26(2), 186–208. https://doi.org/10.1111/j.1467-9353.2004.00170.x
- Morton, J. (2023). Covid-19: The three biggest questions facing NZ in 2023. nzherald.co.nz. Retrieved 22/2/2023 from https://www.nzherald.co.nz/nz/covid-19-the-three-biggest-questions-facing-nz-in-2023/HZH2DFNQI5EABN6P7DYQFWXNWI/.
- Olagoke, A. A., Olagoke, O. O., & Hughes, A. M. (2021). Intention to vaccinate against the novel 2019 coronavirus disease: The role of health locus of control and religiosity. Journal of Religion and Health, 60(1), 65–80. https://doi.org/10.1007/s10943-020-01090-9
- Ouellette, J. A., & Wood, W. (1998). Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychological Bulletin, 124(1), 54–74. https://doi.org/10.1037/0033-2909.124.1.54
- Pérez-Peña, R. (2020). How the vaccine rollout will compare in Britain, Canada and the U.S. The New York Times. https://www.nytimes.com/2020/12/12/world/americas/covid-vaccine-us-uk-canada.html.
- Plohl, N., & Musil, B. (2021). Modeling compliance with COVID-19 prevention guidelines: The critical role of trust in science. Psychology, Health & Medicine, 26(1), 1–12. https://doi.org/10.1080/13548506.2020.1772988
- Pogue, K., Jensen, J. L., Stancil, C. K., Ferguson, D. G., Hughes, S. J., Mello, E. J., Burgess, R., Berges, B. K., Quaye, A., & Poole, B. D. (2020). Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines, 8(4), 582. https://doi.org/10.3390/vaccines8040582
- Quinn, S. C., Parmer, J., Freimuth, V. S., Hilyard, K. M., Musa, D., & Kim, K. H. (2013). Exploring communication, trust in government, and vaccination intention later in the 2009 h1n1 pandemic: Results of a national survey. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science, 11(2), 96–106. https://doi.org/10.1089/bsp.2012.0048
- Rahmani, D., Zeng, C., Goodarzi, A. M., & Vahid, F. (2021). Organizational compliance during COVID-19: Investigating the effects of anxiety, productivity, and individual risk factors among Iranian healthcare employees. Frontiers in Communication, 6(7). https://doi.org/10.3389/fcomm.2021.560451
- Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the health belief model. Health Education Quarterly, 15(2), 175–183. https://doi.org/10.1177/109019818801500203
- Rossettini, G., Conti, C., Suardelli, M., Geri, T., Palese, A., Turolla, A., Lovato, A., Gianola, S., & Dell’Isola, A. (2021). COVID-19 and health care leaders: How could emotional intelligence be a helpful resource during a pandemic? Physical Therapy, 101(9), 1–5. https://doi.org/10.1093/ptj/pzab143
- Servidio, R., Malvaso, A., Vizza, D., Valente, M., Campagna, M. R., Iacono, M. L., Martin, L. R., & Bruno, F. (2022). The intention to get COVID-19 vaccine and vaccine uptake among cancer patients: An extension of the theory of planned behaviour (TPB). Supportive Care in Cancer, 30(10), 7973–7982. https://doi.org/10.1007/s00520-022-07238-5
- Shahrabani, S., Benzion, U., & Yom Din, G. (2009). Factors affecting nurses’ decision to get the flu vaccine. The European Journal of Health Economics, 10(2), 227–231. https://doi.org/10.1007/s10198-008-0124-3
- Shiferaw, K. B., Mengiste, S. A., Gullslett, M. K., Zeleke, A. A., Tilahun, B., Tebeje, T., Wondimu, R., Desalegn, S., & Mehari, E. A. (2021). Healthcare providers’ acceptance of telemedicine and preference of modalities during COVID-19 pandemics in a low-resource setting: An extended UTAUT model. PLoS ONE, 16(4), e0250220. https://doi.org/10.1371/journal.pone.0250220
- Shmueli, L. (2021). Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health, 21(1), 1–13. https://doi.org/10.1186/s12889-021-10816-7
- Siegrist, M., & Zingg, A. (2014). The role of public trust during pandemics. European Psychologist, 19(1), 23–32. https://doi.org/10.1027/1016-9040/a000169
- Tawfiq, E., Azimi, M. D., Feroz, A., Hadad, A. S., Soroush, M. S., Jafari, M., Yaftali, M. S., & Saeedzai, S. A. (2023). Predicting maternal healthcare seeking behaviour in Afghanistan: Exploring sociodemographic factors and women’s knowledge of severity of illness. BMC Pregnancy and Childbirth, 23(1), 561. https://doi.org/10.1186/s12884-023-05750-y
- Timeline -Coronavirus. (2023). New Zealand doctors. Retrieved February 22, 2023, from https://www.nzdoctor.co.nz/timelinecoronavirus
- Tong, S. T., Stoycheff, E., & Mitra, R. (2022). Racism and resilience of pandemic proportions: Online harassment of Asian Americans during COVID-19. Journal of Applied Communication Research, 50(6), 595–612. https://doi.org/10.1080/00909882.2022.2141068
- Trent, M., Seale, H., Chughtai, A. A., Salmon, D., & MacIntyre, C. R. (2022). Trust in government, intention to vaccinate and COVID-19 vaccine hesitancy: A comparative survey of five large cities in the United States, United Kingdom, and Australia. Vaccine, 40(17), 2498–2505. https://doi.org/10.1016/j.vaccine.2021.06.048
- Triandis, H. (1977). Interpersonal behavior. Brooks/Cole Publishing Company.
- Troiano, G., & Nardi, A. (2021). Vaccine hesitancy in the era of COVID-19. Public Health, 194, 245–251. https://doi.org/10.1016/j.puhe.2021.02.025
- van der Linden, S., Roozenbeek, J., & Compton, J. (2020). Inoculating against fake news about COVID-19. Frontiers in Psychology, 11, https://doi.org/10.3389/fpsyg.2020.566790
- Verhallen, T. M. M., & Van Raaij, W. F. (1986). How consumers trade off behavioural costs and benefits. European Journal of Marketing, 20(3/4), 19–34. https://doi.org/10.1108/EUM0000000004639
- Ward, J. K., Alleaume, C., Peretti-Watel, P., Peretti-Watel, P., Seror, V., Cortaredona, S., Launay, O., Raude, J., Verger, P., Beck, F., Legleye, S., L’Haridon, O., & Ward, J. (2020). The French public’s attitudes to a future COVID-19 vaccine: The politicization of a public health issue. Social Science & Medicine, 265, 113414. https://doi.org/10.1016/j.socscimed.2020.113414
- Wilson, S. L., & Wiysonge, C. (2020). Social media and vaccine hesitancy. BMJ Global Health, 5(10), e004206. https://doi.org/10.1136/bmjgh-2020-004206
- Wiysonge, C. S., Ndwandwe, D., Ryan, J., Jaca, A., Batouré, O., Anya, B.-P. M., & Cooper, S. (2022). Vaccine hesitancy in the era of COVID-19: Could lessons from the past help in divining the future? Human Vaccines & Immunotherapeutics, 18(1), 1–3. https://doi.org/10.1080/21645515.2021.1893062
- Wong, L. P., Alias, H., Wong, P.-F., Lee, H. Y., & AbuBakar, S. (2020). The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Human Vaccines & Immunotherapeutics, 16(9), 2204–2214. https://doi.org/10.1080/21645515.2020.1790279
- World Health Organizatoin. (n.d.) Ten threats to global health in 2019. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- Wright, K. B., Riemann, W., & Fisher, C. L. (2022). Work–life-imbalance during the COVID-19 pandemic: Exploring social support and health outcomes in the United States. Journal of Applied Communication Research, 50(1), 54–69. https://doi.org/10.1080/00909882.2021.1965186
- Yang, Z. J. (2015). Predicting young adults’ intentions to get the h1n1 vaccine: An integrated model. Journal of Health Communication, 20(1), 69–79. https://doi.org/10.1080/10810730.2014.904023