To the Editor,
We have taken interest in the article by Siev-Ner I et al. [Citation1], which has been recently published in your journal. While we congratulate the authors for their great effort in calling attention to the value of ultrasound (US) imaging in the management of patellofemoral pain syndrome, we wish to put emphasis on particular issues.
First and foremost, the scanning technique used by the authors to quantify the intra-articular effusion located in the supra-patellar recess, with the knee flexed at 110 degrees, seems to be technically inappropriate. In fact, for localizing the joint fluid mild flexion (20–30°) of the knee is required [Citation2] because excessive flexion is associated with a shift/squeeze of the intra-articular effusion from the supra-patellar recess to the medial and lateral para-patellar recesses [Citation3].
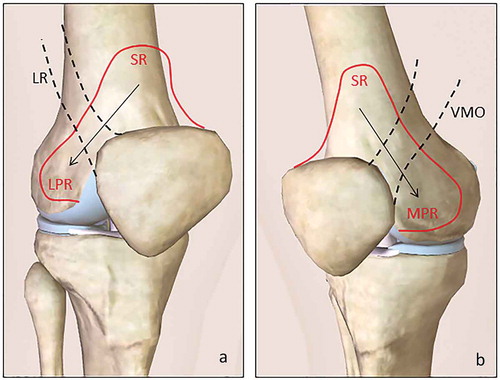
For the same reason, the medial and lateral sagittal views performed during the US examination might be misleading as well. In other words, the vastus medialis obliquus muscle (on the medial side) and the lateral retinaculum (on the lateral side) apply a ‘squeeze effect’ on the supra-patellar recess with an eventual displacement of the intra-articular effusion to the para-patellar recesses () [Citation3]. Moreover, the lack of posterior US imaging, whereby quantification of the joint fluid is an important parameter, is again an important drawback of this study since the gastrocnemius-semimembranosus bursa is often an important reservoir of intra-articular effusion in the painful knee [Citation4].
Figure 1. Schematic drawing shows the ‘squeeze effect’ of the lateral retinaculum on the lateral side (a) and the vastus medialis obliquus muscle on the medial side (b) over the supra-patellar recess with peripheral dislocation of the joint fluid to the para-patellar recesses.
SR: supra-patellar recess, LR: lateral retinaculum, LPR: lateral para-patellar recess, VMO: vastus medialis obliquus muscle, MPR: medial para-patellar recess.
Second, concerning the grading of the effusion, which should be based on a validated B-mode US scoring for the pediatric knee as regard the types of the US scans (i.e. suprapatellar, medial parapatellar and lateral parapatellar views) and the morphological features of the joint tissues (i.e. pre-patellar fat pad elevation/dislocation, anterio-posterior and cranio-caudal degree of extension of effusion, medial/lateral patello-femoral ligaments bulging) [Citation5].
Third; the limited number of patellar tendinopathies, in contrast to the previous pertinent studies (as the authors also mentioned) [Citation6], could again be related with incomplete US evaluation. For instance, Power Doppler mode, with a precise location of the ROI/region of interest at the level of critical zones for injuries (e.g. deep fibers of the tendon at the proximal insertion), could have been performed for identifying early signs of inflammation or remodeling [Citation7].
Concerning the ultrasonographic measurements of femoral cartilage thickness at the level of the trochlear groove; we agree with the authors to measure at the middle of each condyle but not with the recording of the smallest measurement.
Yet, especially in patients with asymmetric knee loading, focal thickening of the cartilaginous layer should be carefully evaluated because it may represent an early sonographic sign of focal cartilage edema [Citation8]. Of note, in those cases, either using the average values or a semiquantitative grading [Citation9] would also be reasonable alternative methods.
Last but not the least, we need to mention that while taking precise measurements, the technical quality of the images should be high in order not to have blurred/unclear margins of bony or cartilage surfaces (like in Figure 3).
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties. Peer reviewers on this manuscript have no relevant financial relationships to disclose.
Additional information
Funding
References
- Siev-Ner I, Stern MD, Tenenbaum S, et al. Ultrasonography findings and physical examination outcomes in dancers with and without patellofemoral pain. Phys Sportsmed. 2018;46:48–55.
- Özçakar L, Kara M, Chang KV, et al. EURO-MUSCULUS/USPRM Basic scanning protocols for knee. Eur J Phys Rehabil Med. 2015;51:641–646.
- Ricci V, Özçakar L. Ultrasonographic imaging of the medial and lateral pouches in the knee: EURO-MUSCULUS/USPRM protocol(s) revisited. Ann Phys Rehabil Med. 2018 Sep 28;pii:S1877-0657(18)31448–9.
- Çağlayan G, Özçakar L, Kaymak SU, et al. Effects of sono-feedback during aspiration of baker’s cysts: a controlled clinical trial. J Rehabil Med. 2016;48:386–389.
- Ting TV, Vega-Fernandez P, Oberle EL, et al. A novel ultrasound image acquisition protocol and scoring system for the pediatric knee. Arthritis Case Res. 2018 Sep 7. DOI:10.1002/acr.23746
- Nilsson C, Leanderson J, Wykman A, et al. The injury panorama in a Swedish professional ballet company. Knee Surg Sports Traumatol Arthrosc. 2001;9:242–246.
- Boesen MI, Boesen M, Langberg H, et al. Musculoskeletal colour/power doppler in sports medicine: image parameters, artefacts, image interpretation and therapy. Clin Exp Rheumatol. 2010;28:103–113.
- Mezian K, Ata AM, Kara M, et al. Ultrasonographic evaluation of the femoral cartilage, achilles tendon and plantar fascia in young women wearing high-heeled shoes. PMR. 2018 Sep 11;pii:S1934-1482(18)30907–9.
- Lee CL, Huang MH, Chai CY, et al. The validity of in vivo ultrasonographic grading of osteoarthritic femoral condylar cartilage: a comparison with in vitro ultrasonographic and histologic gradings. Osteoarthritis Cartilage. 2008;16:352–358.
