ABSTRACT
Hypertension is one of the most prevalent medical disorders in the world and is associated with significant cerebrovascular and cardiovascular morbidity. Pre-bout blood pressure (BP) elevation is extremely common, and ringside physicians must accurately assess the accompanying risk of adverse cerebrovascular and cardiovascular events in the decision to allow participation in combat sports. It is strongly recommended that a ringside physician consider disqualifying a combat sports athlete with severe pre-bout hypertension (systolic BP ≥160 mm Hg and/or diastolic BP ≥100 mm Hg, or stage 2 hypertension in children when indexed by gender, age, and height) from that bout, if it persists despite rest and repeated measurement with accurate equipment. This recommendation is congruent with that of the American College of Sports Medicine, the American College of Cardiology, and the American Heart Association, which recommend non-clearance for sports or exercise testing when BP exceeds those thresholds. Severely elevated BP, as defined above, confers markedly increased risk of morbidity and mortality. Exercise further raises BP markedly. The combination of severely elevated blood pressure and cranial trauma during combat sports is a risk factor for intracranial hemorrhage with a direct impact on the morbidity and mortality associated with ringside combat sports events. Combat sports athletes with SBP ≥130 or DBP ≥90 – and their coaches and families, if available and the athlete consents – should be educated on the causes of hypertension, its acute and chronic risks, and the possible future implications for bout clearance, and the athletes should be referred for evaluation and management.
Preamble: development of this statement
This position statement expresses a collaborative effort of subject matter experts within the Association of Ringside Physicians (ARP). An extensive literature search including but not restricted to MEDLINE, Cochrane Reviews, and non-indexed peer-reviewed articles published in online medical journals was performed regarding combat sports, sports, boxing, martial arts, exercise, blood pressure, hypertension, myocardial infarction, stroke, and intracranial hemorrhage. Unfortunately, there is a significant lack of published literature regarding the consequences and significance of pre-bout blood pressure elevation. Hence, much of this statement is an extrapolation of current recommendations from other scientific bodies, and incorporates both current best practices in combat sports and the collective expertise of the ARP membership, who have provided ringside medical coverage over many years.
Definitions
Hypertension is the repeated or persistent elevation of blood pressure (BP), either systolic (SBP), and/or diastolic (DBP). Elevated BP is one of the most common medical conditions and has a strong, linear correlation with cardio-/cerebro-vascular disease (CCVD) and overall increased risk of death [Citation1]. Normal BP in adults is defined as SBP <120 mm Hg and DBP <80 mm Hg. High BP is categorized into four levels () based on average BP measured on at least two occasions by medical personnel: elevated BP, stage 1 hypertension, stage 2 hypertension, and severe hypertension. Elevated BP is defined as SBP 120–129 mm Hg and DBP <80 mm Hg. Stage 1 hypertension is defined as SBP 130–139 mm Hg or DBP 80–89 mm Hg. Stage 2 hypertension is defined as SBP ≥140 mm Hg or DBP ≥ 90 mm Hg. Severe hypertension is defined as SBP ≥ 160 mm Hg or DBP ≥ 100 mm Hg [Citation1]. These categories, from the 8th Joint National Committee on Hypertension (JNC 8) guidelines, were amended from the 2003 JNC 7 guidelines because more recent studies showed increased CCVD risk even at the lower levels of BP.
Table 1. Categories of elevated blood pressure.
Physiology of blood pressure with regard to exercise
Exercise raises BP due to compensatory increases in heart rate and stroke volume, and therefore cardiac output, in order to supply more active tissues with oxygenated red blood cells. Increased systemic vascular resistance within actively contracting skeletal muscles also raises BP. Systolic BP normally rises much more than DBP. Typical SBP values in men during exercise range from 150 to 210 mm Hg, and up to 190 mm Hg in women. Diastolic BP normally stays the same or rises less than 10 mm Hg during exercise. During exercise, any SBP over 210 mm Hg in men or SPB over 190 mm Hg in women, or DBP over 110 mm Hg in either sex, is considered excessive [Citation2]. However, intra-arterial arm BP values as high as 480/350 mm Hg have been recorded in healthy men during resistance exercise [Citation3].
The type of exercise (static vs dynamic) and intensity of exercise also determine the BP response. Static exercise, which involves forceful contraction of skeletal muscle (strength and power exercise), primarily causes a pressure load on the cardiovascular system and leads to dramatic increases in BP. The more muscle mass involved, the greater the rise in BP. Dynamic exercise, which involves the endurance component of muscle contraction, primarily causes a volume load on the cardiovascular system and normally leads to only small increases in BP [Citation4]. Boxing and mixed martial arts are sports classified as having both high dynamic and high static loads, therefore dramatic increases in BP should be expected during these sports.
Epidemiology of high blood pressure
High BP is the most common abnormal finding during pre-participation cardiovascular screening in athletes [Citation5]. Hypertension is very common, with prevalence of 41% in men age 20–44 and 29% in women age 20–44 using JNC-8 criteria [Citation1]. The prevalence rises dramatically with age. African Americans have the highest overall prevalence among the various races/ethnicities, followed by Asians, Caucasians, and Hispanics. The vast majority of hypertension is ‘essential’ and is caused by several factors including but not limited to advancing age, genetics, excessive salt use, inadequate exercise/fitness, and obesity. Secondary hypertension, which occurs in about 10% of adults, is caused by more specific and often remediable causes such as renal parenchymal disease, renovascular disease, aortic coarctation, drugs (prescription or illicit), obstructive sleep apnea, primary hyperaldosteronism, Cushing’s syndrome, hyperthyroidism, primary hyperparathyroidism, congenital adrenal hyperplasia, pheochromocytoma, and acromegaly [Citation1].
High BP is likely more prevalent in athletes than in healthy controls. A systematic review of 51 studies involving athletes found hypertension (mean SBP ≥130 mm Hg) in two-thirds of the studies [Citation6]. The study using the current threshold for stage 1 hypertension of ≥130 mm Hg (most studies had higher cutoffs) showed hypertension in 45% of athletes compared to 17% in age-matched and gender-matched controls [Citation6]. Though moderate exercise (e.g. 30 minutes most days a week) is known to modestly reduce BP over time in persons with hypertension, this effect has not been proven in athletes. Studies of elite and professional athletes, most of whom train for over 10 hours a week, show a trend toward higher levels than those who train less than 10 hours a week. Proposed mechanisms for higher BP in elite athletes include mental stress and supplement/drug use [Citation5].
There is a paucity of research on combat sports athletes and BP. One study of collegiate athletes in India compared BP in boxing, football, handball, netball, and cycling athletes with that of controls (physical education students). It showed comparable resting SBP and DBP in boxers compared to the other groups. During moderate intensity cycling, boxers had slightly lower SBP than the other athletes. During vigorous cycling boxers had SBP equal to other athletes, but BP was not measured during other sports [Citation7].
Pathophysiology of elevated blood pressure
Elevated BP is known to have a direct log-linear relationship with the risk of CCVD, beginning at a SBP of 115 mm Hg or DPB of 75 mm Hg [Citation1]. Myocardial infarction (MI), angina, heart failure, peripheral artery disease, and abdominal aortic aneurysm are common comorbidities directly caused by elevated BP. The risk for such comorbidities is often compounded by the presence of additional cardiovascular disease risk factors (i.e. smoking, diabetes mellitus, dyslipidemia, overweight/obesity, physical inactivity, unhealthy diet, chronic kidney disease, genetics, increased age, low socioeconomic status, male sex, obstructive sleep apnea, and psychological stress) [Citation1]. Hypertension also has a direct relationship with the risk of ischemic stroke, hemorrhagic stroke, and subarachnoid hemorrhage [Citation1]; however, data clarifying the risk in athletes is lacking. Hypertension is the single most important risk factor for intracerebral hemorrhage [Citation8]. A large meta-analysis showed that BP in excess of 160/90 mm Hg resulted in a nine-fold increase in the risk for intracerebral hemorrhage [Citation9], though this data is not specific to athletes and may represent persons who are on average older and likely have preexisting hypertension. Vigorous exercise has been identified as a trigger for subarachnoid hemorrhage – both aneurysmal and non-aneurysmal – in most studies [Citation10–12]. In the United States, hypertension causes more CCVD deaths than any other modifiable risk factor [Citation13] [Citation14–16].
Resting BP is a useful yet imperfect predictor of cardiovascular risk. As discussed above, BP rises significantly with exercise, but the magnitude of rise may be somewhat commensurate with the workload produced. Research has shown that workload-indexed blood pressure response to exercise (wiBPR, expressed as SBP per metabolic equivalents) is superior to resting or peak exercise SBP in predicting all-cause mortality in healthy men [Citation14]. While some studies suggest wiBPR may have utility in preparticipation screening of athletes at risk for developing hypertension or in stratifying their CCVD risk [Citation15,Citation16], its role is undetermined, and it is impossible to perform immediately prior to a combat sports event.
Exercise and sports only rarely cause CCVD-related events or death in healthy persons and athletes [Citation17–20]. However, the presence of pre-exercise hypertension predicts an exaggerated exercise BP response and theoretically increases the risk of adverse cardiovascular and cerebrovascular events during exercise. For this reason, the American College of Sports Medicine recommends that individuals with SBP ≥160 mm Hg or DBP ≥100 mm Hg should not engage in any exercise, including exercise testing, prior to a medical evaluation and adequate BP management [Citation17]. Furthermore, the American Heart Association and American College of Cardiology have recommended in their Scientific Statement on Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities that athletes with SBP >160 mm Hg or DBP >100 mm Hg ‘… should be restricted, particularly from high static sports, such as weight lifting, boxing, and wrestling, until hypertension is controlled …’ [Citation21].
Of particular concern in boxing, martial arts, and other sports with purposeful or accidental head trauma, is the added risk for intracranial bleeding. Some studies have estimated that up to 31.9% of mixed martial arts matches end as a direct result of head trauma, either by knockout or technical knockout [Citation22]. Additionally, subdural hematomas have been identified as ‘the most common cause of boxing-related mortality’ [Citation23]. Although no studies on athletes are available to quantify the added risk that head trauma brings to the cerebral vasculature in addition to hypertension and vigorous exercise, the risks are likely compounded, and neurological outcomes may be worse in a severely hypertensive athlete who sustains traumatic intracranial bleeding during a bout. Therefore, prudent clinical judgment should tend toward athlete safety, hence the recommended disqualification threshold being 160/100 (severe hypertension).
Pre-bout hypertension may also be a sign of drug, exogenous hormone, and/or supplement use. Many prescription medications and illicit drugs can cause elevated BP; common culprits are listed in . Illicit drug users have a 6.5-times increased risk of hemorrhagic and ischemic stroke; cocaine, amphetamines, Ecstasy, ephedrine, phencyclidine, and LSD are known culprits [Citation24]. Hemorrhagic strokes have also been reported after the use of pre-workout supplements [Citation25–27]. Cocaine use can cause sudden cardiac death, life-threatening arrhythmias, myocardial ischemia and infarction, dilated cardiomyopathy, and acute myocarditis [Citation28]. Amphetamines can cause myocardial infarction [Citation29], and energy drinks have been linked to myocardial ischemia [Citation30]. Androgenic anabolic steroid abuse has been linked to arterial hypertension, accelerated progression of coronary artery disease, and increased risk of myocardial infarction [Citation31]. Participating in combat sports, with its vigorous high-static/high-dynamic exercise and repeated head trauma, while these substances are in the body may compound the risk of significant adverse events.
Table 2. Common prescription and illicit drugs that can elevate BP.
While studies on the prevalence of prescription drug abuse and illicit drug use by combat sports athletes are lacking, many studies document a significant prevalence of abuse in elite and non-elite athletes [Citation32]. The 2009, 2013, and 2017 iterations of the NCAA National Study on Substance Use Habits of College Student-Athletes showed nicotine use by 11–48%, amphetamine use by 3.2–11.0%, cocaine use by 2.2–11.9%, and anabolic steroid use by 0.6–2.2% of wrestlers [Citation33]. Anabolic steroid use was reported by 9.1% of retired National Football League players [Citation34] and by 21% of retired Swedish power sport athletes [Citation35]. The prevalence of higher-risk supplement use (herbal ingredients, caffeine, weight loss or muscle-building supplements, or pre-workout supplements) was 8.3% in collegiate athletes [Citation36]. In most amateur and some professional combat sports clubs and promotions, where thorough drug screening may not be conducted, the prevalence of illicit drug and supplement use may be comparable or even higher in event participants, although further studies are needed to substantiate this.
Managing the athlete with pre-bout hypertension
Sanctioning bodies should require BP measurement/documentation for all licensing physicals and have a firm threshold with respect to BP for licensing a combat sports athlete. Applicants whose SBP is ≥160 mm Hg or DBP ≥100 mm Hg on the licensing physical should not be licensed until proof of BP lower than these thresholds is documented by a medical professional. This is in agreement with the thresholds recommended by the AHA/ACC ‘Scientific Statement on Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities’ [Citation4] and the ACSM Guidelines for Exercise Testing and Prescription, 10th Ed [Citation17].
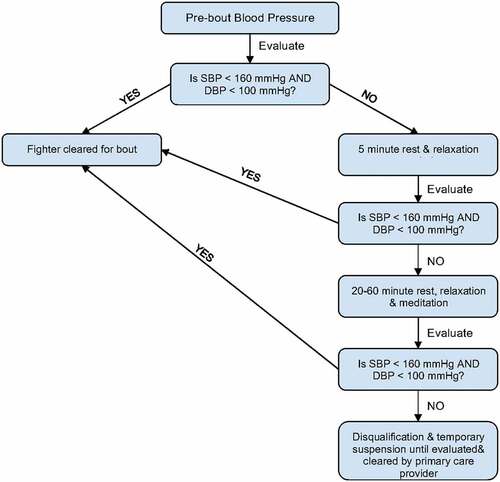
In some jurisdictions BP is measured near the time of weigh-in, and in others it is done hours before the bout. Regardless, ringside physicians conducting pre-bout physicals should always document BP and treat it as a vital sign with life and death implications requiring a prudent bout clearance decision (). Even when a licensing physical (if available to review) has documented BP in the acceptable range, pre-bout hypertension should be recognized as a risk factor for morbidity/mortality and regarded as possible new-onset chronic hypertension. Physicians should always include BP as a pre-bout vital sign and strongly consider requiring SBP <160 mm Hg AND DBP <100 mm Hg for clearance. In athletes under 18 years of age, BP must be indexed to gender, age, and height (https://www.nhlbi.nih.gov/files/docs/bp_child_pocket.pdf). Children with stage 2 hypertension (defined as BP repeatedly at or greater than the 95th percentile plus 12 mmHg when indexed for gender, age, and height) should also be prohibited from participating in high-static sports (e.g. boxing, wrestling, mixed martial arts, and weightlifting) [Citation21,Citation37]. For athletes of all ages, both arms should be used to record BP on the first iteration, and the arm with the higher reading should be used for all subsequent measurements [Citation1]. High BP may just be situational and not pathologic; reassurance, rest, and recheck will in most cases bring it down into acceptable limits. Athletes should be reassured that most high BP comes down with rest. In many cases 5 minutes of rest is sufficient. If not, they should be told to avoid exercise, to relax in a relatively quiet location, to close their eyes and meditate on relaxing scenarios, and await reevaluation by the physician in 20–60 minutes. The physician should check the BP manually or with an automated, calibrated brachial cuff, using an appropriately sized cuff over the bare arm. The athlete should be sitting and with the arm and cuff at the level of the heart. Wrist cuffs should not be used [Citation1].
If an athlete’s pre-bout BP is in the severely elevated range, we also recommend performing an expanded history and physical examination to search for its underlying cause(s) (). In our collective experience, an expanded evaluation and repeated BP measurement will usually categorize hypertensive athletes into one of four categories: 1) spuriously elevated BP due to increased sympathetic tone from pre-bout anxiety; this type is most common and usually improves with rest and relaxation; 2) hypertension secondary to the use of supplements or drugs (); 3) persistently elevated BP that likely represents essential hypertension; or 4) hypertensive emergency (rare) in which there is evidence of cardiac, cerebral, or renal dysfunction, which would warrant referral to an emergency department for immediate treatment. Elucidating the underlying etiology can assist the ringside physician in clearance decisions to reduce the risk of cardiovascular or cerebrovascular morbidity. It can also assist the physician in athlete counseling and follow-up recommendations.
Table 3. Suggested expanded history, physical and testing for severely elevated pre-bout blood pressure. For each finding on the left side of the table, its associated possible cause(s) is/are immediately to the right. Athletes with these findings warrant immediate disqualification from competition and need emergent referral for workup and treatment.
We strongly recommend that athletes with SBP ≥160 mm Hg or DBP ≥100 mm Hg – or stage 2 hypertension in children – that persists despite reassurance, rest, and rechecks be disqualified from the upcoming bout due to increased risk of cardiovascular and cerebrovascular morbidity and mortality. As discussed above, prudent clinical judgment is paramount. The athlete, their coach, and their family, if possible, should be educated on the causes of high BP, and the athletes should be referred appropriately. Athletes with severe hypertension secondary to drug use but without end-organ dysfunction should be advised to abstain from these drugs and to seek treatment in urgent care if worrisome symptoms appear. Athletes with hypertensive emergency should be treated as appropriate for the clinical syndrome while being transported immediately to an emergency department. Asymptomatic athletes with suspected severe essential hypertension should be referred to primary care for evaluation and management. Note also there is absolutely no role for using pre-bout antihypertensive agents in athletes in order to lower BP into an acceptable range, other than the scenario where an athlete needs to take a scheduled or overdue dose of medication that had already been prescribed to treat chronic hypertension.
Athletes with persistent stage 1 or 2 hypertension may be cleared to compete but should be educated by the ringside physician on the long-term risks of uncontrolled hypertension. They should be encouraged to seek further evaluation by their primary care provider and be advised of the thresholds for non-clearance.
Discussion of guidelines
Sudden death in young athletes is a rare event, but when it happens the impact on the sporting community and sometimes even the general population can be profound. In one of the largest high-quality studies on sudden death in athletes, boxing, wrestling, and martial arts represented only 7.8% of the total deaths, while football and basketball accounted for the vast majority (52%) [Citation38]. In boxing, 75% of deaths were from trauma (presumably to the head), and in martial arts 33% were from trauma. In wrestling, only 10% of the deaths were from trauma, whereas 54% were from cardiovascular diseases [Citation39]. A study on deaths just among celebrities – persons of public interest who are household names in a large part of the population – showed that boxing and MMA were the highest risk occupations. Forty-two percent of the boxing and MMA deaths analyzed in the study occurred within or near the ring/cage whereas only 9% of deaths in other sports resulted from sport-related activity (the remainder of deaths was non-sport violence, drug overdose, vehicle/airplane accidents, etc.) [Citation39]. Therefore, ringside physicians, who inherently serve those at highest risk for sports-related morbidity and mortality, should exercise conservative prudence in bout clearance decisions, not only for athlete safety but also because of the intense scrutiny affiliated with ringside medicine.
Consequently, to better promote athlete safety and mitigate the probability of hypertensive-related adverse events, it is the recommendation of the authors of this manuscript that a pre-bout blood pressure threshold for disqualification of SBP ≥ 160 mmHg and/or DBP ≥ 100 mmHg be established as a guideline to sound clinical judgment. These thresholds are consistent with the American College of Sports Medicine, the American Heart Association, and the American College of Cardiology. As combat sports athletes have high levels of static and dynamic vascular stress and are at risk of head trauma, ignoring these recommendations would be unwise and could place athletes at unnecessary increased risk of adverse events.
Qualifying statement
These guidelines are recommendations to assist ringside physicians, combat sports athletes, trainers, promoters, sanctioning bodies, governmental bodies, and others in making decisions and setting policy. These recommendations may be adopted, modified, or rejected according to clinical needs and constraints and are not intended to replace local commission laws, regulations, or policies already in place. In addition, the guidelines developed by the ARP are not intended as standards or absolute requirements, and their use cannot guarantee any specific outcome. Guidelines are subject to revision as warranted by the evolution of medical knowledge, technology, and practice. They provide the basic recommendations that are supported by synthesis and analysis of the current literature, expert and practitioner opinion, commentary, and clinical feasibility.
Acknowledgments
The authors would like to thank the Board of Directors of the Association of Ringside Physicians for their collective wisdom, experience, and collaborative work that greatly enhanced this Position Statement. Members at the time of this document’s approval on 23 January 2021 included Donald Muzzi, John Neidecker, Richard Weinstein, Nitin Sethi, Bradford Lee, Gerard Varlotta, Warren Wang, Kevin deWeber, Louis Durkin, Nicholas Rizzo, Randa Bascharon, Larry Lovelace, and Edward Amores.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guidelines for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2018;71(19):e127–248.
- Sharman JE, LaGerche A. Exercise blood pressure: clinical relevance and correct measurement. J Human Hypert. 2015;29:351–358.
- MacDougall JD, Tuxen D, Sale DG, et al. Arterial blood pressure response to heavy resistance exercise. J Appl Physiol. 1985;58:785–790.
- Levine BD, Baggish AL, Kovacs RJ, et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 1: classification of sports: dynamic, static, and impact. J Am Coll Cardiol. 2015;66(21):2350–2355.
- Berge HM, Isern CB, Berge E. Blood pressure and hypertension in athletes: a systematic review. Br J Sports Med. 2015;49:716–723.
- Helzberg JH, Waeckerle JF, Camilo J, et al. Comparison of cardiovascular and metabolic risk factors in professional baseball players versus professional football players. Am J Cardiol. 2010;106:664–667.
- Desalegn M, Verma SK. Comparison of cardiovascular responses to exercise and recovery pattern in players. J Exer Sci Physiother. 2008;4(1):55–65.
- Ikram MA, Wieberdink RG, Koudstaal PJ. International epidemiology of intracerebral hemorrhage. Curr Atheroscler Repo. 2012;14:300–306.
- O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE) study): a case-control study. Lancet. 2010;376(9735):112–123.
- Fann JR, Kukall Wa, Katon WJ, et al. Physical activity and subarachnoid haemorrhage: a population based case-control study. J Neurol Neurosurg Psychiatry. 2000;69(6):768–772.
- Anderson C, Ni Mhurchu C, Scott D, et al. Triggers of subarachnoid hemorrhage: role of physical exertion, smoking, and alcohol in the Australasian Cooperative Research on Subarachnoid Hemorrhage Study (ACROSS). Stroke. 2003;34[7:1771–1776.
- Vlak MH, Rinkel GJ, Greebe P, et al. Trigger factors and their attributable risk for rupture of intracranial aneurysms: a case-crossover study. Stroke. 2011;42(7):1878–1882.
- Danaei G, Ding EL, Mazaffarian D, et al. The preventable causes of death in the United States: comparative risk assessment of dietary, lifestyle, and metabolic risk factors. PLoS Med. 2009;6:e1000058.
- Hedman K, Cauwenberghs N, Christle JW, et al. Workload-indexed blood pressure response is superior to peak systolic blood pressure in predicting all-cause mortality. Eur J Prev Cardiol. 2020;27(9):978–987.
- Bauer P, Kraushaar L, Hoelscher S, et al. Blood pressure response and vascular function of professional athletes and controls. Sports Med Int Open. 2021;5:E45–E52.
- Bauer P, Kraushaar L, Dorr O, et al. Workload-indexed blood pressure response to a maximum exercise test among professional indoor athletes. Eur J Prev Cardiol. 2021;28:1487–1494.
- Benefits and risks associated with physical activity. In: Riebe D, Ehrman JK, Liguori G, et al., editors. ACSM’s Guidelines for exercise testing and prescription. 10th. Philadelphia: Wolters Kluwer; 2018. p. 1–21.
- Cayen B, Cullen N. Intracerebral haemorrhage in previously healthy adults following aerobic and anaerobic exercise. Brain Inj. 2002;16(5):397–405.
- Onnic E, Montisci R, Corda L, et al. Intracranial haemorrhage during exercise testing. Eur Heart J. 1995;16(2):282–284.
- Bouzas-Mosquera MC, Bouzas-Mossquera A, Peteiro J, et al. Exaggerated exercise blood pressure response and risk of stroke in patients referred for stress testing. Eur J Intern Med. 2014;25(6):533–537.
- Black HR, Sica D, Ferdinand K, et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 6: hypertension. J Am Coll Cardiol. 2015;66(21):2393–2397.
- Hutchinson MG, Lawrence DW, Cusimano MD, et al. Head trauma in mixed martial arts. Am J Sports Med. 2014;42(6):1352–1358.
- Anghinah R, Ianof JN. Traumatic brain injury in fighting sports. In: Anghinah R, Paiva W, Battistella L, et al., editors. Topics in cognitive rehabilitation in the TBI post-hospital phase. New York: Springer; 2018. p. 79–85.
- Fonseca AC, Ferro JM. Drug abuse and stroke. Curr Neurol Neurosci Rep. 2013;13:325–334.
- Harris BF, Winn C, Ableman TB. Hemorrhagic stroke in a young healthy male following use of pre-workout supplement animal rage XL. Mil Med. 2017;182(9):e2030–33.
- Cohen PA, Zeijlon R, Nardin R, et al. Hemorrhagic stroke probably caused by exercise combined with a sports supplement containing β-methylphenyl-ethylamine (BMPEA): a case report. Ann Intern Med. 2015;162(12):879–880.
- Zeijlon R, Andersson B. Cerebral hemorrhage after ingestion of the performance enhancer “Jacked Power.” Healthy woman fell ill during exercise after a single dose. Lakartidningen. 2014;111(41):1782–1784.
- Talarico GP, Crosta ML, Giannico MB, et al. Cocaine and coronary artery diseases: a systematic review of the literature. J Cardiovasc Med (Hagerstown). 2017;18(5):291–294.
- Fischbach P. The role of illicit drug use in sudden death in the young. Cardiol Young. 2017;27(S1):S75–9.
- Lippi G, Carvellin G, Sanchis-Gomar F. Energy drinks and myocardial ischemia: a review of case reports. Cardiovasc Toxicol. 2016;16(3):207–212.
- Barton M, Prossnitz ER, Meyer MR. Testosterone and secondary hypertension: new pieces to the puzzle. Hypertension. 2012;59(6):1101–1103.
- McDuff D, Stull T, Castaldelli-Maia JM, et al. Recreational and ergogenic substance use and substance use disorders in elite athletes: a narrative review. Br J Sports Med. 2019;53:754–760.
- NCAA National study on substance abuse habits of college student-athletes, June 2018. http://www.ncaa.org/sites/default/files/2018RES_Substance_Use_Final_Report_FINAL_20180611.pdf. Accessed 2020 Feb 21.
- Horn S, Gregory P, Guskiewicz KM. Self-reported anabolic-androgenic steroids use and musculoskeletal injuries: findings from the center for the study of retired athletes health survey of retired NFL players. Am J Phys Med Rehabil. 2009;88:192–200.
- Lindqvist AS, Moberg T, Eriksson BO, et al. A retrospective 30-year follow-up study of former Swedish-elite male athletes in power sports with a past anabolic androgenic steroids use: a focus on mental health. Br J Sports Med. 2013;47:965–969.
- Flynn JT, Kaelber DC, Baker CM, et al. Clinical practice guidelines for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140(3):e20171904.
- Sassone J, Muster M, Barrack MT. Prevalence and predictors of higher-risk supplement use among collegiate athletes. J Strength Cond Rs. 2019;33(2):443–450.
- Maron BJ, Doerer JJ, Haas TS, et al. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009;119(8):1085–1092.
- Ball CG, Dixon E, Parry N, et al. Celebrity traumatic deaths: are gangster rapper really “gansta”? Can J Surg. 2013;56(4):E59–62.