ABSTRACT
Chemsex refers to the use of psychoactive substances with sex. We carried out a systematic scoping review of methodological characteristics of chemsex research among men who have sex with men (MSM), published between 2010 and 2020. For inclusion, chemsex had to be the main focus, and studies had to specify GHB/GBL, stimulant (amphetamine, crystal meth, ecstasy/MDMA, cathinones, cocaine) and/or ketamine use with sex as a variable. From 7055 titles/abstracts, 108 studies were included, mostly cross-sectional, and from Western countries. About one-third of studies recruited exclusively from clinical settings. A majority of these recruited from sexually transmitted infection (STI) clinics. The included quantitative studies analyzed possible associations between chemsex and STI health (40%), mental health (15%), drug health (12%), sexological health (10%), and post-diagnostic HIV health (7%). Most studies included GHB/GBL and crystal meth in their operationalization of chemsex. Definitions and operationalizations of chemsex vary greatly in the literature, and researchers of chemsex among MSM should consider ways in which this variation impacts the validity of their results. More studies are needed among MSM in non-high income and non-Western countries, and examination of possible links between chemsex and post-diagnostic HIV health, sexological health, and mental health.
Background
Chemsex refers to the use of psychoactive substances in a context that involves sex (Ballesteros-López et al., Citation2016; Drückler et al., Citation2018; Roux et al., Citation2018; Skryabin et al., Citation2020; Tomkins et al., Citation2018; Turner et al., Citation2015). In research among MSM, drugs such as alcohol, cannabis, and poppers are typically excluded from definitions of chemsex (Glynn et al., Citation2018; Knoops et al., Citation2015; Skryabin et al., Citation2020). Chemsex is often defined as the sexualized use of specific drugs, and typically includes the use of drugs, such as GHB/GBL, crystal meth, and synthetic cathinones with sex. Some authors only consider chemsex to be occurring when either one of these three drugs are used with sex (Bourne et al., Citation2015; Drückler et al., Citation2018; Sewell et al., Citation2019), whereas others have defined chemsex to also include ketamine (Flores-Aranda et al., Citation2019; Frankis et al., Citation2018; Hibbert et al., Citation2019), ketamine or cocaine (Haugstvedt et al., Citation2018; Pakianathan, Whittaker, Lee et al., Citation2018), and amphetamine, ecstasy/MDMA or cocaine use with sex (Evers et al., Citation2019; Glynn et al., Citation2018; Gonzalez-Baeza et al., Citation2018; Skryabin et al., Citation2020; Van Hout et al., Citation2019). In addition to variations in drugs-based definitions of chemsex, some definitions are described as national rather than universal (Bourne, Reid, Hickson, Torres-Rueda, Steinberg et al. Citation2015; Evers, Van Liere et al., Citation2019; Sewell et al., Citation2019), excluding drug use with sex that is not consumed with a sexual purpose or intention in mind (Bourne, Reid, Hickson, Torres-Rueda, & Weatherburn, Citation2015; Pakianathan, Whittaker, Lee et al., Citation2018; Pufall et al., Citation2018; Wong et al., Citation2020), occurring among men who have sex with men (MSM) (Frankis et al., Citation2018; Hibbert et al., Citation2019; Roux et al., Citation2018; Tan et al., Citation2018), or taking place in extended sexual sessions that include multiple sex partners (Ahmed et al., Citation2016; Hibbert et al., Citation2019 Tan et al., Citation2018; Van Hout et al., Citation2019). One could hardly argue that an agreed and universally adopted definition of chemsex exists. Chemsex has been portrayed as being increasingly common among men who have sex with men (MSM) (Bourne, Reid, Hickson, Torres-Rueda & Weatherburn, Citation2015), particularly after technological innovations such as the Internet and smartphone technology changed the way people get into contact with one another (Donnadieu-Rigole et al., Citation2020; Drysdale et al., Citation2020; Guerra et al., Citation2020; Hibbert et al., Citation2021; Lafortune et al., Citation2021).
Sexological, mental, and drug health are all likely to be relevant for researchers concerned with health drivers and consequences of chemsex among MSM (Dolengevich-Segal et al., Citation2019; Hibbert et al., Citation2019; Lafortune et al., Citation2021; Schecke et al., Citation2019; Speulman et al., Citation2019). In an account of the origin of the word “chemsex,” Stuart suggests that MSM who use drugs such as crystal meth, GHB, and mephedrone with sex, do so in order to compensate for a reduced ability to enjoy sex, love, and relationships (Stuart, Citation2019). He argues that this reduction in sexological health and level of social/emotional intimacy is directly attributable to three factors: 1) societal homonegativity and 2) the trauma/stigma of the HIV/AIDS epidemic, both reinforcing representations of gay sex as dirty, disgusting, and dangerous, and 3) the intensification of a rejection culture between MSM after sexual networking moved to smartphone apps. Moreover, sexual identities other than heterosexuality generally carry a higher risk for poor mental health compared to the general population, resulting in higher rates of depression and anxiety, suicide, and substance use disorders (King et al., Citation2008). In a study of crystal meth use with sex and mental health among MSM, Bonn, and colleagues note that this connection is often explained by the minority stress model, which highlights the role of ongoing stress and perceived and enacted stigma as a result of being part of a minority (Bohn, Sander, Kohler et al., Citation2020a).
Syndemic theory provides a theoretical framework that seeks to explain why co-occurring problems within different areas of health can interact and magnify one another within socially stigmatized groups (Singer, Citation2009). It highlights the importance of evaluating possible health drivers and consequences of chemsex within all clinical health domains where MSM are experiencing lower levels of health than the general population, and not only within the domain of sexually transmitted infections (STI). Furthermore, in the case of chemsex, there is not just one relevant type of stigma that may reinforce health inequalities in multiple areas of health at the same time. There are three types of stigmas of relevance to chemsex, namely that toward gay and bisexual men, drug use and positive HIV status. They may interact in different ways with one another, with chemsex, with health, and with other contingencies, a complexity that can be built into analytical models using intersectionality study frameworks.
To the best of our knowledge, to date, there are no analyses of the methodological choices made by researchers studying chemsex among MSM. Our literature search and screening process add to existing reviews by not limiting inclusion to studies of a certain health field only, for example, STI health. Researchers wishing to extract outcome variables from the studies included in our review, would benefit from the broad scope of our inclusion criteria regarding health fields, and the quality of the literature search and screening process.
Several researchers have highlighted the importance of the assumptions and methodological choices made by researchers of chemsex among MSM (Bryant et al., Citation2018; Drysdale et al., Citation2020; Souleymanov et al., Citation2019). Understanding methodological approaches is important in proper interpretation of the collected data, as they may differentially impact how they inform policy and research, and how practitioners might draw on chemsex research to improve health outcomes for MSM. The motivation for this study is to gain insight into how MSM chemsex research has evolved over the last decade, globally, and their methodological approaches and focus with respect to choice of MSM population, operationalization of chemsex, health outcomes, and other variables that may or may not be associated with chemsex. Such an analysis, which effectively both builds on and extends the work of existing reviews on chemsex, can offer important insights and a more diverse understanding of the chemsex-phenomenon and research thereof, and provide practitioners, researchers, and policymakers a foundation from which to advance in follow-up research.
To this end, we aimed to identify all research on chemsex among MSM, irrespective of study location or publication language, published between January 2010 and March 2020, and describe the research with respect to location, publication year, eligibility criteria, recruitment arena, chemsex operationalization, and choice of variables that could be associated with chemsex among MSM.
Methods
The systematic scoping review methodology
We followed the guidelines in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., Citation2019) when defining the review question, searching for studies, selecting studies, and extracting data from eligible studies. We also followed Arksey and O’Malley’s (Arksey & O’Malley, Citation2005) and Levac et al.’s (Levac et al., Citation2010) guidelines for scoping reviews and described our approach in a protocol, which we registered in the CRISTIN database (2058820). We report in accordance with the PRISMA-ScR reporting guideline (Tricco et al., Citation2018).
Inclusion criteria
First, we required chemsex to be the main focus of the study. We also required quantitative studies to specify a chemsex-variable that included at least one of the following eight drugs: GHB/GBL, stimulants (amphetamine, crystal meth, ecstasy/MDMA, cathinones including mephedrone, powder cocaine, crack cocaine), and ketamine. We chose to include these drugs in our operationalization of chemsex, because their use with sex had been defined and labeled as chemsex in previous studies. (Evers, Hoebe et al., Citation2019; Glynn et al., Citation2018; Gonzalez-Baeza et al., Citation2018; Skryabin et al., Citation2020;Van Hout et al., Citation2019).
Second, we included empirical research, meaning the record of someone’s preplanned examination, observation, or experiences, to gain new knowledge and/or test existing knowledge, that includes a description of the methods for data collection and analysis (Goodwin, Citation2005). We included both quantitative and/or qualitative primary research, but not reviews.
Third, eligible studies were published in 2010 or later. This was based on the observation that chemsex practices among MSM fundamentally changed after the emergence of geosexual networking apps such as Grindr since 2009 (Deimel et al., Citation2016; Frankis & Clutterbuck, Citation2017; Tan et al., Citation2018). Smartphone technology has provided technological conditions facilitating relatively anonymous sexual and drug use networking with other MSM within close geographical proximity, through apps that are used globally.
Identifying and selecting relevant studies
We identified eight exemplar studies (Ahmed et al., Citation2016; Glynn et al., Citation2018; Hegazi et al., Citation2017; Melendez-Torres et al., Citation2016; Ottaway et al., Citation2017; Pakianathan, Whittaker, Lee et al., Citation2018; Rich et al., Citation2016; Rosinska et al., Citation2018) from a previous review (Maxwell et al., Citation2019), that met our eligibility criteria. Next, we designed database-specific search strategies that were sensitive enough to find these exemplar studies and similar research, yet specific enough to exclude irrelevant records. The search strategies were designed by a literature search specialist (ER) in collaboration with the other research team members. We searched the following databases: MEDLINE (Ovid), EMBASE (Ovid), PsycINFO (Ovid), Web of Science Core Collection (SCI‐EXPANDED & SSCI) and ProQuest (Sociological Abstracts & Social Services Abstracts). See appendix 1 for the strategy used to search Medline.
The search was carried out in March 2020 (ER). Using Rayyan (Ouzzani et al., Citation2016), two researchers (EA and RB/AEM/VS) independently assessed all study titles and abstracts from the search against the inclusion criteria. In EPPI-Reviewer 4 (Thomas et al., Citation2020) we independently assessed full texts of studies that were deemed potentially relevant in the title/abstract screening, against the same inclusion criteria. If the two researchers disagreed on the inclusion of a study based on their title/abstract or full text, a third researcher was consulted.
Data extraction
One researcher (EA) extracted data from the included studies, using a pre-designed data extraction form. The extraction form was piloted on 20 studies. A second researcher (RB/AEM/VS) checked the accuracy and completeness of the extraction. Disagreements were resolved by reexamining the full study text and subsequent discussion. When necessary data were missing, we contacted study authors to obtain it. We received clarifications from authors of 15 publications (Drysdale et al., Citation2020; Feinstein et al., Citation2018; Friedman et al., Citation2014; Hegazi et al., Citation2017; Khaw et al., Citation2018; Mohammed et al., Citation2016; Pakianathan, Whittaker, Avery et al., Citation2018; Pakianathan, Whittaker, Lee et al., Citation2018; Schecke et al., Citation2019; Sewell et al., Citation2019; Souleymanov et al., Citation2019; Torres et al., Citation2020; Turner et al., Citation2015; Van Hout et al., Citation2019; Wong et al., Citation2020).
Based on the type of method used to analyze possible meanings of chemsex to MSM health, we classified each included study into one of the following mutually exclusive study categories: i) “Qualitative studies,” ii) “Frequency studies,” meaning quantitative studies with no association analysis of chemsex, iii) Association studies regarding chemsex, meaning quantitative studies with association analyses of chemsex, as operationalized in this review among MSM (labeled “MSM Chemsex Association studies”). iv) Association studies not specific to chemsex or MSM, meaning quantitative studies with association analyses of drug use with sex more generally, including other drugs than the operationalization of chemsex chosen for this review, or including <90% MSM in the analysis (labeled “Wider Association studies”), and v) Longitudinal studies, meaning quantitative studies collecting measures of chemsex-engagement at two or more time points from the same individuals.
Our extraction also included: time of publication, study location, sample size, age of participants, participants’ HIV status, recruitment arena, study eligibility criteria, operationalizations of chemsex (as stated in eligibility criteria or when reporting chemsex occurrence), and variable categories that researchers have tested for possible associations with chemsex: STI health, HIV health, sexological health, drug health, mental health and other health, relational factors, societal homonegativity-related factors, and behaviors. Appendix 2 describes the construction of these variables.
Analysis
We performed descriptive analyses in Stata (StataCorp, Citation2019), such as determining study and participant frequencies.
In summarizing the extracted data frequencies graphically, we sought to minimize the risk of reporting our data in a way that could exaggerate or understate differences and tendencies across the studies. One way to do so was to express results in terms of both number of studies and number of MSM participants. We made descriptive bar chart figures with Python v3.8.5 and the Matplotlib library v3.3.2.
For the purpose of our analysis, we created an aggregated “health” variable, in order to differentiate studies that did or did not consider chemsex against MSM health in cross-tabulations or statistical association analyses (see Appendix 2). Studies from more than one country were classified as such, and were not included when registering the locations of individual studies.
Consultation with stakeholders
For this optional step (Arksey & O’Malley, Citation2005), we shared and discussed the study protocol with the Norwegian HIV patient organization (HivNorge), and a queer chemsex user harm reduction organization (Chemfriendly Norge). The feedback was overall positive and resulted in one minor edit to our study protocol: to register which included studies required potential participants to have previous experience of sex work to participate. None of the included studies included sex work in their eligibility criteria.
Online evidence and gap map of research
In order to increase accessibility to primary research about chemsex among MSM—for researchers, health workers, MSM, and the general public—we created online research evidence and gap maps of the studies reviewed. The interactive maps provide reference lists to groups of included studies that share study characteristics reported in our publication. They can be accessed via www.chemsexevidence.com.
Results
The search identified 14,092 records (), of which 7,055 remained after removing duplicates. Of these, we assessed 538 full-texts, and included 108 studies in our scoping review (listed in Appendix 3). Most of the included studies were published as journal articles (81%), 4% as dissertations, 12% as conference abstracts, 2% as letters to editors and 1% as book chapters. One study text was written in Spanish, one in French, and the rest in English. We classified 24% of studies as Qualitative, 16% as Frequency, 41% as MSM Chemsex association, 13% as Wider association, and 6% as Longitudinal studies. illustrates how many studies from the seven study design categories were placed in each of the five study categories. Ten studies, all qualitative, described intentions to produce knowledge about underlying drivers of chemsex, while eight studies described an intention to examine consequences of chemsex, of which one was longitudinal.
Figure 1. Modified Prisma flow chart of the selection process.
Publication timing
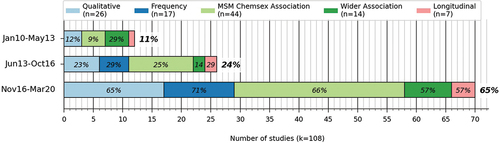
When comparing how many studies were published in three equally long time periods since January 2010, research activity on chemsex increased between 2010 and 2020 (). The number of publications increased by 117% from the first to the second time period, and by another 169% from the second to the third period. From the first to the third period, the increase was nearly fivefold (483%). The pattern was similar across study categories.
Participants
Number of MSM participants
shows the median sample sizes and total number of MSM study participants in each of the five mutually exclusive study categories, and could be established for 91 of the 93 samples identified. Nine samples were used in 25 different publications, and two of these contributed to studies in more than one of the five mutually exclusive study categories. The remaining 84 samples contributed to one publication each.
Table 1. Number of MSM participants.
Study locations
The 108 included studies were from 23 different countries (). 87% of studies were North American, European, or Australian, and these included 79% of MSM participants. The US was represented by 29% of studies (21% of MSM participants), the UK by 23% of studies (21% of MSM participants), the Netherlands by 7% of studies (20% of MSM participants), and finally Australia by 7% of studies (5% of MSM participants). Concerning non-Western study locations, 10% of studies and 8% of MSM participants were from Asia, 1% of studies and 2% of MSM participants from Latin America & the Caribbean, and there were no studies at all from Africa. 9% of studies and 5% of MSM participants were from countries classified as middle-income economies by the World Bank (World Bank Country and Lending Groups, Citation2020).
Table 2. Study locations of the included studies.
Recruitment arenas
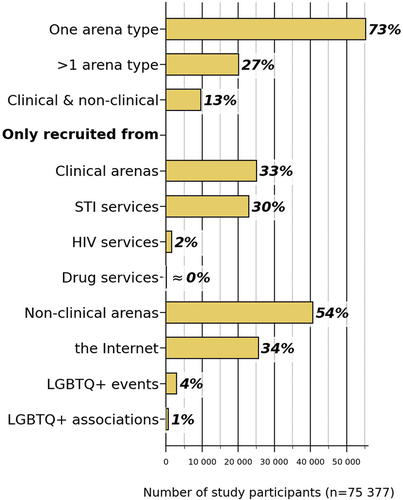
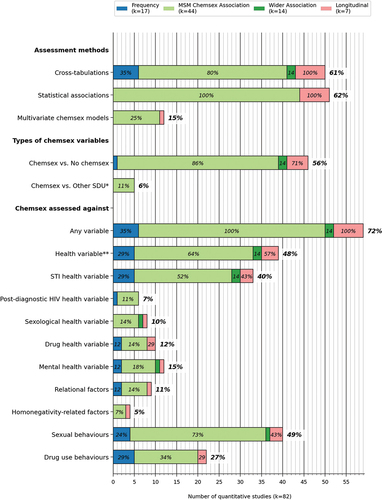
About one-third of the studies (34%) recruited samples from several types of recruitment arenas (), and the mean number of arena types among studies with >1 type was 3.2. Regarding differences in recruitment arenas among study categories, there was a tendency to recruit from >1 arena type among the qualitative and longitudinal studies.
Figure 3. Recruitment arenas of the included studies (by number of studies). All numbers within each bar denote proportions of studies within the same study category. All numbers to the right of each bar denote proportions of all studies.
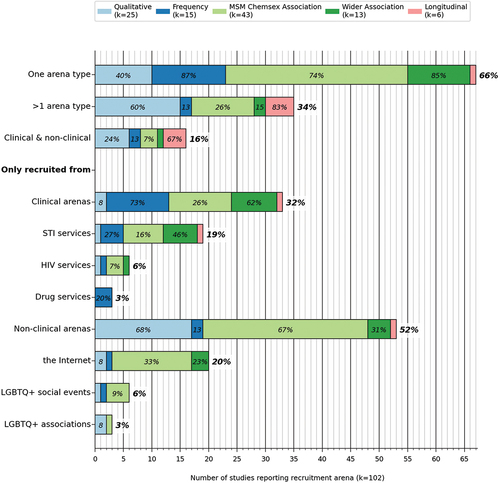
Roughly half (52%) of studies, with 54% of MSM participants, recruited exclusively from non-clinical arenas such as the Internet and/or LGBTQ+ social events/associations (). About one-third (32%) of studies recruited their MSM participants exclusively from clinical arenas (33% of all MSM participants), among which STI clinics dominated (19% of studies, 30% of all MSM participants). Exclusive use of HIV clinics (6% of studies, 2% of all MSM participants) or drug services clinics (3% of studies, <1% of all MSM participants) to recruit study participants was less common. No studies recruited participants via mental- or sexological health services.
Study-level eligibility criteria
About 1 in 5 studies (18%) required previous chemsex engagement for study participation, and these included only 1% of all MSM participants (). Nine percent of studies (4% of all MSM participants) had as an eligibility criteria positive HIV status, and even fewer studies (2%, n = 257) recruited specifically MSM participants with positive HIV status, who at the same time had also engaged in chemsex. 13% of studies required negative HIV status, including four of the seven longitudinal studies. A small number of studies (4%) made drug health-related requirements for participation, such as a previously confirmed clinical diagnosis in drug health, screening scores indicating a high probability of a drug health diagnosis, or having received health services to address a clinical drug health condition. No studies specified mental or sexological health parameters as eligibility criteria.
Figure 5. Eligibility criteria of the included studies (by number of studies). SDU* = use of other drugs with sex than GHB/GBL, stimulants (amphetamine, crystal meth, ecstasy/MDMA, cathinones, cocaine) and/or ketamine. Drug health** = relating to symptoms, diagnoses, follow-up, prognosis/complications of drug health condition in ICD-11. Proportions: all numbers within each bar denote proportion of studies within the same category. All numbers to the right of each bar denote proportion of all studies reporting eligibility criteria.
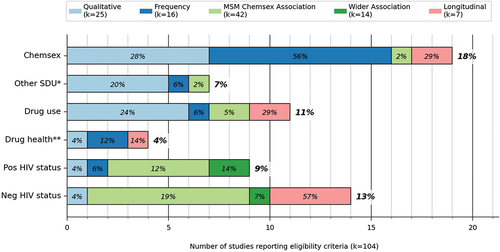
Figure 6. Eligibility criteria of the included studies (by number MSM study participants).
Operationalizations of chemsex
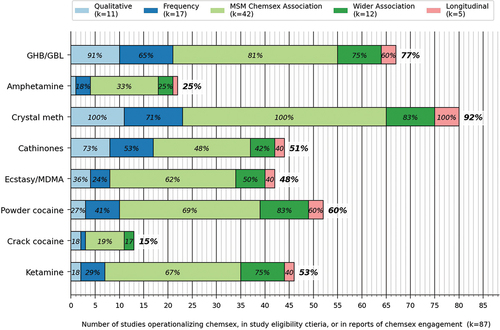
The large majority of our included studies operationalized chemsex as part of their eligibility criteria or when reporting occurrence of chemsex (81%, k = 87). The remaining studies included multi-drug operationalizations including other drugs in addition to either GHB/GBL, stimulants (amphetamine, crystal meth, synthetic cathinones, ecstasy/MDMA, powder cocaine, crack cocaine) or ketamine (6%, k = 6), or none at all (14%, k = 15) (not shown). We registered a total of 32 different multi-drug operationalizations, involving two to eight chemsex drugs. shows the extent to which each of the eight chemsex drugs were included in chemsex operationalizations, among the studies that included at least one such operationalization. The two drugs most frequently used in chemsex operationalizations were crystal meth (92%) and GHB/GBL (77%), while the least frequent drugs used were crack cocaine (15%) and amphetamine (25%). One-quarter (k = 22) of the studies with chemsex operationalizations collected data about chemsex engagement in the last 1–3 months, 18% (k = 16) in the last 4–6 months, and 28% (k = 24) in the last year (not shown).
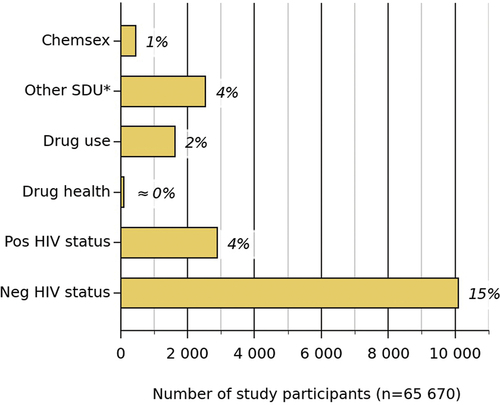
Variables in cross-tabulations and statistical association analyses of chemsex
About three-quarters (72%, k = 59) of the 82 quantitative studies considered possible associations between chemsex and other variables through cross-tabulations or statistical association analyses, although only 15% (k = 12) of the same 82 studies were multivariate analyses of chemsex (). About half of the quantitative studies (48%, k = 39) examined possible associations between chemsex and health variables in cross-tabulations or statistical association analyses. Associations with STI health (k = 33, 40%) was examined about five times more frequently than associations with post-diagnostic HIV health (7%, k = 6), four times more frequently than sexological health (10%, k = 8), and three times more frequently than mental health (15%, k = 12). A small number of studies assessed the association of chemsex and relational factors (11%) and/or homonegativity-related factors (5%).
Figure 8. Quantitative assessments of chemsex against other variables. Numbers within each bar denote proportion of all quantitative studies within the same category. Numbers to the right of each bar denote proportion of all quantitative studies included in the review.
Only five of the 82 quantitative studies compared the health profiles of MSM engaging in different kinds of sexualized drug use, including chemsex. (). Two studies examined differences specifically in health levels among MSM who use different drugs with sex. The first one tested whether MSM who use crystal meth with sex, compared to MSM who use other drugs than crystal meth with sex (including alcohol), experienced poorer STI, mental and/or drug health outcomes (Pakianathan, Whittaker, Avery et al., Citation2018). In addition to health outcomes, the same study considered differences in work and financial impacts between these two groups of MSM. The second study examined whether sexological, mental or STI health differences existed between MSM using GHB/GBL, crystal meth, synthetic cathinones or ketamine with sex, and MSM using other drugs than these with sex (including alcohol; Hibbert et al., Citation2019). The single case-control study we included in the review assessed whether chemsex engagement in the last year differed between MSM with positive HIV status who had or had not recently been diagnosed with acute Shigellosis—a gastroenteric infection that can transmit sexually (Wu et al., Citation2019). Finally, we mention that among the seven longitudinal studies, one analyzed associations between an STI health outcome and chemsex engagement over time (Piyaraj, Citation2014). Three studies analyzed changes to one or more health variables over time, as well as changes to chemsex-engagement over time, but did not assess how changes to chemsex-engagement and health may relate to one another over time (Lyons et al., Citation2014; Mimiaga et al., Citation2019; Santos et al., Citation2014). The remaining three longitudinal studies did not consider changes to any health outcomes over time, focusing instead on behavior rather than health (Coyer et al., Citation2019; Reback et al., Citation2019; Sewell et al., Citation2019).
Discussion
Our systematic scoping review identified a number of characteristics of the rich body of chemsex research among MSM, consisting of 108 studies, 93 samples and about77000MSM from 23 different countries. We found that research activity on chemsex among MSM has increased since 2010, with two-thirds of the studies coming from either the US, the UK, the Netherlands, or Australia. The majority (62%) of the quantitative studies examined statistical associations with chemsex, while 24% of all included studies were qualitative.
We analyzed study locations and found that almost all studies of chemsex among MSM are from Europe, North America, or Australia, or from high-income economies outside these regions. With at least four understudied geographical MSM sub-populations in relation to chemsex, we recommend more chemsex research among MSM from Asia, Africa, and Latin America/the Caribbean, as well as in non-high-income countries in Europe. We recognize that one possible reason for the lack of traction regarding research on chemsex among MSM in these areas may be related to low societal acceptance of LGBTQ+ individuals. By comparing data from MSM who live in different cultural contexts, interactions between cultural factors and possible associations between chemsex and health outcomes can be assessed. For instance, societal homonegativity or relational factors could be measured in different cultural locations, and then incorporated into a cross-cultural international analysis of how they modify associations between chemsex and health outcomes. In their systematic review of chemsex among LGBTQ+ in relation to sexual health outcomes, Hibbert and colleagues call for an increase in international studies (Hibbert et al., Citation2021).
We examined how chemsex was operationalized in the literature and found that few studies examined or tested different drug-specific definitions of chemsex. We did not register any operationalization of chemsex in 19% of the included studies, and among the remaining 81%, we registered 40 different chemsex operationalizations. Of these, almost all included crystal meth and most included GHB/GBL. Relatively few operationalizations included crack cocaine or amphetamine. This suggests that researchers of chemsex among MSM consider the sexualized use of drugs such as crystal meth and GHB/GBL to be more relevant to MSM life and health than sexualized use of amphetamine. Moreover, 32 of the 40 operationalizations were multi-drug operationalizations of chemsex, and there was a tendency to use these to study possible associations between chemsex and health outcomes. As multi-drug variables do not allow for exploration of possible associations between chemsex and health on a drug-by-drug basis, it seems critical to start examining further the potential health differences and similarities between sexualized use of drugs such as amphetamine and crystal meth, or even GHB/GBL and crystal meth. Registering the individual drugs that each study participant in primary studies use with sex would allow for such examinations, and possibly reduce the risk of erroneously considering different drugs used with sex as equivalent to one another. Lafortune and colleagues note in their review that future latent class analyses are likely to reveal multiple profiles of sexual and non-sexual substance use among MSM, as well as their interplay with other variables (Lafortune et al., Citation2021), and we support that. As advanced statistical methods are being developed to meta-analyze structural equation models, it may be possible to aggregate such profiles across studies in a future review (Cheung, Citation2015). In consideration of future low-threshold or harm reduction-based programs, MSM who wish to minimize health risks of chemsex would benefit from information about differences in health risks, depending on which drug is being used for chemsex.
Regarding focus of the included studies, we found that most of them had an individualistic focus, generally examining the possible associations between chemsex and presumed subsequent health drivers, outcomes, or behaviors. Many of these studies focused on the possible link between chemsex and STI health (including HIV status), which corresponds well with the high number of clinical studies recruiting from STI-clinics. Conversely, few studies explored possible associations between chemsex and sexological, drug, mental or post-diagnostic HIV health, relational factors, or experienced or internalized homonegativity. Similarly, none of the studies reviewed had recruited their participants through sexological or mental health clinical services, and relatively few studies had recruited through HIV (6%) and drug clinics (3%). None of the seven longitudinal studies considered changes in sexological or mental health against chemsex engagement over time, while the proportions of quantitative studies considering possible associations between chemsex and sexological (10%) and mental health outcomes (15%) were relatively low. From this we infer that researchers of chemsex among MSM have generally not designed their studies based on narratives proposing that MSM may engage in chemsex to reverse dysfunctions within sexological and/or mental health. Nor have they framed their research in line with theories such as the minority stress model, a research focus tendency highlighted by others as well (Bohn, Sander, Kohler et al., Citation2020a; Lafortune et al., Citation2021). We encourage additional consideration of the role of societal factors on chemsex, the possible interactions between co-occurring epidemics among MSM and societal homonegativity, and additional studies that assess associations between chemsex and levels of STI, sexological, drug, and mental health simultaneously.
Qualitative study findings suggest that some MSM with positive HIV status cope with sexological and mental health reductions caused by HIV stigma, by engaging in chemsex (Ahmed et al., Citation2016; Lafortune et al., Citation2021). Quantitative studies have found positive statistical associations between chemsex and HIV status among MSM (Bourne et al., Citation2014; Desai et al., Citation2018; Edmundson et al., Citation2018; Glynn et al., Citation2018; Graf et al., Citation2018; Hegazi et al., Citation2017; Ostrow et al., Citation2009; Pakianathan, Whittaker, Lee et al., Citation2018; Stevens et al., Citation2020; Tomkins et al., Citation2018). However, we only identified one quantitative study of chemsex among MSM that explored causal dynamics between these two variables. At this time, there seems to be scope for additional qualitative studies and eventually a qualitative evidence synthesis on the role of mental and/or sexological health in driving chemsex engagement among MSM generally, as well as specifically among MSM with positive HIV status, and MSM with clinical sexological or mental health needs. In addition to the already mentioned low proportion (6%) of studies recruiting exclusively from HIV clinics, relatively few (9%) studies required positive HIV status from participants, and only 7% of quantitative studies considered chemsex against post-diagnostic HIV health in cross-tabulations or association analyses. All three findings highlight the scope that exists for additional chemsex studies particularly among MSM with positive HIV status. Further, given that 62% of the studies had a cross-sectional design, more longitudinal and large-scale studies are needed to address health drivers and consequences of chemsex, and changes to levels of chemsex-engagement over time. With regard to experimental study designs, the few intervention studies related to chemsex suggest an important area of future research. Among the seven longitudinal studies in the review, four required negative HIV status for participation and none required positive HIV status. In addition to the implied concern for management of HIV transmission risk when engaging in chemsex, it would be useful with studies that spotlight changes to health over time among MSM with positive HIV status ().
Table 3. Proposed research agenda resulting from this systematic scoping review.
Strengths and limitations
We employed clear inclusion criteria and a systematic process for identifying relevant studies in any publication form. We used duplicate screening, data extraction by a second reviewer, and fit for purpose data analyses. The diverse skill set, experiences, and individual characteristics of the author group were a strength and included sexual and gender identity, age, profession, clinical experience, and experience in drug and MSM research. However, it is likely that gray literature could have been missed, and once new research is done, also systematic scoping reviews become outdated. In contrast to intervention reviews, for scoping reviews this is probably a minor problem, as it is unlikely that a handful of additional studies would change the results of the scoping.
Nonetheless, since our systematic literature search, we observe that a number of new studies on chemsex have been published, that would likely meet our inclusion criteria. While we have not systematically assessed these, we reference a handful below and note that they seem to strengthen our findings, in that they are primarily from high-income countries (Curtis et al., Citation2020; Demant et al., Citation2022; Drückler et al., Citation2021), and have an individualistic focus, typically analyzing the possible associations between chemsex and presumed health drivers (Z. Wang et al., Citation2020), outcomes such as STI/HIV (Adler et al., Citation2022; Flores Anato et al., Citation2022; MacGregor et al., Citation2021), or behaviors (Drückler et al., Citation2021; Whitlock et al., Citation2021). This includes a few studies on drug dependency (Li et al., Citation2021), overdoses, also with fatal outcome, from chemsex use (Batisse et al., Citation2022; Cartiser et al., Citation2021; Drevin et al., Citation2021) and drug-drug interactions (De La Mora et al., Citation2022; Lee et al., Citation2021), and a few more cross-sectional and qualitative studies on drug health more generally (De La Mora et al., Citation2022; Peyriere et al., Citation2022). A study on psychological attachment style, emotional regulation and adverse childhood experiences relation to chemsex was published after our literature search was carried out (González-Baeza et al., Citation2022), in addition to other studies exploring different aspects of mental health in relation to chemsex (Batisse et al., Citation2022; Bohn, Sander, Köhler et al., Citation2020b; Gavín et al., Citation2021; Knoops et al., Citation2022; Tan, O’Hara et al., Citation2021). Relational factors (Herrijgers et al., Citation2020; Nagington & King, Citation2022), and homonegativity-related factors (Tan, Phua et al., Citation2021; Uholyeva & Pitoňák, Citation2022) are also covered in the published chemsex literature since March 2020. Recently, chemsex and possible interactions with new health challenges such as COVID-19 and mpox (previously known as monkeypox) have also started being explored (Ringshall et al., Citation2022; Roux et al., Citation2022; H. Wang et al., Citation2022), with for example, one study finding that the likelihood of practicing chemsex increased with use of PrEP to prevent COVID-19 transmission (Chone et al., Citation2021).
Conclusion
We carried out a systematic scoping review of chemsex among MSM within the last decade, and analyzed how researchers study chemsex among MSM, rather than summarizing study findings. There has been an increase in empirical research on this topic, but most research is among MSM communities in the West or other high-income locations, cross-sectional, and in the area of STI health correlates and behaviors. We identified several knowledge gaps that can be attributed directly to the methodological choices made by researchers, and we encourage future research to address those gaps.
Supplemental Material
Download MS Word (108.7 KB)Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplemental data
Supplemental data for this article can be accessed online at https://doi.org/10.1080/00918369.2023.2170757.
Additional information
Funding
References
- Adler, Z., Fitzpatrick, C., Broadwell, N., Churchill, D., & Richardson, D. (2022). Chemsex and antiretroviral prescribing in an HIV cohort in Brighton, UK. HIV Medicine, 23(7), 797–800. https://doi.org/10.1111/hiv.13239
- Ahmed, A. K., Weatherburn, P., Reid, D., Hickson, F., Torres-Rueda, S., Steinberg, P., & Bourne, A. (2016). Social norms related to combining drugs and sex (“chemsex”) among gay men in South London. International Journal of Drug Policy, 38, 29–35. https://doi.org/10.1016/j.drugpo.2016.10.007
- Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616
- Ballesteros-López, J., Molina-Prado, R., Rodríguez-Salgado, B., Martin-Herrero, J. L., & Dolengevich-Segal, H. (2016). Mephedrone and chemsex. A descriptive analysis of a sample of patients in Madrid. Revista Española de Drogodependencias, 41(4), 47–61. https://www.aesed.com/upload/files/vol-41/n-4/v41n4_chemsex.pdf
- Batisse, A., Eiden, C., Deheul, S., Monzon, E., Djezzar, S., & Peyrière, H. (2022). Chemsex practice in France: An update in Addictovigilance data. Fundamental & Clinical Pharmacology, 36(2), 397–404. https://doi.org/10.1111/fcp.12725
- Bohn, A., Sander, D., Kohler, T., Hees, N., Oswald, F., Scherbaum, N., Deimel, D., & Schecke, H. (2020a). Chemsex and mental health of men who have sex with men in Germany. Frontiers in Psychiatry, 11, 1–10. https://doi.org/10.3389/fpsyt.2020.542301
- Bohn, A., Sander, D., Köhler, T., Hees, N., Oswald, F., Scherbaum, N., Deimel, D., & Schecke, H. (2020b). Chemsex and mental health of men who have sex with men in Germany. Frontiers in Psychiatry / Frontiers Research Foundation, 11, 542301. https://doi.org/10.3389/fpsyt.2020.542301
- Bourne A, Reid D, Hickson F, Torres-Rueda S, Steinberg P and Weatherburn P. (2015). “Chemsex” and harm reduction need among gay men in South London. International Journal of Drug Policy, 26(12), 1171–1176. 10.1016/j.drugpo.2015.07.013
- Bourne, A., Reid, D., Hickson, F., Torres Rueda, S., & Weatherburn, P. (2014). The chemsex study: Drug use in sexual settings among gay and bisexual men in Lambeth, Southward & Lewisham [Sigma Research, London School of Hygiene & Tropical Medicine]. https://sigmaresearch.org.uk/reports/item/report2014a
- Bourne, A., Reid, D., Hickson, F., Torres-Rueda, S., & Weatherburn, P. (2015). Illicit drug use in sexual settings (‘chemsex’) and HIV/STI transmission risk behaviour among gay men in South London: Findings from a qualitative study. Sexually Transmitted Infections, 91(8), 564–568. https://doi.org/10.1136/sextrans-2015-052052
- Bryant, J., Hopwood, M., Dowsett, G. W., Aggleton, P., Holt, M., Lea, T., Drysdale, K., & Treloar, C. (2018). The rush to risk when interrogating the relationship between methamphetamine use and sexual practice among gay and bisexual men. International Journal of Drug Policy, 55, 242–248. https://doi.org/10.1016/j.drugpo.2017.12.010
- Cartiser, N., Sahy, A., Advenier, A. S., Franchi, A., Revelut, K., Bottinelli, C., Bévalot, F., & Fanton, L. (2021). Fatal intoxication involving 4-methylpentedrone (4-MPD) in a context of chemsex. Forensic Science International, 319, 110659. https://doi.org/10.1016/j.forsciint.2020.110659
- Cheung, M. W.-L. (2015). Meta-analysis: A structural equation modeling approach. John Wiley & Sons.
- Chone, J. S., Lima, S., Fronteira, I., Mendes, I. A. C., Shaaban, A. N., Martins, M., & Sousa, Á. F. L. (2021). Factors associated with chemsex in Portugal during the COVID-19 pandemic. Revista Latino-Americana de Enfermagem, 29, e3474. https://doi.org/10.1590/1518-8345.4975.3474
- Coyer, L., Boyd, A., Davidovich, U., Prins, M., & Matser, A. (2019). P544 Trends in recreational drug use and associations with CAS, HIV and STI among HIV negative MSM in Amsterdam between 2008-2017. Sexually Transmitted Infections, 95(Suppl 1), A246. https://doi.org/10.1136/sextrans-2019-sti.619
- Curtis, T. J., Rodger, A. J., Burns, F., Nardone, A., Copas, A., & Wayal, S. (2020). Patterns of sexualised recreational drug use and its association with risk behaviours and sexual health outcomes in men who have sex with men in London, UK: A comparison of cross-sectional studies conducted in 2013 and 2016. Sexually Transmitted Infections, 96(3), 197–203. https://doi.org/10.1136/sextrans-2019-054139
- Deimel, D., Stover, H., Hosselbarth, S., Dichtl, A., Graf, N., & Gebhardt, V. (2016). Drug use and health behaviour among German men who have sex with men: Results of a qualitative, multi-centre study. Harm Reduction Journal, 13(36), 1–11. https://doi.org/10.1186/s12954-016-0125-y
- De La Mora, L., Nebot, M. J., Martinez-Rebollar, M., De Lazzari, E., Tuset, M., Laguno, M., Ambrosioni, J., Miquel, L., Blanch, J., Ugarte, A., Torres, B., González-Cordón, A., Inciarte, A., Chivite, I., Short, D., Salgado, E., Martinez, E., Blanco, J. L., & Mallolas, J. (2022). Do ART and chemsex drugs get along? Potential drug-drug interactions in a cohort of people living with HIV who engaged in chemsex: A retrospective observational study. Infectious Diseases and Therapy, 11(6), 2111–2124. https://doi.org/10.1007/s40121-022-00694-w
- Demant, D., Carroll, J. A., Saliba, B., & Bourne, A. (2022). Information-seeking behaviours in Australian sexual minority men engaged in chemsex. Addictive Behaviors Reports, 16, 100399. https://doi.org/10.1016/j.abrep.2021.100399
- Desai, M., Bourne, A., Hope, V., & Halkitis, P. (2018). Sexualised drug use: LGTB communities and beyond. International Journal of Drug Policy, 55, 128–130. https://doi.org/10.1016/j.drugpo.2018.04.015
- Dolengevich-Segal, H., Gonzalez-Baeza, A., Valencia, J., Valencia-Ortega, E., Cabello, A., Tellez-Molina, M. J., Perez-Elias, M. J., Serrano, R., Perez-Latorre, L., Martin-Carbonero, L., Arponen, S., Sanz-Moreno, J., Fuente, S. D. L., Bisbal, O., Santos, I., Casado, J. L., Troya, J., Cervero-Jimenez, M., Nistal, S., & Ryan, P. (2019). Drug-related and psychopathological symptoms in HIV-positive men who have sex with men who inject drugs during sex (slamsex): Data from the U-SEX GESIda 9416 study. PLoS ONE, 14(12), Article e0220272. https://doi.org/10.1371/journal.pone.0220272
- Donnadieu-Rigole, H., Peyriere, H., Benyamina, A., & Karila, L. (2020). Complications related to sexualized drug use: What can we learn from literature? Frontiers in Neuroscience, 14, 1–8. https://doi.org/10.3389/fnins.2020.548704
- Drevin, G., Rossi, L. H., Férec, S., Briet, M., & Abbara, C. (2021). Chemsex/slamsex-related intoxications: A case report involving gamma-hydroxybutyrate (GHB) and 3-methylmethcathinone (3-MMC) and a review of the literature. Forensic Science International, 321, 110743. https://doi.org/10.1016/j.forsciint.2021.110743
- Drückler, S., Speulman, J., van Rooijen, M., & De Vries, H. J. C. (2021). Sexual consent and chemsex: A quantitative study on sexualised drug use and non-consensual sex among men who have sex with men in Amsterdam, the Netherlands. Sexually Transmitted Infections, 97(4), 268–275. https://doi.org/10.1136/sextrans-2020-054840
- Drückler, S., Van Rooijen, M. S., & De Vries, H. J. C. (2018). Chemsex among men who have sex with men: A sexualized drug use survey among clients of the sexually transmitted infection outpatient clinic and users of a gay dating app in Amsterdam, the Netherlands. Sexually Transmitted Diseases, 45(5), 325–331. https://doi.org/10.1097/OLQ.0000000000000753
- Drysdale, K., Bryant, J., Holt, M., Hopwood, M., Dowsett, G. W., Aggleton, P., Lea, T., & Treloar, C. (2020). Destabilising the ‘problem’ of chemsex: Diversity in settings, relations and practices revealed in Australian gay and bisexual men’s crystal methamphetamine use. International Journal of Drug Policy, 78, 1–8. https://doi.org/10.1016/j.drugpo.2020.102697
- Edmundson, C., Heinsbroek, E., Glass, R., Hope, V., Mohammed, H., White, M., & Desai, M. (2018). Sexualised drug use in the United Kingdom (UK): A review of the literature. International Journal of Drug Policy, 55, 131–148. https://doi.org/10.1016/j.drugpo.2018.02.002
- Evers, Y., Hoebe, C., Dukers-Muijrers, N., Kampman, K., Kuizenga, S., Shilue, D., Bakker, N., Schamp, S., & Van Liere, G. (2019). P519 is chemsex among men who have sex with men perceived as problematic? a cross-sectional study in the Netherlands. Sexually Transmitted Infections, 95(Suppl 1), A237. https://doi.org/10.1136/sextrans-2019-sti.597
- Evers Y J, Van Liere G A, Hoebe C J, Dukers-Muijrers N H and Caylà J A. (2019). Chemsex among men who have sex with men living outside major cities and associations with sexually transmitted infections: A cross-sectional study in the Netherlands. PLoS ONE, 14(5), e0216732 10.1371/journal.pone.021673210.1371/journal.pone.0216732.g00110.1371/journal.pone.0216732.g00210.1371/journal.pone.0216732.t00110.1371/journal.pone.0216732.t00210.1371/journal.pone.0216732.t00310.1371/journal.pone.0216732.s00110.1371/journal.pone.0216732.s002
- Feinstein, B. A., Moody, R. L., John, S. A., Parsons, J. T., & Mustanski, B. (2018). A three-city comparison of drug use and drug use before sex among young men who have sex withmen in the United States. Journal of Gay & Lesbian Social Services, 30(1), 82–101. https://doi.org/10.1080/10538720.2018.1408519
- Flores Anato, J. L., Panagiotoglou, D., Greenwald, Z. R., Blanchette, M., Trottier, C., Vaziri, M., Charest, L., Szabo, J., Thomas, R., & Maheu-Giroux, M. (2022). Chemsex and incidence of sexually transmitted infections among Canadian pre-exposure prophylaxis (PrEP) users in the l’Actuel PrEP Cohort (2013-2020). Sexually Transmitted Infections, 98(8), 549–556. doi:10.1136/sextrans-2021-055215.
- Flores-Aranda, J., Goyette, M., Aubut, V., Blanchette, M., & Pronovost, F. (2019). Let’s talk about chemsex and pleasure: The missing link in chemsex services. Drugs and Alcohol Today, 19(3), 189–196. https://doi.org/10.1108/DAT-10-2018-0045
- Frankis, J., & Clutterbuck, D. (2017). What does the latest research evidence mean for practitioners who work with gay and bisexual men engaging in chemsex? Sexually Transmitted Infections, 93(3), 153–154. https://doi.org/10.1136/sextrans-2016-052783
- Frankis, J., Flowers, P., McDaid, L., & Bourne, A. (2018). Low levels of chemsex among men who have sex with men, but high levels of risk among men who engage in chemsex: Analysis of a cross-sectional online survey across four countries. Sexual Health, 15(2), 144–150. https://doi.org/10.1071/SH17159
- Friedman, M., Kurtz, S. P., Buttram, M. E., Wei, C., Silvestre, A. J., & Stall, R. (2014). HIV risk among substance-using men who have sex with men and women (MSMW): Findings from south Florida. AIDS and Behavior, 18(1), 111–119. https://doi.org/10.1007/s10461-013-0495-z
- Gavín, P., Arbelo, N., Monràs, M., Nuño, L., Bruguera, P., de la Mora, L., Martínez-Rebollar, M., Laguno, M., Blanch, J., & Miquel, L. (2021). Methamphetamine use in chemsex and its consequences on mental health: A descriptive study. Revista espanola de salud publica, 95. (Uso de metanfetamina en el contexto chemsex y sus consecuencias en la salud mental: un estudio descriptivo).
- Glynn, R., Byrne, N., O’Dea, S., Shanley, A., Codd, M., Keenan, E., Ward, M., Igoe, D., & Clarke, S. (2018). Chemsex, risk behaviours and sexually transmitted infections among men who have sex with men in Dublin, Ireland. International Journal of Drug Policy, 52, 9–15. https://doi.org/10.1016/j.drugpo.2017.10.008
- González-Baeza, A., Barrio-Fernández, P., Curto-Ramos, J., Ibarguchi, L., Dolengevich-Segal, H., Cano-Smith, J., Rúa-Cebrián, G., García-Carrillo de Albornoz, A., & Kessel, D. (2022). Understanding attachment, emotional regulation, and childhood adversity and their link to chemsex. Substance Use & Misuse, 1–9. https://doi.org/10.1080/10826084.2022.2148482
- Gonzalez-Baeza, A., Dolengevich-Segal, H., Perez-Valero, I., Cabello, A., Tellez, M. J., Sanz, J., Perez-Latorre, L., Bernardino, J. I., Troya, J., De La Fuente, S., Bisbal, O., Santos, I., Arponen, S., Hontanon, V., Casado, J. L., & Ryan, P. (2018). Sexualized drug use (Chemsex) is associated with high-risk sexual behaviors and sexually transmitted infections in HIV-positive men who have sex with men: data from the U-SEX GESIDA 9416 study. Aids Patient Care and Stds, 32(3), 112–118. https://doi.org/10.1089/apc.2017.0263
- Goodwin, J. (2005). Research in psychology: Methods and design. John Wiley & Sons, Inc.
- Graf, N., Dichtl, A., Deimel, D., Sander, D., & Stover, H. (2018). Chemsex among men who have sex with men in Germany: Motives, consequences and the response of the support system. Sexual Health, 15(2), 151–156. https://doi.org/10.1071/SH17142
- Guerra, F. M., Salway, T. J., Beckett, R., Friedman, L., & Buchan, S. A. (2020). Review of sexualized drug use associated with sexually transmitted and blood-borne infections in gay, bisexual and other men who have sex with men. Drug and Alcohol Dependence, 216, 108237. https://doi.org/10.1016/j.drugalcdep.2020.108237
- Haugstvedt, A., Amundsen, E., & Berg, R. C. (2018). Chemsex among men- a questionnaire study. Tidsskrift for Den Norske Laegeforening, 138(13), 1244–1250. https://doi.org/10.4045/tidsskr.18.0108
- Hegazi, A., Lee, M. J., Whittaker, W., Green, S., Simms, R., Cutts, R., Nagington, M., Nathan, B., & Pakianathan, M. R. (2017). Chemsex and the city: Sexualised substance use in gay bisexual and other men who have sex with men attending sexual health clinics. International Journal of STD & AIDS, 28(4), 362–366. https://doi.org/10.1177/0956462416651229
- Herrijgers, C., Poels, K., Vandebosch, H., Platteau, T., van Lankveld, J., & Florence, E. (2020). Harm reduction practices and needs in a Belgian chemsex context: Findings from a qualitative study. International Journal of Environmental Research and Public Health, 17(23), 9081. https://doi.org/10.3390/ijerph17239081
- Hibbert, M. P., Brett, C. E., Porcellato, L. A., & Hope, V. D. (2019). Psychosocial and sexual characteristics associated with sexualised drug use and chemsex among men who have sex with men (MSM) in the UK. Sexually Transmitted Infections, 95(5), 342–350. https://doi.org/10.1136/sextrans-2018-053933
- Hibbert, M. P., Hillis, A., Brett, C. E., Porcellato, L. A., & Hope, V. D. (2021). A narrative systematic review of sexualised drug use and sexual health outcomes among LGBT people. International Journal of Drug Policy, 93, 1–9. https://doi.org/10.1016/j.drugpo.2021.103187
- Higgins, J., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M., & Welch, V. (2019). Cochrane handbook for systematic reviews of interventions version (2nd ed.). John Wiley & Sons.
- Khaw, C., Raw, L., Zablotska-Manos, I., & Boyd, M. (2018). P77 Chemsex: Prevalence, characteristics and associated risk profiles of men who have sex with men in South Australia. A cross-sectional cohort study. HIV Medicine, 19(Suppl 2), S46. https://doi.org/10.1111/hiv.12613
- King, M., Semlyen, J., Tai, S., Killaspy, H., Osborn, D., Popelyuk, D., & Nazareth, I. (2008). A systematic review of mental disorder, suicide and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 8(70). https://doi.org/10.1186/1471-244X-8-70
- Knoops, L., Bakker, I., van Bodegom, R., & Zantkuijl, P. (2015). Tina and slamming: MSM, crystal meth and intravenous drug use in a sexual setting. Mainline, Soa Aids Netherlands.
- Knoops, L., van Amsterdam, J., Albers, T., Brunt, T. M., & van den Brink, W. (2022). Slamsex in The Netherlands among men who have sex with men (MSM): Use patterns, motives, and adverse effects. Sexual Health, 19(6), 566–573. https://doi.org/10.1071/sh22140
- Lafortune, D., Blais, M., Miller, G., Dion, L., Lalonde, F., & Dargis, L. (2021). Psychological and interpersonal factors associated with sexualized drug use among men who have sex with men: A mixed-methods systematic review. Archives of Sexual Behavior, 50(2), 427–460. https://doi.org/10.1007/s10508-020-01741-8
- Lee, C. Y., Wu, P. H., Chen, T. C., & Lu, P. L. (2021). Changing pattern of chemsex drug use among newly diagnosed HIV-positive Taiwanese from 2015 to 2020 in the era of treat-all policy. AIDS Patient Care and STDs, 35(4), 134–143. https://doi.org/10.1089/apc.2020.0246
- Levac, D., Colquhoun, H., & O’Brien, K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5(69), 1–9. https://doi.org/10.1186/1748-5908-5-69
- Li, C. W., Ku, S. W., Huang, P., Chen, L. Y., Wei, H. T., Strong, C., & Bourne, A. (2021). Factors associated with methamphetamine dependency among men who have sex with men engaging in chemsex: Findings from the COMeT study in Taiwan. The International Journal on Drug Policy, 93, 103119. https://doi.org/10.1016/j.drugpo.2021.103119
- Lyons, T., Tilmon, S., & Fontaine, Y. (2014). Development of a small-group intervention for stimulant-using men who have sex with men. Journal of Groups in Addiction & Recovery, 9(1), 54–70. https://doi.org/10.1080/1556035X.2014.868724
- MacGregor, L., Kohli, M., Looker, K. J., Hickson, F., Weatherburn, P., Schmidt, A. J., & Turner, K. M. (2021). Chemsex and diagnoses of syphilis, gonorrhoea and chlamydia among men who have sex with men in the UK: A multivariable prediction model using causal inference methodology. Sexually Transmitted Infections, 97(4), 282–289. https://doi.org/10.1136/sextrans-2020-054629
- Maxwell, S., Shahmanesh, M., & Gafos, M. (2019). Chemsex behaviours among men who have sex with men: A systematic review of the literature. International Journal of Drug Policy, 63, 74–89. https://doi.org/10.1016/j.drugpo.2018.11.014
- Melendez-Torres, G. J., Hickson, F., Reid, D., Weatherburn, P., & Bonell, C. (2016). Nested event-level case–Control study of drug use and sexual outcomes in multipartner encounters reported by men who have sex with men. AIDS and Behavior, 20(3), 646–654. https://doi.org/10.1007/s10461-015-1127-6
- Mimiaga, M. J., Pantalone, D. W., Biello, K. B., Hughto, J. M. W., Frank, J., O’Cleirigh, C., Reisner, S. L., Restar, A., Mayer, K. H., & Safren, S. A. (2019). An initial randomized controlled trial of behavioral activation for treatment of concurrent crystal methamphetamine dependence and sexual risk for HIV acquisition among men who have sex with men. AIDS Care - Psychological and Socio-Medical Aspects of AIDS/HIV, 31(9), 1083–1095. https://doi.org/10.1080/09540121.2019.1595518
- Mohammed, H., Were, J., King, C., Furegato, M., Nardone, A., & Hughes, G. (2016). Sexualised drug use in people attending sexual health clinics in England. Sexually Transmitted Infections, 92(6), 454. https://doi.org/10.1136/sextrans-2016-052740
- Nagington, M., & King, S. (2022). Support, care and peer support for gay and bi men engaging in chemsex. Health & Social Care in the Community, 30(6), e6396–e6403. https://doi.org/10.1111/hsc.14081
- Ostrow, D., Plankey, M., Cox, C., Li, X., Shoptaw, S., Jacobson, L., & Stall, R. (2009). Specific sex-drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. Journal of Acquired Immune Deficiency Syndromes, 51(3), 349–355. https://doi.org/10.1097/QAI.0b013e3181a24b20
- Ottaway, Z., Finnerty, F., Amlani, A., Pinto-Sander, N., Szanyi, J., & Richardson, D. (2017). Men who have sex with men diagnosed with a sexually transmitted infection are significantly more likely to engage in sexualised drug use. International Journal of Std & Aids, 28(1), 91–93. https://doi.org/10.1177/0956462416666753
- Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Rayyan-a web and mobile app for systematic reviews. Systematic Reviews, 5(1), 210. https://doi.org/10.1186/s13643-016-0384-4
- Pakianathan, M., Whittaker, W., Avery, J., Henderson, C. C., Ribeiro, L., Lee, M. J., Iqbal, F., & Hegazi, A. (2018). P75 Chemsex with crystal methamphetamine, associated risk-taking and patient-reported adverse consequences. HIV Medicine, 19(S2), S45–S46. https://doi.org/10.1111/hiv.12613
- Pakianathan, M., Whittaker, W., Lee, M. J., Avery, J., Green, S., Nathan, B., & Hegazi, A. (2018). Chemsex and new HIV diagnosis in gay, bisexual and other men who have sex with men attending sexual health clinics. HIV Medicine, 19(7), 485–490. https://doi.org/10.1111/hiv.12629
- Peyriere, H., Jacquet, J. M., Peries, M., Tribout, V., Broche, B., Mauboussin, J. M., Makinson, A., Perrollaz, C., Ferreyra, M., Rouanet, I., Montoya-Ferrer, A., El-Majjaoui, S., Corriol-Bonifas, F., Fraisse, T., Grau, F., Laureillard, D., Nagot, N., Reynes, J., & Donnadieu-Rigole, H. (2022). Chemsex in HIV pre-exposure prophylaxis users: Assessment of mood disorders and addictive behavior. Fundamental & Clinical Pharmacology. https://doi.org/10.1111/fcp.12854
- Piyaraj, P. (2014). The impact of internet use to recruit sex partners and methamphetamine use on incident HIV infection among men who have sex with men in Bangkok, Thailand, 2006-2012. Dissertation Abstracts International: Section B: The Sciences and Engineering, 74(11), 89–112.
- Pufall E, Kall M, Shahmanesh M, Nardone A, Gilson R, Delpech V, Ward H. (2018). Sexualized drug use (‘chemsex’) and high-risk sexual behaviours in HIV-positive men who have sex with men. HIV Med, 19(4), 261–270. https://doi.org/10.1111/hiv.12574
- Reback, C. J., Fletcher, J. B., Swendeman, D. A., & Metzner, M. (2019). Theory-based text-messaging to reduce methamphetamine use and HIV sexual risk behaviors among men who have sex with men: Automated unidirectional delivery outperforms bidirectional peer interactive delivery. AIDS and Behavior, 23(1), 37–47. https://doi.org/10.1007/s10461-018-2225-z
- Rich, A. J., Lachowsky, N. J., Cui, Z., Sereda, P., Lal, A., Birch, R., Montaner, J., Moore, D., Hogg, R. S., & Roth, E. A. (2016). Substance use, sexual behaviour and prevention strategies of Vancouver gay and bisexual men who recently attended group sex events. Culture, Health & Sexuality, 18(4), 361–376. https://doi.org/10.1080/13691058.2015.1084649
- Ringshall, M., Cooper, R., Rawdah, W., Perera, S., Bannister, A., Nichols, K., Fitzpatrick, C., & Richardson, D. (2022). Chemsex, sexual behaviour and STI-PrEP use among HIV-PrEP users during the COVID-19 pandemic in Brighton, UK. Sexually Transmitted Infections, 98(4), 312. https://doi.org/10.1136/sextrans-2021-055216
- Rosinska, M., Gios, L., Nostlinger, C., Vanden Berghe, W., Marcus, U., Schink, S., Sherriff, N., Jones, A. M., Folch, C., Dias, S., Velicko, I., & Mirandola, M. (2018). Prevalence of drug use during sex amongst MSM in Europe: Results from a multi-site bio-behavioural survey. International Journal of Drug Policy, 55, 231–241. https://doi.org/10.1016/j.drugpo.2018.01.002
- Roux, P., Donadille, C., Girard, G., Spire, B., Protière, C., & Velter, A. (2022). Impact of COVID-19 pandemic on men who have sex with men that practice chemsex in France: Results from the national ERAS Web survey. American Journal of Men’s Health, 16(1), 15579883211073225. https://doi.org/10.1177/15579883211073225
- Roux, P., Fressard, L., Suzan-Monti, M., Chas, J., Sagaon-Teyssier, L., Capitant, C., Meyer, L., Tremblay, C., Rojas-Castro, D., Pialoux, G., Molina, J. M., & Spire, B. (2018). Is on-demand HIV pre-exposure prophylaxis a suitable tool for men who have sex with men who practice chemsex? Results from a substudy of the ANRS-IPERGAY trial. Journal of Acquired Immune Deficiency Syndromes, 79(2), e69–e75. https://doi.org/10.1097/QAI.0000000000001781
- Santos, G. M., Coffin, P. O., Vittinghoff, E., DeMicco, E., Das, M., Matheson, T., Raiford, J. L., Carry, M., Colfax, G., Herbst, J. H., & Dilley, J. W. (2014). Substance use and drinking outcomes in personalized cognitive counseling randomized trial for episodic substance-using men who have sex with men. Drug and Alcohol Dependence, 138(1), 234–239. https://doi.org/10.1016/j.drugalcdep.2014.02.015
- Schecke, H., Lea, T., Bohn, A., Kohler, T., Sander, D., Scherbaum, N., & Deimel, D. (2019). Crystal methamphetamine use in sexual settings among german men who have sex with men. Frontiers in Psychiatry, 10. https://doi.org/10.3389/fpsyt.2019.00886
- Sewell, J., Cambiano, V., Speakman, A., Lampe, F. C., Phillips, A., Stuart, D., Gilson, R., Asboe, D., Nwokolo, N., Clarke, A., & Rodger, A. J. (2019). Changes in chemsex and sexual behaviour over time, among a cohort of MSM in London and Brighton: Findings from the AURAH2 study. International Journal of Drug Policy, 68, 54–61. https://doi.org/10.1016/j.drugpo.2019.03.021
- Singer, M. (2009). Introduction to syndemics: A critical systems approach to public and community health. Jossey-Bass.
- Skryabin, V. Y., Bryun, E. A., & Maier, L. J. (2020). Chemsex in Moscow: Investigation of the phenomenon in a cohort of men who have sex with men hospitalized due to addictive disorders. International Journal of STD & AIDS, 31(2), 136–141. https://doi.org/10.1177/0956462419886492
- Souleymanov, R., Brennan, D. J., Logie, C., Allman, D., Craig, S. L., & Halkitis, P. N. (2019). Pleasure and HIV biomedical discourse: The structuring of sexual and drug-related risks for gay and bisexual men who Party-n-Play. International Journal of Drug Policy, 74, 181–190. https://doi.org/10.1016/j.drugpo.2019.09.015
- Speulman, J., Druckler, S., Van Rooijen, M., & De Vries, H. (2019). P535 Chemsex & amp; sexual consent: A quantitative study on sexualized drug use in men who have sex with men and non-consensual sex. Sexually Transmitted Infections, 95(Suppl 1), A243. https://doi.org/10.1136/sextrans-2019-sti.612
- StataCorp. (2019). Stata Statistical Software: Release 16.
- Stevens, O., Moncrieff, M., & Gafos, M. (2020). Chemsex-related drug use and its association with health outcomes in men who have sex with men: A cross-sectional analysis of Antidote clinic service data. Sexually Transmitted Infections, 96, 124–130. https://doi.org/10.1136/sextrans-2019-054040
- Stuart, D. (2019). Chemsex: Origins of the word, a history of the phenomenon and a respect to the culture. Drugs and Alcohol Today, 19(1), 3–10. https://doi.org/10.1108/Dat-10-2018-0058
- Tan, R. K. J., O’Hara, C. A., Koh, W. L., Le, D., Tan, A., Tyler, A., Tan, C., Kwok, C., Banerjee, S., & Wong, M. L. (2021). Delineating patterns of sexualized substance use and its association with sexual and mental health outcomes among young gay, bisexual and other men who have sex with men in Singapore: A latent class analysis. BMC Public Health, 21(1), 1026. https://doi.org/10.1186/s12889-021-11056-5
- Tan, R. K. J., Phua, K., Tan, A., Gan, D. C. J., Ho, L. P. P., Ong, E. J., & See, M. Y. (2021). Exploring the role of trauma in underpinning sexualised drug use (‘chemsex’) among gay, bisexual and other men who have sex with men in Singapore. The International Journal on Drug Policy, 97, 103333. https://doi.org/10.1016/j.drugpo.2021.103333
- Tan, R. K. J., Wong, C. M., Chen, M. I., Chan, Y. Y., Bin Ibrahim, M. A., Lim, O. Z., Chio, M. T., Wong, C. S., Chan, R. K. W., Chua, L. J., & Choong, B. C. H. (2018). Chemsex among gay, bisexual, and other men who have sex with men in Singapore and the challenges ahead: A qualitative study. International Journal of Drug Policy, 61, 31–37. https://doi.org/10.1016/j.drugpo.2018.10.002
- Thomas, J. G. S., Brunton, J., Ghouze, Z., O’Driscoll, P., & Bond, M. (2020). EPPI-reviewer: Advanced software for systematic reviews, maps and evidence synthesis. EPPI-Centre, UCL Social Research Institute, University College London.
- Tomkins, A., Ahmad, S., Cannon, L., Higgins, S., Kliner, M., Kolyva, A., Ward, C., & Vivancos, R. (2018). Prevalence of recreational drug use reported by men who have sex with men attending sexual health clinics in Manchester, UK. International Journal of STD & AIDS, 29(4), 350–356. https://doi.org/10.1177/0956462417725638
- Tomkins, A., Vivancos, R., Ward, C., & Kliner, M. (2018). How can those engaging in chemsex best be supported? An online survey to gain intelligence in Greater Manchester. International Journal of STD & AIDS, 29(2), 128–134. https://doi.org/10.1177/0956462417719643
- Torres, T. S., Bastos, L. S., Kamel, L., Bezerra, D. R. B., Fernandes, N. M., Moreira, R. I., Garner, A., Veloso, V. G., Grinsztejn, B., & De Boni, R. B. (2020). Do men who have sex with men who report alcohol and illicit drug use before/during sex (chemsex) present moderate/high risk for substance use disorders? Drug and Alcohol Dependence, 209, Article 107908. https://doi.org/10.1016/j.drugalcdep.2020.107908
- Tricco, A., Lillie, E., Zarin, W., O’Brien, K., Colquhoun, H., Levac, D., Moher, D., Peters, M., Horsley, T., Weeks, L., Hempel, S., Akl, E., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M., Garritty, C., … Straus, S. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850
- Turner, K., Clarke, B., Priestley, C., Scofield, S., & Chapman, C. (2015). P209 ‘The grand slam’: Surveying the local landscape of ‘chemsex’ drug use amongst MSMS in a community outreach sexual health clinic. Sexually Transmitted Infections, 91(Suppl 1), A85. https://doi.org/10.1136/sextrans-2015-052126.253
- Uholyeva, X., & Pitoňák, M. (2022). Chemsex users in Czechia: EMIS survey. Central European Journal of Public Health, 30(2), 86–92. https://doi.org/10.21101/cejph.a6923
- Van Hout, M. C., Crowley, D., O’Dea, S., & Clarke, S. (2019). Chasing the rainbow: Pleasure, sex-based sociality and consumerism in navigating and exiting the Irish Chemsex scene. Culture, Health & Sexuality, 21(9), 1074–1086. https://doi.org/10.1080/13691058.2018.1529336
- Wang, H., D’abreu de Paulo, K. J. I., Gültzow, T., Zimmermann, H. M. L., & Jonas, K. J. (2022). Perceived monkeypox concern and risk among men who have sex with men: evidence and perspectives from the Netherlands. Tropical Medicine and Infectious Disease, 7(10). https://doi.org/10.3390/tropicalmed7100293
- Wang, Z., Yang, X., Mo, P. K. H., Fang, Y., Ip, T. K. M., & Lau, J. T. F. (2020). Influence of social media on sexualized drug use and chemsex among Chinese men who have sex with men: Observational prospective cohort study. Journal of Medical Internet Research, 22(7), e17894. https://doi.org/10.2196/17894
- Whitlock, G. G., Protopapas, K., Bernardino, J. I., Imaz, A., Curran, A., Stingone, C., Shivasankar, S., Edwards, S., Herbert, S., Thomas, K., Mican, R., Prieto, P., Nestor Garcia, J., Andreoni, M., Hill, S., Okhai, H., Stuart, D., Bourne, A., & Conway, K. (2021). Chems4EU: Chemsex use and its impacts across four European countries in HIV-positive men who have sex with men attending HIV services. HIV Medicine, 22(10), 944–957. https://doi.org/10.1111/hiv.13160
- Wong, N. S., Kwan, T. H., Lee, K. C. K., Lau, J. Y. C., & Lee, S. S. (2020). Delineation of chemsex patterns of men who have sex with men in association with their sexual networks and linkage to HIV prevention. International Journal of Drug Policy, 75, Article 102591. https://doi.org/10.1016/j.drugpo.2019.10.015
- World Bank Country and Lending Groups. (2020). The World Bank. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519
- Wu, H. H., Shen, Y. T., Chiou, C. S., Fang, C. T., & Lo, Y. C. (2019). Shigellosis outbreak among MSM living with HIV: A case-control study in Taiwan, 2015-2016. Sexually Transmitted Infections, 95(1), 67–70. https://doi.org/10.1136/sextrans-2017-053410